ABSTRACT
Objectives
Blood pressure (BP) values ≥120/70 mmHg considerably increase the risk of pulmonary hypertension and renal dysfunction in Sickle Cell Disease (CSD) patients and ultimately increased morbidity and mortality. This has led to the development of the term relative systemic hypertension (RSH). RSH was defined as Systolic BP 120–139 mm Hg or diastolic BP 70–89 mm Hg, whereas systemic hypertension is defined as Systolic BP ≥ 140 mm Hg or diastolic BP ≥ 90 mm Hg. Systematic identification of BP variations and risk factors in SCD patients could promote effective management. This review aimed to identify factors associated with BP variation among SCD patients.
Methods
We searched PubMed, Scopus, Web of Science, and Google Scholar up to December 2020 with no geographical or language restrictions. Two reviewers independently screened and summarized data from eligible studies.
Results
Advancing age, gender, higher body weight, hemoglobin, eGFR, triglycerides, greater hematocrit, higher blood viscosity, history of blood transfusion, and targeted variants in DRD2 and MIR4301 genes were independently associated with the risk of hypertension in SCD patients.
Conclusion
Interventions that consider these risk factors may potentially contribute to lower BP pressure in SCD patients and prevent the development of severe complications.
1. Introduction
Sickle cell disease (SCD) is an inherited, autosomal, recessive condition caused by several mutations in the β-globin gene (HBB). SCD encompasses any one of the syndromes, which arise from the mutation that leads to substitution of valine for glutamic acid in a single nucleotide polymorphism (SNP) in the sixth codon of the HBB gene on chromosome 11. This mutation leads to the production of sickle hemoglobin (HbS), with altered physical properties of hemoglobin (Hb) [Citation1–3]. According to a systematic review by the Global Burden of Disease Study, 3.2 million people live with SCD, 43 million people have sickle cell trait (i.e. are carriers of the mutation), and 176,000 people die due to SCD-related complications per year [Citation4]. The most common and the most severe form of SCD is homozygous HbSS (sickle cell anemia), resulting from the inheritance of βS gene from both parents. The HbSS genotype accounts for 70% of the cases of SCD in patients of African ancestry. Other forms of SCD include the inheritance of the βs gene in combination with hemoglobin C or β- Thalassemia mutations, resulting in HbSC or HbSβThal genotypes, respectively [Citation1,Citation2].
SCD patients show substantial heterogeneity in the presentation and clinical course of the disease [Citation2]. Typically, the pathobiology of SCD is a vicious cycle of four major processes. First, under deoxygenation conditions, HbS molecules polymerize to form bundles. The polymer bundles form long fibers that impair the erythrocyte membrane, leading to erythrocyte sickling. Second, the normally freely flowing cytosol of the erythrocyte becomes viscous making the cell much less deformable. This leads to the blockage of blood vessels, disrupting the blood supply, referred to as vaso-occlusion. