Abstract
Background and purpose Proximal bone loss due to stress-shielding is a matter of concern after uncemented femoral hip revision. We have used short, proximally hydroxyapatite-coated prostheses in revision since 1989, and we now report the results.
Methods 60 patients (62 hips) were revised because of aseptic loosening. Bone defects prior to revision were mostly of type II according to the Gustilo-Pasternak and Endo-Klinik classifications. Follow-up time was 73 (24–161) months. 9 patients had died before follow-up; 8 of these still had the stem in place. Clinical assessment was performed with the Harris hip score. Radiographs were evaluated for bone defects at revision, postoperative stem fixation, and periprosthetic bone remodeling.
Results Mean Harris hip score was 75 (30–100) points. There was no stem loosening or progressive subsidence. 8 patients had mild to moderate thigh pain. Osteolysis, present at revision, had diminished, partially or completely, in four-fifths of the hips at follow-up. 4 hips had required re-revision due to fracture or dislocation. The 6-year prosthesis survival rate was 95% (95% CI: 0.83–0.98).
Interpretation Uncemented revision with a short, proximally hydroxyapatite-coated prosthesis is a reliable procedure with encouraging results in the medium term if bone defects at revision are moderate.
Cemented revision for prosthetic loosening after cemented total hip arthroplasty (THA) has shown an unacceptably high failure rate (Dohmae et al. Citation1988, Eisler et al. Citation2000, Haydon et al. Citation2004). This method might be chosen in the elderly patient with low demands regarding activity. In active patients with a poor bone stock, hip revision with cement and impacted morselized allograft bone has shown good long-term results (Gie et al. Citation1993, Ornstein et al. Citation2002, Ullmark et al. Citation2002, Halliday et al. Citation2003). Uncemented hip revision after aseptic loosening has been promising in the short to medium term (Bohm and Bischel Citation2001, Moreland and Moreno Citation2001, Trikha et al. Citation2005) and also in the long term (Wagner Citation1987, Paprosky et al. Citation1999, Raman et al. Citation2005, Reikerås and Gunderson Citation2006). Most stems used in these studies are long-stemmed, extensively coated, or distally anchored. A disadvantage with these stems is the transfer of excessive load distally, leading to diminished proximal bone stock. Stress-shielding could lead to an increased risk of periprosthetic fractures and even stem loosening (Engh et al. Citation1987, Huiskes Citation1990). Several studies of proximally coated uncemented stems in hip revision have shown a high incidence of failure due to aseptic loosening or fracture (Berry et al. Citation1995, Malkani et al. Citation1996, Mulliken et al. Citation1996). The reason for this is insufficient fixation of the implant in the proximal metaphysis due to poor bone stock. However, Kelly et al. (Citation2006) reported good results with a proximally coated stem in hip revision. We have used a similar stem and now report our results.
Patients and methods
Patients
All patients who had been reoperated at the Orthopedic Department of Danderyd Hospital with the proximally porous- and HA-coated tapered Bi-Metric stem between 1989 and 2002 due to aseptic loosening were included in the study. We used this prosthesis for revision in younger patients and in elderly patients who had a good bone stock. 62 hips in 60 patients were reoperated (). The index diagnoses were primary osteoarthritis (44 hips), fractures and related complications (9 hips), inflammatory arthritis (5 hips), and developmental dysplasia (4 hips). The mean time between the first hip arthroplasty and the revision was 7 (1–19) years. 41 of the hips had been operated only once in the same hip before revision. Mean follow-up time was 6 (2–13) years. At follow-up, 9 of the 60 patients had died. 1 of these had been re-revised 3 months after the uncemented stem revision due to a fracture adjacent to a peroperative fenestration. The other 8 patients still had their stem in place. No stem-related problems were found in these patients. 1 patient had only attended the radiographic part of the study.
