Abstract
Background Hip osteoarthritis in Japanese patients is in most cases secondary and purpose to congenital dislocation of the hip or acetabular dysplasia—often associated with a deformed femoral head. Thus, we examined the outcome of rotational acetabular osteotomy (RAO) procedures in patients with early-stage osteoarthritis secondary to developmental dysplasia of the hip, and its relationship to femoral head deformity.
Patients and methods We retrospectively reviewed the outcome of RAO procedures in 49 hips of 48 patients (43 females). All patients had radiographic evidence of early-stage osteoarthritis. The mean age was 33 (13–54) years at surgery, and the mean duration of follow-up was 13 (10–17) years. The roundness index of the femoral head was measured on preoperative radiographs. Clinical follow-up was performed using the Merle d'Aubigné and Postel system.
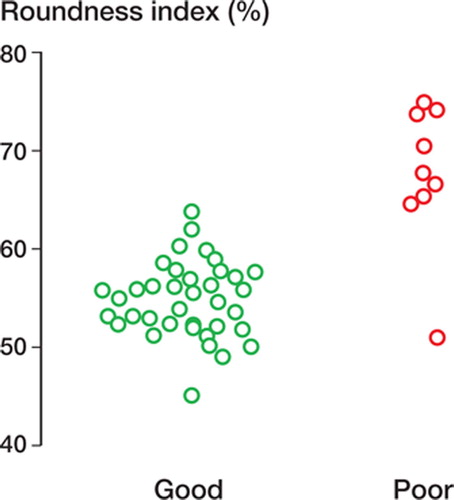
Results The mean preoperative clinical score was 13 points; this had improved to 17 points at the most recent follow-up (p < 0.001). Radiographically, this procedure gave adequate improvement of femoral head coverage. At follow-up, stage of osteoarthritis was unchanged in 38 hips and had progressed in 11 hips. 2 of the 11 hips with progression of the osteoarthritic stage had obvious technical failure and were excluded from subsequent comparisons. The mean preoperative round index of the femoral head was different for the 38 hips with no obvious progression than for the 9 hips that showed progression (55% and 68%, respectively; p < 0.001).
Interpretation Patients with a deformed femoral head may experience progression of osteoarthritis within 10 years of the RAO procedure, even in early-stage osteoarthritis.
Developmental dysplasia of the hip is the most common cause of secondary osteoarthritis in young adults. Steel's triple osteotomy (Steel Citation1973), Wagner's spherical acetabular osteotomy (Wagner Citation1976), the rotational acetabular osteotomy (RAO) developed by Ninomiya and Tagawa (Citation1984), and Ganz periacetabular osteotomy (Ganz et al. Citation1988) allow the femoral head to be covered with articular cartilage and have been used successfully in patients with developmental dysplasia of the hip and no or early osteoarthritic involvement (Nakamura et al. Citation1998b, Schramm et al. Citation1999, Siebenrock et al. Citation1999, Nozawa et al. Citation2000, Takatori et al. Citation2001). Acetabular dysplasia is common in the general population in Europe (Jacobsen et al. Citation2005). In Japan, hip osteorthritis is in most cases secondary, mainly due to congenital dislocation of the hip joint or acetabular dysplasia—often associated with a deformed femoral head (Hoaglund et al. Citation1985, Nakamura et al. Citation1989a).
In this study, we estimated the deformity of the femoral head in 48 patients. Here we report on the relationship between the long-term outcome of RAO with a minimum follow-up of 10 years and the preoperative deformity of the femoral head in early-stage osteoarthritis.
Patients and methods
Since 1985, we have performed the RAO procedure developed by Ninomiya and Tagawa (Citation1984) in 236 patients with developmental dysplasia of the hip (257 hips). Between 1985 and 1995, we performed RAO without concomitant femoral osteotomies for early-stage osteoarthritis (with acetabular dysplasia) on 60 hips (59 patients). The indication was a center-edge angle (CE angle) (Wiberg Citation1939) of less than 20° on radiographs, progressive pain that interfered with daily activities, and an age of less than 60 years. 1 patient was excluded from the study group because she developed a systemic disease that affected her ambulation significantly after the operation.
