Abstract
Background and purpose — The anatomical uncemented stem, SP-CL (Static Physiologicus – CementLess), designed to facilitate insertion and to avoid stress concentration at solitary contact points, has been on the market since 2014 but is not well documented. We studied its clinical performance, migration, and associated bone remodeling in a randomized controlled trial, with the Corail stem as control.
Patients and methods — 79 patients (80 hips) were primarily recruited and 71 patients (72 hips, 36 SP-CL, 36 Corail) attended the last follow-up at 2 years. The Oxford Hip Score (OHS) was the primary outcome. In addition, we assessed stem migration, changes in bone mineral density, and development of radiolucencies by RSA, DXA, and conventional radiography.
Results — At 2 years Oxford Hip Score was similar between the SP-CL and Corail stem. At 2 years the SP-CL stems showed a median distal migration of 0.23 mm (–0.1 to 5.2) and the Corail stems of 0.11 mm (–0.4 to 4.4). The SP-CL stems showed slightly more loss of bone mineral density in Gruen region 7 (p = 0.003).
Interpretation — We found no difference in clinical results between the SP-CL and the well-documented Corail stem. The same stem stability was reached between 1 and 2 years postoperatively for both stems. As a next step we think that the SP-CL stem should be studied in a multi-center setting, before being accepted for general use.
The SP-CL stem was first introduced in 2014 but few studies (Citation1, Citation2) have yet been performed to evaluate this stem in a clinical setting. We performed a randomized controlled trial, comparing the SP-CL stem with use of the Corail stem as reference based on its thorough documentation, not least in national registers (Citation3–6). Evaluation was performed with Oxford Hip Score (OHS), PROMs, RSA, and postoperative changes of bone mineral density around the stem measured with DXA. OHS at 2 years was the primary outcome. We hypothesized that these outcomes should be equal between groups.
Patients and methods
Patients eligible for uncemented total hip arthroplasty (THA), who attended the outpatient clinic at the Sahlgrenska University Hospital, Mölndal, Sweden were asked to participate. Inclusion criteria were femoral anatomy suitable for both of the 2 stem designs, age between 35 and 75 years, and primary or secondary osteoarthritis. Exclusion criteria were ongoing treatment with corticosteroids, active cancer disease, known osteoporosis or osteomalacia, inflammatory arthritis, anatomy unsuitable for either stem design, or difficulties in speaking or understanding the Swedish language.
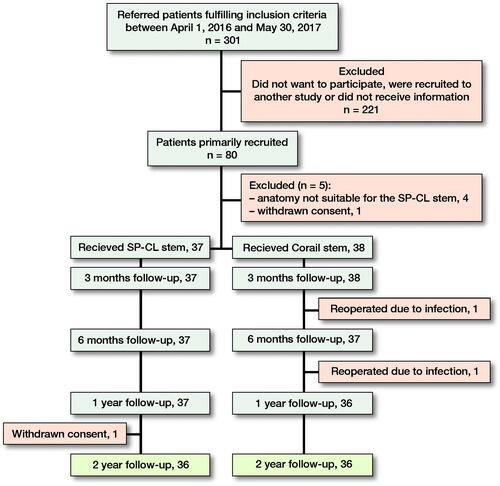
Patients were recruited between April 1, 2016 and May 30, 2017. 301 patients referred to our outpatient clinic were eligible for participation. 80 patients were recruited; 5 patients dropped out before surgery (). Patients were randomized using envelopes; neither surgeon nor patient were blinded. A research coordinator (nurse) performed the randomization. No stratification was used.
The SP-CL stem (Waldemar Link, Hamburg, Germany) is S-shaped in the frontal plane and has an anteversion of 5°. The stem is made of Tilastan-S (TiAl6V4) and has a proximal plasma-spray coating with calcium phosphate (HX coating). Distally the tip is polished.
The Corail (DePuy Synthes, Raynham, MA, USA) is an uncemented straight, hydroxyapatite-coated stem. Since 2009 it has been the most frequently used uncemented stem in Sweden for primary THA (Citation5).