Implant
The patients were reoperated with the Bi-Metric femoral stem (Biomet Inc., Warsaw, IN, USA). This is a collarless, tapered stem (3°) made of titanium alloy, where the proximal 30% of the stem has a porous-coated (100–200 μm) surface with plasma-sprayed HA (thickness 40–70 μm, crystallinity 50–70%, purity > 95%). The distal 70% has a textured surface. The femoral component is available in 13 proportional sizes and has a modular head of cobalt chrome. Only 1 offset option was available.
Surgery
All operations were performed using a posterior approach. 53 of the 62 revised stems were cemented and 9 were uncemented; 1 of these was a hemiarthroplasty. Bone grafting around the neck of the stem was carried out simultaneously in 33 of the cases. In 24 of the operations, only the stem was revised. At follow-up, 39 of the patients had a cemented polyethylene cup and 21 patients an uncemented cup. The patients were mobilized on the day after the revision under the supervision of a physiotherapist. Postoperative weight bearing was individualized according to the preferences of the surgeon.
Clinical evaluation
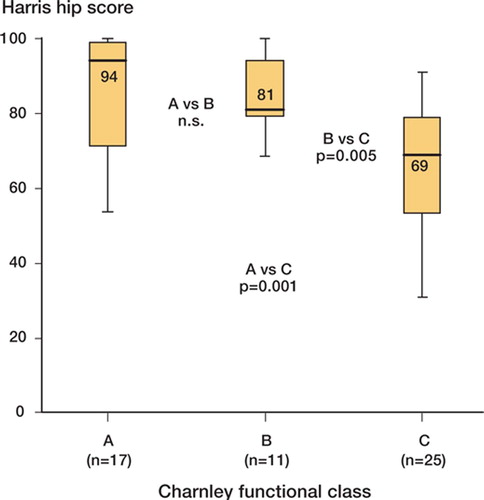
We evaluated the patients clinically with an interview and physical examination performed by one of the authors (MS) who had not been involved in the operations. We categorized the patients according to Charnley's clinical classification (Charnley Citation1972). At follow-up, 26 patients were classified as belonging to class C, i.e. they had disabilities other than the hip that interfered with their functional capacity ().
Table 1. Demographic data for the patients
Clinical outcome was assessed with the Harris hip score (HHS) and with questions concerning mid-thigh pain. The mid-thigh pain was graded by the patient as mild, moderate, or severe.
Radiographic evaluation
Standardized anterioposterior and lateral radiographs after the index operation were compared with radiographs taken before and immediately after the revision, and with radiographs taken at the time of survey. A coefficient—the ratio of the actual diameter and the measured diameter of the femoral head—was calculated for each radiograph and was used to adjust all measurements for magnification.
We analyzed the radiographs in order to address 3 particular issues. Firstly, we classified bone defects prior to revision surgery. Secondly, we determined the degree of fixation of the stem, and thirdly, the amount of the periprosthetic bone remodeling. We classified bone defects according to the classifications of Gustilo and Pasternak (Citation1988) and Endo-Klinik (Engelbrecht and Siegel Citation1989). Stem fixation was assessed using the criteria of Engh's fixation/stability score (FSS) for uncemented femoral implants (Engh et al. Citation1990): absence/appearance of endosteal bone bridges (spot welds), absence/appearance of reactive lines in the coated region of the stem, absence/appearance of reactive lines in the uncoated region, pedestal formation, calcar modeling, and interface deterioration (widening radiolucent lines). Migration of the femoral implant was defined as a change in the vertical distance between the easily identified inferior border of the coating to the most medial point of the lesser trochanter or as any change in alignment or rotation. The subsidence was considered definite if the change was more than 4 mm (Malchau et al. Citation1995).
Figure 1. Box plot of Harris hip score (53 hips) in the different Charnley classes. (HHS; median, quartile and extreme
We also assessed presence of focal osteolysis (scalloping) with defined borders and distal cortical hypertrophy, defined as new enlargement of the external femoral diameter around the distal part of the prosthesis, compared to the radiographs taken immediately postoperatively. We recorded the radiographic changes according to Gruen zones on the anterioposterior radiographs. Heterotopic ossification was recorded using the grading system of Brookeretal. (1973).