10 patients were lost to follow-up after more than 10 years. We were able to contact 3 of these patients by telephone; however, they did not visit our hospital. We could not contact the other 7 patients because they had moved elsewhere. Their mean age at the time of surgery was 35 (21–45) years, and the mean duration of follow-up was 5 (1–7) years. Radiographically, none of these patients showed signs of progression of arthritis. The remaining 48 patients (43 females; 49 hips) with more than 10 years of follow-up attended for clinical and radiographic assessment. The mean length of the postoperative follow-up was 13 (10–17) years. The mean age at operation was 33 (13–54) years.
Partial weight bearing with crutches was allowed in the sixth postoperative week, and full weight bearing at 4 months. The severity of osteoarthritis was radiographically staged into 4 groups as follows, based on the joint space, using a modified version of the classification system advocated by the Japanese Orthopedic Association (Nakamura et al. Citation1998). Early stage: more than 2 mm of joint space remaining. Early advanced stage: less than 2 mm of joint space, but no contact with the sub-chondral bone of the acetabulum and the femoral head. Late advanced stage: the subchondral bone of the acetabulum and the femoral head in contact within a localized area (less than 15 mm width) or less than 2 mm of joint space of more than 15 mm width. End stage: extensive loss of joint space (more than 15 mm width). In patients with a normal contralateral hip, half of the contralateral hip joint space was used in the classification system instead of 2 mm.
The functional results were evaluated by the hip joint scoring system of Merle d’ Aubigné and Postel (1954), which assigns a maximum of 6 points for each of 3 categories: pain, mobility, and gait function. A full score of 18 denotes normal hip function. Accordingly, a score of 17 or 18 points was considered excellent; 15 or 16 points, good; 13 or 14 points, fair; and 12 points or less, poor.
To evaluate deformity of the femoral head we used the roundness index, calculated as the ratio of the distances from the medial border to the top of the femoral head and the medial border to the lateral border of the femoral head () (Okano et al. Citation2003).
Anteroposterior radiographs were taken pre-operatively, 3 months postoperatively, and at the time of follow-up. We assessed position of the femoral head and hip morphology. The parameters evaluated included CE angle (Wiberg Citation1939), acetabular head index (AHI) (Heyman and Herndon Citation1950), and acetabular roof angle (Massie and Howorth Citation1950) ().
Figure 2. Radiographic parameters. A: CE angle; B: ace-tabular roof angle. Acetabular head index (AHI) = a/b × 100.
All radiographs were performed in the supine position. Anteroposterior radiographs were taken with a source-to-film distance of 110 cm. The patient's feet were internally rotated with the toes at 15 ± 5° to ensure that the X-ray beam was centered on the superior aspect of the pubic symphysis.
To test the reproducibility of the radiographic measurements, 3 authors (KO, HE, and MO) measured the CE angle, AHI, acetabular roof angle, and minimum width of the joint space in five randomly selected hips. Each observer measured each hip 3 times, with a 1-week interval between measurements. The values were then averaged. The data were analyzed for intraob server and interobserver variances and the coefficient of variation was calculated to be less than 5%. Thus, the reproducibility of the measurements was considered to be reasonable.
We used the Mann-Whitney U test to detect any association between outcome and the radiographic parameter, roundness index. Statistical significance was assumed at p-values less than 0.05.
Results
All patients had survived more than 10 years without any secondary operations. Most of them could walk without a cane for more than 30 min. Functionally, excellent or good results were seen in 44 hips, fair results in 3 hips, and poor results in 2 hips. The mean Merle d’ Aubigné clinical score improved from 13 (7–16) points preoperatively to 17 (11–18) points postoperatively (p < 0.001), mainly because of increased scores for pain reduction and walking ability. The mean pain score improved from 3.1 (1–5) points to 5.6 (3–6) points (p < 0.001). The mean mobility score decreased significantly from 5.7 (5–6) points to 5.3 (4–6) points (p = 0.007), and the mean walking ability score improved from 3.9 (1–6) points to 5.8 (3–6) points (p < 0.001).
