Abstract
Background and purpose Hip replacement using a hemiarthroplasty is a common surgical procedure in elderly patients with fractures of the femoral neck. The optimal surgical approach regarding the risk of dislocation is controversial. We analyzed factors influencing the stability of the hemiarthroplasty, with special regard to the surgical approach.
Patients and methods We studied 720 consecutive patients on whom 739 hemiarthroplasties were performed between 1996 and 2003, either as a primary operation for a displaced fracture of the femoral neck or as a secondary procedure after failed internal fixation of a fracture of the femoral neck. Logistic regression analyses were performed in order to evaluate factors associated with prosthetic dislocation.
Results The multivariate regression analysis showed that the posterolateral approach was the only factor associated with a significantly increased risk of dislocation: OR 3.9 (CI: 1.6–10) for the posterolateral approach with posterior repair and OR 6.9 (CI: 2.6–19) for the posterolateral approach without posterior repair. Age, sex, indication for surgery, the surgeon's experience, and type of HA had no statistically significant effect on the dislocation rate.
Interpretation Compared to the anterolateral approach, the posterolateral approach was associated with a significantly increased risk of dislocation in patients with femoral neck fractures treated with HA. A posterior repair appears to reduce the rate of dislocation, although not to the same low level as in patients operated using the anterolateral approach.
Hip replacement using a hemiarthroplasty (HA) is a common surgical procedure in elderly patients with fractures of the femoral neck, either as a primary operation for displaced fractures or as a secondary procedure after failed internal fixation (IF). Dislocation of the prosthesis is relatively rare, but causes substantial morbidity and may contribute to an increased mortality rate (Blewitt and Morti-more Citation1992). The main surgical approaches to the hip are either anterolateral (Hardinge Citation1982) or posterolateral (Moore Citation1957). The posterior approach can be performed with or without re-attachment of the short external rotators and the posterior joint capsule (posterior repair). A reduced incidence of dislocation after posterior repair has been reported (Ko et al. Citation2001).
The question of optimal surgical approach and its influence on the stability of the HA remains controversial. A recent Cochrane review (Parker and Pervez Citation2002) found only one randomized controlled trial (RCT). In that study, which involved 114 patients with a femoral neck fracture treated with a cemented Thompson prosthesis, Sikorski and Barrington (Citation1981) compared complications and mortality of patients operated on by the anterolateral or the posterolateral approach. Owing to the quality of information obtained from this single trial, the reviewers were not able to draw any conclusion regarding the optimal surgical approach.
This particular issue is difficult to evaluate in the context of a conventional RCT, as most surgeons have their individual preference regarding the surgical approach. The second best method of dealing with this question is probably randomization by surgeon or a large prospective cohort trial in which the surgical approach used is the treating surgeon's own preference.
In the context of a prospective cohort trial, we investigated the factors influencing the stability of an HA with special regard to the surgical approach. The null hypothesis used was that the surgical approach has no influence on the stability of the HA.
Patients and methods
All patients operated on in our department since 1996 have been registered in a clinical audit in which all major complications during the first 6 weeks after surgery were recorded and validated. From the audit, we identified 739 consecutive HAs performed due to a non-pathological femoral neck fracture in 720 patients between 1996 and 2003. In order to identify all patients with a dislocation of their HA, the records for these patients were searched from the date of surgery until 2005, or if the patient had died earlier, until the date of death. Finally, by using the Swedish personal identification number we searched the National Board of Health and Welfare's national registry to find any patients who had possibly been treated for dislocation of their HA at another Swedish hospital. No such cases were found. The median follow-up time, including patients who had died during follow-up, was 2.3 (0–10) years.