According to the Ethics Board of Karolinska Institutet, no permission was required for this study (04-453/3). The investigation was approved by the committee for protection against radiation at Danderyd Hospital (2003-3).
Table 2. Femoral bone defects at revision (53 hips)
Statistics
We used the Mann-Whitney U test for non-parametric variables (independent groups) to assess the association between HHS and Charnley's clinical classification. The statistical analyses were performed with the statistical package JMP 6.0 (SAS Institute, Cary, NC). The results were considered significant at p-values of < 0.05.
Results
Clinical results
Between the femoral revision operation and the follow-up, 5 patients had undergone a cup revision. At follow-up, the mean HHS score was 75 (30–100) points. 23 of the patients had a good or excellent result with an HHS of > 79 points, 18 patients had a poor outcome (HHS of < 70 points). We noted a lower HHS for patients in Charnley's class C compared to patients in class A (p < 0.001) and B (p < 0.005) (). We found no difference in HHS between patients with different types of bone defects at revision. 4 patients complained of mild thigh pain and 4 other patients of moderate pain. None of the patients suffered from severe thigh pain. 28 patients used no support for walking and 28 patients had no limp at all.
Radiographic results
Bone defects were mostly of type II in both classifications, and no type IV defect was observed (). We saw no stem loosening. All stems showed several signs of rigid fixation. In 30 hips, endosteal bone bridges (spot welds) were noted and there was a total absence of reactive lines in 37 hips (). In 44 hips, initial lucencies had been obliterated—either partially or completely—with new bone formation at follow-up (). 5 stems had subsided by more than 4 mm at follow-up; all showed other signs of stability. The maximum subsidence was 8 mm. None of the stems migrated into varus, valgus, or rotated. In 2 hips, new formation of focal osteolysis was detected in Gruen zone 1. Several additional signs of remodeling were observed; these are listed in .
Complications
9/62 hips had dislocations; 7 of these had only 1 dislocation and 2 had recurrent dislocations. Of the 2 latter patients, 1 was successfully treated with exchange of liner and a larger size of head. The other has cerebral paresis and has not been reoperated. We had 4 peroperative fissures during stem insertion. 3 were noted at operation and were treated with partial weight bearing, and 2 of them also with cerclage wires. The fourth patient, who got a fissure in the lesser trochanter peroperatively, suffered from pain and subluxations. The stem subsided and he was re-revised using impacted morselized bone allograft and a cemented stem. 4 fractures were seen postoperatively. 2 of these were fissures without loosening of the stem. They were treated nonoperatively. 1 patient sustained a fracture, just after being operated, through a fenestration done at the revision operation. He was re-revised using a longer stem. The fourth patient fell on his hip 2 years after the revision and then complained of pain and subluxation phenomenon. During the revision that followed, we noted that the stem had subsided and rotated in retroversion—and had subsequently been osseointegrated again. In all, 4 hips have been re-revised on the femoral side. The 6-year prosthesis survival rate was 95% (95% CI: 0.83–0.98).
2 patients had a postoperative wound infection and 1 patient got a deep infection in the hip. 1 patient developed a clinically apparent deep vein thrombosis. 1 patient suffered from a sciatic nerve injury with partial loss of skin sensibility but no loss of motor function. No case of pulmonary embolus or vascular complication was seen.
Figure 3. Remodeling changes around the stem. Arrows indicate spot welds (A), pedestal formation (B), and distal cortical hypertrophy (C).
Table 3. Bone remodeling at follow-up (53 hips)
Discussion
The frequency of loosening after revision with second-generation cementing technique is 15—20% at 10 years of follow-up, and third-generation cementing technique has not improved these results (Eisler et al. Citation2000). One cause of the high incidence of mechanical failure after cemented revision may be the lack of endosteal cancellous bone in the femur. This leads to a decrease in shear strength between the cement and the bone, due to inferior cement-bone micro-interlock (Dohmae et al. Citation1988, Berry Citation1998). If bone stock is poor, or if endosteal cancellous bone is lacking, other surgical methods are said to give better results. Impaction bone grafting with morselized allograft bone and cementation of the stem have been used in femoral revision arthroplasty. This technique has obvious advantages in bone stock restitution. Several authors have reported good or excellent results (Ullmark et al. Citation2002, Halliday et al. Citation2003, Mahoney et al. Citation2005). However, impaction bone grafting surgery is technically demanding and time consuming. There are well-known complications associated with this technique, such as major subsidence and per- and postoperative fractures (Eldridge et al. Citation1997, Pekkarinen et al. Citation2000, van Biezen et al. Citation2000, Ornstein et al. Citation2002).