An uncemented Delta-TT cup (trabecular titanium, Lima Corporate, Milan, Italy) supplied with liners made of highly crosslinked polyethylene (“X-Lima”) was used in both groups.
51 operations (19 Corail, 32 SP-CL) were done through a posterior incision (Moore) and 24 (19 Corail, 5 SP-CL) through a direct lateral incision (Gammer) according to the preference of the surgeon. All patients were operated on in lateral decubitus position. Patients were encouraged to fully weight-bear as soon as tolerated. 16 surgeons performed the operations.
73 patients (44 males) were operated on unilaterally, 1 female on both sides with a SP-CL stem and a Corail stem (75 hips, ).
Table 1. Baseline demographics and choice of surgical approach. Values are count unless otherwise specified
3 patients left the study before the follow-up at 2 years. 2 of these patients (2 hips) were revised due to infection and 1 patient (1 hip) did not want to participate after 12 months’ follow-up ().
Clinical outcome measures
OHS, EQ-5D, Pain-VAS, Satisfaction-VAS, and EQ-VAS were filled in preoperatively, and at 3, 6, 12, and 24 months. The forms were sent out by mail and then collected during the visit to the outpatient clinic. The patient also filled in the Forgotten Joint Score (FJS) preoperatively and at 12 and 24 months and questions related to the Charnley score preoperatively. Harris Hip Score (HHS) was recorded preoperatively, and after 12 and 24 months’ follow-up. This form was filled in by the physician.
Radiostereometric analysis
During surgery, 7–9 0.8-mm tantalum markers were inserted into the proximal femur. A uniplanar technique was used including 2 digital detectors with an angle of about 40° between the X-ray tubes and with use of cage 77 (RSA Biomedical, Umeå, Sweden). Translation of the femoral head center represented stem migration. The median mean error of rigid body fitting in those patients followed for 2 years was 0.208 (0.046–0.349), the median condition number 28 (17–82) and the median number of used markers in the reference segment 7 (4–9). RSA examinations within the RSA guidelines for mean error of rigid body fitting and condition number were available for all hips at each follow-up occasion presented in . In 71 of the hips double examinations were made to determine precision. The smallest detectable motions in an individual case at the 99% significance limit were 0.16, 0.16, 0.41, and 0.47 mm for medial (+) or lateral (–), proximal (+) or distal (–), anterior (+) or posterior (–), and total (vectorial sum) translations corresponding to the standard deviation of the error times 2.66 and based on a supposed 0-value of the mean difference between the 2 examinations. In the SP-CL group 37/37 accepted/available RSA examinations were available up to 1 year and 36/36 at 2 years. The corresponding shares in the Corail group was 38/38 at 3 months and thereafter 36/36 at all follow-up occasions up to 2 years.
Conventional radiography
Radiographs including AP, true lateral, and pelvic views were obtained pre- and postoperatively, and at 1 and at 2 years. The location of radiolucent lines was related to Gruen regions. The percentage of bone–stem interface occupied by radiolucent lines at 2 years was calculated using measuring tools in mdeskTM (RSA Biomedical, Umeå, Sweden).
Bone densitometry
DXA scans were performed with a Hologic Discovery QDR DXA scanner, software Hologic Discovery Apex, version 12.7.3 (Hologic Inc, Marlborough, MA, USA). Scan mode used was the metal removal program. Changes in bone mineral density between a postoperative examination and at 6 months, 1 (data not shown) and 2 years were related to the 7 Gruen regions. 8 hips (1 SP-CL, 7 Corail) were excluded due to technical problems (hardware breakdown, access to software), leaving 64 hips (35 SP-CL, 29 Corail) with complete data at 2 years.
Statistics
Our primary outcome was OHS at 2 years. Secondary outcomes were stem subsidence at 2 years, FJS at 2 years, EQ-VAS at 2 years, changes of bone mineral density between the postoperative examination and 2 years, and any revision for non-infectious reasons. The remaining outcomes were recorded to facilitate comparison with previous studies.
When this study was planned, we hypothesized that a difference at 2 years in OHS of 5 points could be detected with 79% power based on a sample size of 32 observations in each group and an assumed standard deviation of 7. To allow for dropouts, 80 patients were recruited. Recalculation of the power based on the numbers available (72 hips), and the standard deviations observed resulted in a power of 78%.