Baseline data for all patients included, also in relation to the surgical approach, are given in . The mean age was 84 (54–103) years for women (n = 592) and 82 (55–97) years for men (n = 147). An anterolateral surgical approach was used for 431 hips and a posterolateral approach for 308 hips. A posterior repair was performed in 176 of these 308 hips (57%). Information regarding whether a posterior repair had been performed was lacking for 3 patients. Posterior repair was defined as a repair of the short external rotators with or without a simultaneous repair of the posterior capsule. The indication for the HA procedure was a displaced femoral neck fracture (Garden III and IV) (Garden Citation1961) in 457 patients (primary HA) and revision surgery after failed IF of a femoral neck fracture in 282 patients (secondary HA). The number of surgeons was 59, and the surgeon was a certified specialist in orthopedic surgery (post-registrar or consultant) for 604 hips and a registrar for 135 hips. The prostheses used were an uncemented Unipolar HA (Austin-Moore; dePuy/Johnson-Johnson, Sollen-tuna, Sweden) in 389 hips, a cemented Unipolar (Exeter Unipolar; Howmedica, Malmö, Sweden) in 127, and a cemented Bipolar (Exeter Bipolar; Howmedica) in 223. In all patients with a bipolar HA, a 28-mm head with a Bicentric (Howmedica) or a Universal Head Replacement (UHR; Howmedica) was used.
Table 1. Baseline data for all patients included, in relation to surgical approach (n = 739)
During the study period, we did not routinely use any validated instrument for assessment of cognitive function. For most of the patients, however, there was information regarding cognitive function or dementia in the patient's records, based on the physician's subjective assessment.
Comparing patients operated on using the anterolateral or the posterolateral approach, there were no differences regarding age or sex. However, the anterolateral approach was used more often in primary HAs (p < 0.001), by inexperienced surgeons (p < 0.001), and in cemented HAs (p < 0.001). The explanation for these variations was probably that the Austin Moore HA and the posterolateral approach were the most commonly used during the initial phase of the study period. As a result of published reports regarding the use of cemented implants (Parker and Gurusamy Citation2006) and our own experience regarding surgical approach (Tidermark et al. Citation2003, Blomfeldt et al. Citation2005), we gradually changed over to the use of cemented HAs and the anterolateral approach during the latter phase of the study period. At each point in time, however, the selection of the surgical approach was determined by the surgeon's own preference.
Statistics
The statistical software used was SPSS 15.0 for Windows. The Mann-Whitney U-test was used for scale variables in independent groups. Nominal variables were tested by the Chi-square test or Fisher's exact test. All tests were two-sided. Logistic regression analyses were performed in order to evaluate factors associated with prosthetic dislocation. Age, sex, indication for surgery, the surgeon's experience, type of HA, and surgical approach were tested as independent variables in the model. First, crude associations for each variable were studied in a univariate model. Secondly, a multivariate model was used to study the adjusted associations. The associations are presented as odds ratios (ORs) with 95% confidence intervals (CIs). The results were considered significant at p < 0.05.
Results
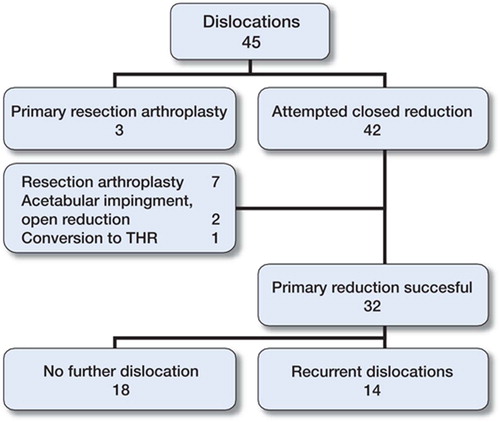
Dislocation of the HA occurred in 45 of 739 hips (6%). The anterolateral approach was associated with a lower risk of dislocation compared to the posterolateral approach with or without posterior repair (3.0%, 8.5%, and 13%, respectively) (p < 0.001) (). There was a trend toward less frequent dislocations in older patients and in Unipolar HAs. The sex of the patient, the indication for surgery, and the experience of the surgeon had no influence on the dislocation rate.