Osteoarthritic stage was unchanged at the time of follow-up in 38 hips and had progressed in 11 hips. At the time of follow-up, 5 hips were graded as being at the early advanced stage, 3 hips were graded as being at the late advanced stage, and 2 hips were graded as being at the end stage. 2 of the 11 hips with progressed osteoarthritic stage had obvious technical failure and were excluded from subsequent comparisons. 1 of the excluded hips had incomplete coverage of the femoral head (AHI of 70%) and the other had intraarticular damage from the chisel. Thus, we compared the remaining 9 hips with poor outcome without technical failure (the “poor” group) to the 38 hips with a good outcome (the “good” group). The mean age at surgery and mean length of the follow-up period were 32 (13–54) years and 13 years, respectively, for the good group, and 38 (32–47) years and 14 years for the poor group. Thus, both the age at surgery and the follow-up time were similar in the two groups.
The mean preoperative roundness index of the femoral head was different: 55% (45–63) in the good group and 68% (51–75) in the poor group (p< 0.001) (). The CE angle, AHI, and acetabular roof angle were improved after surgery (p < 0.001) with no significant preoperative, postoperative, and follow-up differences in these parameters between the groups (Table).
Figure 3. Roundness index of the femoral head and radiological results (good versus poor: p < 0.001).
Comparison of radiographic parameters between the "good" and "poor" groups (unaltered osteoarthritic stage and progressed osteoarthritic stage, respectively)
Complications
There were no cases of deep-tissue infection or major neurovascular complications. 2 patients developed transient irritation of the lateral femoral cutaneous nerve. Thrombosis of the deep femoral vein occurred in 1 patient. There was technical failure, as described above, in 2 patients. Both hips had been operated in the early years, soon after RAO had been introduced at our hospital.
Discussion
Satisfactory long-term results of RAO have been reported for early-stage osteoarthritis secondary to developmental dysplasia of the hip (Nakamura et al. Citation1998b, Takatori et al. Citation2001, Nozawa et al. Citation2002). Furthermore, the efficacy of this procedure has also been shown in patients with severe dysplasia of the hip at an early stage (Takatori et al. Citation1996, Nozawa et al. Citation2000, Clohisy et al. Citation2005). We found that RAO was not effective in maintaining the preoperative osteoarthritic stage in patients with a severely deformed femoral head, even in early osteoarthritis of the hip.
Our study has several limitations. Firstly, the round index that we proposed only addressed a two-dimensional aspect of the three-dimensional structure of the femoral head. However, we usually used anteroposterior radiographs to decide the indications for pelvic osteotomy. Secondly, 6 of 11 patients in whom osteoarthritis progressed still had good clinical results (a total hip score of 15–16) at the time of follow-up. However, 5 of these 6 patients experienced mild pain when walking.
Matsui et al. (Citation1997) described factors that were significantly associated with the outcome of RAO procedures in early-stage osteoarthritis, and reported that among other factors, deformity of the head—while not a significant factor—might well influence the long-term outcome.
The influence of shape of the femoral head on the radiographic result of RAO in early osteoarthritis has been considered in previous studies. Ninomiya (Citation1996) suggested that an additional procedure, such as valgus osteotomy, should be considered for acetabular dysplasia associated with a severely deformed femoral head. However, the authors did not define “severe deformity”. Nakamura et al. (Citation1998a) divided patients with early osteoarthritis into two groups, “round” and “not-round”, according to the shape of the femoral head— where “round” was defined as the curvature with an equidistant radius of the femoral head from the joint surface. The “not-round” group had a significantly poorer radiographic outcome than the “round” group. Takatori et al. (Citation2001) reported that the osteoarthritis had progressed radiographically in 8 of 15 patients with early osteoarthritis after 20 years. All 8 hips in which the osteoarthritic stage had progressed had a deformed femoral head. In contrast, 4 of the 7 patients without progression of coxarthrosis had a spherical femoral head.
