Abstract
Background and purpose — Currently, no clear evidence exists on the pattern of use of antithrombotics at admission in hip fracture patients and how this has changed over time. We investigated temporal trends in—and factors associated with—the use of antithrombotics in patients admitted with a fractured hip.
Patients and methods — This was a population-based cohort study including all patients aged 18 years or above who were admitted with a hip fracture in Denmark from 1996 to 2012. The Danish national registries were used to collect information on medication use, vital status, and comorbidity.
Results — From 1996 to 2012, the proportion of patients using antithrombotics in general increased by a factor of 2.3 from 19% to 43% (p < 0.001). More specifically, the use of anticoagulants increased by a factor of 6.8 and the use of antiplatelets increased by a factor of 2.1. When we adjusted for possible confounders, the use of antithrombotics still increased for every calendar year (relative risk (RR) = 1.03, CI: 1.03–1.04; p < 0.001). Age, sex, and Charlson comorbidity index were all associated with the use of antithrombotics (all p < 0.001).
Interpretation — The proportion of hip fracture patients using antithrombotics at admission has increased substantially in Denmark over the last 2 decades. This highlights the need for evidence-based guidelines on how to handle patients using antithrombotics to ensure safe surgery and to avoid surgical delay.
Patients admitted with a fractured hip often have several comorbidities that can affect the perioperative period, and they often have poor outcomes (Abrahamsen et al. Citation2009, Baker et al. Citation2014). Current evidence from non-randomized studies suggests that surgical delay is associated with increased mortality in these patients (Daugaard et al. Citation2012, Nyholm et al. Citation2015). There is therefore a strong focus on minimizing the time from admission to surgery. One of the factors that can lead to surgical delay is the use of antithrombotics at admission, due to the risk of bleeding complications. Warfarin and the antiplatelet drug clopidogrel have received special attention regarding safe surgery in hip fracture patients (Al-Rashid and Parker Citation2005, Ahmed et al. Citation2014, Gleason and Friedman Citation2014, Gleason et al. Citation2014, Doleman and Moppett Citation2015). In addition to balancing the risk of bleeding against early surgery, it is also important to consider the risk of thromboembolism when discontinuing antithrombotic therapy (Gleason and Friedman Citation2014).
During the last 2 decades, several new antithrombotics have been marketed for indications such as atrial fibrillation, and for prevention of venous thromboembolism. In addition, there has been a trend towards more aggressive treatment and prevention of thromboembolic events—as, for example, associated with atrial fibrillation—and a corresponding increase in the use of antithrombotics (Karve et al. Citation2012, Shroff et al. Citation2014).
It is believed that the use of antithrombotics on admission is becoming increasingly common in patients who have been admitted with a fractured hip. However, as far as we know, there have been no studies investigating the pattern of use of antithrombotics in these patients and how this has changed over time. This information would be useful in order to estimate the size of the problem and thereby highlight the need for evidence-based guidelines on the matter.
The main aim of this study was to determine the temporal trends in the use of antithrombotics for hip fracture patients at admission, using data from national registries. Secondly, we wanted to investigate factors associated with the use of antithrombotics and to compare the trends observed in hip fracture patients with those seen in the background population.
Patients and methods
Study population
Using the Danish National Patient Registry (DNPR), we identified all patients aged 18 years or more who were admitted with a fractured hip (ICD-10 codes DS720 (femoral neck), DS721 (pertrochanteric), and DS722 (subtrochanteric)) in Denmark during the period from the January 1, 1996 to December 31, 2012. Patients who appeared twice due to a contralateral fracture or to subsequent hip fractures were included with the index fracture only. 154,047 patients were eligible for inclusion and composed the study cohort.
National patient registries—outcome and covariates
All Danish citizens are registered in the Danish Civil Registration System (CRS) using a unique 10-digit civil registration number (CRN). The unique CRN makes it possible to retrieve information on individuals from a variety of national registries. The use of the CRN in all public records enables almost complete follow-up and traceability, and it is possible to extract data on birth date and sex from the number (Schmidt et al. Citation2014). Demographic information on people living legally in Denmark such as vital status, emigration etc., is available from the CRS.
