Abstract
Background Treatment of hips with abnormal anatomy is challenging, and requires demanding surgical technique. We report the preoperative planning and the functional outcome of 38 patients with severe distorted anatomy who were treated with custom implants.
Patients and methods 38 consecutive patients (48 hips) were selected for customized femoral implants. The diagnosis was arthrosis due to congenital dislocation of the hip (CDH). We used plain radiographs, CT, and CAD-CAM analysis. The mean age was 47 (22–69) years and the mean preoperative D'Aubigne score was 10 (6–12). The mean follow-up time was 6 (4–8) years.
Results All implants had optimal fit and fill. There were 2 revisions due to infection. No patients had thigh pain and no patients had aseptic loosening. There were 5 intraoperative and 6 postoperative complications. The mean postoperative D'Aubigne score was 17 (10–18).
Interpretation Preoperative planning with modern technology and customized implants makes the procedure accurate, easier for the surgeon, and safer for the patient.
The treatment of severe deformed hip due to congenital and developmental diseases or trauma remains a challenging problem, and the surgical technique is demanding (Huo et al. Citation1993). Preoperative planning and templating has been advocated by Muller (Citation1992) as an integral part of total hip arthroplasty. There are currently numerous implants of different sizes and offsets, which makes preoperative planning imperative.
In our clinic, more than 600 young adult patients with neglected and distorted anatomy of the hip— due to congenital dysplasia of hip (CDH)—have been treated with hip arthroplasty. This prospective study reports the preoperative planning, the selection, and the clinical follow-up results for a series of hips with severe distorted proximal anatomy using customized grit-blasted femoral components.
Patients and methods
Between March 1998 and March 2002, 170 consecutive patients with severe deformed anatomy of the hip joint were included in our protocol (188 dysplastic hips). Our clinic is a reference center for CDH and a single treatment protocol has been used by the senior author for the last 10 years (Xenakis et al. Citation1996). The protocol consists of: (1) pelvis AP and hip lateral radiographs, (2) CT of hip, femur, femoral condyle, foot, and (3) CT. When the anatomy is severely distorted, a CAD-CAM is used for selection of a suitable implant. 38 patients (48 abnormal hips) were selected for customized cementless prostheses, as suitable off-the-shelf stems were unavailable for these severely deformed femurs. Informed consent was obtained from all patients.
Preoperative data
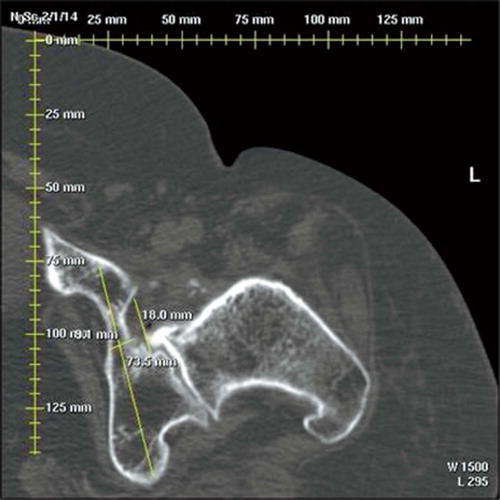
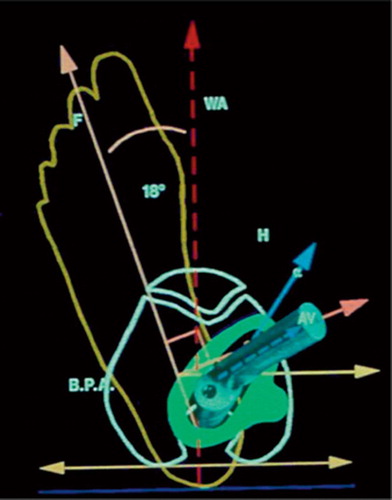
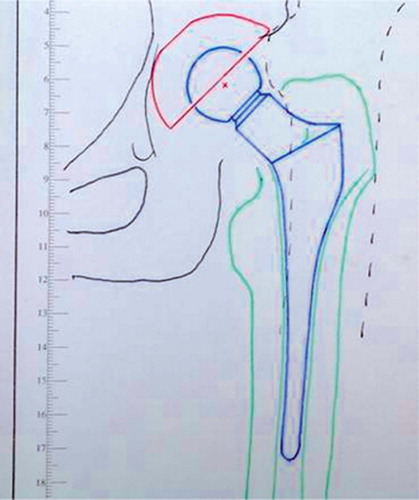
The radiographic analysis is based on a frontal view of the pelvis and a lateral view of the hip. Data from the CT are necessary for the intramedullary design of the stem, and for planning the extramedullary part of reconstruction. To assess the intramedullary femoral anatomy, scans every 5 mm until the lesser trochanter, and then every 10 mm until the middle of the femur are made. 4 additional scans are necessary to complete the planning. The first one is through the acetabulum to reveal bone stock (), and the other three provide data for the anteversion of the prosthetic neck: above the lesser trochanter (giving the axis of the upper femur), at the knee condylar axis, and in the foot by the second metatarsus axis. Finally, a CT topogram is performed for measurement of leg length. We calculate the offset from the topogram according to the opposite hip. If the opposite hip is abnormal, based on our experience, we calculate 4-cm offset for small patients with narrow pelvis and 4.5-cm offset for heavy, obese patients. The initial data are processed further to determine the mechanical parameters and the planning of the entire operation is done. Then the choice of prosthesis or the design is made, followed by construction of a customized arthroplasty (). The entire process follows the principles of CAD-CAE-CAM and is based on CT scanning data.
