Abstract
Background and purpose Malunion after a distal radius fracture can be treated with an osteotomy of the distal radius. Often autologous iliac crest bone graft is used to fill the gap, but this is associated with donor site morbidity. Instead of bone graft, we have used a slow-resorbing bone substitute in combination with a minimally invasive fixation technique.
Patients and methods 25 consecutive patients with a dorsal malunion after a distal radius fracture underwent an osteotomy. A TriMed buttress pin and a radial pin plate were used for fixation, and Norian SRS as bone substitute. The patients were followed for a minimum of 1 year and range of motion, grip strength, DASH scores, and the radiographic correction were measured.
Results Forearm rotation improved from 137° to 155°, flexion/extension from 102° to 120°, and radioul-nar deviation from 32° to 43°. Grip strength increased from 62% of the contralateral hand to 82%. DASH scores decreased from 36 to 23. Radiographically, all osteotomies but 1 healed and the radiographic correction achieved was consistent over the first year.
Interpretation Osteotomy of the distal radius is effective in increasing motion and grip strength after a malunited distal radial fracture. Patient satisfaction is high and subjective results measured with DASH are good. Using a bone substitute, the operation can be performed as an outpatient procedure and donor-site pain avoided. No loss of the radiographic correction achieved was noted during osteotomy healing.
Distal radial fractures are common, with an annual incidence of 25 per 10,000 inhabitants (Robertsson et al. Citation1990). Most patients heal and have restored function but almost one-fifth suffer from residual symptoms such as pain, nerve symptoms, and disability after 1 year (MacDermid et al. Citation2003). Malunion is a major cause of residual symptoms and appears in about 5% of the fractures (Cooney et al Citation1980). Any malunion that results in an incongruity of the distal radio ulnar joint may lead to ulnar side pain and reduced forearm rotation (af Ekenstam and Hagert Citation1985, Bronstein et al. Citation1997). The patients may suffer from reduced grip strength, poor hand and arm function, and from a poor cosmetic appearance. To correct the deformity and thereby relieve the symptoms, an osteotomy can be performed (Fernandez Citation1982, Trousdale and Linscheid Citation1995, Prommersberger et al. Citation2002, Van Cauwelaert de Wyels and De Smet Citation2003). The healed fracture is cut at the fracture site and length and/or angle is corrected by using an opening-wedge technique. An iliac crest bone graft is often used to fill the gap, either as a single block of cortico-cancellous bone or just as a non-structural cancellous graft (Ring et al. CitationA>2002). A high incidence of donor site morbidity has been reported (Arrington et al. Citation1996, Silber et al. Citation2003), most commonly in the form of pain but also as wound infection or fracture of the iliac crest (Arrington et al. Citation1996).
To avoid donor site morbidity, a bone substitute can be used instead of bone grafting. Norian SRS is an injectable calcium phosphate paste that sets to carbonated hydroxyapatite in situ. It has been used previously, mainly in surgery for distal radial fractures (Kopylov et al. Citation1996) but also for osteotomies of malunited distal radial fractures (Luchetti Citation2004).
We evaluated the safety of using a bone substitute as gap filler in combination with a stable but still minimally invasive fixation technique.
Patients and methods
Since 2002, all patients undergoing an osteotomy of the distal radius at our department have been followed prospectively regarding expectations, range of motion, and DASH scores. 25 patients with a malunion and a dorsal malposition after a distal radial fracture underwent an osteotomy between November 2002 and October 2005 with the TriMed system and Norian SRS. During this period, 12 other patients were operated but not included in the study. Of these, 3 were operated using a dorsal AO plate and bone graft from the iliac crest, 3 were operated using Norian SRS and a dorsal AO plate, 4 patients had volarly displaced malunions, and 2 patients underwent intraarticu-lar osteotomies. The mean age in the study group was 52 (25–74) years, and 9 patients were men and 16 women. 7 patients were retired; 10 rated their work as light and 8 rated it as heavy manual work. The operations were performed 16 months (range 3–33) after the initial fracture, except for 1 patient who was operated 10 years after the initial injury. 11 patients were operated on their dominant wrist.
An occupational therapist interviewed and examined the patients preoperatively, and at 3 and 12 months postoperatively. Range of motion was measured using a goniometer for flexion/extension, ulnar/radial deviation, and pronation/supination. Grip strength was measured using a dynamometer (Jamar; Preston Corp, Jackson, MI). The patients rated their pain at activity and at rest on a 10-cm visual analog scale (VAS) and the functional outcome was evaluated using the Swedish version of the DASH (Atroshi et al. Citation2000). Preoperatively, a protocol was filled in where the patients noted their expectations of the outcome of the surgery in a 5-grade Likert scale regarding pain, function, mobility, and cosmetic appearance.
