Abstract
Background and purpose Implant dislocation is one of the commonest complications following primary total hip replacement (THR). We investigated the effect of body mass index (BMI) and tobacco use on the risk of this complication.
Subjects and methods Through linkage between the Swedish Construction Workers’ cohort and the Swedish Inpatient Register, 2,106 male patients who had undergone primary THR between 1997 and 2004 were identified. We used Cox multivariable regression analysis to study the association between BMI and tobacco use and the risk of implant dislocation.
Results 53 patients (2.5%) developed implant dislocation during a mean of 2 (0–3) years of follow-up. We found overweight and obesity to be associated with increased risk of implant dislocation (HR = 2.5,95% CI: 1.1–5.5 and HR = 3.7, 95% CI: 1.5–9.3, respectively as compared to those of normal weight). There was no statistically significant association between tobacco use and the risk of dislocation.
Interpretation Greater attention should be given to high BMI as a risk factor for implant dislocation following THR.
Implant dislocation is one of the commonest complications after total hip replacement (THR), and occurs in 1–4% of patients (Lindberg et al. Citation1982, McCollum et al. Citation1990, Hedlundh et al. Citation1992). Between 1979 and 2005, implant dislocation was the second most common cause of reoperations registered in the Swedish National Hip Arthroplasty Register and accounted for 11% of all the documented reoperations (Herberts et al. Citation2005). Similar results have been reported by the Norwegian Arthroplasty Register (Havelin et al. Citation2000).
In addition to inconvenience for the patient, implant dislocation is associated with increased hospital costs. Sanchez-Sotelo et al. (Citation2006) recently reported that each episode of closed reduction following implant dislocation represents 19% of the hospital cost of an uncomplicated THR.
Many factors have been suggested to be associated with implant dislocation following THR (Morrey Citation1997). These can be divided into disease-related and patient-related factors (e.g. developmental dysplasia of the hip, high age, and alcohol abuse), factors associated with surgical technique and design (e.g. posterior approach and excessively retroverted/antroverted cup orientation) and post-surgical factors (e.g. extreme positions of the limb such as excessive flexion or rotation).
Two lifestyle factors that could affect the outcome after THR are high body mass index (BMI) and tobacco use. Both of these risk factors have been reported to increase the risk of short-term complications such as wound infections and pulmonary events following THR (Moller et al. Citation2003, Sadr Azodi et al. 2006). Previous studies have not found any significant association between high BMI and the risk of implant dislocation in patients undergoing primary THR (Woolson and Rahimtoola Citation1999, Khatod et al. Citation2006, McLaughlin and Lee Citation2006). However, these studies involved between 1 and 28 events of implant dislocation, which could have resulted in insufficient statistical power to study the association between high BMI and the risk of implant dislocation.
To our knowledge, there have been no previous studies investigating the possible association between tobacco use and the risk of implant dislocation following THR. Smoking is associated with reduced bone mineral density (Szulc et al. Citation2002) and impeded bone healing following various types of fractures (W-Dahl and Toksvig-Larsen Citation2004, Castillo et al. Citation2005, Little et al. Citation2006). Thus, smoking could also have an effect on the risk of implant dislocation.
We used a large, nationwide occupational cohort with prospectively collected information on exposure to investigate the effect of BMI and tobacco use on the risk of implant dislocation following primary THR.
Subjects and methods
The Swedish Construction Workers cohort
The Swedish Construction Industry's Organisation for Working Environment Safety and Health (Byg-ghälsan), established in 1968, provided outpatient medical services to construction workers all over Sweden from 1969 through 1992 (Engholm et al. Citation1987). The main activity was preventable heath check-ups, offered to all blue- and white-collar workers in the building industry through regular personal invitation and through visits to—or advertisements at—virtually all major building sites. The resulting cohort consisted of 386,000 construction workers and most of them were men (95%).