Surgical planning
Center of rotation. The first step is to locate the center of rotation in the true acetabulum, and the socket size. The anteroposterior diameter of the acetabulum is precisely assessed with the CT scan view. The next step is the location of the greater trochanter according to this new center of rotation, and the desired lengthening as measured on the scanogram. This position will determine the level of the femoral cut. The final step is determination of the neck anteversion with the angle between the longitudinal plane through the axis of the femur and the center of the femoral head and the posterior condylar plane.
If the femur is substantially longer than the con-tralateral femur, a shortening osteotomy of the femur should be performed. In order not to cause any disturbance in the area where the femoral component will be placed, the osteotomy is performed more distally than the end of the prosthesis and the femur is shortened to make the limbs of equal length. The osteotomy is performed before reduction of the femoral stem. The osteotomy is stabilized with an LC-DCP plate. If there is an axial deviation of the knee, which is most often valgus deformity, this may be corrected at the same time. The necessary angles of the osteotomies and the length of the portion of bone to be excised are calculated by the computer.
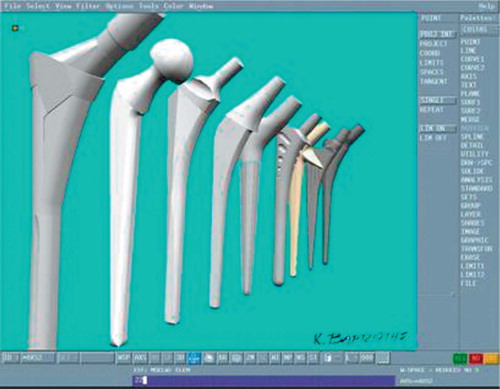
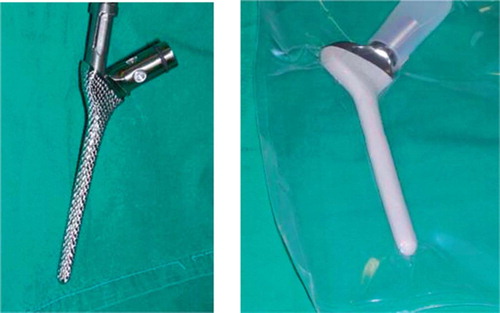
The next important step is that of selection of the type of prosthesis. The selection of the stem is not easy, due to the irregular geometry of the medullary canal of the femur and also because of the need to restore the proper mechanics of the hip. From the preceding design and simulation of the procedure on the computer, the position of the trochanter, and the offset of the prosthesis, the selection that satisfies the basic requirements is made from an arthroplasty library in the computer (). A trial implantation of the prostheses that has been selected is simulated on the computer and the one that best fulfills the criteria of the best implantation is chosen. If this evaluation shows that no prosthesis fulfills the criteria of satisfactory implantation, then production of a customized prosthesis is chosen (). The custom prosthesis has a custom grit-blasted broach, which is undersized by 2 mm and is used for impaction of the cancelous bone of the femoral canal. Also, the custom broach is tapered, thus enabling the use of trial heads.
As regards the acetabulum, a special cup with a hook for anchorage in the foramen obturatum— and the possibility of screw placement on healthy ilium bone—is used in all cases.