Table 2. Incidence of prosthetic dislocations
Information regarding cognitive function and/or dementia based on the physician's subjective assessment was available for 598 patients. Based on these data, there was no selection bias based on cognitive function to any of the surgical approaches. Of the patients operated with the anterolateral approach, 93 of 419 (22%) were assessed as having some degree of cognitive dysfunction or dementia, as compared to 43 of 179 (24%) who were operated with the posterolateral approach (p = 0.7). As expected, the dislocation rate was higher in patients with cognitive dysfunction or dementia than in those without: 14/136 (10%) and 19/462 (4%), respectively (p = 0.009). Due to the fact that the data were incomplete and based on a subjective assessment, we did not include cognitive function as a variable in the regression analyses.
Since the anterolateral approach was used more often in primary HAs, and also by inexperienced surgeons and in the cemented HAs, logistic regression analyses were performed in order to evaluate factors of importance for dislocation (). The univariate analyses indicated a significantly increased risk of dislocations in hips operated on using the posterolateral approach with or without posterior repair, and a decreased risk in cemented Unipolar HAs. The multivariate regression analysis showed that the posterolateral approach was the only factor associated with a significantly increased risk of dislocation: OR3.9 (CI 1.6–10) forthepos-terolateral approach with posterior repair and OR 6.9 (CI 2.6–19) for the posterolateral approach without posterior repair. The age, sex, indication for surgery, the surgeon's experience, and type of HA had no statistically significant effect on the dislocation rate.
Table 3. Logistic regression to evaluate factors associated with prosthetic dislocation (n = 739, except in the univariate analysis of surgical approaches and all multivariate analyses due to 3 missing values regarding information on posterior repair)
The first dislocation occurred early (within 6 weeks) in 39 patients and late in 6 patients. All late dislocations were in patients who had been operated by the posterolateral approach. In 42 patients of 45, an attempted closed reduction was performed after the first dislocation (). In the remaining 3 patients, all with severe dementia, the uncemented Austin-Moore prosthesis was removed without an attempt at reduction. The primary closed reduction was successful in 32/42 hips. Of the remaining 10 hips, 7 uncemented Austin-Moore HAs were extracted in patients with severe dementia, some non-ambulant, due to instability or irreducibility. 2 hips showed incongruence of the joint on the post-reduction radiograph due to acetabular impingement (soft tissue and cement, respectively) and both underwent open reduction. None of these patients had any further dislocation. Finally, 1 hip showed severe instability during the reduction procedure, which was considered to be caused by a shallow acetabular socket. This arthroplasty was converted to a THR. Consequently, 34 of the 45 hips remained with the prosthesis in situ after the primary dislocation, including the 2 that had undergone open reduction (see above). Of these, 14 had recurrent dislocations. There were no dissociations of the cemented Bipolar HAs during the study period.
Comparing patients who were operated through the anterolateral or posterolateral approach, there were no differences regarding general complications, i.e. cardiovascular, thromboembolic, or cere-brovascular complications, pneumonia, or death within the first 6 weeks (data not shown).
Discussion
This prospective cohort study strongly indicates that a posterolateral surgical approach, as compared to an anterolateral one, carries a significantly increased risk of prosthetic dislocation in patients with fractures of the femoral neck, while other factors such as age, sex, indication for surgery, the surgeon's experience, and type of HA do not appear to affect the dislocation rate. As compared to the anterolateral approach, the risk of dislocation was markedly increased after a posterolateral approach, both without posterior repair (OR 6.9) and with posterior repair (OR 3.9).
In the only previously published RCT on this issue, Sikorski and Barrington (Citation1981) concluded that the anterolateral approach was the safest operation when performing HA in patients with fractures of the femoral neck. However, their conclusion was based on the finding of an increased mortality rate in patients who had been operated with the posterolateral approach, and not by differences in dislocation rate. A recent critical review of their study has questioned the validity of these conclusions (Parker and Pervez Citation2002).