Radiographs were taken preoperatively, postoperatively, and at follow-up after 1 year—except for 1 patient who was lost to follow-up and had her last radiograph at 3 months postoperatively. 2 patients could not be included in the prospective protocol, were identified later, and had their follow-up radiographs taken 4 years postoperatively. A radiologist (MG) performed all radiograph measurements. Radial shortening was measured as ulnar variance from the distal radial surface to the distal ulnar surface, according to the method of perpendiculars on AP radiographs of the wrist obtained in the neutral position. The radial inclination angle was measured on the AP radiographs and the dorsal angula-tion on the lateral view, expressed as the angle of joint surface relative to the length of the radial axis (Mann et al. Citation1992).
Operative technique
All osteotomies were operated using the TriMed system for fixation and Norian SRS as the gap filler. The TriMed system is a fragment-specific fixation device for distal radial fractures consisting of plates and pins. In the current osteotomy technique, a radial pin plate and a dorsal buttress pin were used ( and ). Norian SRS (Synthes GmbH, Switzerland) is a non-or slowly resorbing bone substitute and consists of calcium phosphate. It is mixed to a paste suitable for injection into the gap and sets to carbonated hydroxyapatite after 10 min in situ. The resistance to compressive forces exceeds 10 MPa initially and increases to 55 MPa after 12 h (Kopylov Citation2001), which is superior to cancellous bone but inferior to cortical bone.
Figure 1. A. Dorsal buttress pin with washer and bicortical screw. B. Radial pin plate with pins and screws. C. Preoperative radiograph. D. The fixation device and the bone substitute in place.
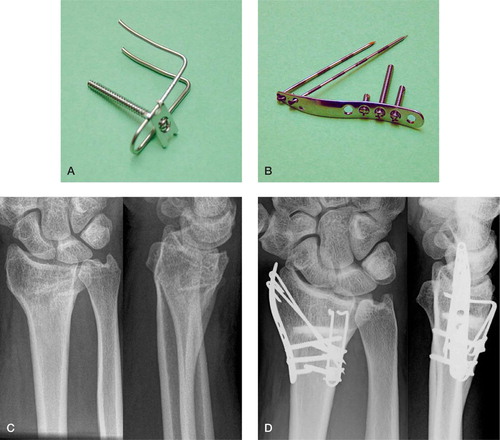
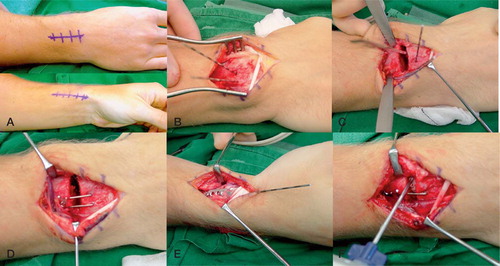
Figure 2 A. The operation was carried out with the arm in a prone position. 2 short incisions were made, one radially through the first extensor compartment and a second dorsal incision through the fourth compartment. B. The joint line was marked with 2 parallel pins into the distal radius and the holes were later used for the dorsal buttress pin. C. The osteotomy was then performed with an oscillating saw and the malposition reduced. A temporary fixation was achieved by a pin driven through the radial styloid and into the radius, proximal to the osteotomy, thereby bridging the osteotomy. D. When optimal positioning was accomplished, the fixation was secured by the dorsal buttress pin and the radial pin plate (E). F. Norian SRS was injected into the bone defect and left to harden as the extensor retinaculum and skin were closed. A bulky dressing and a dorsal cast completed the operation.
Postoperatively, the wrists were immobilized in a plaster cast for 2 weeks and thereafter active mobilization was encouraged in a removable soft splint.
Statistics
Student's paired t-test was used to compare pre-and postoperative data and also to evaluate radio-graphic changes within the first year. For comparison of pre-and postoperative DASH scores and pain scores, Wilcoxon's signed-rank sum test was used. SPSS software version 14.0 was used.
Results
The mean operation time was 88 (57–144) min. All patients but one were admitted as outpatients and 18 of the 25 patients could return home the same day; the others returned home the morning after. 2 patients never came to the intended pre-and postoperative evaluations done by the occupational therapists, and were followed only by their surgeon. For these 2 patients, some data could be extracted from the medical records and used for analysis regarding range of motion and grip strength at 3 months post-operatively. Final radiographs and data regarding range of motion, grip strength, and DASH in these 2 patients were not collected at the proper time— but at 4 years after the operation instead. Their final DASH scores were 0 and 7, respectively, and at the final follow up they were free of pain; but as preoperative DASH and pain scores were not recorded, their results were not part of the statistical evaluation. 1 patient had her last follow-up at 3 months and refused the final radiograph. 3 patients were missed at the 3-month follow-up but they did come to the 1-year follow-up.
