Abstract
Background and purpose Fast-track surgery has been reported to improve rehabilitation outcome after major surgery, with length of hospitalization and muscle strength as outcome measures. We assessed the effect of optimization of perioperative care during admission on self-reported functional outcome, and compared patient status 6 months after THR with an age-matched healthy cohort.
Patients and methods 79 THR patients were randomized to optimized perioperative care (OPC) or conventional perioperative care (CPC). 61 patients fulfilled the requirements of the study protocol. Endpoint outcome was measured by SF-36 and WOMAC. To compare functional outcome in the THR group with that in healthy controls, we used data from a representative sample of 4,098 non-institutionalized Danish adults collected by the Danish National Institute of Public Health.
Results We found similar improvements in SF-36 and WOMAC scores for the OPC and CPC groups postoperatively, except for the total WOMAC score and the WOMAC subscore "function"—in which the CPC group did statistically significantly better. The OPC and CPS groups had similar score levels. 6 months after surgery, THR patients scored higher overall in the general health subscale and lower in three physical subscales of SF-36 compared to age-matched healthy controls.
Interpretation We found no evidence for the effect of optimization strategies during admission on self-reported functional outcome after THR. Although THR patients improved considerably after treatment, their physical status remained below the level of the healthy controls. Our results may indicate that the potential for functional improvement in THR patients is not fully realized, but this must be studied further.
Multimodal rehabilitation or fast-track surgery combine modern concepts of patient care with multimodal anesthetic and analgesic methods. It has been introduced to improve recovery, reduce hospitalization, and improve rehabilitation after surgery (Wilmore and Kehlet Citation2001, Henriksen et al. Citation2002, Kehlet and Wilmore Citation2002, Citation2005, Anderson et al. Citation2003, Gatt et al. Citation2005, Kehlet and Husted et al. Citation2006a, Citationb, Citationc, Petersen et al. Citation2006).
Preoperative education followed by postoperative home-based rehabilitation appears to be effective in reducing the length of stay and in improving function and quality of life after THR (Siggeirs-dottir et al. Citation2005). Whether perioperative enforced mobilization and nutrition during admission can affect postoperative self-reported functional outcome in late-phase rehabilitation after total hip replacement (THR) has, however, not yet been demonstrated in any controlled study.
We assessed the usefulness of optimization of perioperative care during admission on self-reported functional outcome after THR, and compared patients' self-reported functional status after 6 months with that of an age-matched healthy cohort.
Patients and methods
In this paper we present our findings from prolonged follow-up of a cohort defined by a previous randomized controlled trial (RCT) (Petersen et al. Citation2006). The study was approved by the local ethics committee and was carried out in accordance with the Helsinki Declaration.
Patients with osteoarthritis who were scheduled for elective primary unilateral THR and perioperative epidural analgesia were assessed for eligibility. Exclusion criteria were chronic opioid use, chronic pain syndrome, rheumatoid arthritis, fractures, and mental disorders.
Randomization was carried out on the day of admission by the use of sealed envelopes. Block randomization into blocks of 8 was used. The sequences were computer-generated.
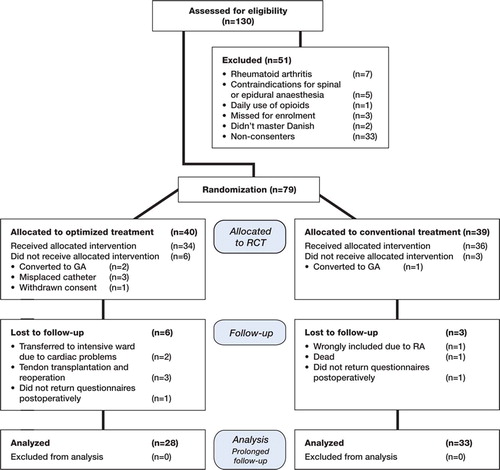
130 patients were identified as potential participants, 18 patients did not meet the inclusion criteria, and 33 declined to participate (). Thus, 79 patients were randomized to receive optimized perioperative care (OPC) or conventional perioperative care (CPC). 61 patients, 28 in the OPC group and 33 in the CPC group, constituted the study population of this prolonged follow-up study.