38 patients (36 women) had 48 custom-made total hip components implanted for one of the following diagnoses: 16 high dislocations, 28 low dislocations, and 4 dysplastic joints (according to Hartofilakidis et al. (Citation1996)) with arthritis. The mean age of patients was 47 (22–69) years. The mean weight was 72 (59–88) kg and the mean height was 162 (145–174) cm. 12 patients had had previous corrective surgery: 9 pelvic osteotomies, 1 hip arthrodesis, and 2 femoral osteotomies. 10 patients underwent bilateral surgery in staged operations. All the patients had had a limp since childhood and many had significant groin or thigh pain. Each patient was rated preoperatively according to D'Aubigne and Postel (Citation1954). The mean clinical score preoperatively was 10 (6–12).
There were 15 stovepine and 17 champagne-fluted femoral canals. In 16 femurs, the anatomy was highly deformed and they did not fit into any category. The mean anteversion of the femur was 30° (20–45). The position of the cup was planned in the true acetabulum. The CT scan showed thin bone stock in 47 acetabula and we decided to use femoral head autograft. Preoperative leg discrepancy was 23 (0.25–48) mm. In 9 hips with a high degree of dislocation, a femoral shortening was planned to avoid limb lengthening of > 3 cm, which might have led to sciatic neuropraxia.
Operative technique
THA was performed under general anesthesia in all patients. All the operations were done by the same surgeon (TX) using a posterolateral approach with the patient in a lateral position. The external rotators of the hip were maintained with sutures where possible. After exposure of the acetabulum and removal of excess labrum and capsule, reamers were used to increase its size. The cup was always placed in the true acetabulum and was fixed to the ilium with screws. The smallest cup was size 40 and the biggest 54. In 46 hips, where all patients were younger than 50 years old, a ceramic head was used—but a metallic head was in 2 other patients. The size of the head was 22 in 42 hips and 28 in 6 hips. Then a custom broach was used for impaction of cancelous bone, and the custom stem was put in place (). Intravenous cephalosporin was given before the surgery and every 8 h postoperatively, for 24 h. Low-molecular-weight heparin was given for 4 weeks postoperatively. In all patients, a cell saver and reinfusion drain was used. Indomethacin, 75 mg daily for 15 days, was given to all patients to prevent heterotopic ossification.
Postoperative rehabilitation
Patients were mobilized with physical therapy on postoperative day 1. They remained with partial weight bearing on the operative side for 6 weeks and then progressed to full weight bearing with one crutch until 3 months. Postoperatively, the patient was seen at 1.5, 3, and 6 months, and then annually with repeat radiographs. Fixation of the femoral component was assessed using the criteria of Engh et al. (Citation1990). Loosening of the acetabular component was defined as > 3 mm of migration or > 3° angulation. Heterotopic ossification was evaluated according to Brooker et al. (Citation1973). Acetabular osteolysis was classified according to DeLee and Charnley (Citation1976). Osteolysis on the femoral side was classified according to Gruen et al. (Citation1979). Pain, motion, and walking were evaluated according to D'Aubigne and Postel (Citation1954). The mean follow-up time was 69 (50–96) months. No patient was lost to follow-up.
Statistics
In the absence of a control group in our sample, we descriptively compared our data with those of previously reported series in which custom-made prostheses (Huo et al. Citation1993, Bert Citation1996) or commercially available prosthetic designs (Woolson and Harris Citation1983) had been used.
Regarding performance of the prostheses over time in our sample, we used Kaplan-Meier survival analysis. We performed 2 survival analyses, using a different definition of failure in each one. In the first approach, failure was defined as radio-graphic evidence of osteolysis (a complication that can be directly attributed to the prosthesis itself). In the second approach, failure was defined as a revision operation having been carried out. This is a conservative approach to judging the long-term performance of an implant, since surgical revision in our patients was performed due to septic loosening, which (most likely) cannot be attributed to the prosthesis itself. Participants who were not considered failures were censored on the last date of follow-up. In order to compare pain, stiffness, and walking ability before and after surgery (D'Aubigne clinical scale), we used one-sample t-test.
Results
The average time of surgery was 77 (70–110) min. The mean stay in the hospital was 8 (7–15) days. The D'Aubigne score increased ().
