Abstract
Background and purpose Our institution began using the Kinemax total knee arthroplasty system in 1988, both with and without cement fixation. We report 10–year survival figures.
Methods Theater records showed that 284 Kinemax total knee arthroplasties had been performed 1988 through 1993. Life-table survival estimates were used to determine the probability of survivorship 10 years after surgery for the total group and by age, sex, diagnosis, and mode of fixation. Median follow-up was 11 (0.8–15) years for unrevised knees in patients who were still alive.
Results The 10–year cumulative survivorship was higher (93%, 95% CI: 81–97) when both components had been cemented than if either, or both, were uncemented (77%, CI: 67–83; p < 0.001). There was an increased incidence of failure in patients who were less than 60 years of age at the time of surgery (p = 0.004).
Interpretation The smooth-backed Kinemax knee without cement was found to be associated with a high failure rate at 10 years. The 10–year cumulative survival results of the cemented prosthesis are acceptable.
The Kinemax knee system has evolved from its precursor, the Kinematic knee, and was introduced in 1988. The Kinematic design has an “anatomical” (asymmetrical) patellofemoral articulation and a metal-backed tibial component. Despite the fact that 10–year survival has been quoted as being as high as 92% (Cobb et al. Citation1990, Rand et al. Citation2003), problems were encountered with patellar component loosening (Mason et al. Citation1994) and fracture of the medial tibial tray (Abernethy et al. Citation1996).
The Kinemax was developed with a return to symmetrical patellofemoral articulation. It allows the option of either sacrificing or retaining the posterior cruciate ligament, and the same smooth-surfaced components can be implanted with or without cement. Early results were encouraging, and Ewald (Citation1996) reported no component loosening or revisions in 521 cemented Kinemax knees at 5 years, with only a 1% incidence of patellar complications. This cohort of patients came from the institution where the surgeons were involved with the design of the Kinemax and their 10–year results showed a cumulative survival rate of 96% (Wright et al. Citation2004).
In an independent study, Back et al. (Citation2001) found a survival rate of 99% at 5 years in 364 cemented implants (from an initial sample of 422), and all revisions were for either trauma or infection. The Norwegian Joint Registry (Furnes et al. Citation2002) reported 213 Kinemax implants with 5–year survival of 98%. The frequency of patellofemoral complications with the Kinemax has been found to be acceptable, and lower than for previous implants (Harwin Citation1998). In Citation1992 Nafei et al. published a comparison of 26 cemented Kinemax knees with 19 uncemented knees and 30 hybrid cases (in which only the femoral component was cemented). Of the uncemented knees and hybrids, 10 had been revised less than 2 years postoperatively (compared to none of the cemented knees). The decision of whether or not to use cement was made intraoperatively, based on judgement of the fit of the prosthesis.
The Kinemax total knee replacement system was first implanted in our institution (the Freeman Hospital, Newcastle-upon-Tyne, UK) in 1988—with both cemented and uncemented fixation of the smooth-backed components—and was used in patients with osteoarthritis and inflammatory arthritis. Due to concerns regarding the use of cement at that time, the surgeons had preferred uncemented fixation; the decision to use cemented fixation was based on intraoperative subjective findings of bone quality. In some cases the bone quality was felt to be acceptable for one component but not the other, in which case one was cemented and the other not. If, having inserted one or both components without cement, there was felt to be poor stability or hold, then—again—cement was used. It should be noted that even at this time, there were few centers using uncemented fixation, and the use of uncemented smooth-backed components has since fallen out of use.
Here we report our 10–year survival analysis of the cemented and uncemented smooth-backed Kinemax total knee arthroplasty at our institution.
Patients and methods
Our Local Joint Ethics Committee approved the study. Theater records were used to find patients in whom Kinemax implants had been used between November 1988 and May 1993.
Patient demographic details were recorded, along with the operating surgeon, the side, and the catalog numbers of all implants used. The case notes of the patient were then retrieved, and from these the indication for surgery (osteoarthritis, rheumatoid disease, or other), operative details (use of cement, the state of the posterior cruciate ligament (PCL), and patellar resurfacing), and follow-up assessments were recorded—including the date of the last radiographs of the prosthesis. If the prosthesis had not been revised, the date of the last clinical and radiographic follow-up of the prosthesis was noted. If any revision surgery had been carried out, the clinical and radiographic indications for this were recorded, along with the date of revision and the operative findings.
If patients were alive with the primary arthroplasty in situ, and had not been reviewed more than ten years postoperatively, they were offered an appointment for clinical and radio-graphic review by an independent observer (DJC) or by our arthroplasty nurse specialists.