The primary variable, OHS at 2 years, was analyzed in a linear model with fixed effects for stem (Corail and SPCL) and OHS preoperatively. A 2nd model was also examined including type of incision, since this distribution was unequal in the 2 stem groups. The estimated mean difference, together with 95% confidence intervals (CI), is presented.
Since most secondary variables had non-normal distribution, we used a Mann–Whitney test and Wilcoxon signed-rank test except for measurements of bone mineral density change, which had a normal distribution in both groups at 2 years. At 2 years, comparison of this outcome was done using a t-test. All statistical tests were 2-sided and performed at the 5% level of significance. Results are presented as means with 95% confidence intervals (CI) or medians with ranges.
The average difference in migration between Corail and SP-CL over all timepoints was also studied using linear mixed models. The model included age, sex, stem, visit (factor variable), and the interaction of stem by visit as fixed effects. In a second model we also added choice of incision as a fixed effect. Patient was a random factor. Unstructured covariance pattern was utilized. The absolute migration values were log transformed in the analysis. The results of the analysis were anti-logarithmized and stated as geometric means and ratio of geometric means together with CI. We used IBM SPSS Statistics (IBM Corp, Armonk, NY, USA) and SAS/STAT (SAS Institute, Cary, NC, USA).
Ethics, registration, data sharing, funding, and potential conflicts of interest
All patients signed giving informed consent according to the Helsinki guidelines. The study was approved by the ethics committee of Gothenburg (nr 140-15), and is registered in the National Clinical Trials database (NCT04599582). Data may be shared after ethical approval and consent of the principal investigator. Funding was received from the Swedish State under the agreement between the Swedish government and the county councils, the ALF agreement (721791), IngaBritt and Arne Lundberg Research Foundation, Felix Neubergh Foundation, and Link Germany. Individual potential conflicts of interests: KR, MM, and EN: none, JK: previous board member RSA Biomedical, Sweden.
Results
Clinical results
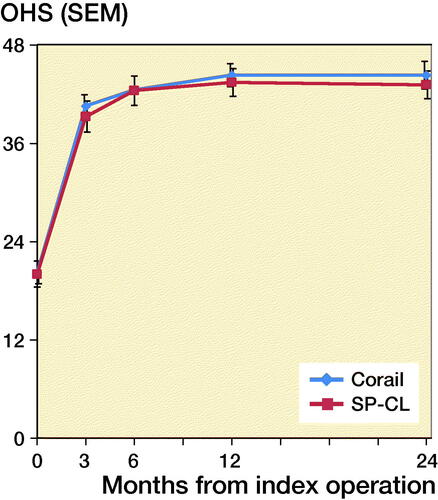
At 3 months the OHS had almost doubled in both groups, from median values of about 20 to about 40 ( and Table 2, see Supplementary data). The increase continued between 3 and 6 months in both groups (p < 0.001). Thereafter the median values increased slightly and without statistical significance at 2 years. In the linear model, the estimated mean difference at 2 years was –0.70 (CI –4.3 to 2.9) and after adjustment for incision 0.04 (CI –4.0 to 4.0, Table 3, see Supplementary data). Reduced pain, improved general health, and degree of satisfaction with the operation were observed 3 months after the operation without any further substantial changes on the following occasions (, Table 2, see Supplementary data).
At 2 years none of the PROMs (OHS, FJS, EQ-5D, EQ-VAS, Pain-VAS, Satisfaction-VAS) differed between the 2 groups. The mean and median Harris Hip Scores at 2 years were close to equal (Table 2, see Supplementary data). Up to 2 years, 2 hips with Corail stem were reoperated on due to infection, but none of the stems for non-infectious reasons.
