Abstract
Background and purpose There are limited popula-tion-based data on utilization, outcomes, and trends in total knee arthroplasty (TKA). The purpose of this study was to examine TKA utilization and short-term outcomes in a pre-paid health maintenance organization (HMO), and to determine whether rates and revision burden changed over time. We also studied whether this population is representative of the general population in California and in the United States.
Methods Using hospital utilization and membership databases from 1995 through 2004, we calculated incidence rates (IRs) of primary and revision TKA for every 10,000 health plan members. The demographics of the HMO population were compared to published census data from California and the United States.
Results The age and sex distributions of the study population were similar to those of the general population in California and the United States. 15,943 primary TKAs and 1,137 revision TKAs were performed during the 10-year period. Patients below the age of 65 accounted for one-third of all primary replacements and one-third of all revision replacements. IRs of primary TKAs increased from 6.3 per 10,000 in 1995 to 11.0 per 10,000 in 2004, at a rate of 5% per year (p<0.001). IRs of revision TKAs increased from 0.41 per 10,000 in 1995 to 0.74 per 10,000 in 2004 (p=0.4). Revision burden remained stable over the 10-year observation period. Surgical complications were higher in revision TKA than in primary TKA (10% vs. 7.7%; p=0.007). 90day complication rates for primary and revision TKA including death were 0.3% and 0.6% (p=0.1) and for pulmonary embolism 0.5% and 0.4% (p=0.6). 90day re-admission rates for primary and revision TKA including infection were 0.5% and 4.2% (p<0.001), for myocardial infarction 0.1% each, and for pneumonia 0.2% and 0.4% (p=0.08).
Interpretation The incidence of primary and revision TKA increased between 1995 and 2005. The rates of postoperative complications were low. Comparisons of the study population and the underlying general populations of interest indicate that this population can be used to predict the incidences and outcomes of TKA in the general population of California and of the United States as a whole.
Although the epidemiology of total hip and knee arthroplasty (THA and TKA) has been studied extensively in Europe, there have been few studies from the United States (US). From those few reports, however, there appears to be agreement that the incidence rates for total joint replacement in the US are rising—especially those for TKA (Jain et al. Citation2005, Citation2006, Crowninshield et al. Citation2006, Kurtz 2006).
Development of a population-based approach to the epidemiology of TKA in the US has been problematic. The most complete population-based record of healthcare in the US is arguably the Medicare database, which has been used to study rates of hip and knee replacement (Friedman and Elixhauser Citation1993, Katz et al. Citation1996, Heck et al. Citation1998, Escalante et al. Citation2002, Mahomed et al. Citation2003, Citation2005). The coding of Medicare data has well-known limitations, however, both in terms of coding bias and in terms of the level of detail regarding any given procedure (Heck et al. Citation1998, Losina et al. Citation2003). Furthermore, the Medicare database includes only patients who are 65 years or older, or who have retired due to disability. In the US, the increasing number of younger, active individuals who undergo TKA will not be captured by the existing Medicare database.
The purpose of this study was to evaluate the epidemiology, trends, and outcomes of TKA in Southern California using the computerized data systems of Kaiser Permanente (KP), a prepaid group model health maintenance organization (HMO). We investigated whether this HMO population could be used to draw inferences regarding the underlying population of California and the United States as a whole.
Patients and methods
We conducted a retrospective review of the number of primary total knee replacements and revision total knee replacements at Southern California Kaiser Permanente between 1995 and 2004. Complications and re-admission rates for total knee replacement procedures were calculated for 1997 through 2004.