Our finding of an increased dislocation rate after the posterolateral approach is in accordance with the results of previous non-randomized trials. In a prospective study involving 531 patients, Keene and Parker (Citation1993) reported an increased dislocation rate using the posterolateral approach. However, they also reported a longer operating time and an increased infection rate and blood loss using the anterior approach. The conclusion drawn by Keene and Parker was that the favored approach should be according to the surgeon's preference. In a systematic review of the literature, Varley and Parker (Citation2004) reported a higher dislocation rate using the posterior approach than with the anterior one, 5.1% as opposed to 2.4%. Finally, in a retrospective study, Pajarinen et al. (Citation2003) reported a dislocation rate of 16% using the posterior approach as compared to 7% using the anterior approach in 338 patients treated with a Thomson HA.
Our results indicate that a posterior repair may reduce the dislocation rate after a posterolateral approach, although the difference did not reach statistical significance. In a retrospective review, Ko et al. (Citation2001) compared the dislocation rate for 1,483 patients operated on through the posterior approach without posterior repair between 1986 and 1997 with 205 patients operated with posterior repair between 1998 and 1999. A posterior approach with re-attachment of the capsule and the external rotators seemed to reduce the dislocation rate from 1.9% to zero. However, in the former group 19% of the patients were excluded due to incomplete records and inadequate follow-up, and in the latter group the posterior repair procedure was performed or supervised by two of the authors with special interest in hip arthroplasty surgery. These circumstances may reduce the generaliz-ability of the results of that study, a notion that is supported by the remarkably low dislocation rate compared to previous studies (Pajarinen et al. Citation2003, Varley and Parker Citation2004). Moreover, no other factors of potential importance for increased risk of dislocation such as age, sex, indication for surgery, the surgeon's experience, and type of prosthesis were included in the analysis.
We did not find an increased dislocation rate in secondary HAs. This finding is in contrast to that in a previous report from a non-randomized study by Roberts and Parker (Citation2002) on patients treated with an Austin-Moore HA. There are no obvious reasons why a secondary HA should have an increased dislocation rate. On the one hand, the surgical procedure during a secondary HA operation is often more technically demanding. Also, these patients have often suffered a long period of time with pain and disability before the secondary HA, probably resulting in poor muscle function. On the other hand, secondary HA is usually an elective procedure with an optimized patient. Moreover, the stiff joint capsule developed during the often long time to failure of the internal fixation may also reduce the risk of instability to values comparable to those of patients with a degenerative joint disease.
Surprisingly, the experience of the surgeons did not significantly affect the risk of dislocation. This may be partly explained by the fact that the registrars in our study were routinely assisted by a senior orthopedic surgeon when performing the HA procedure. The experience of the surgeon may be more important in a THR procedure, where the critical and more difficult part of the procedure with regard to stability is to position the acetabular component optimally.
The univariate analysis indicated a lower dislocation rate for the cemented unipolar HA. However, the posterior approach was used less often with this particular prosthesis and the multivariate analysis did not show any difference in dislocation rates between the different prosthetic designs.
Prosthetic dissociation—i.e. an inter-prosthetic dislocation—may be a problem in dislocations in patients with bipolar HAs, necessitating an open reduction and thereby introducing an added surgical risk, including infection. Varley and Parker (Citation2004) reported that 12% of all dislocations in bipolar HAs were dissociations. We found no dissociations with the Exeter bipolar prosthesis used in our study.
In patients with their prosthesis in situ after the primary dislocation, 14 of 34 suffered recurrent dislocations. This finding is in agreement with the re-dislocation rate of 50% reported by Blewitt and Mortimer (Citation1992). The high rate of re-dislocations necessitating repeated closed reductions or open revision surgery may be one explanation for the high mortality rate previously reported (Blewitt and Mortimore Citation1992, Keene and Parker Citation1993).