Outcome according to the D'Aubigne-Postel scale
The mean abduction angle of the cup was 46.03° (38–55). In 14 shallow-flat acetabula the depth was increased by breakage of the inner wall, followed by deposition of morselized bone graft, which was taken from the excised femoral head. Over an average of 4 months, it was incorporated and formed strong bone in the pelvis—which was evident on all radiographs.
In 9 patients with a high degree of dislocation, a shortening osteotomy of the femur—in 5 patients 3 cm and in 4 patients 2 cm—was done, as programmed by the preoperative planning. In 3 patients, a valgus knee deformity was corrected simultaneously. All the osteotomies had healed clinically and radiographically after an average of 4 months ().
Figure 6. A. Low CDH of the right hip and high CDH of the left hip. B. The same patient: right THA at 55 months and left THA at 65 months after surgery.
The mean postoperative leg discrepancy was 2 (0–20) mm. Preoperatively, the average length of the effective lever arm of the abductor mechanism for the affected hip was 15 (5–28) mm. This lever arm was increased to an average of 31 (27–37) mm. There was an average gain in length of this lever arm of 23 mm due to the design of the stem and lateral advancement of the greater trochanter.
None of the patients had thigh pain. There were no cases of aseptic loosening. All patients except 2 (who were 67 and 69 years old) were satisfied with the operation.
Operative problems and complications
There were 5 intraoperative complications. An undisplaced fracture of the trochanteric area occurred in 1 patient with prior valgus osteotomy. The stability of the prosthesis was secured by wiring the proximal femur. 1 patient developed a partial lesion of the peroneal part of the sciatic nerve. There was fully recovery 14 months later. In this patient, the lengthening of the limb did not exceed 2 cm. Dislocation of the operated hip occurred during the first week in one patient. Replacement with a longer head was necessary. In another patient with a very narrow and sclerotic canal, it was necessary to use an intramedullary nail as a guide of via a distal cortical window, to open the canal. This was a problem that had not been addressed preoperatively. The patient developed septic loosening 25 months later. In another patient with prior arthrodesis of the hip, an injury of the femoral vein occurred—which was repaired with no complications.
Postoperative complications
There were 6 complications postoperatively. One patient developed superficial wound infection 25 days postoperatively, which healed with oral antibiotics. There were 2 revisions for septic loosening, 25 and 40 months postoperatively. 1 patient developed heterotopic ossification of Brooker grade III 4 years postoperatively, which was removed surgically. 1 patient developed a linear osteolytic lesion in Gruen zone 6, but the stem was stable without clinical symptoms of loosening. There was 1 cup revision due to mechanical failure (breakage of the hook).
Radiographically, all patients except one with an osteolytic lesion appeared to have stable bony ingrowth with no signs of instability (reactive lines, calcar atrophy, or interface deterioration) (Engh et al. Citation1990).
Survival analysis
When failure was defined as possible acetabular and femoral radiographic loosening, there was 1 failure at 30 months; mean survival was 95 months (95% CI; 92–97). Probability of failure-free survival was 98% at 30 months. When failure was defined as revision of the femoral prosthesis, there were 2 failures: 2 revisions due to septic loosening 25 and 46 months after surgery; mean survival was 94 months (95% CI: 90–97). Probability of failure-free survival was 98% at 25 months and 96% at 46 months.
Discussion
Several experimental studies have indicated that a close geometric fit between an uncemented stem and the endosteal bone of the proximal femur is essential for physiological transfer of load and mechanical stability (Hua and Walker Citation1995). Examination of the size and the geometry of 200 cadaver femurs showed that the shape of the proximal femoral canal is very variable; in fact, more variable than most contemporary designs of femoral component can accommodate (Noble et al. Citation1988). In the face of this variability, line-to-line or surface-to-surface contact cannot be expected between uncemented implants and much of the endosteal surface. A gap of 0.35 mm or more may hamper the bridging of trabecular bone to the implant surface, and micromotions in the range of 150–500 μ induce a fibrous layer around titanium alloy prostheses and reduce the mechanical stability of the implant (Pilliar et al. Citation1986). To accommodate the great variability in the three-dimensional shape of the femoral canal, custom femoral stems have been designed. The rationale for such prostheses is to fit the prosthesis to the femur rather than shaping the femur to fit the prosthesis (Bargar Citation1989).