Radiostereometric results
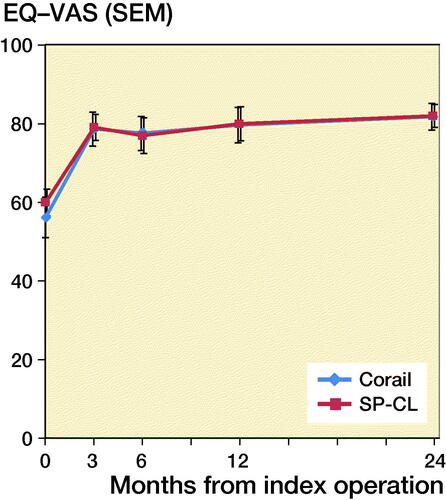
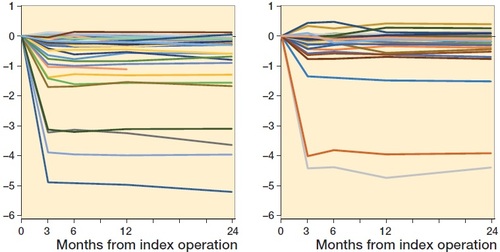
In both groups the mean and median femoral head center migration had a medial, distal, and posterior direction ( and , Table 4, see Supplementary data). Almost all this migration occurred during the first postoperative 3 months. At 2 years there was no statistically significant difference between the 2 groups for any of the translation variables recorded.
Figure 4. Mean medial–lateral (left), proximal–distal (middle), and anterior–posterior migration (right) up to 2 years in 36 SP-CL and 35 Corail stems with RSA data on each follow-up occasion.
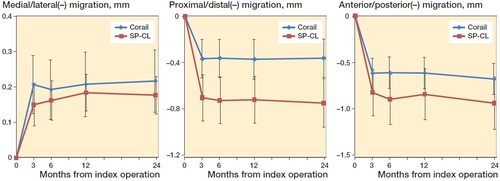
Figure 5. Proximal–distal case-by-case migration up to 2 years in individual SP-CL and Corail stems.
The median migration during the 2nd year of observation along the 3 cardinal axes was less than 0.1 mm without any statistical significant difference (Table 4, see Supplementary data). 5 SP-Cl stems and 10 Corail stems out of 36 with complete data in each group showed migration above the 99% detection level after the 1-year follow-up. In this subgroup the median value of translation along any of the 3 cardinal axes varied between –0.07 and 0.04 mm (SP-CL) and –0.02 and 0.00 (Corail), and the corresponding observed minimum and maximum values between –0.41 and 0.51 (SP-CL) and –0.55 and 0.60 mm (Corail).
Evaluation including the series of observation (repeated measurement of overall treatment effect) in the 1st linear mixed model revealed that the absolute migration values along any of the cardinal axes or the total translations were similar between the SP-CL and Corail stems (Table 5, see Supplementary data). After addition of incision, statistically significantly more proximal–distal stem migration was observed with use of the SP-CL stem.
Standard radiography
Postoperatively, radiolucent lines were not observed around any of the hips. After 2 years, radiolucent lines on either the AP or the lateral view had appeared around 7 SP-CL stems and 9 Corail stems (Table 6, see Supplementary data).
At 2 years, and in those cases with any visible radiolucent lines, their relative length on the AP view was 5% (1 SP-CL stem) and median 7% (Citation6–16) (8 Corail stems). On the lateral view the corresponding median values were 10% (Citation6–13) (6 SP-CL stems) and 9% (Citation7–17) (8 Corail stems).
Bone mineral density (BMD)
On the lateral side of the stem (Gruen regions 1–3) and at the tip of the stem (region 4) the mean bone mineral density had decreased at 2 years in both groups without any statistically significant difference between them (Table 7, see Supplementary data). On the medial side, SP-CL stems showed a mean decrease of BMD in regions 6 and 7, whereas the Corail stem showed a decrease only in region 7. The observed differences were statistically significant for region 7 (p = 0.003).
Discussion
In this randomized evaluation of THAs performed either with the SP-CL or the Corail stem, we could not observe any difference in primary outcome, OHS, and the other clinical outcome variables were similar. The SP-CL stems showed more pronounced early migration and lost more bone mineral in the calcar region.
The evaluation with various PROM instruments in combination with stem migration by RSA and measurements of bone mineral density changes is a strength of this study. Use of a single cup design can also be regarded as an advantage since this will increase the probability that any differences, if present, at first hand could be supposed to be caused by the choice of stem.