In order to compare the self-reported functional status of the THR patients with that of the healthy controls, we used data from a representative sample of 4,098 non-institutionalized Danish adults. These data were collected from February through August 1994 as a part of a population health survey carried out by the Danish National Institute of Public Health (Bjorner et al. Citation1997). All THR patients and healthy controls were classified into 6 age-matched groups.
All patients received standardized multimodal anesthesia and analgesia throughout the periopera-tive and postoperative period. The epidural catheter was removed after 48 h and Oxycontin (oxycodon hydrochloride) 10 mg twice a day and acetaminophen 1 g 4 times a day were given.
When the postoperative hemoglobin (HB) was < 5.5 mmol/L and if the patient had clinical symptoms (dizziness during mobilization), a blood transfusion was given.
All patients received physiotherapy for half an hour daily on weekdays. All of them were discharged with an exercise program for home training. No further rehabilitation was done. Patients were considered for discharge when sufficient pain relief had been achieved (estimated as a VAS score of < 3 cm while resting and < 5 cm during mobilization), and when the patient was able to maintain personal hygiene, to walk with sticks, and to climb stairs. Discharge was at the discretion of departmental surgeons.
The OPC group
The OPC group was given an optimized treatment regime involving pre- and postoperative strategies. Patient education was given the day before surgery by the investigators. The patients were introduced to standard plans for mobilization and energy intake. They were informed about the optimized treatment regime and the expectations they had in common were discussed. Transfer and walking techniques that would be required after surgery were trained. Devices to be used postoperatively were introduced and given to the patient.
Postoperatively, patients were encouraged to follow the written standard goals as follows. Mobilization was started on the first postoperative day. Scheduled time out of bed increased by 2 h a day, from 2 h on the day after surgery to 12 h on the sixth postoperative day. Furthermore, patients were asked to walk the length of the ward corridor (2 × 50 m) a scheduled number of times, increasing by 100 m a day from 100 m on the second postoperative day to 500 m on sixth postoperative day.
Eating and drinking despite lack of appetite was encouraged from the day of the operation. Registration and calculation of energy intake was performed on a daily basis. Supplementary energy intake: 200 mL of a protein-rich drink (Fortimel; Nutricia, Zoetermeer, the Netherlands) was served 3 times a day between the main meals.
The CPC group
The CPC group received none of the optimized measures listed. After surgery mobilization, oral fluid, and diet were introduced in a stepwise manner. The treating team responded to the wishes and condition of the patient in providing postoperative care, and no attempt was made to enforce mobilization or to encourage patients to eat and drink despite their lack of appetite.
To control the efficacy of the optimization strategies, all patients were asked to keep time records for leaving and returning to bed. Distance walked was measured using a marked area of the corridor in the ward, and all intake of nutrients was registered in a food record. Data were registered in a patient diary and patients were assessed by one of the researchers on a daily basis.
Process indicators
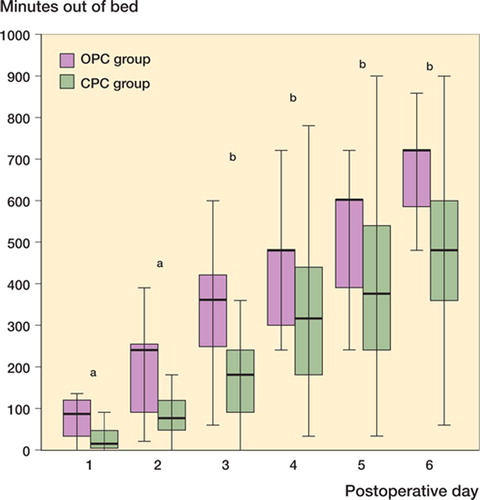
Analysis of the process indicators (mobilization and nutrition) showed that patients in the OPC group were mobilized to a far greater extent than patients in the CPC group (). The average total time out of bed was 37 h (SD 10) in the OPC group and 26 h (SD 14) in the CPC group (p < 0.001). The median total walking distance was 1,500 (255–4,050) m in OPC group and 1,200 (247–7,900) m in CPC group (p = 0.04). The average energy and protein intake in the OPC group was 103 kJ/kg (SD 26) and 1.25 g/kg (SD 0.35), respectively, as compared to 76 kJ/kg (SD 24) and 0.74 g/kg (SD 0.25) in the CPC group (p < 0.001).