Two factors led us to use cementless and custom implants: the high rate of loosening of cemented implants in young patients (Dorr et al. Citation1983, Davlin et al. Citation1990) and the fact that suitable cementless stems have been unavailable for these severely deformed femurs. Our main concern was to achieve the optimal proximal fit on the metaphy-seal cortex and the prosthesis in the center of the femoral canal. One option for cementless femoral implants for these deformed hips would be the modular stems. These implants have shown very good results in complex revisions involving severe bone deficiency (Bono et al. Citation2000). However, the fretting in modular connections and the proximal stress shielding is of great concern (Bobyn et al. Citation1994). In searching the literature in English, we have not found any studies examining the modular implant in congenital hip dysplasia. Moreover, in 28 of our patients the femur size was too small for a modular implant. We therefore decided to reproduce and follow the anatomy by designing the femoral implant according to the preoperative planning.
Our study does have some limitations. It is not a randomized clinical trial, and a longer follow-up—at least 10 years—is necessary for evaluation of implant fixation (Murray et al. Citation1995). We do, however, believe that due to the severe deformed anatomy it would be impractical to design a randomized trial, and we have not found any studies of custom implants with 10 years of follow-up.
We planned the reconstruction with cementless implants with the use of CT scanning and CAD/CAM studies. CT imaging and 3D reconstruction of the femoral canal have been used by several research groups during the past 15 years (Bargar Citation1989, Xenakis et al. Citation1996). When using cementless acetabular components, CT is used to show the size of the socket—especially in the anteroposterior plane. In our study, CT showed that bone grafting was necessary in 47 cases. In 10 cases with inadequate depth a cotyloplasty of the inner acetabular wall was performed (Hartofilakidis et al. Citation1996) due to inadequate depth. We consider it to be a good choice, with good initial stability. The special cups with the hook for anchorage in the obturator foramen gave good initial stability and automatically indicated the center of rotation at the place that had been determined in the preoperative planning. There was only 1 loosening, due to mechanical failure (breakage of the hook).
The size, the design of the implants, and the position of implantation were selected and aided by the computer simulation, and not empirically during surgery. One problem with these deformed femurs was the increased anteversion: 30° (20–45). Data provided by CT in designing of the stem included the anteversion of the femur, and it was not necessary to use a modular neck (Gorski Citation1988) or perform an osteotomy of the upper femur (Holtgrewe and Hungerford Citation1989, Paavilainen et al. Citation1990) for the proximal fitting. Also, reproduction of the anatomy with the custom implants was favorable for the abductor lever arm and it was not necessary to use lateralized liners to restore the offset.
A shortening osteotomy of the femur was planned in 9 patients to avoid lengthening, which may affect the sciatic nerve if more than 3 cm. In contrast to other authors (Reikeraas et al. Citation1996), we prefer to perform the osteotomy more distally than the prosthesis. We are aware of the stress area between the plate and the implant; however, the results of this technique are very favorable. A sub-trochanteric osteotomy may cause nonunion, loosening, and nerve injuries (Paavilainen et al. Citation1990, Citation1993). The only drawback with the distal femoral osteotomy is that it entails surgery at another site, with additional fixation.
Clinical outcomes regarding pain, mobility, and walking have been positive in some studies using custom femoral prostheses with cement (Huo et al. Citation1993), but other authors have reported no significant improvement in either pain, mobility, or walking (Woolson and Harris Citation1983, Bert Citation1996). The clinical outcomes were good in our patients. There were only 2 patients with low postoperative scores, and they were the oldest patients (67 and 69 years old).
The technical difficulties associated with total hip replacement in the dysplastic hip have been well emphasized (Crowe et al. Citation1979, Hartofilakidis et al. Citation1996). In our series of 48 hips, there were 5 intraoperative complications and 6 postoperative complications. In studies with cemented customized components or cemented small components, the rate of complications was similar (Woolson and Harris Citation1983, Huo et al. Citation1993). The age, sex, diagnosis, follow-up, height, and weight of the patients in these studies were similar to those of our patients.
Contributions of authors
PK: main author of the manuscript, which was also his thesis. KS: collected the data. TS: reviewed the manuscript and made corrections to the paper. TX: the senior surgeon for these patients, and also reviewed the manuscript.