Primary osteoarthritis is an extremely rare condition in Japan (Nakamura et al.Citation1989). The most common causes of osteoarthritis include congenital dislocation of the hip joint and acetabular dysplasia. Various degrees of femoral head deformity are associated with osteoarthritis secondary to developmental dysplasia of the hip ().
Figure 4. Various degrees of deformity of the femoral head and the associated roundness index. As deformation of the femoral head increases, the top of the femoral head moves laterally. The black square shows the top of the femoral head.
To our knowledge, there have been no reports detailing how deformity of the femoral head may influence the long-term outcome of RAO. We used the roundness index ( Okano et al. Citation2003) and found that it was different in patients with good and poor results. All patients with a roundness index of more than 64% had progression of osteoarthritis. One possible reason for this radiographic deterioration is that the weight-bearing load was concentrated laterally on the femoral head as a shearing force, and resulted in progressive narrowing of the joint space over a period of more than 10 years ().
Figure 5. A. 34-year-old woman with early-stage osteo-arthritis preoperatively. The hip score was 10 points and the roundness index was 68%. B. 3 months postoperatively. C. 11 years postoperatively: narrowed joint space on the lateral side; late advanced stage coxarthrosis. The hip score was 15 points.
Preoperative functional radiography was also performed in all our patients. 6 of 9 hips in the “poor” group showed good joint congruency on preoperative anteroposterior plain radiographs of the hip in abduction. RAO for early-stage osteoarthritis in patients with a deformed femoral head must be considered carefully despite good congruency on preoperative radiographs in abduction.
Yanagimoto et al. (Citation2005) reported indications for Chiari osteotomy based on the roundness index for advanced osteoarthritis. A flat femoral head, defined as a roundness index of more than 65%, predicted a good surgical outcome; however, patients with a spherical femoral head may still experience early progression to osteoarthritis. If the preoperative roundness index of the femoral head is higher than 64%, progression of arthritis cannot be prevented by the RAO procedure in the long term, even in early coxarthrosis. Another kind of osteotomy, such as Chiari pelvic osteotomy (Chiari Citation1974), should be selected for patients with severe deformity of the femoral head.
In conclusion, early-stage osteoarthritis with a round femoral head is considered a good indication for RAO because of favorable results at 10 years and beyond. In contrast, patients with a severely deformed femoral head—defined as a round index of more than 64% and early-stage osteoarthritis— may experience progression of osteoarthritis within 10 years after RAO.
No competing interests declared.
Contributions of authors
All authors contributed to the conception and design of the study and manuscript preparation. In addition, individual authors contributed as follows. KO: data collection, data proceeding, statistical analysis, and writing of manuscript. HE: data collection and interpretation. MO and HS: interpretation.