The numbers of total knee replacement procedures between 1995 and 2004 were obtained using the Kaiser Permanente Southern California (KPSC) Clinical Utilization Database, a hos-pital-based administrative database. ICD 9-CM codes (International Classification of Diseases, Ninth Revision, Clinical Modification) were used to query the administrative data according to the algorithm reported by Katz et al. (Citation2004). Total knee replacement patients were identified based on the following procedure codes: 81.54 (total knee replacement) and 81.55 (revised total knee replacement). 12 patients with a diagnosis at admission— or a principal discharge diagnosis—of metastatic or bone cancer (170, 170.6, 170.7, 170.9, 195.3, 195.5, 198, 198.5, 199.0, 733.1, 733.14) were excluded from the study. Patients with a primary total knee replacement and a diagnosis at admis-sion—or a principal discharge diagnosis—of fracture (6 patients) (820, 821, 822, 823), infection (4 patients) (711, 711.0, 711.00, 71105, 7116, 71160, 711.65, 711.9, 711.90, 711.95, 730, 730.0, 730.00, 730.1, 730.10, 730.15, 730.2, 730.20, 730.25, 730.9, 730.90, 730.95, 996.6, 996.60, 996.66, 996.67), or other complications from the internal prosthetic device/implant/graft (17 patients) (v540, 996.4, 996.7, 996.70, 996.77, 996.78) were also excluded. After exclusion of these 39 patients, 15,943 patients were identified as having a primary TKA and 1,137 were identified as having a revision TKA performed at KPSC facilities between 1995 and 2004. Demographics and ASA scores were obtained from this utilization database.
We calculated incidence rates for total knee replacement and revision total knee replacement by dividing the number of procedures done each year from 1995 to 2004 by the total number of KPSC members reported at the end of that year. Incidence rates are reported per 10,000 health plan members. Sex-specific incidence rates were also calculated. The trends in incidence rates for primary TKA and revision TKA were modeled using a negative binomial regression with age group (< 65 and≥65 years old), sex, and calendar year as covariates. Interactions between covariates were also examined. The negative binomial regression model predicting number of primary TKAs from calendar year, sex, and age group was statistically significant (p<0.001; dispersion=0.02). A separate negative binomial model (p<0.001; dispersion=0.008) was created to further investigate the effect of age categories on increasing rates of surgery, which was also found to be statistically significant.
KPSC membership grew at an average rate of 4% per year, averaging 2.1 million members during the study period. To assess whether the HMO study population is representative of the underlying population of Southern California and the United States, we compared KPSC demographics (age, sex) to concurrent census data for California and the US (US Census Data 2007).
Complications and re-admissions were identified using the KPSC Clinical Utilization Database.
These data were only available from 1997 through 2004. Surgical complications and 90-day complication rates for pulmonary embolism (PE), deep venous thrombosis (DVT), and death were calculated. Re-admissions within 90 days of the index procedure were identified for infection, myocardial infarction, and pneumonia requiring hospitalization. Complication rates and re-admission rates for primary and revision procedures were compared using the Pearson Chi-square test and Fisher's exact test.
Negative binomial regression was performed using the SAS statistical software package (version 9.1.3; SAS Institute, Cary, NC). All other analyses were performed using SPSS software (release 14.0.0; SPSS Inc., Chicago, IL).
Results
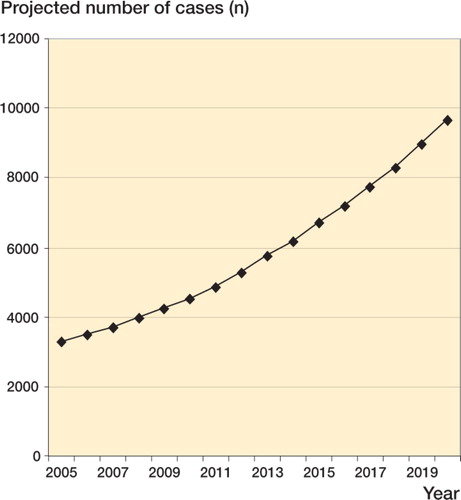
Incidence rates for primary TKA rose between 1995 and 2004, from 6.3 (95% CI: 5.9–6.7) to 11.0 (CI: 10.5–11.4) at a rate of 5.1% (CI: 3.6–6.7) per year (p<0.001) (). Furthermore, in patients who were younger than 65 the rate of surgery increased by 8.8% (CI: 6.7–10) annually while in patients older than 65, the rate increased by 2.1% (CI: 0.6–3.6) annually. The regression model also showed a 1.6-fold (CI: 1.5–1.8) increased risk of females having TKA (p<0.001).
Figure 1. Annual incidence rates for primary TKA (left panel) and revision TKA (right panel), with breakdown according to sex. 95% confidence intervals are shown.
For revision procedures the incidence rate rose during the 10-year period, from 0.41 (CI: 0.31–0.51) to 0.74 (CI: 0.63–0.86), but this increase was not statistically significant (p=0.4). The model was then repeated with age and sex only, and male sex was found to be the sole predictive variable for revision procedures (p<0.001; dispersion=0.009). Males had a 1.3-fold (CI: 1.2–1.6) higher risk of revision than females (p<0.001). Age and calendar year were not predictive of revision surgery rates. Revision burden remained stable, with the lowest revision burden rate of 5.3% in 1997 and the highest of 7.9% in 2002.