The DNPR contains information on all somatic hospital admissions dating back to 1977, and, since 1995, also psychiatric admissions and outpatient visits (Lynge et al. Citation2011). In the DNPR, every hospital visit is registered with a set of data that includes a single primary discharge diagnosis or an unlimited amount of secondary diagnostic codes. This classification is done using International Disease Classification (ICD) codes. Data from the DNPR were used to define the study cohort of all hip fracture patients in Denmark from 1996 to 2012, and to retrieve data on comorbidities for the patients included—dating back to 1995. This was done in the form of the Charlson comorbidity index (CCI), which was coded based on the method described by Quan et al. (Citation2005). In addition, we included information on the following individual groups of comorbidities, based on a previous diagnosis of the ICD-10 codes indicated: atrial fibrillation/flutter (I48), ischemic heart disease (I20–25), pulmonary embolism (I26), stroke/TCI (G458–459, I63–64), arterial thromboembolism (I74), deep vein thrombosis (I801–803, I808–809, I821-823, I828–829), valvular disease (I05–08, I091, I098, I34–39, Z952–954), and conditions with artificial heart valve (Z952–954).
Similarly to the DNPR, all prescription drugs sold in Denmark are registered in the Danish National Prescription Database (DNPB) using the CRN. The database covers the use of all prescription pharmaceuticals used outside of hospitals, including use at, for example, nursing homes. Data collection goes back to 1994 and loss to follow-up is unlikely (Kildemoes et al. Citation2011). Data available from the DNPB include date, anatomical therapeutic chemical (ATC) codes, dosage etc. We defined use of a certain drug as there having been at least 2 redeemed prescriptions for the individual drug within the year preceding the hip fracture.
Anticoagulants were included in the form of vitamin K antagonists (ATC code B01AA) and new oral anticoagulants (NOAC) (ATC code B01AE07 (Dabigatran) and B01AF (Rivaroxaban and Apixaban)). Antiplatelet drugs were included in the form of low-dose acetylsalicylic acid (ATC code B01AC06), clopidogrel (ATC code B01AC04), dipyridamole (ATC code B01AC07), prasugrel (ATC code B01AC22), ticagrelor (ATC code B01AC24), and combination drugs ((ATC code B01AC30 (Asasantin)). Use of antithrombotics was defined as use of any of the above-mentioned anticoagulants or antiplatelet drugs. Data on non-oral antithrombotics such as heparins were not included. The primary outcome was the proportion of users of the individual antithrombotics for each of the years from 1996 to 2012.
To obtain information on the use of antithrombotics in the general Danish population for comparison, we used publicly available data on use of prescription medications and demographics of the Danish population. Statens Serum Institut metadata on the use of prescription medication in Denmark is available online at www.medstat.dk (Statens Serum Institut). The data are based on the DNPB, and drugs are listed according to ATC codes. Data on medication use in different age groups and according to sex are available for each year since 1999. Subjects are registered if they redeemed at least 1 prescription in the year in question. The output can be given as total number of patients who redeemed a prescription for the drug in question during a particular year. As the data are aggregated, it is not possible to deduce whether the same person uses one or more antithrombotics. Thus, it is not possible to add the number of individuals from different ATC codes.
To calculate the proportion of users in the general population, we also used information on the number of people living in Denmark on January 1 of each year in different age groups and by gender. This information is publicly available through Statistics Denmark (Statistics Denmark). An indication of the total number of people aged 18 years or more living in Denmark is given in .
Statistics
For baseline characteristics, continuous variables were compared using Student t-tests for normally distributed variables and Mann-Whitney U-tests for non-parametric variables. Categorical variables in the form of baseline characteristics and proportions were compared using Pearson’s chi-squared test. The Cochran-Armitage trend test was used to test for trends in the proportions of patients using antithrombotics over time, in univariate analysis.
Relative risk (RR) estimates for the use of antithrombotics were calculated using multivariable Poisson regression with robust error variance, as described by Zou (Citation2004). Analysis of time series data can be influenced by autocorrelation that affects the error terms, but not the estimates themselves. In the Poisson regression, we therefore decided to use an autoregressive correlation matrix specified in the repeated statement in proc genmod in SAS. The model included the available variables—year, sex, age, and CCI—but not all known confounders.
2-sided p-values <0.05 were considered significant. Statistical analyses and data management were conducted using SAS version 9.3 through a secure remote connection provided by Statistics Denmark.
Ethics
According to Danish law, ethical committee approval is not required for this type of observational study. The data were obtained through secure remote access to Statistics Denmark (ref. 704670).
Results
Baseline characteristics
154,047 patients were included, and 33% of them used 1 or more antithrombotics on admission. Among the users of antithrombotics, there was a higher proportion of men and a higher mean age (). Furthermore, the users of antithrombotics had a higher degree of comorbidity and a higher unadjusted 30-day mortality (all p < 0.001). Specific diseases for which antithrombotics are the treatment or part of it (for example, atrial fibrillation) were much more prevalent among users of antithrombotics.
Table 1. Baseline characteristics
Temporal trends in the use of antithrombotics—hip fracture patients
From 1996 to 2012, there was a 2.3-fold increase in the use of antithrombotics, a 6.8-fold increase in the use of anticoagulants, and a 2.1-fold increase in the use of antiplatelet drugs ( and ). The 2 newer antiplatelet drugs ticagrelor and prasugrel are not included in the table due to the very low numbers of users. For ticagrelor, there was 1 user in 2011 and 14 in 2012, and for prasugrel, 1 user in 2010.
Figure 1. Proportion of hip fracture patients who used antithrombotics, 1996 to 2012. Panel A shows the overall results, whereas panels B and C show the results for the individual anticoagulants and antiplatelet drugs, respectively. w/o ASA: without patients who used only acetylsalicylic acid.
* p-value for trend <0.001.
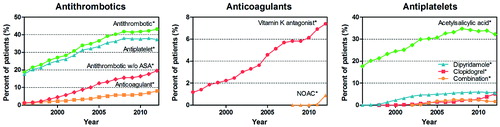
Table 2. Temporal trends in the use of antithrombotics, 1996 to 2012
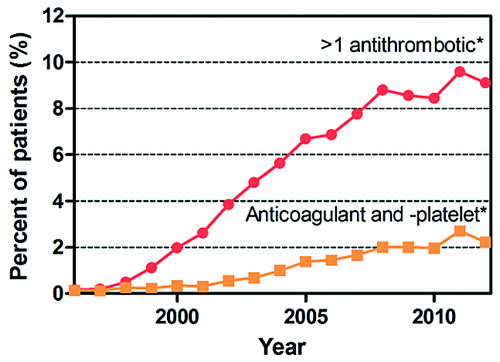
In addition to the increase in the use of antithrombotics in general, there was also a statistically significant increase in the number of patients using more than 1 antithrombotic (). From 1996 to 2012, there was a 54-fold increase in the proportion of patients using more than 1 antithrombotic and a 16-fold increase in the proportion of patients using anticoagulants and antiplatelet drugs concomitantly.
Figure 2. Proportion of hip fracture patients who used more than 1 antithrombotic from 1996 to 2012. * p-value for trend <0.001.
A multivariable Poisson regression analysis was conducted in order to determine what factors were associated with the use of antithrombotics, and to control for possible confounders (). There was an increase in relative risk regarding the use of both anticoagulants and antiplatelet drugs per annual increase in time since admission, even when controlling for confounding factors. Looking at other factors, there was an association between age, comorbidity (CCI), and gender, and increasing use of antithrombotics.
Table 3. Multivariable analysis – factors associated with the use of antithrombotics
Table 4. Use of antithrombotics in the general Danish population in 1999 and 2012
Temporal trends in the use of antithrombotics—the general population
To determine whether the trend observed in the hip fracture patients was comparable to the trend in the general population, we looked at the percentage of individuals in the general population (aged 18 years or more) who redeemed prescriptions for specific antithrombotics during the period 1999 to 2012. There was a statistically significant increase in the number of subjects using antithrombotics from 1999 to 2012 (). Most of the hip fracture patients were 60 years old or more (> 91%), and the use of antithrombotics increased with age. Thus, we also looked at the use of antithrombotics in those aged 60 years or above in the general population. As this was only a crude comparison between hip fracture patients and the general population, no formal statistical analyses were used to compare the 2 populations.
Discussion
This study, covering the entire Danish population, shows for the first time that there has been a substantial increase in the use of antithrombotics in hip fracture patients. The increase was seen for both anticoagulants and antiplatelet drugs.
The last 2 decades have seen the approval and marketing of several new antithrombotics, and their gradual uptake in patients is indicated by the results in . This includes drugs such as clopidogrel (which was approved in Denmark in 1998) and, most recently, the NOACs (which were first approved in Denmark in 2008). In addition to these new drugs, there has also been an increase in the number of patients using older drugs such as aspirin and vitamin K antagonists. In comparing the data from the hip fracture patients with that from the general population, it is clear that the trends observed in hip fracture patients reflect those seen in the general population. The increase in the number of users of antithrombotics is in line with the results of studies showing increased use of, for example, anticoagulants for stroke prevention in atrial fibrillation (Karve et al. Citation2012, Shroff et al. Citation2014).