Another alternative in femoral revision is the use of uncemented implants. The aim of using these components is to achieve biological fixation, i.e. ingrowth of endosteal bone by new bone formation within the porous surface structure of the implant (Turner et al. Citation1986, Engh et al. Citation1987, Engh and Bobyn Citation1988, Rosenberg Citation1989). In a revision situation, proximal bone stock in the femur is often compromised. To achieve early postoperative stability, most uncemented stems are designed to bypass the proximally damaged zone and to achieve initial stability from press-fit distally. Distally anchored stems have shown good clinical results in the short- to medium-term (Wagner Citation1987, Kolstad et al. Citation1996, Isacson et al. Citation2000, Bohm and Bischel Citation2001). These long stems have the disadvantage of inducing severe stress-shielding, thus causing further bone loss proximally. Removal of such a stem would be more technically demanding and the outcome is likely to be worse thereafter. In an attempt to achieve sufficient initial stability with shorter stems, extensively porous-coated or HA-coated, canal-filling cobalt-chrome or titanium alloy stems have been used with good or excellent results (Lawrence et al. Citation1994, Paprosky et al. Citation1999, Moreland and Moreno Citation2001, Crawford et al. Citation2004, Raman et al. Citation2005, Trikha et al. Citation2005, Reikerås and Gunderson Citation2006). At least initially, the biological fixation is probably most pronounced in the distal part of the stem because the contact between the stem surface and the host bone is more intimate in this region, and the surrounding bone stock is of better quality distally than in the compromised proximal bone. Extensively coated stems get fixated both proximally and distally.
Stress-shielding is still of some concern to varying degrees. Reikerås and Gunderson (Citation2006) concluded that they had no stress transfer in the distal direction because they had a low amount of proximal bone loss and a low incidence of distal cortical hypertrophy. In other studies with extensively coated stems, there were signs of stress-shielding (Paprosky et al. Citation1999, Moreland and Moreno Citation2001). These divergent results may have been caused by different stem designs. The stem used in the study by Reikerås and Gunderson (Citation2006) is of tapered titanium alloy with a narrow tip. Cylindrical stems probably cause more load transfer distally than tapered stems do, and titanium alloy stems are less stiff than cobalt-chrome stems—which might contribute to the degree of stress-shielding. Theoretically, stress-shielding could increase the risk of periprosthetic fractures, avulsions of muscle insertions in the trochanteric region, and even the risk of stem loosening. These theoretical problems have not been seen clinically yet, but the follow-up time may not be long enough.
In an attempt to reduce stress-shielding, stems with only proximal coating have been used. Depending on the length, shape, and surface of the stem, they are more or less likely to get fixated distally also. According to this, it would be difficult to strictly categorize these implants into a uniform group. The aim, though, of using any of these components is to enhance the proximal fixation in order to prevent further bone loss proximally and to minimize the load transfer distally. Earlier studies with stems aimed at proximal fixation have not shown entirely promising results ().
Our report deals with the results of using a proximally porous- and hydroxyapatite-coated uncemented tapered stem in femoral revisions because of aseptic loosening. We have used this stem in cases when it was judged that the bone stock at revision could give initial rigid stability to the implant. This seems to be a key factor in achieving good results in hip revisions using uncemented stems.