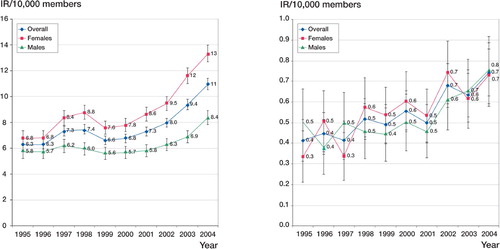
With respect to age and sex distribution, membership of Kaiser Permanente of Southern California (KPSC) was representative of the general populations of California and the United States. A significant proportion of the patients who underwent primary or revision TKA were less than 65 years old (34% of all primary TKAs and 34% of all revision TKAs) (). The proportion of female TKA patients was higher than the proportion of male patients in both primary procedures (61% vs. 38%) and revision procedures (54% vs. 46%) (p<0.001). Mean age was the same for primary TKAs and revision TKAs (68 years). Primary TKA patients had lower ASA scores than those who underwent revision knee replacements (p<0.001) ().
Figure 2. Number of primary TKA cases (left panel) and revision TKA cases (right panel) per year according to age.
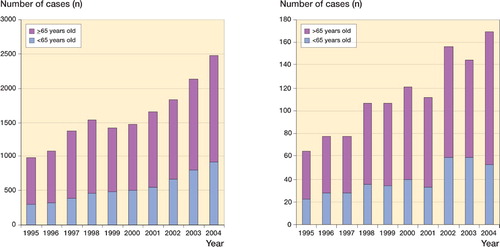
Using our negative binomial regression model, we could estimate that the IR of primary TKA in the year 2020 per 10,000 members would be 18 for males under 65, 62 for males 65 and older, 27 for females under 65, and 77 for females 65 and older. The total projected number of primary TKAs to be done at KPSC is depicted in .
Table 1. Demographics
Surgical complication rates were higher in revision procedures than in primary procedures (10.1% vs. 7.7%, p=0.004). Complication rates regarding PE were similar in primary and revision procedures (0.5% vs. 0.4%, p=0.6) as were DVT (0.6% vs. 0.8%, p=0.4) and death (0.3% vs. 0.6%, p=0.1). The overall rate of re-admission in revision surgery was higher than in primary surgery (15.4% vs. 8.3%, p<0.001). The infection rate was also higher in revision procedures (4.2% vs. 0.5%, p<0.001). There was no difference in the rates of re-admission due to myocardial infarction and pneumonia between primary and revision procedures ().
Table 2. Complications and re-admission rates
Discussion
We examined the incidence rates and perioperative complications of TKA over a 10-year period in members of Kaiser Permanente of Southern California, a non-profit community-based prepaid healthcare system in the United States. The study population averaged 2.1 million members during the study period, corresponding to 6% of the general population of California. KPSC is similar in many respects to nationalized healthcare systems in Europe, in that all healthcare services are covered prospectively by the health plan on an annual basis. Analysis of population demographics revealed that the KPSC population is representative of the general population of California and the United States.
The calculation of annual incidence rates, trends, and outcomes provides information for researchers, administrators, and clinicians to predict future need for TKA in an aging population. The 75–79-year-old subgroup had the highest incidence rates for primary TKA (51 per 10,000 members in 2004) and the greatest numerical increase in incidence rate over the 10-year observation period. Patients below the age of 65 years consituted a substantial proportion of the total number of TKAs (one-third of both primary procedures and revisions) and contributed the greatest percentage rise in incidence rates.