1 patient underwent a reinsertion of the triangular fibro-cartilaginar complex (TFCC) at the same time as the osteotomy. 2 patients underwent an ulnar shortening osteotomy at 8 and 19 months after the osteotomy, because of persistent pain and poor range of motion. These patients were included in the final analysis. Six patients had the implant removed at an average of 13 (11–16) months after the osteotomy, and 2 other patients are scheduled for removal.
Minor complications involving transient tingling and numbness from the radial nerve branches were reported initially in 6 cases, but had disappeared by the last follow-up. 1 major complication occurred. The bone substitute fragmented before osseous union and the plate and screws were broken at 2 months postoperatively. The patient was reoperated using conventional bone grafting and fixation with a dorsal AO plate. The osteotomy healed and the patient was satisfied, and had a good clinical result at final follow-up but was excluded from the final analysis. Radiographically, all the remaining osteotomies healed and the dorsal angulation and the ulnar length relative to the radius decreased postoperatively; the improvement was consistent over time. The mean axial shortening preoperatively was 4.0 (SD 2.2) mm, and decreased to 2.6 (2.1) mm postoperatively and 2.5 (2.1) mm at the final follow-up. The mean radial inclination was 20° (9.8) preoperatively, 21° (3.7) postoperatively, and 22° (4.2) at the final follow-up. Dorsal angulation was 16° (9.8) preoperatively, −0.1° (10) postoperatively, and 0.0° (11) at the final follow-up (). At 1 year postoperatively, the range of motion was increased compared to preoperatively: in forearm rotation from 137° (32) to 155° (24), in flex ion/extension from 103° (20) to 120° (15), and in radial/ulnar deviation from 32° (14) to 43° (10). Grip strength on the uninjured side increased from 62% (18) to 82% (20) (). The mean DASH score decreased from 36 (16) to 23 (19). Pain at rest as measured on a VAS decreased from 3.9 (2.2) to 2.0 (1.6) and pain at activity from 6.3 (2.2) to 3.7 (2.4) ().
Table 1. Radiographic parameters preoperatively, postoperatively, and at final follow-up
Table 2. Objective results
Table 3. Subjective measures preoperatively, at 3 months, and at 1 year postoperatively
Patient expectations
21 of the 25 patients answered the questionnaire regarding their preoperative expectations. Preoperatively, the patients considered pain during activity and a limited range of motion in forearm rotation to be the most important symptoms to be improved by the operation, with a median rank of 4 on a 5-grade Likert scale (0 = not important; 5 = very important). Pain at rest was considered less important with a median rank of 2, and cosmetic appearance even lower with a median rank of 1. 20 patients replied at 3 months postoperatively, 10 of whom had their expectations fulfilled regarding pain at rest and 12 patients of whom had their expectations fulfilled regarding range of motion. In total, 13 patients already considered their overall expectations of the operation to have been fulfilled at 3 months. At 1 year postoperatively, all 25 patients answered. 21 patients had had their expectations fulfilled regarding pain at rest and 20 patients regarding range of motion. 20 patients considered that their overall expectations of the operation to had been fulfilled at the final follow-up.
Discussion
Norian SRS appears to be a safe alternative to bone autograft. With the use of a bone substitute we can avoid donor site problems associated with the harvest of iliac crest bone graft and in most patients the osteotomy of the distal radius can be performed as an outpatient procedure. Studies on distal radial osteotomies have seldom reported donor site problems. In one study of distal radial osteotomies, continuous pain was reported at the donor site in 1 of 20 patients but short-term problems were not mentioned (Ring et al. CitationA>2002). In spinal fusion studies focusing on donor site problems in the short term, incidences ranging from 16% to 99% and persistent pain for over 6 months in 26–41% of patients have been reported (Heary et al. Citation2002, Silber et al. Citation2003, Sasso et al. Citation2005). Donor site complications other than pain have also been reported. Major complications—defined as patients requiring a major change in treatment, prolonged hospitalization, or reoperation—have been reported in 24 of 414 patients and minor complications such as superficial infections, seromas, or minor haematomas in 41 patients (Arrington et al. Citation1996). These high complication rates may in part be explained by the large bone grafts usually used for spinal fusion surgery; however, all these problems can be avoided by using a bone substitute.