One limitation of our study was the lack of a pre-operative assessment of cognitive function based on a validated instrument. Cognitive dysfunction appears to be a significant risk factor for dislocation in hip fracture patients treated with a primary THR (Johansson et al. Citation2000), but its influence on the dislocation rate after a primary HA has not been properly evaluated. As expected, cognitive dysfunction or dementia was also a significant risk factor for dislocation in hip fracture patients treated with an HA. However, according to data from patients' records based on the physician's subjective assessment, there did not appear to be any selection bias of patients with cognitive dysfunction or dementia to any of the surgical approaches.
The strengths of our study were the large number of consecutively included patients, the relatively long follow-up time, and the validation of data on dislocation via the national registry of the National Board of Health and Welfare. Thus, we believe that our conclusion regarding the risk factors for dislocation that we studied is valid for other populations also.
No competing interests declared.
Contributions of authors
AE and LJL: study design, data collection and analysis, and preparation of the manuscript; JT: study design, data analysis, and preparation of the manuscript; HT: study design and preparation of the manuscript.
- Blewitt N, Mortimore S. Outcome of dislocation after hemi-arthroplasty for fractured neck of the femur. Injury 1992; 23(5)320–2
- Blomfeldt R, Törnkvist H, Ponzer S, Söderqvist A, Tidermark J. Internal fixation versus hemiarthroplasty for displaced fractures of the femoral neck in elderly patients with severe cognitive impairment. J Bone Joint Surg (Br) 2005; 87(4)523–9
- Garden R S. Low-angle fixation in fractures of the femoral neck. Journal of Bone and Joint Surgery (Br) 1961; 43(4)647–53
- Hardinge K. The direct lateral approach to the hip. J Bone Joint Surg (Br) 1982; 64(1)17–9
- Johansson T, Jacobsson S A, Ivarsson I, Knutsson A, Wahlström O. Internal fixation versus total hip arthroplasty in the treatment of displaced femoral neck fractures: a prospective randomized study of 100 hips. Acta Orthop Scand 2000; 71(6)597–602
- Keene G S, Parker M J. Hemiarthroplasty of the hip - the anterior or posterior approach? A comparison of surgical approaches. Injury 1993; 24(9)611–3
- Ko C K, Law S W, Chiu K H. Enhanced soft tissue repair using locking loop stitch after posterior approach for hip hemiarthroplasty. J Arthroplasty 2001; 16(2)207–11
- Moore A T. The self-locking metal hip prosthesis. J Bone Joint Surg (Am) 1957; 39(4)811–27
- Pajarinen J, Savolainen V, Tulikoura I, Lindahl J, Hirvensalo E. Factors predisposing to dislocation of the Thompson hemiarthroplasty: 22 dislocations in 338 patients. Acta Orthop Scand 2003; 74(1)45–8
- Parker M J, Pervez H. Surgical approaches for inserting hemiarthroplasty of the hip. Cochrane Database of Systematic Reviews 2002, Issue 3, Art. No.: CD001707. DOI: 10.1002/14651858.CD001707
- Parker M J, Gurusamy K. Arthroplasties (with and without bone cement) for proximal femoral fractures in adults. Cochrane Database of Systematic Reviews 2006, Issue 3, Art. No.: CD001706. DOI: 10.1002/14651858. CD001706.pub3
- Roberts C, Parker M J. Austin-Moore hemiarthroplasty for failed osteosynthesis of intracapsular proximal femoral fractures. Injury 2002; 33(5)423–6
- Sikorski J M, Barrington R. Internal fixation versus hemiarthroplasty for the displaced subcapital fracture of the femur. A prospective randomised study. J Bone Joint Surg (Br) 1981; 63(3)357–61
- Tidermark J, Ponzer S, Svensson O, Söderqvist A, Törnkvist H. Internal fixation compared with total hip replacement for displaced femoral neck fractures in the elderly. A randomised, controlled trial. J Bone Joint Surg (Br) 2003; 85(3)380–8
- Varley J, Parker M J. Stability of hip hemiarthroplasties. Int Orthop 2004; 28(5)274–7