There appears to be a slight plateau in the number of users of antiplatelet drugs, and a continued increase in the number of patients using anticoagulants over the last 4–5 years. It is difficult to predict, however, how the use of antithrombotics will change in the future, but most interesting in this context is perhaps how the use of NOACs will change. This study only covered a limited length of time following approval and marketing of the first NOAC in Denmark in 2008, and it was only in 2011 that NOACs were approved for atrial fribrillation in Denmark. It can be expected that there will be a marked increase in the number of patients using NOACs on admission in the years to come. This is supported by the fact that an increasing number of patients with atrial fribrillation in Denmark are now started on NOACs instead of warfarin (Olesen et al. Citation2015). The increasing use of NOACs could be a problem due to the lack of an antidote, and problems with reliable coagulation tests (Harder and Graff Citation2013). Furthermore, the use of NOACs can affect the choice of anesthesia, as neuraxial anesthesia will often be contraindicated in patients who are on NOACs (Benzon et al. Citation2013).
There is a consensus that surgery on hip fracture patients should be performed as soon as possible (Fernandez et al. Citation2015). In this context, several studies have looked at the association between the use of antithrombotics on admission and outcome in hip fracture patients. In general, these studies have been of small scale, with few cases and a retrospective case-control design. This is exemplified by a recent systematic review and meta-analysis on early surgery in patients taking clopidogrel (Doleman and Moppett Citation2015). Pooling of all available studies with data on mortality yielded only 207 users of clopidogrel and 29 events (deaths) in that group. The study found that there was no increased risk of mortality in patients taking clopidogrel, but, as the authors indicated, the published studies have had shortcomings and additional studies are needed. The same is true for studies on vitamin K antagonists (Al-Rashid and Parker Citation2005, Collinge et al. Citation2012, Ahmed et al. Citation2014, Gleason et al. Citation2014).
The low level of evidence in the studies on how to handle the use of antithrombotics in hip fracture patients at admission is also reflected by the lack of consensus on which algorithms should be used in these patients (Inman et al. Citation2007, Palan et al. Citation2007, Lavelle et al. Citation2008). There appears to be a need for clear evidence-based guidelines on the subject.
The limitations of our study were mainly related to the definition of use of the individual drugs. Use was defined as a minimum of 2 prescriptions redeemed within the last year, in order to only include chronic users. If a patient had just started taking the drug and had only redeemed 1 prescription, they would not have been classified as users, leading to an underestimation of the number of users.
Similarly, a patient could have stopped taking the medicine but still have redeemed 2 prescriptions within the last year, leading to an overestimation of the number of users. All in all, we believe that this was of minor importance—due to the large number of patients included and the likelihood of the 2 scenarios balancing each other out. In addition, although the patients might actually have redeemed prescriptions for the drugs, we have no information on whether or not the patients actually took them.
The strengths of the study include the large number of patients, which covered all Danish hip fracture patients and the entire Danish population over a 17-year period. This permitted a comprehensive analysis of temporal patterns in the use of even rarely used drugs. As the study covered an entire population, this would also increase the generalizability of the results, and it is likely that the trends observed in the Danish population match those in other western countries. Another strength of the study was the use of the Danish national registries, which gave complete data on all prescriptions redeemed in Denmark at the individual level thanks to the civil registration number. The data were collected in an unbiased fashion from the registries, which contrasts with chart review.
An additional finding in our study was that the annual number of hip fractures appears to have decreased substantially during the time frame investigated. This warrants further investigation in future studies.
In summary, the use of antithrombotics in hip fracture patients on admission increased substantially from 1996 to 2012 in Denmark. This included the use of anticoagulants and antiplatelet drugs, and the combined use of the 2. These results highlight the need for evidence-based guidelines on how to handle patients taking antithrombotics on admission, in order to avoid surgical delay and ensure safe surgery.
CMM conceived the idea for the study. All the authors participated in the design of the study and in interpretation of the data. CMM, BA, and HLJ collected the data. CMM drafted the manuscript. All the authors participated in critical revision of the manuscript. CMM conducted the statistical analysis.
There are no competing interests regarding this study. BA declares receipt of support from institutional research contracts to Holbæk Hospital from Amgen, Novartis, and UCB.
- Abrahamsen B, van Staa T, Ariely R, Olson M, Cooper C. Excess mortality following hip fracture: a systematic epidemiological review. Osteoporos Int 2009; 20(10): 1633–50.
- Ahmed I, Khan M A, Nayak V, Mohsen A. An evidence-based warfarin management protocol reduces surgical delay in hip fracture patients. J Orthop Traumatol 2014; 15(1): 21–7.
- Baker P N, Salar O, Ollivere B J, Forward D P, Weerasuriya N, Moppett I K, et al. Evolution of the hip fracture population: time to consider the future? A retrospective observational analysis. BMJ Open 2014; 4(4): e004405.