Assessment of exposure
On average, every person underwent 3 (1–9) health check-ups, 2–3 years apart. Information on exposure was collected by means of an extensive self-administered questionnaire before each visit to the clinic. Among other things, this questionnaire covered detailed smoking history and anthropometric measures. To avoid misunderstandings or inconsistencies, the answers were double-checked by a nurse at the time of the visit. The quality of the smoking data has been reviewed previously (Nyrén et al. Citation1996). Briefly, in that study missing data on duration of smoking was noted in 1.3% of current smokers and 1.4% of previous smokers. Perfect concordance between reports on smoking status 2–3 years apart was found in 89% of cases. Inconsistencies (e.g. subjects who indicated that they were current or ex-smokers in the first questionnaire and then asserted that they had never smoked in the second questionnaire) were found in 2.6% of cases.
The Swedish Inpatient Register
National healthcare in Sweden is based on administratively independent county councils and is funded mainly by local taxes. The private sector is small and provides mainly elective care. Established in 1964, the National Board of Health and Welfare has collected data on individual hospital discharges in the Inpatient Register (Hansson et al. Citation1996). Besides the national registration number (NRN) (uniquely identifying each resident in Sweden), each record could contain as many as 8 discharge diagnoses, coded according to the current International Classification of Diseases (ICD). Furthermore, each record lists up to 12 surgical codes assigned according to the Swedish Classification of Operations and Major Procedures. Patients are identified through their NRN, which are included in each record. The register has been evaluated for validity and completeness, and the codes for the main diagnoses were correct at the 3-digit level for 92–94% of the records on surgical patients (Naessen et al. Citation1989, Nilsson et al. Citation1994). For surgical procedures (excluding endoscopies and biopsies), the codes were incorrect in 2% of the records and they were missing in 5.3% (Nilsson et al. Citation1994).
Cohort identification
We used the Swedish NRN for linkage to the Swedish Inpatient Register, to identify all construction workers who were discharged from hospital with a procedure code of total hip replacement between 1997 and 2004. We included construction workers who had undergone unilateral THR due to primary osteoarthritis of the hip. Most of this cohort consisted of male patients (94%); thus, we restricted our material to male subjects. To reduce possible confounding, we excluded patients who had undergone previous THR; who had diagnosis codes for rheumatic diseases, secondary osteoarthritis, or lower extremity fractures; all cases of previous orthopedic surgical procedures from the lower back to the ankle joint; and individuals with erroneous personal identification numbers. Furthermore, we excluded individuals who were ever discharged from hospital with diagnosis codes indicating alcohol or drug abuse. The final cohort consisted of 2,106 subjects.
Follow-up
The outcome of interest was the first-time event of implant dislocation corrected by a non-surgical repositioning. Study subjects were also followed until the end of follow-up, emigration, or death— as provided through linkage with the Swedish Emigration Register and the Cause of Death Register (Lagerlund et al. Citation2005)—whichever occurred first. Furthermore, patients were censored at the time of admission to hospital if they underwent reoperation due to prosthesis-related complications. The information about which hip (right or left) that had undergone THR was missing for the majority of the subjects (91%). Therefore, we also chose to censor patients at the time of a new THR or other hip prosthesis surgery. The cohort was followed for a maximum of 8 years, up to the end of 2004.
This study was approved by the ethical board review committee of Umeå University (§235/03, dnr 03–191).
Statistics
The BMI of the patients was categorized into 3 groups according to the World Health Organisation (WHO) criteria: normal weight (18.5–24.9 kg/ m2), overweight (25–29.9 kg/m2), and obese (30+ kg/m2). When assessing the amount of tobacco smoked on a daily basis, cigarettes were assumed to contain 1 g of tobacco, and cigars 6 g. Pipe smokers reported the amount of tobacco (in grams) consumed each week. Pack years was defined as the total amount of tobacco smoked every day multiplied by the length of time the patient had been smoking, and divided by 20. Pack years were then divided into 3 categories (never-smokers, 0–19.9 pack years, 20+). The overall smoking status was categorized as never-smoker, previous smoker, and current smoker.