Analysis
Life table survival estimates were used to determine the estimated probability of survivorship at a minimum of 10 years after primary total knee arthroplasty. Survivorship analysis was generated using aseptic loosening, polyethylene wear, and instability as endpoints.
Univariate analyses of associations between aseptic failure and the binary independent variables were conducted using Chi-squared tests. A 5% significance level was maintained throughout these analyses, and all tests were two-sided. Data were analyzed using SAS (version 8.0).
Results
We identified 302 Kinemax total knee arthroplasties from theater records covering the specified period. Of these, in 24 records (held as scanned logbook pages on CD-ROM) patient details were unidentifiable due to poor-quality images. This left a study group of 284 knees in 248 patients (36 bilateral cases). For 106 knees, the patients (number) had already died at the time of review (9 of whom had been revised). The median follow-up time for deceased, unrevised patients was 5 years. For 178 knees, the patients (number) were still alive at the time of review (40 of whom had been revised). Median follow-up time for the 138 unrevised knees in living patients was 10.6 (0.8–14.7) years; 59 unrevised knees were reviewed for longer than 10 years.
79 patients were alive with the primary prosthesis in situ and had less than 10 years of follow-up documented in their case notes. These patients were invited for clinical and radiographic review, and 30 attended the review. In the case of three patients who were thought to still be alive, we could find no record of follow-up and failed to make contact with them. For those who did not attend, we used the date and assessment from their last documented clinic and radiological review. For these patients this was documented as their last follow-up, and patients were censored at that point. The case notes could not be retrieved in 10 cases. There were thus 89 unrevised knees in living patients with 10–year follow-up and 49 knees were lost to follow-up ().
Figure 1. Flow chart representing follow-up for patients who had Kinemax knee replacement at least 10 years previously, and showing when knees were censored or listed as having failed.
The mean age at surgery was 62 (16–90) years. 152 patients (62%) were female. The diagnosis was osteoarthritis in 137 cases (58%), rheumatoid arthritis in 93 cases (39%), and other diagnoses (including juvenile chronic arthritis and psoriatic arthritis) in 7 cases. In 11 cases, there was no record of the diagnosis. In two-thirds of cases, the operating surgeon was one of the authors (IMP) and 3 other surgeons operated on the remaining cases.
All cases received antibiotic prophylaxis with cefuroxime at induction and at least 2 doses post-operatively. The patella was resurfaced in only 1 case, and the PCL retained in all cases. Both tibial and femoral components were fixed with Palacos bone cement in 109 cases (42%). Neither component was cemented in 130 cases (50%). Of the remainder, the tibia alone was cemented in 3 cases, and the femoral component alone in 20 cases. There was no record available of the fixation in 22 cases.
Revision surgery was carried out in 49 cases (20%) (). The cumulative survival rate at 10 years was 80% (95% CI: 74–85). 37 knees underwent revision surgery for aseptic failure, which included revisions for loosening, polyethylene wear, and instability. The following analyses focus on the aseptic failures that resulted in revision surgery, and associated risk factors.
Table 1. Indications for revision surgery and reoperations
The cumulative survival rate at 10 years was 84% (95% CI: 78–89). The survival curves for cemented and uncemented knees using the date of revision surgery for aseptic failure as an endpoint are shown in . Bivariate analysis of factors influencing survivorship at 10 years showed significant differences between cemented and uncemented fixation of the components (p < 0.001), and—independently—between patients less than 60 years old or those 60 years old or more at primary surgery (p = 0.004). There was a higher proportion of revisions for aseptic failure in patients with rheumatoid arthritis than in patients with osteoarthritis (p = 0.036) (). Most aseptic failures that resulted in revision were in patients who were under 60 years at the time of surgery and in whom the components were uncemented; the accumulation of these risk factors had a catastrophic effect on the life of the prosthesis (). A higher proportion of patients who were less than 60 years of age at the time of surgery (96/123, 78%) had an uncemented technique compared to patients who were ≥ 60 years old at the time of surgery (50/127, 39%) (p < 0.001).
Figure 2. Kaplan-Meier Survival estimates with 95% confidence intervals for uncemented and cemented knees using date of revision surgery as an endpoint for failures.