We chose to use 2 classification systems to determine bone defects prior to revision. The systems differ in their sensitivity in classification of bone defects. The classification from Endo-Klinik (Engelbrecht and Siegel Citation1989) is more sensitive to small bone defects. If the initial stem has subsided, it is referred to as a type II defect. That is not the case in the Gustilo and Pasternak (Citation1988) classification, where there is also a large step between a type II and a type III defect. To be considered as a type II defect, there must be a large defect involving the lesser trochanter and the posterior-medial wall of the proximal femur. We had very few such extensive bone defects in our series which contributed to the excellent radiographic outcome. As a consequence of the small bone defects, we were able to achieve initial stability of almost all implants—and 100% well-fixated stems at follow-up. We could not see any difference in clinical result associated with the bone defects. This is probably due to the fact that there was rigid fixation of all stems in our study and—as compared to other materials—the great proportion of patients were in Charnley's functional class C, thus contributing to a lower HHS than would have been the case if it were only the operated hip that interfered with their functional capacity.
Table 4. Studies on uncemented femoral revisions with proximally coated stems
The clinical result, with a mean HHS of 75 points, is of the same order as in other studies of uncemented femoral revision using stems aimed at proximal fixation (Malkani et al. Citation1996, Mulliken et al. Citation1996). These studies concluded that the overall results, clinically and radiographically, were suboptimal. During the follow-up in our study, we found that the patients were satisfied with their reoperated hip but almost half of them had other disabilities impairing their functional capacity, for example inflammatory arthritis, knee osteoarthritis, or spinal stenosis (). We believe that this is the reason for us not finding a higher HHS. 8 of 62 hips had mild-to-moderate thigh pain and no patients suffered from severe thigh pain. This compares favorably with other studies (Moreland and Moreno Citation2001, Raman et al. Citation2005, Trikha et al. Citation2005). Radiographically, several patients showed signs of load transfer distally, which suggests a possible reason for their mid-thigh pain. The fact that few of the patients suffered from pain was probably due to the rigid fixation of the stem. Although the pain parameter is referred to in many studies concerning uncemented stems, we consider that this parameter is difficult to evaluate because of its low specificity.
Compared to other studies, we had a larger proportion of stem subsidence (19/53 hips). Although some of the stems had subsided when we compared the radiographs taken immediately after revision with the radiographs taken at follow-up, they all had several radiographic signs of stable fixation. It is possible that a proximally-coated, tapered stem is more likely to subside initially in the smooth femoral canal with lack of cancellous bone than a cylindrical, extensively coated implant. We saw no continuous subsidence or progressive radiolucent lines in the coated region of the stems. The radiolucent lines adjacent to the stems on the radiographs taken immediately after revision had been filled out with new bone in four-fifths of the hips at follow-up (). Spot welds were seen in half of the hips, and they were usually distributed in Gruen's zones 1 and 7, i.e. in the coated region of the stem (). In primary arthroplasty, using the same prosthesis, the incidence of spot welds is higher (Bodén et al. Citation2006). The reason for this may be that the endocortex in the proximal femur is smooth with less trabecular bone in a revision situation. In addition to this, as a result of earlier surgery, the femoral bone is altered—leading to unspecific skeletal findings on the radiographs. These signs, in combination with proximal osteopenia (), sometimes made the evaluation regarding osteolysis and spot welds difficult.
Figure 4. Remodeling changes around the stem. Arrows indicate proximal osteopenia (A), distal cortical hypertrophy (B), and pedestal formation (C).
This stem is designed to be osseointegrated in the proximal part of the femur, thus aiming at load transfer proximally and preventing from further bone loss in this region. However, our radio-graphic data revealed that this is not the case. The stem becomes osseointegrated both proximally and distally. We saw several signs of stress-shielding—such as calcar resorption, proximal cortical thinning, proximal osteopenia, and distal cortical hypertrophy—of varying degrees (– ). The larger stems used in femoral revision are stiffer than the stems used in primary arthroplasty, and patients in need of femoral revision have lower femoral bone density than patients in need of a primary hip arthroplasty. Both of these factors will contribute to a more pronounced stress-shielding after femoral revision than after a primary arthroplasty. It is important to mention that both the sensitivity and the specificity of evaluating bone loss radiographically are low. On plain radiographs, bone loss is not detected until about one-third of the bone is lost and the loss is not reproducibly recognized until two-thirds of the bone is resorbed (Engh et al. Citation2000); thus, it is sometimes difficult to differentiate whether bone remodeling seen in the femur is due to osteopenia or to osteolysis.