Endpoint outcome
The 36-item Short Form Health Survey (SF-36) and the Western Ontario and McMaster University Osteoarthritis Index (WOMAC) were completed preoperatively, and 3 and 6 months postoperatively. Endpoint outcome measures were: changes in scores over time and changes in score level of the SF-36 and WOMAC variables.
The SF-36 is a generic, self-administered instrument for measuring different aspects of quality of life (Ware and Sherbourne Citation1992, Ware and Gandek Citation1998). The SF-36 scores range from 0 to 100, with a higher score indicating better health status.
The WOMAC is a disease-specific, self-administered instrument developed for the study of patients with osteoarthritis of the knee or hip (Bellamy Citation1997, Citation2002). It has a multidimensional scale comprising 24 items grouped into 3 dimensions: pain, stiffness, and physical function. We used the visual analog scale formats (WOMAC VA3 series) from 0–10 cm, where 0 represents no symptoms and 10 represents the worst possible symptoms.
Statistics
SF-36 and WOMAC variables are described by means or mean changes and 95% confidence intervals (CIs), and analyzed by a repeated measurements model. Changes over time (parallel curves) and score level (average over time) were compared between the OPC group and the CPC group, and tested for significant differences.
6 months postoperatively, scores of the SF-36 subscales "general health", "physical functioning", "role physical", and "physical component summary scale" for the THR patients were compared with matching scores for the healthy controls.
A weighted estimate of the differences between groups was calculated after stratification into 6 age groups using the weights (1/SEE2), where SEE is the standard error of the estimate within a particular age group. The significance level was p = 0.05. We used SPSS software version 11.0 for Windows.
Results
61 patients completed the study (, ). No significant differences in change of score were seen between groups, except for the total WOMAC score and the WOMAC subscale "function", where the CPC group had a higher change in score (p = 0.03 for both comparisons) (). The changes over time were all significant (all p-values were < 0.001 except for two (0.007 and 0.009)), and there were no significant difference between the OPC group and the CPC group regarding level.
Table 1. Overall comparison of demographics and perioperative data for the study population
Table 2. Changes in WOMAC and SF 36 scores between baseline and follow-up 3 and 6 months postoperatively. Differences in changes over time baseline and 3 months; baseline and 6 months between groups were analyzed and tested for statistically significant differences by a repeated measurements model
WOMAC showed a minor ceiling effect 3 and 6 months postoperatively in all domains, and SF-36 showed both floor and ceiling effects preoperatively, and also 3 and 6 months postoperatively ().
Table 3. Psychometric properties of WOMAC and SF-36 at baseline and at follow-up 3 and 6 months postopera-tively, showing the number of patients with the lowest score (floor effect) and the number of patients with the highest score (ceiling effect). Study population was 61 patients
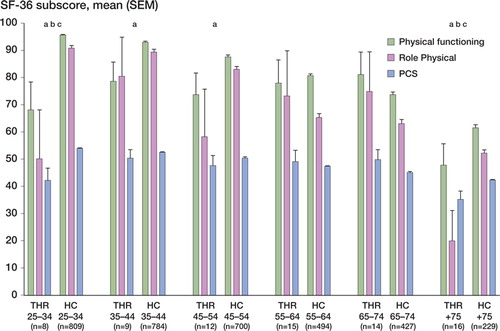
A comparison of the stratified and weighted scores of the SF-36 subscales "general health" (GH), "physical functioning" (PF), "role physical" (RP), and "physical component summary" (PCS) between THR patients and healthy controls showed that the THR patients had an overall higher score in the subscale GH (95% CI: 0.1–1, p = 0.05) than the healthy controls, but a lower score in all three physical subscales (PF, RP, and PCS) (95% CI: 4.0–13, p ≤ 001; 95% CI: 3.3–27, p = 0.01; and 95% CI: 0.1–5.8, p = 0.05, respectively).
