Abstract
Background The long-term results of uncemented total hip arthroplasties vary widely due to differences in design, metal alloy, coating, surface structure, and porosity.
Patients and methods We retrospectively studied 75 cementless Zweymüller SL stems in combination with Endler titanium-backed threaded cups (Z-E) in 70 patients. 35 patients were women, and the mean age at surgery was 52 (24–68) years. 16 patients died and 1 emigrated, 7 patients (of which 1 later died) subsequently underwent revision, and the remaining 47 patients with 50 original arthroplasties were followed up after a median of 16 (15–18) years.
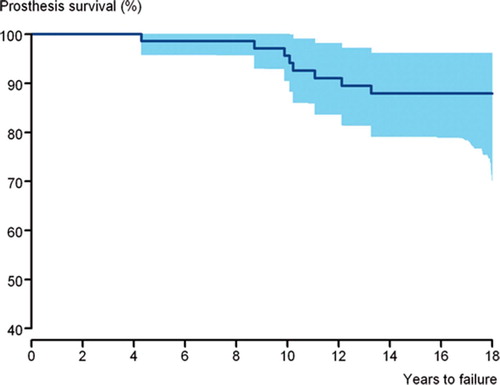
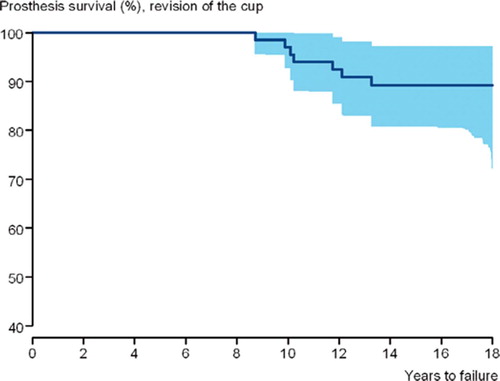
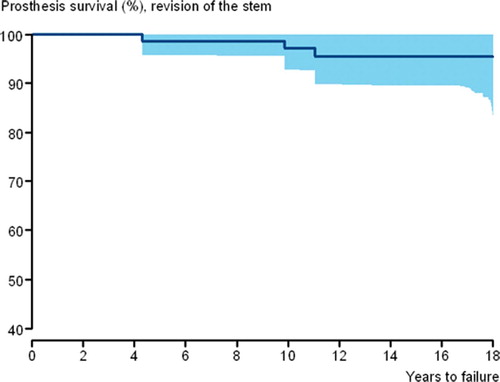
Results Revision of 8 hips resulted in an 18-year Kaplan-Meier estimated overall survival rate of 88% (CI: 79–96). 6 of 7 cup revisions were due to liner wear and osteolysis, and 1 was due to aseptic loosening. 2 of 3 stem revisions were due to femoral loosening and 1 was due to fracture of the neck of the stem. The clinical results were good, with a mean Harris hip score of 89 (54–100). Half of 70 hips in 65 patients had ectopic bone formation. All unrevised implants were radiographically stable, with a mean liner wear of 0.07 mm/year.
Interpretation These long-term results demonstrate that the combination of a Zweymüller SL stem and an Endler titanium-backed screw cup is a good hip arthroplasty in young and active patients. A prefixed polyethylene liner is a drawback, necessitating exchange of the whole cup in cases with polyethylene wear.
The Zweymüller stem was introduced in combination with the uncemented Endler all-polyethylene cup (Zweymuller and Semlitsch Citation1982, Endler et al. Citation1983). However, the latter showed unacceptable revision rates due to aseptic loosening (Havelin et al. Citation1995b). An identical c.p titanium-backed cup with a prefixed UHMW polyethylene liner replaced the original Endler cup. With respect to loosening, long-term survival of 98–100% for the Zweymüller stem in combination with screw cups other than the all-polyethylene Endler has been reported after 13–15 years of follow-up (Garcia-Cimbrelo et al. Citation2003, Grubl et al. Citation2006). In reports from the Norwegian Arthroplasty Register, the Zweymüller SL stem and the Endler metal-backed cup had revision rates of 1% at 4.5 and 5 years of follow-up, respectively (Havelin et al. Citation1995a, Citationb). To our knowledge, the long-term results of the Zweymüller-Endler metal combination have not been evaluated previously. We thus conducted a retrospective follow-up study of young patients who received a Zweymüller SL stem combined with an Endler metal screw cup at two Norwegian hospitals from 1988 through 1990.