Population-based studies on the epidemiology and outcome of TKA in the US have used Medicare data, on the assumption that the Medicare database is an accurate reflection of the subset of the popula tion undergoing TKA. To our knowledge, this assumption has not been validated. P-value From our data, however, it appears that the assumption is incorrect: the Medicare database would miss up to one-third of 0.007 patients undergoing total knee replace-0.6ment in our population because they are below the age of enrollment. Even the use of the Nationwide Inpatient Sample data offers an incomplete picture because it lacks clinical outcome data (Jain et al. Citation2005, Mahomed et al. Citation2005). In the study by Mahomed et al. of Medicare TKA rates in the year 2000, incidence rates varied by US region. For the Pacific census division, they reported incidence rates of 45 and 4.0 per 10,000 for primary and revision TKA, respectively. For the same year, the IRs for primary and revision TKA in the Medicare age group within the Kaiser Health plan were 44 (95% CI: 42–47) and 3.9 (95% CI: 3.2–4.6) per 10,000 members, respectively. Furthermore, Jain et al. (Citation2005) reported on trends in incidence in TKA patients from 1990 to 2000 and showed rising rates among all patients, with the greatest percentage increases seen in the 40- to 49-year age group (95%) and the 50- to 59year age group (54%) (2005). This high-percentage rise in TKA in younger age groups is reflected by our own findings. The increasing incidence rates of TKA reported here are consistent with those from the Swedish and Norwegian arthroplasty registries. From 1995 to 2005, the Norwegian registry reported an increase in incidence rates for TKA in the 70- to 79-year-old population of 25–53 per 10,000 in females and 8–26 per 10,000 in males (http://www.haukeland.no/nrl/Report2007.pdf http://www.knee.nko.se/english/online/uploaded-Files/110_SKAR2007_Engl1.2.pdf).
In contrast to our findings and to those of Mahomed et al. (Citation2005) and Jain et al. (Citation2005), Olmstead County's Mayo clinic statistics reported much lower incidence rates of TKA from 1971 to 1986 (Quam et al. Citation1991). TKA incidence rates rose from 2.1 per 10,000 person-years for 1971 through 1974 to 6.1 per 10,000 for 1983 through 1986, with women having higher rates than men. The TKA rates in our study were substantially higher than those reported by Quam et al. (Citation1991). While sex differences and trends were similar, the differences between incidence rates calculated for the two studies may be the result of inclusion of uninsured people in Quam's denominator, regional demographic differences, surgeon and patient preferences, or the more recent time period of our study. Kurtz et al. (Citation2006) used the Poisson regression model to predict the number of primary and revision TKA surgeries in the United States using the National Inpatient Sample (NIS). Their goodness of fit was calculated with a scaled Pearson chi-square average of 1.11 (1.03 for primary TKA and 1.11 for revision TKA). Our data fit best with the negative binomial regression model, however. Kurtz et al. (Citation2006) predicted a 238% increase in the total number of procedures from 2005 to 2020. Our data predict a 200% increase in primary TKA from 2005 to 2020. Kurtz et al. also found a stable revision burden over the observation period, which was also our experience.
In comparison to the data reported by Mahomed et al. (Citation2005), our lower 90-day mortality rate of 0.3% at 90 days (as opposed to 0.7%) reflects both the inclusion of patients below the age of 65 in our study population and the fact that TKA procedures performed within the Kaiser system are carried out by high-volume surgeons in high-volume institutions. Patient age, surgeon volume, and hospital volume have previously been reported to have a significant effect on patient mortality (Parvizi et al. Citation2001, Katz et al. Citation2004, Soohoo et al. Citation2006).
We also discovered a higher rate of re-admis-sion within 90 days for infection in revision TKA than in primary TKA (4.2% vs. 0.5%, p<0.001). A prior history of knee implant surgery has been shown to be associated with an increased risk of infection after TKA (Lazzarini et al. Citation2001). The PE and MI rates at 90 days were low (0.5% and 0.1%, respectively, for primary TKA and 0.4% and 0.1%, respectively, for revision TKA). No statistically significant differences between primary and revision surgery were found with regard to PE outcome. The PE rates in the present study were also lower than in the Medicare population, and are consistent with published rates from smaller studies (Mantilla et al. Citation2002, Bullock et al. Citation2003, Hervey et al. Citation2003, Feinglass et al. 2004a, Citationb).
The steady revision burden over the 10-year observation period is particularly interesting. With the advent of improvements in implant design, implant materials, surgical technique, and training of surgeons, one would expect to have seen a reduction in the revision burden over time. Foran et al. (Citation2004) described other factors (including increasing patient obesity, activity, and life-expectancy) that may increase the revision burden. Crowninshield et al. (Citation2006) described the changing demographics in total joint arthroplasty patients—including heavier weight, more physical activity, and living for 25% longer. These changes in the population at risk combined with the increasing incidence of TKA may contribute to the lack of reduction in revision burden seen, in spite of the presumed improvements in technology and technique.