During the postoperative course up to 2 years, the evolution of OHS, EQ-VAS, Pain-VAS, and patient satisfaction was similar in the 2 groups. At 2 years the mean and median OHS difference was close to 0. This is far from what has been regarded as a clinically relevant group difference (Citation7).
Compared with the OHS, the FJS has been found to have less ceiling effect (Citation8, Citation9), but suffers from a more pronounced floor effect. FJS has also been found to be more responsive to changes in the postoperative course after THA, probably because it evaluates whether the patient perceives the presence of their operated hip. In the evaluation of a newly designed stem the FJS might therefore be a more sensitive tool than the OHS. When our study was planned in 2015, the minimal important change or difference for FJS was not known and has, according to our knowledge, only been studied for patients undergoing total knee arthroplasty (Citation10, Citation11).
The interpretation of uncemented stem migration is still controversial. van der Voort et al. (Citation12) performed a systematic review of RSA studies of early stem migration and survival studies using long-term aseptic revision rates due to loosening as outcome variable. The authors concluded that there were not enough published results to draw conclusions about any influence of early migration and the revision of uncemented or cemented polished force-closed stems. Nonetheless, the early migration of uncemented stems has been the subject of numerous studies (Citation13–19). These studies have revealed 3 basic types of distal stem migration: early stability, early subsidence followed by stability within about 1 year, and continuous subsidence resulting in clinical loosening. In the 1st group, the proximal–distal migration of the stem stays within 0.15–0.2 mm in both directions and appears to do so for up to at least 7 years (Citation17). In the 2nd group, the subsidence is more variable. It often stays within 0.5 mm, but it might amount to as much as about 20 mm (Citation20).
De Vries et al. (Citation21) also performed a meta-analysis of hip arthroplasty survival and RSA studies including cemented and uncemented stems. In the uncemented group, the stem subsidence showed great variability, between 0.01 and 1.8 mm among 7 different stem designs. No specific threshold for acceptable migration was presented. They called for more standardized reporting and more long-term follow-up studies of original RSA cohorts.
In our study all migration variables measured were numerically slightly lower for the Corail than for the SP-CL stem, but in the main analysis without statistically significant difference. After stratification for choice of incision, we observed significantly more subsidence with the SP-CL stem. Whether this difference can be related to stem design or is technique or surgeon related remains unknown. This question cannot be further explored due to the small number of cases operated on with a direct lateral approach and an SP-CL stem and due to study design, where choice of incision was left to the discretion of the surgeon. Between the 1- and 2-year follow-up 10 Corail stems and 5 SP-CL stems still showed detectable migration, which adds to the uncertainty concerning the clinical significance of increased early subsidence of the SP-CL stems. The subsidence during the 2nd year was small overall and did not in any case exceed 0.27 mm. We do not know if this migration occurred only early or more slowly throughout the 2nd postoperative year. 3 of the 15 stems with detectable migration during the 2nd year also had radiolucent lines. Whether these stems are at risk of future clinical loosening remains to be seen. Recently Sandberg et al. (Citation1) used a new CT-based method, Sectra CT Micromotion Analysis (CTMA), to measure subsidence of 20 SP-CL stems up to 1 year after implantation. Their method had about the same precision as observed by us. They observed a median subsidence of 0.6 mm at 1 year. Although these figures are 2–3 times higher than found by us almost all stems seemed to have reached a stable position after the follow up at 3 months. Consistent with our finding of a posterior migration of the femoral head, Sandberg et al. observed an internal rotation of the stem when related to a fixed femur.
Heyland et al. (Citation22) performed a finite element analysis and compared the strain distribution among the Corail, CLS, and 3 modifications of the SP-CL stems with use of loads derived from gait lab data. Their modelling showed that the SP-CL stem had a more even load transfer than the Corail stem and less focus of stress. We could not verify that use of the SP-CL stem loaded the medial side of the femur in a more physiological way as these stems tended to have more loss of BMD in region 6 and definitely so in region 7 when compared with femurs with a Corail stem. The reason for this discrepancy is not known. It should, however, be noted that Heyland et al. (Citation22) based their calculations on a standard Corail stem without collar, whereas our study included stems both with and without a collar and the coxa vara and high offset versions of the Corail stem.