Patients, implants, and methods
Between August 1988 and March 1990, 70 patients received 75 hip arthroplasties with Zweymüller SL stem and Endler metal-backed screw cup (Z-E combination) at the Martina Hansens Hospital (MHH) and Rikshospitalet Medical Center (RMC) (52 and 23 arthroplasties, respectively). The Z-E combination was chosen for all patients less than 60 years of age and also 10 particularly active patients between 60 and 70 years of age. The 35 women (38 hips) and 35 men (37 hips) together had a mean age of 52 (24–68) years. Osteoarthritis was the commonest diagnosis ().
Table 1. Diagnoses
13 hips had undergone prior surgery (4 shelf operations a.m. Spitzy, 3 osteosynthesis for femoral neck fracture, 1 Smith-Peterson cup, 1 hemiprosthesis, 1 proximal femoral osteotomy, 1 fixation of slipped femoral head, 1 open removal of loose cartilage, 1 open reduction of traumatic hip dislocation). Most patients were in Charnley category B (Charnley Citation1972) ().
Table 2. Breakdown of patient numbers according to Charnley categories. A: unilateral hip disorder; B: bilateral hip disorder; C: other conditions directly impeding mobility
Implants
The uncoated Zweymüller SL femoral stem (Allopro, Baar, Switzerland) was made of grit-blasted Protasul-100 (Ti6Al7Nb alloy) with an average surface roughness of ra = 3–5 μm. The rectangular cross-sectional shape was tapered in the frontal plane with an anterior and a posterior beam (). It was available in 8 standard and 6 special sizes.
We used 14/16 neck cones supporting 3 different lengths of 32-mm Al2O3 heads (Biolox; Ceramtec AG, Plochingen, Germany). The acetabular component (Endler Titanium Metal-Backed; Allopro, Baar, Switzerland), which was a further development of the Endler all-polyethylene screw cup (Endler et al. Citation1983), had a forged metal backing made of c.p. titanium without perforations, containing a prefixed ultra-high-molecular weight (UHMW) polyethylene insert. Externally, it was shaped like a truncated cone, supplied with wide threads and grit-blasted with a mean surface roughness of ra = 4–5 μm. It was available in 7 sizes (52— 72 mm outer diameter) and sterilized by gamma irradiation (). Median cup size used was 61 (52–68) mm, giving a mean polyethylene liner thickness of 9.7 (4.5–2.5) mm.
Operation
The patients were operated in the supine position using the direct lateral approach. After reaming of the acetabulum, accurate threads were cut and the Endler component screwed in. The femoral canal was reamed to exactly match the stem that was subsequently inserted. Mean operation time was 98 (55–155) min; peroperative blood loss was 1.1 (0.3–3.0) L. The antibiotic and antithrombotic prophylaxis at one hospital (MHH) included Cefalotin (Keflin) 2 g × 2 for one day and dextran 500 mL (Macrodex) intravenously peroperatively, followed by warfarin for 3 months postoperatively. At the other hospital (RMC), cloxacillin (Ekvacillin) 4 g per day for 3 days and dextran 500 mL (Macrodex) intravenously peroperatively followed by Heparin 5000 IE × 2 for 7 days postoperatively were used. No prophylaxis for ectopic bone formation was given. Active abduction exercises were started during the postoperative hospital stay. Patients were allowed partial weight bearing with crutches for 3 months, after which full weight bearing was allowed.