We had 2 cases with proximal focal osteolysis. Several hips showed signs of proximal osteopenia. Even though the stem is designed to prevent unloading of the proximal part of the femur, we found no other explanation for the proximal osteopenia than that the stems also get a distal fixation in the diaphysis, contributing to partial unloading of the proximal part of the femur.
During the revision operation, after insertion of the uncemented stem, we often noted a non-circumferential space between the proximal body of the stem and the surrounding bone. We did not always fill this space with impacted bone chips. Despite the presence of this gap, we found no distal osteolysis at follow-up. A possible explanation for this is that the HA coating has sealed off the interface between the bone and the implant, thus preventing migration of debris into the peri-implant space (Rahbek et al. Citation2005). HA was introduced to enhance the osteoconductive properties of uncemented hip implants (Geesink et al. Citation1987). It has been found that supplementary HA also has osteogenetic capacity (Furlong and Osborn Citation1991). Within the gap between host bone and implant, bone formation is induced not only from the side of the host bone but also from the side of the HA-coated implant, enabling bone to bridge over wider gaps and to do so more rapidly than without the use of HA.
Dislocation was the most common complication in our series (9 of 62 hips). This is higher than in other studies. We believe that this was caused by our use of 22- to 29-mm head size (except in 3 cases in which the head diameter was 32 mm), and that we only had 1 offset option available at that time. We had 4 peroperative fractures during stem insertion and also noted 4 postoperative fractures. These figures are lower than what other groups have reported (Malkani et al. Citation1996, Mulliken et al. Citation1996).
One strength of our study is that we were able to re-examine all patients. The weaknesses are the retrospective design and the fact that we did not have recordings of HHS prior to revision.
No competing interests declared.
Contributions of authors
MS examined all patients, collected the data, analyzed the radiographs, and prepared the manuscript. OS contributed with manuscript preparation, some statistical analyses, and examination of several patients. HB and TA scrutinized the radiographs and revised the manuscript. PA designed the study, supervised the statistical analyses, and proofread the manuscript.
- Berry D J, Harmsen W S, Ilstrup D, Lewallen D G, Cabanela M E. Survivorship of uncemented proximally porous-coated femoral components. Clin Orthop 1995, 319: 168–77
- Berry D J. Cemented femoral revision. In: Hip surgery: materials and developments, L Sedel, M E Cabanela. Martin Duniz, London 1998; 287
- Bodén H, Salemyr M, Sköldenberg O, Ahl T, Adolphson P. Total hip arthroplasty with an uncemented hydroxyapa-tite-coated tapered titanium stem. Excellent results at a minimum of 10-years follow-up in 104 hips. J Orthop Sci 2006; 11(2)175–9
- Bohm P, Bischel O. Femoral revision with the Wagner SL revision stem. Evaluation of one hundred and twenty-nine revisions followed for a mean of 4.8 years. J Bone Joint Surg (Am) 2001; 83(7)1023–31
- Brooker A F, Bowerman J W, Robinson R A, Riley L H, Jr. Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg (Am) 1973; 55(8)1629–32
- Charnley J. The long-term results of low-friction arthroplasty of the hip performed as a primary intervention. J Bone Joint Surg (Br) 1972; 54(1)61–76