The differences in scores were more distinct among the younger and the older age groups, especially in relation to the variables RP and PCS
Discussion
In this follow-up study investigating the usefulness of two different perioperative treatment regimes after THR on self-reported functional outcome 3 and 6 months postoperatively, we found that there were no significant differences between groups except for the total WOMAC result and the WOMAC subscale "function". This result could be a coincidence caused by multiple testing (p-values were close to 0.05), but generally speaking the CPC group did better postoperatively than the OPC group. We have no clear explanation for this finding, but as the OPC group was hospitalized for a significantly shorter time than the CPC group (Petersen et al. Citation2006), we cannot eliminate the possibility that length of stay was a confounding factor.
Another explanation for the poor result of our intervention compared to that of others (Siggeirsdottir et al. Citation2005) may be that the intervention was only carried out during hospitalization. In the study by Siggeirsdottir et al., intervention was continued after discharge by offering home visits during the first 2 weeks after discharge, in order to ensure that the rehabilitation course was being followed after hospitalization. As a result of our study design, we do not know whether patients in the OPC group continued the recommended regimes after discharge.
Another weakness of our study was the lack of blinding. Both caretakers and patients knew which treatment patients were receiving, and this could have introduced bias regarding a general increase in mobilization and energy intake in the CPC group—and thereby an underestimation of the efficacy of the optimization strategies. Yet another weakness was that we did not assess patients' biochemistry, body composition, or muscle strength in order to be able to compare our results with those of other studies (Henriksen et al. Citation2002, Gatt et al. Citation2005).
The SF-36 showed a more conspicuous ceiling effect postoperatively than the WOMAC. Validity and responsiveness are the most important criteria when deciding which particular instrument to use in a clinical trial (Bellamy et al. Citation1997). Although generic instruments are useful in providing comprehensive health ratings that can be used with various disorders, they may be inferior to disease-specific instruments in their responsiveness in relation to intervention studies where measurements are repeated. The lack of responsiveness may be caused by a ceiling effect, which means that improvements cannot be detected in patients with a maximum score at baseline.
In accordance with other studies (Angst et al. Citation2001, Bachmeier et al. Citation2001, Patt and Mauerhan Citation2005, Quintana et al. Citation2005), we found that the illness-specific instrument (WOMAC) was more responsive to changes over time than the generic instrument (SF-36).
The functional outcome after 3 months in the THR group was in accordance with the results of other studies with a longer follow-up period (Bachmeier et al. Citation2001, Juul et al. Citation2006, Quintana et al. Citation2005). This indicates that the main improvements after THR are seen rather early in late-phase rehabilitation.
Although the THR patients generally achieved a higher score in the subscale "general health" than the controls after 6 months, their overall scores in the 3 physical subscales were lower. Our results may indicate that the potential for improvement in function for THR patients is not fully realized, but this must be studied further. The difference was more conspicuous in the young and the old age groups, which seems important when the need for a course of postoperative rehabilitation is considered because the young THR patients are expected to return to full working capacity and ideally the old patients should stay out of domiciliary care.
Figure 3. Scores of THR patients and healthy controls in the SF-36 subscales physical functioning (PF), role physical (RP), and physical component summary scale (PCS) broken down according to patient age (age groups according to Bjorner et al. (Citation1997)). Scores are presented as mean an SEM. Statistically significant differences in mean scores between patients and controls are shown as follows: a = PF: p < 0.05; b = RP: p < 0.05; c = PCS: p < 0.05.
No competing interests declared.
Contributions of authors
MP participated in the entire planning process and execution of the study, data collection, statistical analysis, and preparation of the manuscript. NA participated in the planning process and in the statistical analysis and preparation of the manuscript. KS performed many of the THRs and participated in the entire process, especially in preparation of the manuscript.
This project was supported by grants from "Forskningsini-tiativet Århus Amt" and the Society of Danish Physiotherapists.