We found that in using a bone substitute instead of a bone graft, it is possible to use a minimally invasive fixation technique. It can be argued that Norian SRS takes too long, if ever, to resorb. On the other hand, resorption during the healing period that is too fast—using iliac crest bone graft or a fast resorbing bone substitute—adds a risk of loss of the correction. Faster-resorbing gap fillers make the fixation more important, and more rigid solutions necessary, which in turn reduces the bone healing response by stress shielding. However, when using a non-resorbing bone substitute such as Norian SRS, the fixation is also important. In a series of distal radius osteotomies, the non-resorbing Norian SRS was combined with pinning for fixation (Luchetti Citation2004). The correction achieved was lost during consolidation and an increased dorsal angulation of 5° compared to the value immediately postoperatively was reported after 3 years. It has been shown previously that with a rigid fixation of the osteotomy, a cancellous graft can be used instead of cortico-cancellous graft (Ring et al. CitationA>2002). In our study we had little or no secondary loss of position, except for the patient with fragmentation of the bone substitute and breakage of the fixation device. The fixation material chosen appears to be sufficiently stable and the rate of hydroxyapatite degradation is acceptable. Without being bulky, the TriMed system is more rigid than pins alone and achieves the same fixation strength as a volar angle stable plate in cadaver studies (Taylor et al. Citation2006). In the failed case, the shortest 3-hole radial pin plate (RPP) was used and we therefore use the 5-hole RPP at present as the minimal length.
Our objective results regarding mobility, increased grip strength, and pain relief are good and similar to previous studies on osteotomies of the distal radius using bone grafts (Fernandez Citation1982, Hove and Molster Citation1994, Jupiter and Ring Citation1996, Flinkkila et al. Citation2000, Prommersberger et al. Citation2002, Ring et al. CitationA>2002, Van Cauwelaert de Wyels and De Smet Citation2003). The final range of motion with an extension and flexion of 120° is on a par with previously reported series ranging from 87° (Jupiter and Ring Citation1996) to 132° (Ring et al. CitationA>2002). Also, forearm rotation of 156° is comparable with the results of other studies reporting from 145° (Jupiter and Ring Citation1996) to 173° (Flinkkila et al. Citation2000). Grip strength increased to 82% of the uninjured side, whereas in other studies it has ranged from 66% (Ring et al. CitationA>2002) to 83% (Flinkkila et al. Citation2000). Equally good results have been shown when Norian SRS has been used as bone substitute, with reduced pain, improved grip strength, and improved range of motion; however, there were only 6 patients in the study (Luchetti Citation2004).
Minor complications such as tingling from the cutaneous radial nerve branches did occur in our series, and they are related to the choice of implant and surgical exposure. These complications were all transient and had disappeared by the last follow-up. One-quarter (6/24) of our patients have had their implants removed and another 2 patients are scheduled for removal. Removal was not done routinely, but only at the patient's request.
We used DASH for subjective results, which decreased from 35 to 23 at the final follow-up. For comparison, only 1 study has reported a DASH score in distal radial osteotomies, with a mean (26) similar to ours (Van Cauwelaert de Wyels and De Smet Citation2003). These results suggest that the operation offers a substantial improvement of symptoms, but no normalization. Although 20 of the 25 patients had their expectations fulfilled by the operation after 1 year, they still experienced some problems in daily life at that time point. In the normal population, the DASH score would be at least 10–15 points lower and thus a full restoration of the symptoms was not accomplished in this study or in any other. Still, the initial fracture treatment has to be optimal but the osteotomy of the distal radius offers a good solution if malunion occurs.
No competing interests declared.
Contributions of authors
AA reviewed the literature, planned and performed the study, and wrote the manuscript. MT participated in planning and performing the study and in writing the manuscript. MG performed the radiological measurements and revised the manuscript. PK planned and performed the study and revised the manuscript.The authors wish to thank occupational therapists Margareta Wollmark and Ulrika Wijk for excellent assistance. The project was supported by Region Skåne, Lund University Hospital, the Alfred Österlund Foundation, the Greta and Johan Kock Foundation, the Crafoord Foundation, the Maggie Stephens Foundation, Swedish Research Council—Medicine (09509), Stiftelsen för Bistånd åt Rörelsehindrade i Skåne, and by the Medical Faculty of Lund University.