Few would argue about the value of TKA for society, but in the face of rapidly increasing volume, the surgeon must be equipped with evidence-based data to aid the patient in the preoperative decision-making process. Surgical technique and implant characteristics are being critically examined to determine their effect on patient outcome and implant survivorship (Hervey et al. Citation2003, Katz et al. Citation2004). On the other hand, patient characteristics have not been evaluated as critically. The increased incidence rates for TKA in young patients in our investigation portend future increases in the numbers of revision knee procedures. Increasing rates of obesity (Foran et al. Citation2004), the documented success of knee replacement procedures (Callaghan et al. Citation2005, Dixon et al. Citation2005), direct-to-consumer marketing, geographical variation in TKA utilization (Mahomed et al. Citation2005), and the leading edge of “baby-boomers” seeking to maintain an active lifestyle are all factors causing higher incidence rates. One area of particular concern for the US population is obesity. Conflicting reports exist regarding the importance of weight for the outcome of TKA surgery (Winiarsky et al. Citation1998, Foran et al. Citation2004, Namba et al. Citation2005, Amin et al. Citation2006). By furthering our understanding of the role of the surgeon, hospital, implant, and patient in the causes of failure of TKA, we can aim to improve the outcomes of primary and revision surgery.
Our study had several limitations. The data were collected retrospectively from administrative databases. The clinical utilization database that we used is organized according to subject areas and integrates different operational databases within the KP system. It is time variant, and does not get updated. As with all studies based on such databases, this one depends on the accuracy of coding. Furthermore, we assumed that our surgeons follow American standards regarding recommendation of TKA. Surgeon training, volume, availability of operating rooms and hospital bed space, and remuneration may all have a bearing on observed rates of TKA in the United States.
In summary, our study provides incidence rates, 90-day complication rates, and trends in the incidence of total knee replacement over a ten-year period. Our data should facilitate prediction of healthcare costs and resource management for any healthcare system in California or in the United States as a whole. In future research, efforts should be made to investigate the underlying reasons for the rise in incidence rates over time. Special attention should be paid to understanding what is causing the increased incidence of TKA noted in younger patients, and also why the revision burden has not improved over time.
No competing interests declared.
MK: developed research question, lead research team, prepared manuscript. MI: co-developed analysis plan, performed data extraction and data analysis. EP: co-developed analysis plan. SB: co-authored manuscript. RN: co-authored manuscript. RB: statistics expert, produced the negative binomial models. DF: research team oversight, manuscript reviewer.
- Amin A. K, Patton J. T, Cook R. E, et al. Does obesity influence the clinical outcome at five years following total knee replacement for osteoarthritis?. J Bone Joint Surg (Br) 2006; 88(3)335–40
- Bullock D. P, Sporer S. M, Shirreffs T. G, Jr. Comparison of simultaneous bilateral with unilateral total knee arthroplasty in terms of perioperative complications. J Bone Joint Surg (Am) 2003; 85(10)1981–6
- Callaghan J. J, O'Rourke M. R, Iossi M. F, et al. Cemented rotating-platform total knee replacement. a concise follow-up, at a minimum of fifteen years, of a previous report. J Bone Joint Surg (Am) 2005; 87(9)1995–8
- Crowninshield R. D, Rosenberg A. G, Sporer S. M. Changing demographics of patients with total joint replacement. Clin Orthop Relat Res 2006; 443: 266–72
- Dixon M. C, Brown R. R, Parsch D, et al. Modular fixed-bear-ing total knee arthroplasty with retention of the posterior cruciate ligament. A study of patients followed for a minimum of fifteen years. J Bone Joint Surg (Am) 2005; 87(3)598–603
- Escalante A, Barrett J, del Rincon I, et al. Disparity in total hip replacement affecting Hispanic Medicare beneficiaries. Med Care 2002; 40(6)451–60
- Feinglass J, Amir H, Taylor P, et al. How safe is primary knee replacement surgery? Perioperative complication rates in Northern Illinois. Arthritis Rheum 2004a 1993-1999; 51(1)110–6
- Feinglass J, Koo S, Koh J. Revision total knee arthroplasty complication rates in Northern Illinois. Clin Orthop Relat Res 2004b; 429: 279–85
- Foran J. R, Mont M. A, Rajadhyaksha A. D, et al. Total knee arthroplasty in obese patients: a comparison with a matched control group. J Arthroplasty 2004; 19(7)817–24
- Friedman B, Elixhauser A. Increased use of an expensive elective procedure: total hip replacements in the 1980s. Med Care 1993; 31(7)581–99
- Heck D. A, Melfi C. A, Mamlin L. A, et al. Revision rates after knee replacement in the United States. Med Care 1998; 36(5)661–9
- Hervey S. L, Purves H. R, Guller U, et al. Provider Volume of Total Knee Arthroplasties and Patient Outcomes in the HCUP-Nationwide Inpatient Sample. J Bone Joint Surg (Am) 2003; 85(9)1775–83
- Jain N. B, Higgins L. D, Ozumba D, et al. Trends in epidemiology of knee arthroplasty in the United States, 19902000. Arthritis Rheum 2005; 52(12)3928–33
- Jain N. B, Higgins L. D, Guller U, et al. Trends in the epidemiology of total shoulder arthroplasty in the United States from 1990-2000. Arthritis Rheum 2006; 55(4)591–7
- Katz B. P, Freund D. A, Heck D. A, et al. Demographic variation in the rate of knee replacement: a multi-year analysis. Health Serv Res 1996; 31(2)125–40
- Katz J. N, Barrett J, Mahomed N. N, et al. Association between hospital and surgeon procedure volume and the outcomes of total knee replacement. J Bone Joint Surg (Am) 2004; 86(9)1909–16
- Kurtz S. M, Lau E, Ke Zhao Mowat F, Ong K, Halpern M. The Future Burden of Hip and Knee Revisions: U.S. Projections from 2005 to 2030. 2006
- Lazzarini L, Pellizzer G, Stecca C, et al. Postoperative infections following total knee replacement: an epidemiological study. J Chemother 2001; 13(2)182–7
- Losina E, Barrett J, Baron J. A, et al. Accuracy of Medicare claims data for rheumatologic diagnoses in total hip replacement recipients. J Clin Epidemiol 2003; 56(6)515–9
- Mahomed N. N, Barrett J. A, Katz J. N, et al. Rates and outcomes of primary and revision total hip replacement in the United States medicare population. J Bone Joint Surg (Am) 2003; 85(1)27–32
- Mahomed N. N, Barrett J, Katz J. N, et al. Epidemiology of total knee replacement in the United States Medicare population. J Bone Joint Surg (Am) 2005; 87(6)1222–8
- Mantilla C. B, Horlocker T. T, Schroeder D. R, et al. Frequency of myocardial infarction, pulmonary embolism, deep venous thrombosis, and death following primary hip or knee arthroplasty. Anesthesiology 2002; 96(5)1140–6
- Namba R. S, Paxton L, Fithian D. C, et al. Obesity and perioperative morbidity in total hip and total knee arthroplasty patients. J Arthroplasty 2005; 20(7(Suppl 3)46–50
- Parvizi J, Sullivan T. A, Trousdale R. T, et al. Thirty-day mortality after total knee arthroplasty. J Bone Joint Surg (Am) 2001; 83(8)1157–61
- Quam J. P, Michet C. J, Jr., Wilson M. G, et al. Total knee arthroplasty: a population-based study. Mayo Clin Proc 1991; 66(6)589–95
- Soohoo N. F, Zingmond D. S, Lieberman J. R, et al. Primary total knee arthroplasty in California 1991 to 2001: does hospital volume affect outcomes?. J Arthroplasty 2006; 21(2)199–205
- The Norwegian Arthroplasty Register, 2007 Report www.haukeland.no/nrl/Report2007.pdf
- The Swedish Knee Arthroplasty Register -Part 1, Annual Report 2007 http://www.knee.nko.se/english/online/ uploadedFiles/110_SKAR2007_Engl1.2.pdf
- U.S. Census Data. Annual Estimates of the Population by Age and Sex for California: April 1, 2000 to July 1, 2006. Population Division, U.S. Census Bureau. May 17, 2007. Available from http://www.census.gov/popest/states/asrh/SC-EST2006-02.html
- Winiarsky R, Barth P, Lotke P. Total knee arthroplasty in morbidly obese patients. J Bone Joint Surg (Am) 1998; 80(12)1770–4