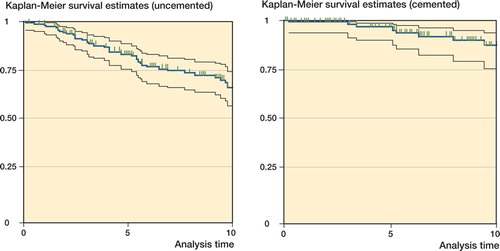
Table 2. Bivariate analysis for aseptic failures resulting in revision surgery
Table 3. Survivorship analysis by accumulated risk factors for aseptic failures resulting in revision surgery
Discussion
In our study population, younger age at implantation appears to have been an independent risk factor for revision before 10 years. The Norwegian Joint Registry (Furnes et al. Citation2002) found an increased rate of revision in patients less than 60 years at surgery, and more failures have been seen in rheumatoid patients with total knee replacements who were less than 55 years old in the Swedish registry (Robertsson et al. Citation1997). The Swedish Knee Registry has, however, identified poorer survivorship of TKA for younger patients with OA, but not rheumatoid disease (Robertsson et al. Citation1997). Younger age has also been identified as a risk factor for failure in two American series (Rand et al. Citation2003, Vasquez-Vela Johnson et al. Citation2003). There has been a move in recent years towards more conservative management of early knee osteoarthritis in younger patients, including osteotomy and unicon-dylar knee arthroplasty (Pagnano et al. Citation2005).
Although our series of Kinemax total knee arthroplasties used smooth-backed components in both cemented and uncemented modes, it has again raised the issue of cementless fixation. The use of uncemented total knee arthroplasty remains controversial. Originally devised in an attempt to reduce failure rates primarily associated with cement fixation, several studies using an uncemented technique have reported divergent results (Campbell et al. Citation1998, Duffy et al. Citation1998, McCaskie et al. Citation1998, Bergher et al. Citation2001, Schroder et al. Citation2001, Khaw et al. Citation2002, Parker et al. Citation2002, Vasquez-Vala Johnson et al. Citation2003). We found a significantly higher rate of revision, particularly for aseptic loosening, when one or both components were uncemented. Unlike many other comparisons of cemented and uncemented components, however, these components were of the same smooth-backed design regardless of the method of fixation. In other components, particularly the PFC, there seems to be a similarly higher failure rate if the smooth-backed component designed for cementing is inserted without cement (Duffy et al. Citation1998). In one series in which specifically designed uncemented components were compared with cemented components, results appeared similar (Parker et al. Citation2002), but McCaskie et al. (Citation1998) found poorer results with uncemented porous-coated implants. The use of porous-coated uncemented arthroplasty specifically in patients under 50 years of age has also been reported (Hofmann et al. Citation2002); although there were no revisions at mean a follow-up of 9 years in 75 knees, 12 polyethylene liners had been exchanged-5 because of wear. Using data from the Swedish Knee Registry, Robertson et al. (Citation1997) found that uncemented tibial components had a significantly poorer survivorship in TKA for OA (but not RA). There was no difference in survival rate when only the femur or patella was uncemented.
One further possible factor in the early failure of the uncemented Kinemax knee is the design of the femoral component, whereby the anterior and posterior flanges of the implant are parallel. This may increase the risk of an imperfect fit—especially relevant if no cement is used, and magnified by its smooth-backed nature. When the Kinemax Plus prosthesis was introduced, the femoral component was designed with a slight wedge shape to improve the press fit. The survivorship of this implant (cemented) at 7 years has been reported to be 95% (Forster et al. Citation2002).
Our series represents high-volume early use of the Kinemax implant. It should also be remembered that there was a hypothesis at the time regarding “cement disease”, and there were moves away from cemented implants, particularly in younger patients. We found an overall survival rate of 93% for the cemented Kinemax total knee at 10 years. Previous reports have found more favorable 10–year results, and a recent study from Boston found 96% survivorship at ten years in cemented Kinemax knees (Wright et al. Citation2004). Patients in our cohort were on average 8 years younger than those in the Boston group, and a higher proportion had rheumatoid arthritis (39% in our series, 20% in the Boston series). In our series, these factors were both found to be associated with a significantly lower survival rate, independently of the mode of fixation.
Our findings demonstrate the satisfactory long-term results of the Kinemax design, but highlight the problems of using components without cement unless they are specifically designed for that purpose, particularly in younger patients.
No competing interests declared.
Contributions of authors
DJC: data collection and writing of manuscript. MK: assistance with data collection, and writing of manuscript. IMP: lead operating surgeon. AWM: overall supervision of study. EAL: study design and statistical analysis.