Limitations
We used the OHS as primary outcome, because we primarily wanted to evaluate the clinical outcome from the patient’s perspective. Based on the small group difference observed it seems unlikely that we would be able to verify a group difference of clinically significant magnitude by inclusion of a bigger sample. Absent difference in clinical outcome between the SP-CL and Corail groups was also supported with use of other patient- and examiner-reported outcomes.
During the time for our study the SP-CL stem with 126° CCD (caput–collum–diaphyseal angle) and only implants with standard neck length were available. We tried to compensate for this by only recruiting hips suitable for the SP-CL design available, nevertheless this means that our study lost some external validity.
Our RSA measurements were based on femoral head translations, which means that we had no information on stem rotations or translation of other parts of the stem (e.g., the shoulder or the tip). On the other hand, much of the basic information regarding stem migration was based on the technique used by us (Citation13, Citation23, Citation24) and we do not think that a more comprehensive evaluation would have changed the overall conclusions of our study. Roughly medial–lateral femoral head translation could be interpreted as varus–valgus tilting and anterior–posterior translations as ante- and retroversion. The true relationship between head translations and stem rotations is, however, complex and cannot be accurately computed because the center of stem rotation was not known.
Conclusion
We found similar clinical results with use of either the SP-CL or the well-documented Corail stem. The clinical relevance of a tendency to increased subsidence of the SP-CL stem during the postoperative 3 months is difficult to interpret, not least against the background of similar migration and number of stable stems between 1 and 2 years. A more physiological loading resulting in less loss of BMD with use of the SP-CL stem could not be verified. We think that the SP-CL stem should be studied in a multi-center setting, before being accepted for general use.
iort_a_1993606_sm9047.pdf
Download PDF (37 KB)KR: collecting data, statistical analyses, writing and editing manuscript. EN: statistical analysis and editing manuscript. MM: editing manuscript and statistical analysis. JK: study design, statistical analysis, writing and editing manuscript.
Acta thanks Inari Laaksonen, Marc J Nieuwenhuijse and Nienke Wolterbeek for help with peer review of this study.
Supplementary data
Tables 2–7 are available as supplementary data in the online version of this article, http://dx.doi.org/10.1080/17453674.2021. 1993606
- Sandberg O, Tholen S, Carlsson S, Wretenberg P. The anatomical SP-CL stem demonstrates a non-progressing migration pattern in the first year: a low dose CT-based migration study in 20 patients. Acta Orthop 2020: 1–6.
- Tootsi K, Lees L, Geiko B, Martson A. Intraoperative complications in total hip arthroplasty using a new cementless femoral implant (SP-CL(R)). J Orthop Traumatol 2020; 21(1): 8.
- de Reus I M A, Sprekenbrink-Spooren A, van Steenbergen L N, Denissen G W A, Rijnsburger E, van der Togt C R. Online LROI annual report 2019; 2019. https://www.lroi-report.nl/
- Graves S, de Steiger R, Lewis P L. Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR). Hip, Knee & Shoulder Arthroplasty 2019. http://www.aoa.org.au/
- Kärrholm J, Rogmark C, Nauclér E, Vinblad J, Mohaddes M, Rolfson O. Svenska Höftprotesregistret Årsrapport 2018; 2019. https://shpr.registercentrum.se/
- Reed M, Howard P, Brittain R, Lawrence S, Stonadge J, Wilkinson M, et al. National Joint Registry 17th Annual Report 2020. https://reports.njrcentre.org.uk/
- Beard D J, Harris K, Dawson J, Doll H, Murray D W, Carr AJ, et al. Meaningful changes for the Oxford hip and knee scores after joint replacement surgery. J Clin Epidemiol 2015; 68(1): 73–9.
- Hamilton D F, Giesinger J M, MacDonald D J, Simpson A H, Howie C R, Giesinger K. Responsiveness and ceiling effects of the Forgotten Joint Score-12 following total hip arthroplasty. Bone Joint Res 2016; 5(3): 87–91.