The Kaplan-Meier method was used to estimate the crude cause-specific survival distribution of time from surgery to the event of implant dislocation, and both log-rank and Wilcoxon test were used to preliminarily study the effect of BMI and smoking on the risk of implant dislocation. Cox proportional hazards regression model was used to test the null hypothesis of no effect of BMI and smoking status, while taking into account the simultaneous and independent effects of age at the time of surgery, calendar period, and fixation principle (use of cement or not). Parameter estimates and 95% confidence intervals (CIs) were obtained by maximizing the partial log-likelihood. We divided the follow-up period into 2 parts: 0–3 years and 3–8 years. All 2,106 patients were available for the first study period, which started at the day of admission to the hospital in order to undergo THR and continued until implant dislocation or censoring had occurred, or up to 3 years after surgery. 897 patients who did not develop implant dislocation or were not censored, were included in the second follow-up period, which lasted up to the end of the follow-up period. There were only 2 cases of implant dislocation during the second follow-up period. Thus, bivariable and multivari-able Cox analyses could only be performed for the first follow-up period.
When using log(-log(estimated survival function)) and more advanced statistical techniques (Lin et al. Citation1990) we did not find any evidence of interaction between patient-related risk factors and the time to implant dislocation for the first follow-up period. The procedure was based on the “st” commands in STATA 9.2 (Stata Statistical Software, College Station, TX).
Results
Baseline characteristics of the study cohort are shown in . 53 patients (2.5%) developed implant dislocation. In the obese group, 4% of patients developed implant dislocation as compared to 1.2% of those of normal weight. In the heaviest tobacco smoking group 3.3% of the patients developed implant dislocation, whereas 2.4% of never-smokers had implant dislocation ().
Time to an event of implant dislocation from 0 to 3 years after primary THR, by BMI and smoking status.
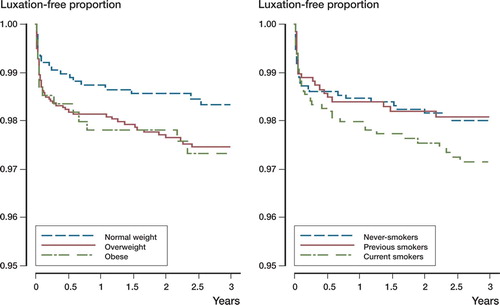
Table 1. Characteristics of 2,106 patients who underwent total hip replacement. Distribution of variables by survival status as of December 31, 2004
Age-adjusted hazard ratios for implant dislocation occurring from 0 to 3 years after primary THR were computed for BMI and tobacco-related variables (). When adjusted for age at time of surgery, overweight and obese patients had increased risk (HR = 2.4, 95% CI: 1.1–5.2 and HR = 3.6, 95% CI: 1.4–8.9, respectively) of implant dislocation compared to those of normal weight.
Table 2. Hazard ratios for implant dislocation from 0 to 3 years following primary THR, adjusted for age at time of surgery
When adjusted for age, calendar period, smoking status, and fixation principle, overweight and obesity remained to be significantly associated with an increased risk of implant dislocation compared to those of normal weight (HR = 2.5, 95% CI: 1.1–5.5; HR = 3.7, 95% CI: 1.5–9.3, respectively) (). In the same model, obese patients had 65% increased risk of dislocation (HR = 1.7, 95% CI: 0.84–3.2) compared to the overweight patients. However, this association was not statistically significant (p = 0.1). There was no significant association between overall smoking status or pack years of smoking and the risk of implant dislocation up to 3 years after the primary THR.
Table 3. BMI, smoking status and the risk of implant dislocation from 0 to 3 years following primary THR. Multi-variable proportional hazards model
Discussion
We found that high BMI was significantly associated with an increased risk of implant dislocation following primary THR. In a recently published study on patients undergoing hip revision arthroplasty, the risk of implant dislocation was 6 times higher in obese patients than in non-obese patients (Kim et al. Citation2006). These two results support the hypothesis that high BMI is an important risk factor for implant dislocation.