- Anderson A D G, MC Naught C E, MacFie J, Tring I, Baker P, Mitchell C J. Randomized clinical trial of multimodal optimization and standard perioperative surgical care. Br J Surg 2003; 90: 1497–504
- Angst F, Aeschlimann A, Steiner W, Stucki G. Responsiveness of the WOMAC osteoarthritis index as compared with the SF-36 in patients with osteoarthritis of the legs undergoing a comprehensive rehabilitation intervention. Ann Rheum Dis 2001; 60: 834–40
- Bachmeier C J, March L M, Cross M J, Lapsley H M, Tribe K L, Courtenay B G, Brooks P M. A comparison of outcomes in osteoarthritis patients undergoing total hip and knee replacement surgery. Osteoarthritis Cartilage 2001; 9: 137–46
- Bellamy N. Osteoarthritis clinical trials: candidate variables and clinimetric properties. J Rheumatol 1997; 24: 768–78
- Bellamy N. WOMAC: a 20-year experiential review of a patient-centered self-reported health status questionnaire. J Rheumatol 2002; 29: 2473–6
- Bellamy N, Kirwan J, Boers M, Brooks P, Strand V, Tugwell P, Altman R, Brandt K, Dougados M, Lequesne M. Recommendations for a core set of outcome measures for future phase III clinical trials in knee, hip, and hand osteoarthritis. Consensus development at OMERACT III. J Rheumatol 1997; 24: 799–802
- Bjorner J B, Damsgaard M T, Watt T, Bech P, Rasmussen N K, Kristensen T S, et al. Danish Manual for the SF-36. Læmiddelindustriforeningen. LIF, Copenhagen 1997
- Gatt M, Anderson A D G, Reddy B S, Hayward–Sampson P, Tring I C, MacFie J. Randomised clinical trial of multi-modal optimization of surgical care in patients undergoing major colonic resection. Br J Surg 2005; 92: 1354–62
- Henriksen M G, Jensen M B, Hansen H V, Jespersen T W, Hessov I. Enforced mobilization, early oral feeding, and balanced analgesia improve convalescence after colorectal surgery. Nutrition 2002; 18: 147–52
- Husted H, Hansen H C, Holm G, Bach–Dal C, Rud K, Andersen K L, Kehlet H. Accelerated versus conventional hospital stay in total hip and knee arthroplasty II: organizational and clinical differences. Ugeskr Laeger 2006a; 168: 2144–8
- Husted H, Hansen H C, Holm G, Bach–Dal C, Rud K, Andersen K L, Kehlet H. Accelerated versus conventional hospital stay in total hip and knee arthroplasty III: patient satisfaction. Ugeskr Laeger 2006b; 168: 2148–51
- Husted H, Hansen H C, Holm G, Bach–Dal C, Rud K, Andersen K L, Kehlet H. Length of stay in total hip and knee arthroplasty in Danmark I: volume, morbidity, mortality and resource utilization. A national survey in orthopaedic departments in Denmark. Ugeskr Laeger 2006c; 168: 2139–43
- Juul O, Sigmundsson F G, Ovesen O, Andersen M O, Ernst C, Thomsen K. No difference in health-related quality of life in hip osteoarthritis compared to degenerative lumbar instability at pre- and 1-year postoperatively: a prospective study of 101 patients. Acta Orthop 2006; 77: 748–54
- Kehlet H, Wilmore D W. Multimodal strategies to improve surgical outcome. Am J Surg 2002; 183: 630–41
- Kehlet H, Wilmore D W. Fast-track surgery. Br J Surg 2005; 92: 3–4
- Patt J C, Mauerhan D R. Outcomes research in total joint replacement: a critical review and commentary. Am J Orthop 2005; 34: 167–72
- Petersen M K, Madsen C, Andersen N T, Soballe K. Efficacy of multimodal optimization of mobilization and nutrition in patients undergoing hip replacement: a randomized clinical trial. Acta Anaesthesiol Scand 2006; 50: 712–7
- Quintana J M, Escobar A, Bilbao A, Arostegui I, Lafuente I, Vidaurreta I. Responsiveness and clinically important differences for the WOMAC and SF-36 after hip joint replacement. Osteoarthritis Cartilage 2005; 13: 1076–83
- Siggeirsdottir K, Olafsson O, Jonsson H, Iwarsson S, Gudnason V, Jonsson B Y. Short hospital stay augmented with education and home-based rehabilitation improves function and quality of life after hip replacement: randomized study of 50 patients with 6 months of follow-up. Acta Orthop 2005; 76: 555–62
- Ware J E, Jr, Gandek B. Overview of the SF-36 Health Survey and the International Quality of Life Assessment (IQOLA) Project. J Clin Epidemiol 1998; 51: 903–12
- Ware J E, Jr., Sherbourne C D. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 1992; 30: 473–83
- Wilmore D W, Kehlet H. Management of patients in fast track surgery. BMJ 2001; 322: 473–6