Patient information was obtained from the hospital records and cross-checked with the Norwegian Arthroplasty Register (NAR). Information on revisions throughout 2006 was received from the NAR and linked to the original data. 16 patients died during the follow-up period (17 hips), mean 9 (0–16) years after the operation; 1 of them had been revised prior to his death. 1 patient emigrated (1 hip). 8 arthroplasties in 7 patients were revised, leaving 6 patients alive with 7 revised hips. The remaining 47 patients with 50 original arthroplasties in situ were followed up after a median of 16 (15–18) years. Information was obtained on Harris Hip score (HHS) (Harris Citation1969), body mass index (BMI, kg/m2), and the EQ-5D self-assessment score (EuroQuol Citation1990).
Radiographs of 5 hips in 4 patients who died after 6 months, 7 months, 2 years, and 5 years— of causes unrelated to the procedure—had been destroyed. All patients were evaluated with 3 or more radiographs (postoperatively, and at least 1 later control in addition to the follow-up examination) except for 1 patient who only had postoperative and follow-up radiographs. Standardized frontal radiographs were analyzed if there was ectopic bone formation (Brooker et al. Citation1973). Loosening and osteolytic lesions were assessed according to the methods and zones of De Lee and Charnley (Citation1976) and Hodgkinson et al. (Citation1988), evaluating migration and demarcation/osteolysis around the acetabular component and the zones of Gruen for the femoral component. The frontal radiographs were evaluated. Focal/expansile osteolysis was defined as any focal area of bone loss adjacent to the prosthesis where the demarcated space had a round or scalloped appearance extending away from the surface of the implant. Radiolucent lines adjacent to the prosthesis were classified as linear osteolysis when they exceeded 1 mm (Zicat et al. Citation1995). Polyethylene wear was estimated according to Dorr and Wan (Citation1996) (). Stability was assessed according to Engh et al. (Citation1990), evaluating the presence of endosteal new bone formation in the gap between the bone and the implant and absence of reactive lines around the implant, and measuring implant migration on subsequent radiographs.
Figure 3. Frontal radiograph with Gruen femoral zones 1–7 and De Lee-Charnley acetabular zones I—III. Polyethylene wear was estimated along a line from the superior to the inferior edge margins of the cup. The distances from the superior (A) and the inferior (B) edge margins to the femoral head were measured with a manual calliper. Linear wear was calculated using the formula (A-B) /2.The measurements were corrected for magnification using the 32-mm diameter of the femoral head.

Statistics
The statistical comparisons of means were done with the Student t-test for independent observational series, and the Student t-test for paired samples when comparing outcome at surgery and follow-up. The chi-square test was used for categorical outcome factors. Prosthesis lifetime was defined as the time interval from insertion of the prosthesis until revision (surgical removal or exchange of one or more components). Kaplan-Meier estimated survival curves with 95% confidence intervals (CIs) were established with all revisions, revision of the cup, and revision of the stem as endpoints. A modified lower confidence limit was calculated based on the number of prostheses still at risk, thus leading to a confidence interval that becomes wider at each censored observation. When a patient died or emigrated, the lifetime of the prosthesis was censored at the relevant date and again at the end of the study (December 31, 2006). Cox multiple regression analyses provided relative revision risk estimates (hazard rate ratios) for sex, age (cut-off points at tertile values 50.7 and 56.6), diagnosis (primary osteoarthritis vs. other diagnoses), and BMI (< 25 vs. ≥ 25). 5 patients operated bilaterally with the Z-E prosthesis were included in the study. To investigate the effect of including both hips of bilaterally-operated patients, analyses were performed on a data set including one randomly chosen hip. We found the same outcome as when we included all hips (data not shown). Furthermore, a marginal Cox regression model was fitted. S-PLUS 7.0 (Insightful Corp., New York, NY) and SPSS version 12.0 for Windows were used for the statistical analyses.
Results
Clinical results
The mean BMI increased from 24.7 (SD 3.7, n = 73) at surgery to 26.2 (SD 4.3, n = 47) at follow-up (p < 0.001). The 3 high-wear patients had a lower BMI at surgery than the others (23 vs. 25), the difference increasing at follow-up (23 vs. 27), but this was not statistically significant (p = 0.2).
Clinical and patient satisfaction results included a mean HHS of 89 (54–100), an EQ-5D index score of 0.75 (−0.10–1.00), and EQ VAS of 77 (30–100). The lower patient satisfaction in the grade 3 ectopic bone group (mean HHS = 82 (54–100), EQ-5D = 0.66 (−0.10–1.00), and Euro VAS = 74 (30–90)) compared to the grade 0 group (mean HHS = 89 (56–100), EQ-5D = 0.76 (0.16–1.0) and Euro VAS = 77 (40–91)) was not statistically significant for any parameter (p = 0.2, p = 0.3 and p = 0.6, respectively). 37 out of 47 patients had an HHS of >80.
Radiographic results
All unrevised components were stable, showing intimate contact along the whole or the greater part of the bone-implant interface. In the unrevised patients, there was focal osteolysis in Charnley zone I in 6 hips, measuring 22 (11–32) mm2. No linear osteolysis was observed on the acetabular side. 1 femur showed a focal osteolysis (25 mm2) in Gruen zone 5 and also linear osteolysis in zones 1 and 7, extending into zones 2 and 6 (). 3 stems had linear osteolysis along most of the Gruen zones 1 and 7, and 1 stem showed small focal proximal osteolysis in zones 1 (9 mm2) and 7 (10 mm2). 1 stem showed small focal proximal osteolysis in zone 7 (21 mm2).
There was no Broker grade 4 ectopic bone formation in the 70 hips that were available for examination. 33 of the hips did not show any ectopic bone formation, and the remainder were equally distributed between grades 1, 2, and 3.
Ectopic bone was removed from 2 hips (grade 3) after 1 and 8 years because of pain and restricted mobility. 1 operation was successful and 1 resulted in recurrent production of bone. These were graded as 1 and 3, respectively, at the follow-up.
The mean polyethylene wear at follow-up was 1.19 (0–3.6) mm, resulting in a mean wear rate of 0.07 mm per year. 3 cups showed a wear rate of > 0.2 mm/year; 2 of them demonstrated asymptomatic osteolysis in Charnley zone 1. Being asymptomatic and with no threat of wear-through, they are not scheduled for revision.
Revisions and survivorship analysis
8 hips in 7 patients were revised after a median of 10 (4–13) years ().
Table 3. Characteristics of the reoperated hips
Of the revised implants, 6 sockets were exchanged due to polyethylene wear—2 with threatening wear-through of the liner (1 of them with acetabular osteolysis in Charnley zone 1), 3 with trochanteric femoral osteolysis, and 1 with concomitant femoral loosening. 1 socket was exchanged because of loosening. The former 5 sockets were stable and osseointegrated, and had to be chiseled out. 3 stems were removed, 2 due to loosening and 1 due to femoral stem fracture. All cases of osteolysis (4 femoral and 1 acetabular) were emptied and filled with bone from the ipsilateral iliac crest (2 patients) or bone bank-derived allograft (3 patients).
The 18-year overall survival rate was 88% (CI: 80–96): 89% (CI: 82–97) for the cups and 95% (CI: 90–100) for the stems ().
Cox regression analysis revealed a higher revision rate for the indication primary osteoarthrosis than for other reasons for operating, when adjusting for sex, age, and BMI (RR = 6, p = 0.03). Age, sex, and BMI had no statistically significant effect on the revision rate. Results from additional analyses accounting for correlated data were similar to those given above.
Complications
3 out of 5 fissures (1 calcar and 4 trochanteric) were secured with cerclage peroperatively. 1 patient was reoperated because of bleeding. Pareses of the sciatic and femoral nerves were seen in 1 and 2 patients, respectively; and 3 patients developed deep-vein thrombosis. All of these complications resolved completely. There were no luxations or infections.
Discussion
The limitations of our study are its retrospective, unblinded design with lack of a control group, the variable observations during the follow-up period, and lack of clinical results from the patients who died. The strengths of our study include the high follow-up rate, the long observation period, and cross-checking of the patients with a national health register (NAR).
The 18-year cumulative survivorship rates of 88% for the combination, 89% for the cup, and 95% for the stem were high, particularly since the patients were young. Our results are in accordance with some mid- and long-term results for the same femoral component and a similar uncemented screw socket (Grubl et al. Citation2006). The cup used in the latter study (CSF) has a conical screw shell of grit-blasted c.p. titanium with a surface roughness of approximately 4–5 μm, like the Endler cup, but the CSF liner was exchangeable. Centers using total cemented arthroplasties such as Exeter (Franklin et al. Citation2003) and Charnley (Wroblewski et al. Citation2007) have also reported high long-term survival, where the rate of aseptic loosening has been higher and the revision rate due to liner wear lower than in our series. Our survival rates surpass those of comparable uncemented and cemented alternatives reported by the population-based Scandinavian registers (Havelin et al. Citation2000, Eskelinen et al. Citation2005) due to lower femoral revision rate and similar acetabular revision rate.
Design and surface structure
Experimentally, Goldberg et al. (Citation1995) favored a grit-blasted titanium alloy surface of Ra= 4 μm approximately rather than a polished or fiber-mesh surface of the same material. Titanium implants with a rough surface have the ability to promote extensive bone-implant contact, as demonstrated histologically in both experimental (Albrektsson and Johansson Citation2001) and human retrieval studies (Lintner et al. Citation1988). The design of the press-fit rectangular stem and the truncated conical-screw socket with exact cutting threads provides excellent primary stability (Zweymuller et al. Citation1988), facilitating bone in-growth. Smooth-surfaced prosthe-ses such as the Mecring titanium alloy screw cup, the Weill c.p. titanium screw cup (Aldinger et al. Citation2004) and the all-polyethylene screw cup of Endler (Havelin et al. Citation1995b) have shown poor results. Hydroxyapatite-coated implants have increased bone in-growth compared to non-coated implants (Soballe Citation1993), but wear, osteolysis, and loosening related to coat flaking and third-body particles have reduced the survival rate of HA-coated acetabular components (Rokkum et al. Citation1999). The excellent long-term bony fixation of the Zweymüller-Endler metal combination and the inferior mid- and long-term results of the HA-coated acetabular components suggests that HA is redundant.
Osteolysis, wear, and loosening
A solid acetabular metal shell without coat and holes obstructs communication between the articulation and the bone-metal interface, except for the edges—thus preventing access of submicron particles from the articulation (polyethylene, metallic, or ceramic particles), which could otherwise induce inflammation and osteolysis (Santavirta et al. Citation1990). Linear osteolysis in uncemented arthroplasties is a negative predictive factor concerning implant loosening, whereas focal osteolysis has less impact on the results (Zicat et al. Citation1995). The use of a prefixed UHMW polyethylene insert may reduce movements between polyethylene and metal shell, thus hampering wear, but it is a major drawback that the whole cup must be chiselled out when revising for wear. To our knowledge, all modern threaded cups have exchangeable inserts, so this disadvantage no longer exists. A mean liner wear rate of 0.07 mm/year is acceptable, but 3 cups had high wear exceeding 0.2 mm/year. There were no differences in any other parameters between high-wear and low-wear patients in our study. The ceramic heads may have diminished the wear rate, as shown in other studies (Kim et al. Citation2005), but volumetric wear increases with 32-mm heads (Shaju et al. Citation2005), which was our only ceramic option. The wear rate in this study was comparable to that of cemented arthroplasties (Wroblewski et al. Citation2004), but the revision rate due to liner wear was too high—representing the major problem with uncemented acetabular sockets. Similar findings were demonstrated by Della Valle et al. (Citation2004) in a long-term follow-up of Harris-Galante 1 sockets. New bearing surfaces (ceramic-on-ceramic, metal-on-metal, or the use of highly crosslinked UHMW polyethylene) (Santavirta et al. Citation2003) may reduce wear and prolong implant survival, but the long-term results remain to be seen. Our 32-mm alumina head does not seem to have increased implant loosening, and together with the lateral surgical approach it has probably protected against dislocations (Byström et al. Citation2003). A 28-mm head reduces volumetric wear (Oparaugo et al. Citation2001) and allows a thicker liner, but it was not available with the Endler cup.
The overall patient satisfaction was high, with an HHS of 89 after 15–18 years. The self-assessed estimation of health scored lower in our patients than in an average age-corrected Scandinavian population (Bjork and Norinder Citation1999, Burström et al. Citation2001). High HHS and lower quality of life assessment points to reasons other than hip disorder. Self-assessment scores have limitations (Aamodt et al. Citation2004) and a broader psychosocial interview might have revealed the difference. This was beyond the scope of our investigation, however.
Ectopic bone formation in arthroplasties varies in different studies and with the different types of arthroplasty, and it can influence the clinical results (Neal et al. Citation2002). Average HHS was similar in the groups with ectopic bone formation (88) and without it (89), but the 9 patients with grade 3 had a lower average HHS (82) than the overall group. The difference was not statistically significant, but reduced functional results with Brooker grade 3 and 4 ectopic bone formation have been shown by Hirota et al. (Citation1997). NSAIDs given prophylacti-cally reduce ectopic bone formation, but they may have a negative effect on results in the longer term (Persson et al. Citation2005).
BMI increased during the observation period, following the general tendency in the population (Fogelholm et al. Citation2000). Neither short-term studies (Moran et al. Citation2005) nor long-term ones (McLaughlin and Lee Citation2006) have shown any increase in revisions or other complications due to increased BMI, except for a higher rate of stem loosening in the extremely obese (with BMI > 35) (Munger et al. Citation2006). None of our patients were extremely obese at surgery, and only 1 was obese at follow-up; thus, no negative effect of a high BMI was seen.
In summary, we found good clinical and radio-graphic results with this uncemented screw cup with press-fit femur in this relatively young group. Survival analysis gave results comparable to those for the best cemented and uncemented arthroplasties available. A prefixed acetabular liner is a major drawback, necessitating the removal of the whole screw cup when revising for polyethylene wear.
Contributions of authors
OR: planning and execution of the study, collection and analysis of data, and writing of the manuscript. PS: planning and execution of the study, and collection of the data. MR and BE: contributed to the interpretation of the data and the statistics, and to the preparation and revision of the manuscript.
No benefits have been received or will be received from a commercial party related directly or indirectly to the subject of this article. No funds were received in support of this study.
- Albrektsson T, Johansson C. Osteoinduction, osteoconduction and osseointegration. Eur Spine J (Suppl 2) 2001; 10: S96–101
- Aldinger P R, Thomsen M, Lukoschek M, Mau H, Ewerbeck V, Breusch S J. Long-term fate of uncemented, threaded acetabular components with smooth surface treatment: minimum 10-year follow-up of two different designs. Arch Orthop Trauma Surg 2004; 124(7)469–75
- Bjork S, Norinder A. The weighting exercise for the Swedish version of the EuroQol. Health Econ 1999; 8(2)117–26
- Brooker A F, Bowerman J W, Robinson R A, Riley L H, Jr. Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg (Am) 1973; 55(8)1629–32
- Burström K, Johannesson M, Diderichsen E. Health-related quality of life by disease and socio-economic group in the general population in Sweden. Health Policy 2001; 55(1)51–69
- Byström S, Espehaug B, Furnes, Havelin L I. Femoral head size is a risk factor for total hip luxation: a study of 42,987 primary hip arthroplasties from the Norwegian Arthroplasty Register. Acta Orthop Scand 2003; 74(5)514–24
- Charnley J. The long-term results of low-friction arthroplasty of the hip performed as a primary intervention. J Bone Joint Surg (Br) 1972; 54(1)61–76
- De Lee J G, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop 1976, 121: 20–32
- Della Valle C J, Berger R A, Shott S, Rosenberg A G, Jacobs J J, Quigley L, Galante J O. Primary total hip arthroplasty with a porous-coated acetabular component. A concise follow-up of a previous report. J Bone Joint Surg (Am) 2004; 86(6)1217–22
- Dorr L D, Wan Z. Comparative results of a distal modular sleeve, circumferential coating, and stiffness relief using the Anatomic Porous Replacement II. J Arthroplasty 1996; 11(4)419–28
- Endler M, Plenk J, Jr., Grundschober G, Girtler D, Schnabl H. Results of experimental testing of a screw-in in polyethylene acetabulum in sheep. Z Orthop Ihre Grenzgeb 1983; 121(1)64–73
- Engh C A, Massin P, Suthers K E. Roentgenographic assessment of the biologic fixation of porous-surfaced femoral components. Clin Orthop 1990, 257: 107–28
- Eskelinen A, Remes V, Helenius I, Pulkkinen P, Nevalainen J, Paavolainen P. Total hip arthroplasty for primary osteoarthrosis in younger patients in the Finnish arthroplasty register. 4,661 primary replacements followed for 0–22 years. Acta Orthop 2005; 76(1)28–41
- EuroQuol G T. Euroquol: a new facility for the measurement of health related quality of life. Healt Policy 1990; 16: 199–208
- Fogelholm M, Kujala U, Kaprio J, Sarna S. Predictors of weight change in middle-aged and old men. Obes Res 2000; 8(5)367–73
- Franklin J, Robertsson O, Gestsson J, Lohmander L S, Ingvarsson T. Revision and complication rates in 654 Exeter total hip replacements, with a maximum follow-up of 20 years. BMC Musculoskelet Disord 2003; 4(6)1–5
- Garcia-Cimbrelo E, Cruz-Pardos A, Madero R, Ortega-Andreu M. Total hip arthroplasty with use of the cement-less Zweymuller Alloclassic system. A ten to thirteen-year follow-up study. J Bone Joint Surg (Am) 2003; 85(2)296–303
- Goldberg V M, Stevenson S, Feighan J, Davy D. Biology of grit-blasted titanium alloy implants. Clin Orthop 1995, 319: 122–9
- Grubl A, Chiari C, Giurea A, Gruber M, Kaider A, Marker M, Zehetgruber H, Gottsauner-Wolf F. Cementless total hip arthroplasty with the rectangular titanium Zweymuller stem. A concise follow-up, at a minimum of fifteen years, of a previous report. J Bone Joint Surg (Am) 2006; 88(10)2210–5
- Harris W H. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg (Am) 1969; 51(4)737–55
- Havelin L I, Espehaug B, Vollset S E, Engesaeter L B. Early aseptic loosening of uncemented femoral components in primary total hip replacement. A review based on the Norwegian Arthroplasty Register. J Bone Joint Surg (Br) 1995a; 77(1)11–7
- Havelin L I, Vollset S E, Engesaeter L B. Revision for aseptic loosening of uncemented cups in 4,352 primary total hip prostheses. A report from the Norwegian Arthroplasty Register. Acta Orthop Scand 1995b; 66(6)494–500
- Havelin L I, Engesaeter L B, Espehaug B, Furnes O, Lie S A, Vollset S E. The Norwegian Arthroplasty Register: 11 years and 73,000 arthroplasties. Acta Orthop Scand 2000; 71(4)337–53
- Hirota S, Takeuchi E, Fujita S, Inui H, Oda T, Fuji T. Ectopic bone formation after total hip arthroplasty. Bull Hosp Jt Dis 1997; 56(4)206–10
- Hodgkinson J P, Shelley P, Wroblewski B M. The correlation between the roentgenographic appearance and operative findings at the bone-cement junction of the socket in Charnley low friction arthroplasties. Clin Orthop 1988, 228: 105–9
- Kim S Y, Kim D H, Oh C W, Kim P T, Ihn J C. Total hip arthroplasty with the use of nonmodular cementless acetabular component. J Arthroplasty 2005; 20(5)632–8
- Lintner F, Zweymuller K, Bohm G, Brand G. Reactions of surrounding tissue to the cementless hip implant Ti-6Al-4V after an implantation period of several years. Autopsy studies in three cases. Arch Orthop Trauma Surg 1988; 107(6)357–63
- McLaughlin J R, Lee K R. The outcome of total hip replacement in obese and non-obese patients at 10-to 18-years. J Bone Joint Surg (Br) 2006; 88(10)1286–92
- Moran M, Walmsley P, Gray A, Brenkel I J. Does body mass index affect the early outcome of primary total hip arthroplasty?. J Arthroplasty 2005; 20(7)866–9
- Munger P, Roder C, Ackermann-Liebrich U, Busato A. Patient-related risk factors leading to aseptic stem loosening in total hip arthroplasty: a case-control study of 5,035 patients. Acta Orthop 2006; 77(4)567–74
- Neal B, Gray H, MacMahon S, Dunn L. Incidence of heterotopic bone formation after major hip surgery. ANZ J Surg 2002; 72(11)808–21
- Oparaugo P C, Clarke I C, Malchau H, Herberts P. Correlation of wear debris-induced osteolysis and revision with volumetric wear-rates of polyethylene: a survey of 8 reports in the literature. Acta Orthop Scand 2001; 72(1)22–8
- Persson P E, Nilsson O S, Berggren A M. Do non-steroidal anti-inflammatory drugs cause endoprosthetic loosening? A 10-year follow-up of a randomized trial on ibuprofen for prevention of heterotopic ossification after hip arthroplasty. Acta Orthop 2005; 76(6)735–40
- Rokkum M, Brandt M, Bye K, Hetland K R, Waage S, Reigstad A. Polyethylene wear, osteolysis and acetabular loosening with an HA-coated hip prosthesis. A follow-up of 94 consecutive arthroplasties. J Bone Joint Surg (Br) 1999; 8(4)582–9
- Santavirta S, Hoikka V, Eskola A, Konttinen Y T, Paavilainen T, Tallroth K. Aggressive granulomatous lesions in cementless total hip arthroplasty. J Bone Joint Surg (Br) 1990; 72(6)980–4
- Santavirta S, Bohler M, Harris W H, Konttinen Y T, Lappalainen R, Muratoglu O, Rieker C, Salzer M. Alternative materials to improve total hip replacement tribology. Acta Orthop Scand 2003; 74(4)380–8
- Shaju K A, Hasan S T, D'Souza L G, McMahon B, Masterson E L. The 22-mm vsthe 32-mm femoral head in cemented primary hip arthroplasty long-term clinical and radiological follow-up study. J Arthroplasty 2005; 20(7)903–8
- Soballe K. Hydroxyapatite ceramic coating for bone implant fixation. Mechanical and histological studies in dogs. Acta Orthop Scand (Suppl 255) 1993; 64: 1–58
- Wroblewski B M, Siney P D, Fleming P A. Wear of the cup in the Charnley LFA in the young patient. J Bone Joint Surg (Br) 2004; 86(4)498–503
- Wroblewski B M, Siney P D, Fleming P A. Charnley low-frictional torque arthroplasty in young rheumatoid and juvenile rheumatoid arthritis: 292 hips followed for an average of 15 years. Acta Orthop 2007; 78(2)206–10
- Zicat B, Engh C A, Gokcen E. Patterns of osteolysis around total hip components inserted with and without cement. J Bone Joint Surg (Am) 1995; 77(3)432–9
- Zweymuller K, Semlitsch M. Concept and material properties of a cementless hip prosthesis system with Al2O3 ceramic ball heads and wrought Ti-6Al-4V stems. Arch Orthop Trauma Surg 1982; 100(4)229–36
- Zweymuller K A, Lintner F K, Semlitsch M F. Biologic fixation of a press-fit titanium hip joint endoprosthesis. Clin Orthop 1988, 235: 195–206
- Aamodt A, Nordsletten L, Havelin L I, Indrekvam K, Utvag S E, Hvidng K. Documentation of hip prostheses used in Norway: a critical review of the literature from 1996–2000. Acta Orthop Scand 2004; 75(6)663–76