- Benzon H T, Avram M J, Green D, Bonow R O. New oral anticoagulants and regional anaesthesia. Br J Anaesth 2013; 111Suppl1: i96–113.
- Collinge C A, Kelly K C, Little B, Weaver T, Schuster R D. The effects of clopidogrel (Plavix) and other oral anticoagulants on early hip fracture surgery J Orthop Trauma 2012; 26(10): 568–73.
- Daugaard C L, Jørgensen H L, Riis T, Lauritzen J B, Duus B R, van der Mark S. Is mortality after hip fracture associated with surgical delay or admission during weekends and public holidays? A retrospective study of 38,020 patients. Acta Orthop 2012; 83(6): 609–13.
- Doleman B, Moppett I K. Is early hip fracture surgery safe for patients on clopidogrel? Systematic review, meta-analysis and meta-regression. Injury 2015; 46(6): 954–62.
- Fernandez M A, Griffin X L, Costa M L. Management of hip fracture. Br Med Bull 2015; 115(1): 165–72.
- Gleason L J, Friedman S M. Preoperative management of anticoagulation and antiplatelet agents. Clin Geriatr Med 2014; 30(2): 219–27.
- Gleason L J, Mendelson D A, Kates S L, Friedman S M. Anticoagulation management in individuals with hip fracture. J Am Geriatr Soc 2014; 62(1): 159–64.
- Harder S, Graff J. Novel oral anticoagulants: clinical pharmacology, indications and practical considerations. Eur J Clin Pharmacol 2013; 69(9): 1617–33.
- Inman D S, Michla Y, Partington P F. Perioperative management of trauma patients admitted on clopidogrel (Plavix). A survey of orthopaedic departments across the United Kingdom. Injury 2007; 38(5): 625–30.
- Karve S, Levine D, Seiber E, Nahata M, Balkrishnan R. Trends in ambulatory prescribing of antiplatelet therapy among US ischemic strokeatients: 2000–2007. Adv Pharmacol Sci 2012; 2012: 846163.
- Kildemoes H W, Sørensen H T, Hallas J. The Danish National Prescription Registry. Scand J Public Health 2011 Jul; 39(7 Suppl): 38–41.
- Lavelle W F, Demers Lavelle EA, Uhl R. Operative delay for orthopedic patients on clopidogrel (plavix): a complete lack of consensus. J Trauma 2008; 64(4): 996–1000.
- Lynge E, Sandegaard J L, Rebolj M. The Danish National Patient Register. Scand J Public Health 2011; 39(7 Suppl): 30–3.
- Nyholm A M, Gromov K, Palm H, Brix M, Kallemose T, Troelsen A, Danish Fracture Database Collaborators. Time to surgery is associated with thirty-day and ninety-day mortality after proximal femoral fracture: a retrospective observational study on prospectively collected data from the Danish Fracture Database Collaborators. J Bone Joint Surg Am 2015; 97(16): 1333–9.
- Olesen J B, Sørensen R, Hansen M L, Lamberts M, Weeke P, Mikkelsen A P, Køber L, Gislason G H, Torp-Pedersen C, Fosbøl E L. Non-vitamin K antagonist oral anticoagulation agents in anticoagulant naïve atrial fibrillation patients: Danish nationwide descriptive data 2011–2013. Europace 2015; 17(2): 187–93.
- Palan J, Odutola A, White S P. Is clopidogrel stopped prior to hip fracture surgery–A survey of current practice in the United Kingdom. Injury 2007; 38(11): 1279–85.
- Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi J-C, Saunders L D, Beck C A, Feasby T E, Ghali W A. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 2005; 43(11): 1130–9.
- Al-Rashid M, Parker M J. Anticoagulation management in hip fracture patients on warfarin. Injury 2005; 36(11): 1311–5.
- Schmidt M, Pedersen L, Sørensen H T. The Danish Civil Registration System as a tool in epidemiology. Eur J Epidemiol 2014; 29(8): 541–9.
- Shroff G R, Solid C A, Herzog C A. Atrial fibrillation, stroke, and anticoagulation in Medicare beneficiaries: trends by age, sex, and race, 1992-2010. J Am Heart Assoc 2014; 3(3): e000756.
- Statens Serum Institut. Statens Serum Institut. http://www.medstat.dk (date last accessed 16 September 2015).
- Statistics Denmark. Statistics Denmark. http://www.statistikbanken.dk/folk2 (date last accessed 16 September 2015).
- Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol 2004; 159(7): 702–6.