- Crawford C H, Malkani A L, Incavo S I, Morris H B, Krupp R J, Baker D. Femoral component revision using an extensively hydroxyapatite-coated stem. J Arthroplasty 2004; 19(1)8–13
- Dohmae Y D, Bechtold J E, Sherman R E, Puno R M, Gustilo R B. Reduction in cement-bone interface shear strength between primary and revision arthroplasty. Clin Orthop 1988, 236: 214–20
- Eisler T, Svensson O, Iyer V, Wejkner B, Schmalholz A, Larsson H, Elmstedt E. Revision total hip arthroplasty using third-generation cementing technique. J Arthroplasty 2000; 15(8)974–81
- Eldridge J D, Smith E J, Hubble M J, Whitehouse S L, Learmonth I D. Massive early subsidence following femoral impaction grafting. J Arthroplasty 1997; 12(5)535–40
- Emerson R H, Jr, Head W C, Higgins L L. Clinical and radio-graphic analysis of the Mallory-Head femoral component in revision total hip arthroplasty. A minimum 8.8-year and average eleven-year follow-up study. J Bone Joint Surg (Am) 2003; 85(10)1921–6
- Engelbrecht E, Siegel A. Endo-Klinik klassifikation. Radio-loge 1989; 29(10)508–18
- Engh C A, Bobyn J D. The influence of stem size and extent of porous coating on femoral bone resorption after primary cementless hip arthroplasty. Clin Orthop 1988, 231: 7–28
- Engh C A, Bobyn J D, Glassman A H. Porous-coated hip replacement. The factors governing bone ingrowth, stress shielding, and clinical results. J Bone Joint Surg (Br) 1987; 69(1)45–55
- Engh C A, Massin P, Suthers K E. Roentgenographic assessment of the biologic fixation of porous-surfaced femoral components. Clin Orthop 1990, 257: 107–28
- Engh C A, Jr, McAuley J P, Sychterz C J, Sacco M E, Engh C A, Sr. The accuracy and reproducibility of radiographic assessment of stress-shielding. A post-mortem analysis. J Bone Joint Surg (Am) 2000; 82(10)1414–20
- Furlong R J, Osborn J R. Fixation of hip prostheses by hydroxyapatite ceramic coatings. J Bone Joint Surg (Br) 1991; 73(5)741–5
- Geesink R G, de Groot K, Klein C P. Chemical implant fixation using hydroxyl-apatite coatings. The development of a human total hip prosthesis for chemical fixation to bone using hydroxyl-apatite coatings on titanium substrates. Clin Orthop 1987, 225: 147–70
- Gie G A, Linder L, Ling R S, Simon J P, Slooff T J, Tim-perley A J. Impacted cancellous allografts and cement for revision total hip arthroplasty. J Bone Joint Surg (Br) 1993; 75(1)14–21
- Gustilo R B, Pasternak H S. Revision total hip arthroplasty with titanium ingrowth prosthesis and bone grafting for failed cemented femoral component loosening. Clin Orthop 1988, 235: 111–9
- Halliday B R, English H W, Timperley A J, Gie G A, Ling R S. Femoral impaction grafting with cement in revision total hip replacement. Evolution of the technique and results. J Bone Joint Surg (Br) 2003; 85(6)809–17
- Haydon C M, Mehin R, Burnett S, Rorabeck C H, Bourne R B, McCalden R W, MacDonald S J. Revision total hip arthroplasty with use of a cemented femoral component. Results at a mean of ten years. J Bone Joint Surg (Am) 2004; 86(6)1179–85
- Huiskes R. The various stress patterns of press-fit, ingrown, and cemented femoral stems. Clin Orthop 1990, 261: 27–38
- Isacson J, Stark A, Wallensten R. The Wagner revision prosthesis consistently restores femoral bone structure. Int Orthop 2000; 24(3)139–42
- Kelly S J, Incavo S J, Beynnon B. The use of a hydroxyapa-tite-coated primary stem in revision total hip arthroplasty. J Arthroplasty 2006; 21(1)64–71
- Kolstad K, Adalberth G, Mallmin H, Milbrink J, Sahlstedt B. The Wagner revision stem for severe osteolysis. 31 hips followed for 1.5-5 years. Acta Orthop Scand 1996; 67(6)541–4