- Larsson A, Rolfson O, Kärrholm J. Evaluation of Forgotten Joint Score in total hip arthroplasty with Oxford Hip Score as reference standard. Acta Orthop 2019; 90(3): 253–7. 1599252.
- Ingelsrud L H, Roos E M, Terluin B, Gromov K, Husted H, Troelsen A. Minimal important change values for the Oxford Knee Score and the Forgotten Joint Score at 1 year after total knee replacement. Acta Orthop 2018; 89(5): 541–7.
- Holtz N, Hamilton D F, Giesinger J M, Jost B, Giesinger K. Minimal important differences for the WOMAC osteoarthritis index and the Forgotten Joint Score-12 in total knee arthroplasty patients. BMC Musculoskelet Disord 2020; 21(1): 401.
- van der Voort P, Pijls B G, Nieuwenhuijse M J, Jasper J, Fiocco M, Plevier J W, et al. Early subsidence of shape-closed hip arthroplasty stems is associated with late revision: a systematic review and meta-analysis of 24 RSA studies and 56 survival studies. Acta Orthop 2015; 86(5): 575–85.
- Önsten I, Carlsson A S, Sanzen L, Besjakov J. Migration and wear of a hydroxyapatite-coated hip prosthesis: a controlled roentgen stereophotogrammetric study. J Bone Joint Surg Br 1996; 78(1): 85–91.
- Luites J W, Spruit M, Hellemondt G G, Horstmann W G, Valstar E R. Failure of the uncoated titanium ProxiLock femoral hip prosthesis. Clin Orthop Relat Res 2006; 448: 79–86.
- Ström H, Nilsson O, Milbrink J, Mallmin H, Larsson S. Early migration pattern of the uncemented CLS stem in total hip arthroplasties. Clin Orthop Relat Res 2007; 454: 127–32.
- Baad-Hansen T, Kold S, Olsen N, Christensen F, Søballe K. Excessive distal migration of fiber-mesh coated femoral stems. Acta Orthop 2011; 82(3): 308–14.
- Thien T M, Thanner J, Kärrholm J. Fixation and bone remodeling around a low-modulus stem: seven-year follow-up of a randomized study with use of radiostereometry and dual-energy X-ray absorptiometer. J Arthroplasty 2012; 27(1): 134–42 e1.
- Lazarinis S, Mattsson P, Milbrink J, Mallmin H, Hailer N P. A prospective cohort study on the short collum femoris-preserving (CFP) stem using RSA and DXA: primary stability but no prevention of proximal bone loss in 27 patients followed for 2 years. Acta Orthop 2013; 84(1): 32–9.
- Budde S, Seehaus F, Schwarze M, Hurschler C, Floerkemeier T, Windhagen H, et al. Analysis of migration of the Nanos(R) short-stem hip implant within two years after surgery. Int Orthop 2016; 40(8): 1607–14.
- Schewelov T, Ahlborg H, Sanzen L, Besjakov J, Carlsson A. Fixation of the fully hydroxyapatite-coated Corail stem implanted due to femoral neck fracture: 38 patients followed for 2 years with RSA and DEXA. Acta Orthop 2012; 83(2): 153–8.
- de Vries L M, van der Weegen W, Pilot P, Stolarczyk P A, Sijbesma T, Hoffman E L. The predictive value of radiostereometric analysis for stem survival in total hip arthroplasty: a systematic review. Hip Int 2014; 24(3): 215–22.
- Heyland M, Checa S, Kendoff D, Duda G N. Anatomic grooved stem mitigates strain shielding compared to established total hip arthroplasty stem designs in finite-element models. Sci Rep 2019; 9(1): 482.
- Mjöberg B, Selvik G, Hansson L I, Rosenqvist R, Önnerfalt R. Mechanical loosening of total hip prostheses: a radiographic and roentgen stereophotogrammetric study. J Bone Joint Surg Br 1986; 68(5): 770–4.
- Kärrholm J, Borssen B, Löwenhielm G, Snorrason F. Does early micromotion of femoral stem prostheses matter? 4–7-year stereoradiographic follow-up of 84 cemented prostheses. J Bone Joint Surg Br 1994; 76(6): 912–17.