- Chiari K. Medial displacement osteotomy of the pelvis. Clin Orthop 1974, 98: 55–71
- Clohisy J C, Barrett S E, Gordon J E, Delgado E D, Schoe-necker P L. Periacetabular osteotomy for the treatment of severe acetabular dysplasia. J Bone Joint Surg (Am) 2005; 87: 254–9
- Ganz R, Klaue K, Vinh T S, Mast J W. A new periacetabular osteotomy for the treatment of hip dysplasiasTechnique and preliminary results. Clin Orthop 1988, 232: 26–36
- Heyman C H, Herndon C H. Legg-Perthes disease A method for the measurement of the rentogenographic result. J Bone Joint Surg (Am) 1950; 32: 767–78
- Hoaglund F T, Shiba R, Newberg A H, Leung K Y. Diseases of the hip A comparative study of Japanese Oriental and American white patients. J Bone Joint Surg (Am) 1985; 67: 1376–83
- Jacobsen S, Sonne-Holm S, Soballe K, Gebuhr P, Lund B. Hip dysplasia and osteoarthrosis: a survey of 4151 subjects from the Osteoarthrosis Substudy of the Copenhagen City Heart Study. Acta Orthop 2005; 76: 149–58
- Massie W K, Howorth M B. Congenital dislocation of the hip. Part I. Methods of grading results. J Bone Joint Surg (Am) 1950; 32: 519–41
- Matsui M, Masuhara K, Nakata K, Nishii T, Sugano N, Ochi T. Early deterioration after modified rotational acetabular osteotomy for the dysplastic hip. J Bone Joint Surg (Br) 1997; 79: 220–4
- Merle d'Aubigne R, Postel M. Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg (Am) 1954; 36: 451–75
- Nakamura S, Ninomiya S, Nakamura T. Primary osteoarthritis of the hip joint in Japan. Clin Orthop 1989, 241: 190–6
- Nakamura S, Morimoto S, Takatori Y, Umeyama T, Ninomiya S. Rotational aectabular osteotomy for the hip with no or early osteoarthritis relationship between femoral head deformity and long-term results. Hip Joint 1998a; 24: 38–40, (in Japanese)
- Nakamura S, Ninomiya S, Takatori Y, Morimoto S, Umeyama T. Long-term outcome of rotational acetabular osteotomy: 145 hips followed for 10–23 years. Acta Orthop Scand 1998b; 69: 259–65
- Ninomiya S. Rotational acetabular osteotomy-long-term results. J Jpn Orthop Assoc 1996; 70: 7–16, (in Japanese)
- Ninomiya S, Tagawa H. Rotational acetabular osteotomy for the dysplastic hip. J. Bone Joint Surg (Am) 1984; 66: 430–6
- Nozawa M, Shitoto K, Hirose T, Matsuda K, Michino K, Kajihara H, Maezawa K, Kurosawa H. Rotational acetab-ular osteotomy for severely dysplastic acetabulum. Arch Orthop Trauma Surg 2000; 120: 376–9
- Nozawa M, Shitoto K, Matsuda K, Maezawa K, Kurosawa H. Rotational acetabular osteotomy for acetabular dys-plasia. A follow-up for more than ten years. J Bone Joint Surg (Br) 2002; 84: 59–65
- Okano K, Enomoto H, Osaki M, Shindo H. Clinical results of rotational acetabular osteotomy (RAO) for advanced osteoarthritis of the hip-evaluation of the shape of the femoral head. Hip Joint 2003; 29: 102–8, (in Japanese)
- Schramm M, Pitto R P, Rohm E, Hohmann D. Long-term results of spherical acetabular osteotomy. J Bone Joint Surg (Br) 1999; 81: 60–6
- Siebenrock K A, Scholl E, Lottenbach M, Ganz R. Bernese periacetabular osteotomy. Clin Orthop 1999, 363: 9–20
- Steel H H. Triple osteotomy of the innominate bone. J Bone Joint Surg (Am) 1973; 55: 343–50
- Takatori Y, Ninomiya S, Nakamura S, Morimoto S, Sasaki T. Long-term follow-up results of rotational acetabular osteotomy in painful dysplastic hips: efficacy in delaying the onset of osteoarthritis. Am J Orthop 1996; 25: 222–5
- Takatori Y, Ninomiya S, Nakamura S, Morimoto S, Moro T, Nagai I, Mabuchi A. Long-term results of rotational acetabular osteotomy in patients with slight narrowing of the joint space on preoperative radiographic findings. J Orthop Sci 2001; 6: 137–40
- Wagner H. Osteotomies for congenital hip dislocation. The hip. Proceedings of the Fourth Open Scientific Meeting of The Hip Society. CV Mosby, St. Louis 1976; 45–66
- Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint: with special reference to the complication of osteoarthritis. Acta Chir Scand (Suppl.) 1939; 83: 1–135
- Yanagimoto S, Hotta H, Izumida R, Sakamaki T. Long-term results of Chiari pelvic osteotomy in patients with developmental dysplasia of the hip: indications for Chiari pelvic osteotomy according to disease stage and femoral head shape. J Orthop Sci 2005; 10: 557–63