- Lawrence J M, Engh C A, Macalino G E, Lauro G R. Outcome of revision hip arthroplasty done without cement. J Bone Joint Surg (Am) 1994; 76(7)965–73
- Mahoney C R, Fehringer E V, Kopjar B, Garvin K L. Femoral revision with impaction grafting and a collarless, polished, tapered stem. Clin Orthop 2005, 432: 181–7
- Malchau H, Kärrholm J, Wang Y X, Herberts P. Accuracy of migration analysis in hip arthroplasty. Digitized and conventional radiography, compared to radiostereometry in 51 patients. Acta Orthop Scand 1995; 66(5)418–24
- Malkani A L, Lewallen D G, Cabanela M E, Wallrichs S L. Femoral component revision using an uncemented, proximally coated, long-stem prosthesis. J Arthroplasty 1996; 11(4)411–8
- Moreland J R, Moreno M A. Cementless femoral revision arthroplasty of the hip: minimum 5 years followup. Clin Orthop 2001, 393: 194–201
- Mulliken B D, Rorabeck C H, Bourne R B. Uncemented revision total hip arthroplasty: a 4-to-6-year review. Clin Orthop 1996, 325: 156–62
- Ornstein E, Atroshi I, Franzén H, Johnsson R, Sandquist P, Sundberg M. Early complications after one hundred and fourty-four consecutive hip revisions with impacted morselized allograft bone and cement. J Bone Joint Surg (Am) 2002; 84(8)1323–8
- Paprosky W G, Greidanus N V, Antoniou J. Minimum 10-year-results of extensively porous-coated stems in revision hip arthroplasty. Clin Orthop 1999, 369: 230–42
- Pekkarinen J, Alho A, Lepistö J, Ylikoski M, Ylinen P, Paavilainen T. Impaction bone grafting in revision hip surgery. A high incidence of complications. J Bone Joint Surg (Br) 2000; 82(1)103–7
- Peters C L, Riviero D P, Kull L R, Jacobs J J, Rosenberg A G, Galante J O. Revision total hip arthroplasty without cement: subsidence of proximally porous-coated femoral components. J Bone Joint Surg (Am) 1995; 77(8)1217–26
- Rahbek O, Kold S, Bendix K, Overgaard S, Søballe K. Superior sealing effect of hydroxyapatite in porous-coated implants: experimental studies on the migration of polyethylene particles around stable and unstable implants in dogs. Acta Orthop 2005; 76(3)375–85
- Raman R, Kamath R P, Parikh A, Angus P D. Revision of cemented hip arthroplasty using a hydroxyapatite-ceramic-coated femoral component. J Bone Joint Surg (Br) 2005; 87(8)1061–7
- Reikerås O, Gunderson R B. Excellent results with femoral revision surgery using an extensively hydroxyapatite-coated stem: 59 patients followed for 10-16 years. Acta Orthop 2006; 77(1)98–103
- Rosenberg A. Cementless total hip arthroplasty: femoral remodeling and clinical experience. Orthopaedics 1989; 12(9)1223–33
- Suominen S, Santavirta S. Revision total hip replacement using the bias proximal porous-coated femoral component. Ann Chir Gynaecol 1996; 85(4)347–51
- Trikha S P, Singh S, Raynham O W, Lewis J C, Mitchell P A, Edge A J. Hydroxyapatite-ceramic-coated femoral stems in revision hip surgery. J Bone Joint Surg (Br) 2005; 87(8)1055–60
- Turner T M, Sumner D R, Urban R M, Rivero D P, Galante J O. A comparative study of porous coatings in a weight-bearing total hip-arthroplasty model. J Bone Joint Surg (Am) 1986; 68(9)1396–409
- Ullmark G, Hallin G, Nilsson O. Impacted corticocancellous allografts and cement for revision of the femur component in total hip arthroplasty. J Arthroplasty 2002; 17(2)140–9
- van Biezen F C, ten Have B L, Verhaar J A. Impaction bone-grafting of severely defective femora in revision total hip surgery. 21 hips followed for 41-85 months. Acta Orthop Scand 2000; 71(2)135–42
- Wagner H. Revision prosthesis for the hip joint in severe bone loss. Orthopäde 1987; 16(4)295–300