The increased risk of implant dislocation in overweight and obese patients may reflect a more complicated surgical procedure, where an excessive mass of adipose and muscle tissues in the hip region can make the surgical procedure more difficult and result in suboptimal orientation of the prosthetic components. In addition, the greater load on the hip prosthesis due to high BMI may increase the risk of implant dislocation.
Our study has some limitations. We did not have any information on the level of physical activity. High physical activity is a factor that could increase the risk of implant dislocation. In turn, high physical activity is inversely associated with being overweight (Borodulin et al. Citation2007). Thus, if there is confounding by such a risk factor, it would bias our results towards null. Furthermore, assessment of the history of alcohol abuse by reviewing the Swedish Inpatient Register did not provide us with any information on patients treated on an outpatient basis. Therefore, there might be some residual confounding by alcohol abuse in our analyses. On the other hand, alcohol abuse is a contraindication for planned total hip replacement. We believe that such residual confounding, although possible, would be quite small.
Using the Swedish Inpatient Register, we were unable to study the possible effect-modifying impact of different prosthesis-related or surgically-related factors such as cup size or surgical incision on the risk of implant dislocation. Furthermore, the effect of weight change since entry to the Construction Workers' Cohort and throughout the follow-up period could not be evaluated either. Consequently, we could not evaluate the possible misclassification introduced by this issue. However, previous studies have shown that obese patients do not generally lose weight following THR (Jain et al. Citation2003, Donavan et al. Citation2006). Therefore, we do not believe that such possible misclassification would influence our results in any appreciable way.
Almost 60% of patients who undergo primary THR are women (Herberts et al. Citation2005). Differences in risk behavior may differ between the sexes, and we have only studied male patients. However, it is unlikely that high BMI or tobacco smoking would affect the risk of implant dislocation differently in female patients.
To our knowledge, our study is the largest of its kind to investigate the effect of BMI on the risk of implant dislocation. The exposure data were collected prospectively, which reduced the possibility of information bias. We were also able to eliminate the possible confounding effect of different preop-erative diagnoses such as rheumatoid arthritis or hip fractures by excluding these factors from the study material.
In conclusion, high BMI is an important risk factor for implant dislocation after primary THR. The mechanism by which high BMI increases the risk of implact dislocation warrants further studies.
We wish to express our special thanks to the Olle Engkvist Byggmästare Foundation for a scholarship to OSA, which made this investigation possible. No benefits have been received or will be received from any commercial party, related directly or indirectly to the subject of this article.
Contributions of authors
OSA designed the study, analyzed the data, and drafted the paper. The analyses of data were supervised by RB. All coauthors participated in the analysis and interpretation of data, and contributed to subsequent drafts. RB is the guarantor.
- Borodulin K, Mäkinen T, Fogelholm M, Lahti-KoskI M, Prättälä R. Trends and socioeconomic differences in overweight among physically active and inactive Finns in 1978–2002. Prev Med 2007 Feb 15; [Epub ahead of print].
- Castillo R C, Bosse M J, MacKenzie E J, Petterson B M. LEAP Study Group. Impact of smoking on fracture healing and risk of complications in limb-threatening open tibia fractures. J Orthop Trauma 2005; 19: 151–7
- Donovan J, Dingwall I, McChesney S. Weight change 1 year following total knee or hip arthroplasty. ANZ J Surg 2006; 76: 222–5
- Engholm G, Englund A, Fletcher A C, Hallin N. Respiratory cancer incidence in Swedish construction workers exposed to man-made mineral fibres and asbestos. Ann OccupHyg 1987; 31: 663–75
- Hansson L E, Nyren O, Hsing A W, Bergstrom R, Josefs-son S, Chow W H, Fraumeni J F, Adami H-O. The risk of stomach cancer in patients with gastric or duodenal ulcer disease. N Engl J Med 1996; 335: 242–9
- Havelin L I, Engesaeter L B, Espehaug B, Furnes O, Lie S A, Vollset S E. The Norwegian Arthroplasty Register: 11 years and 73,000 arthroplasties. Acta Orthop Scand 2000; 71: 337–53
- Hedlundh U, Ahnfelt L, Fredin H. Incidence of dislocation after hip arthroplasty. Comparison of different registration methods in 408 cases. Acta Orthop Scand 1992; 63: 403–6
- Herberts P, Malchau H, Garellick G. Annual Report 2005. The Swedish National Hip Arthroplasty Register
- Jain S A, Roach R T. Travlos. Changes in body mass index following primary elective total hip arthroplasty. Correlation with outcome at 2 years. Acta Orthop Belg 2003; 69: 421–5
- Khatod M, Barber T, Paxton E, Namba R, Fithian D. An analysis of risk of hip dislocation with a contemporary total joint registry. Clin Orthop 2006, 447: 19–23
- Kim Y, Morshed S, Joseph T, Bozic K, Ries M. Clinical impact of obesity on stability following revision total hip arthroplasty. Clin Orthop 2006; 453: 142–6
- Lagerlund M, Bellocco R, Karlsson P, Tejler G, Lambe M. Socio-economic factors and breast cancer survival- a population-based cohort study (Sweden). Cancer Causes Control 2005; 16: 419–30
- Lin D Y, Wei L J, Zing Z. Checking the Cox model with cumulative sums of martingale-based residuals. Biomet-rica 1990; 80: 557–72
- Lindberg H O, Carlsson Å S, Gentz C-F, Pettersson H. Recurrent and non-recurrent dislocation following total hip arthroplasty. Acta Orthop Scand 1982; 53: 947–52
- Little C P, Burston B J, Hopkinson-Woolley J, Burge P. Failure of surgery for scaphoid non-union is associated with smoking. J Hand Surg (Br) 2006; 31B: 252–5
- McCollum D E, Gray W J. Dislocations after total hip arhtro-plasty. Clin Orthop 1990, 261: 159–70
- McLaughlin J R, Lee K R. The outcome of total hip replacement in obese and non-obese patients at 10- to 18-years. J Bone Joint Surg (Br) 2006; 88: 1286–92
- Moller A M, Pedersen T, Villebro N, Munkgaard A. Effect of smoking on early complications after elective orthopaedic surgery. J Bone Joint Surg (Br) 2003; 85: 178–81
- Morrey B F. Difficult complications after hip joint replacement. Dislocation. Clin Orthop 1997, 344: 179–87, Review
- Naessen T, Parker R, Persson I, Zack M, Adami H O. Time trends in incidence rates of first fracture in the Uppsala Health Care Region, Sweden, 1965–1983. Am J Epidemiol 1989; 130: 289–99
- Nilsson A C, Spetz C L, Carsjo K, Nightingale R, Smedby B. Reliability of the Hospital Registry. The diagnostic data are better than their reputation. Lakartidningen 1994; 598: 603–5
- Nyrén O, Bergström R, Nyström L, Engholm G, Ekbom A. Adami H-O et al. Smoking and colorectal cancer: a 20-year follow-up study of Swedish construction workers. J Natl Cancer Inst 1996; 88: 1302–7
- Sanchez-Sotelo J, Haidukewych G J, Boberg C J. Hospital cost of dislocation after primary total hip arthroplasty. J Bone Joint Surg (Am) 2006; 88: 290–4
- Szulc P, Garnero P, Claustrat B, Marchand F, Duboeuf F, Delmas P D. Increased bone resorption in moderate smokers with low body weight: the Minos study. J Clin Endocrinol Metab 2002; 87: 666–74
- W-Dahl A, Toksvig-Larsen S. Cigarette smoking delays bone healing: a prospective study of 200 patients operated on by the hemicallotasis technique. Acta Orthop Scand 2004; 75: 347–51
- Woolson S T, Rahimtoola Z O. Risk factors for dislocation during the first 3 months after primary total hip replacement. J Arthroplasty 1999; 14: 662–8