- Bargar W L. Shape the implant to the patient. A rationale for the use of custom-fit cementless total hip implants. Clin Orthop 1989, 249: 73–8
- Bert J M. Custom total hip arthroplasty. J Arthroplasty 1996; 11(8)905–15
- Bobyn J D, Tanzer M, Krygier J J, Dujovne A R, Brooks C E. Concerns with modularity in total hip arthroplasty. Clin Orthop 1994, 298: 27–36
- Bono J V, McCarthy J C, Lee J, Carangelo R J, Turner R H. Fixation with a modular stem in revision total hip arthroplasty. Instr Course Lect 2000; 49: 131–9
- Brooker A F, Bowerman J W, Robinson R A, Riley L H, Jr. Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg (Am) 1973; 55(8)1629–32
- Crowe J F, Mani V J, Ranawat C S. Total hip replacement in congenital dislocation and dysplasia of the hip. J Bone Joint Surg (Am) 1979; 61(1)15–23
- D'Aubigne R M, Postel M. Function al results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg (Am) 1954; 36(3)451–75
- Davlin L B, Amstutz H C, Tooke S M, Dorey F J, Nasser S. Treatment of osteoarthrosis secondary to congenital dislocation of the hip. Primary cemented surface replacement compared with conventional total hip replacement. J Bone Joint Surg (Am) 1990; 72(7)1035–42
- DeLee J G, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop 1976, 121: 20–32
- Dorr L D, Takei G K, Conaty J P. Total hip arthroplasties in patients less than forty-five years old. J Bone Joint Surg (Am) 1983; 65(4)474–9
- Engh C A, Massin P, Suthers K E. Roentgenographic assessment of the biologic fixation of porous-surfaced femoral components. Clin Orthop 1990, 257: 107–28
- Gorski J M. Modular noncemented total hip arthroplasty for congenital dislocation of the hip. Case report and design rationale. Clin Orthop 1988, 228: 110–6
- Gruen T A, McNeice G M, Amstutz H C. "Modes of failure" of cemented stem-type femoral components: a radio-graphic analysis of loosening. Clin Orthop 1979, 141: 17–27
- Hartofilakidis G, Stamos K, Karachalios T, Ioannidis T T, Zacharakis N. Congenital hip disease in adults. Classification of acetabular deficiencies and operative treatment with acetabuloplasty combined with total hip arthroplasty. J Bone Joint Surg (Am) 1996; 78(5)683–92
- Holtgrewe J L, Hungerford D S. Primary and revision total hip replacement without cement and with associated femoral osteotomy. J Bone Joint Surg (Am) 1989; 71(10)1487–95
- Hua J, Walker P S. Closeness of fit of uncemented stems improves the strain distribution in the femur. J Orthop Res 1995; 13(3)339–46
- Huo M H, Salvati E A, Lieberman J R, et al. Custom-designed femoral prostheses in total hip arthroplasty done with cement for severe dysplasia of the hip. J Bone Joint Surg (Am) 1993; 75(10)1497–504
- Muller M E. Lessons of 30 years of total hip arthroplasty. Clin Orthop 1992, 274: 12–21
- Murray D W, Carr A J, Bulstrode C J. Which primary total hip replacement?. J Bone Joint Surg (Br) 1995; 77(4)520–7
- Noble P C, Alexander J W, Lindahl L J, Yew D T, Granberry W M, Tullos H S. The anatomic basis of femoral component design. Clin Orthop 1988, 235: 148–65
- Paavilainen T, Hoikka V, Solonen K A. Cementless total replacement for severely dysplastic or dislocated hips. J Bone Joint Surg (Br) 1990; 72(2)205–11
- Paavilainen T, Hoikka V, Paavolainen P. Cementless total hip arthroplasty for congenitally dislocated or dysplastic hips. Technique for replacement with a straight femoral component. Clin Orthop 1993, 297: 71–81
- Pilliar R M, Lee J M, Maniatopoulos C. Observations on the effect of movement on bone ingrowth into porous-surfaced implants. Clin Orthop 1986, 208: 108–13
- Reikeraas O, Lereim P, Gabor I, Gunderson R, Bjerkreim I. Femoral shortening in total arthroplasty for completely dislocated hips: 3–7 year results in 25 cases. Acta Orthop Scand 1996; 67(1)33–6
- Woolson S T, Harris W H. Complex total hip replacement for dysplastic or hypoplastic hips using miniature or microminiature components. J Bone Joint Surg (Am) 1983; 65(8)1099–108
- Xenakis T A, Gelalis I D, Koukoubis T D, Soucacos P N, Vartziotis K, Kontoyiannis D, Tatsis C. Neglected congenital dislocation of the hip. Role of computed tomography and computer-aided design for total hip arthroplasty. J Arthroplasty 1996; 11(8)893–8