- af Ekenstam F, Hagert C G. The distal radio ulnar joint. The influence of geometry and ligament on simulated Colles' fracture. An experimental study. Scand J Plast Reconstr Surg 1985; 19(1)27–31
- Arrington E D, Smith W J, Chambers H G, Bucknell A L, Davino N A. Complications of iliac crest bone graft harvesting. Clin Orthop 1996, 329: 300–9
- Atroshi I, Gummesson C, Andersson B, Dahlgren E, Johansson A. The disabilities of the arm. shoulder and hand (DASH) outcome questionnaire: reliability and validity of the Swedish version evaluated in 176 patients. Acta Orthop Scand 2000; 71(6)613–8
- Bronstein A J, Trumble T E, Tencer A F. The effects of distal radius fracture malalignment on forearm rotation: a cadaveric study. J Hand Surg (Am) 1997; 22(2)258–62
- Cooney W P, 3rd, Dobyns J H, Linscheid R L. Complications of Colles' fractures. J Bone Joint Surg (Am) 1980; 62(4)613–9
- Fernandez D L. Correction of post-traumatic wrist deformity in adults by osteotomy. bone-grafting. and internal fixation. J Bone Joint Surg (Am) 1982; 64(8)1164–78
- Flinkkila T, Raatikainen T, Kaarela O, Hamalainen M. Corrective osteotomy for malunion of the distal radius. Arch Orthop Trauma Surg 2000; 120(1–2)23–6
- Heary R F, Schlenk R P, Sacchieri T A, Barone D, Brotea C. Persistent iliac crest donor site pain: independent outcome assessment. Neurosurgery 2002; 50(3)510–6, discussion 516-7
- Hove L M, Molster A O. Surgery for posttraumatic wrist deformity. Radial osteotomy and/or ulnar shortening in 16 Colles' fractures. Acta Orthop Scand 1994; 65(4)434–8
- Jupiter J B, Ring D. A comparison of early and late reconstruction of malunited fractures of the distal end of the radius. J Bone Joint Surg (Am) 1996; 78(5)739–48
- Kopylov P. Injectable calcium phosphate bone substitute in distal radial fractures. 2001, Thesis. Dept. of Orthopaedics, Lund University
- Kopylov P, Jonsson K, Thorngren K G, Aspenberg P. Injectable calcium phosphate in the treatment of distal radial fractures. J Hand Surg (Br) 1996; 21(6)768–71
- Luchetti R. Corrective osteotomy of malunited distal radius fractures using carbonated hydroxyapatite as an alternative to autogenous bone grafting. J Hand Surg (Am) 2004; 29(5)825–34
- MacDermid J C, Roth J H, Richards R S. Pain and disability reported in the year following a distal radius fracture: a cohort study. BMC Musculoskelet Disord 2003; 4(1)24
- Mann F A, Wilson A J, Gilula L A. Radiographic evaluation of the wrist: what does the hand surgeon want to know? Radiology 1992; 184(1)15–24
- Prommersberger K J, Van Schoonhoven J, Lanz U B. Outcome after corrective osteotomy for malunited fractures of the distal end of the radius. J Hand Surg (Br) 2002; 27(1)55–60
- Ring D, Roberge C, Morgan T, Jupiter J B. Osteotomy for malunited fractures of the distal radius: a comparison of structural and nonstructural autogenous bone grafts. J Hand Surg (Am) 2002; 27(2)216–22
- Robertsson G O, Jonsson G T, Sigurjonsson K. Epidemiology of distal radius fractures in Iceland in 1985. Acta Orthop Scand 1990; 61(5)457–9
- Sasso R C, LeHuec J C, Shaffrey C. Iliac crest bone graft donor site pain after anterior lumbar interbody fusion: a prospective patient satisfaction outcome assessment. J Spinal Disord Tech (Suppl 18) 2005; 77–81
- Silber J S, Anderson D G, Daffner S D, Brislin B T, Leland J M, Hilibrand A S, Vaccaro A R, Albert T J. Donor site morbidity after anterior iliac crest bone harvest for single-level anterior cervical discectomy and fusion. Spine 2003; 28(2)134–9
- Taylor K F, Parks B G, Segalman K A. Biomechanical stability of a fixed-angle volar plate versus fragment-specific fixation system: cyclic testing in a c2-type distal radius cadaver fracture model. J Hand Surg (Am) 2006; 31(3)373–81
- Trousdale R T, Linscheid R L. Operative treatment of malunited fractures of the forearm. J Bone Joint Surg (Am) 1995; 77(6)894–902
- Van Cauwelaert de Wyels J, De Smet L. Corrective osteotomy for malunion of the distal radius in young and middle-aged patients: an outcome study. Chir Main 2003; 22(2)84–9