- Abernethy P J, Robinson C M, Fowler R M. Fracture of the metal tray after Kinematic total knee replacement: a common cause of failure. J Bone Joint Surg (Br 1996; 78(2)220–5
- Back D L, Cannon S R, Hilton A, Bankes M J, Briggs T W. The Kinemax total knee arthroplasty. Nine years experience. J Bone Joint Surg (Br) 2001; 83(3)359–63
- Berger R A, Lyon J H, Jacobs J J, Barden R M, Berkson E M, Sheinkop M B, Rosenberg A G, Galante J O. Problems with cementless total knee arthroplasty at 11 years follow-up. Clin Orthop 2001, 392: 196–207
- Campbell M D, Duffy G P, Trousdale R T. Femoral component failure in total knee arthroplasty. Clin Orthop 1998, 356: 58–65
- Cobb A C, Ewald F C, Wright J, Sledge C B. The Kinematic knee survivorship analysis of 1934 knees. J Bone Joint Surg (Br) 1990; 72: 532–6
- Duffy G P, Berry D J, Rand J A. Cement versus cement-less fixation in total knee arthroplasty. Clin Orthop 1998, 356: 66–72
- Ewald F C. Boston experience with the Kinematic/Kinemax knee systems. The Total Knee Symposium, Killarney Ireland 1996
- Forster M C, Kothari P, Howard P W. Minimum 5 year follow-up and radiologic analysis of the all-polyethyl-ane tibial component of the Kinemax Plus System. J Arthroplasty 2002; 17(2)196–200
- Furnes O, Espehaug B, Lie S A, Vollset S E, Engesaeter L B, Havelin L I. Early failures among 7174 primary total knee replacements: a follow-up study from the Norwegian Arthroplasty Register 1994–2000. Acta Orthop Scand 2002; 73(2)117–29
- Harwin s f. Patellofemoral complications in symmetrical total knee arthroplasty. J Arthroplasty 1998; 13(7)753–62
- Hofmann A A, Heithoff S M, Camargo M. Cementless total knee arthroplasty in patients 50 years or younger. Clin Orthop 2002, 404: 102–7
- Khaw F M, Kirk L M, Morris R W, Gregg P J. A randomised, controlled trial of cemented versus cementless press-fit condylar total knee replacement. Ten year survival analysis. J Bone Joint Surg (Br) 2002; 84(5)658–66
- Mason M D, Ewald F C, Wright J, Thomas W H, Poss R, Sledge C B, Walker P S. Ten to 13 year review of a non-constrained cruciate-retaining total knee. Orthop Trans 1994; 17: 1091–5
- McCaskie A W, Deehan D J, Green T P, Lock K R, Thompson J R, Harper W M, Gregg P J. Randomised, prospective study comparing cemented and cementless total knee replacement: results of press-fit condylar total knee replacement at five years. J Bone Joint Surg (Br) 1998; 80(6)971–5
- Nafei A, Neilsen S, Kristensen O, Hvid I. The press-fit Kinemax knee arthroplasty. High failure rate of non-cemented implants. J Bone Joint Surg (Br) 1992; 74(2)243–6
- Pagnano M W, Clarke H D, Jacofsky D J, Amendola A, Repicci J A. Surgical treatment of the middle-aged patient with arthritic knees. Instr Course Lect 2005; 54: 251–9
- Parker D A, Rorabeck C H, Bourne R B. Long-term follow-up of cementless versus hybrid fixation for total knee arthroplasty. Clin Orthop 2002, 388: 68–76
- Rand J A, Trousdale R T, Ilstrup D M, Harmsen W S. Factors affecting the durability of primary total knee prostheses. J Bone Joint Surg (Am) 2003; 85(2)259–65
- Robertsson O, Knutson K, Lewold S, Goodman S, Lidgren L. Knee arthroplasty in rheumatoid arthritis. A report from the Swedish Knee Arthroplasty Register on 4381 primary operation 1985–1995. Acta Orthop Scand 1997; 68(6)545–53
- Schroder H M, Berthelsen A, Hassani G, Hansen E B, Sol-gaard S. Cementless porous-coated total knee arthroplaty: 10–year results in a consecutive series. J Arthroplasty 2001; 16(5)559–67
- Vazquez-Vela Johnson G, Worland R L, Keenan J, Noram-buena N. Patient demographics as a predictor of the ten-year survival rate in primary total knee replacement. J Bone Joint Surg (Br) 2003; 85(1)52–6
- Wright R J, Sledge C B, Poss R, Ewald F, Walsh M E, Lin-gard E A. Patient-reported outcome and survivorship after Kinemax total knee arthroplasty. J Bone Joint Surg (Am) 2004; 86: 2464–70
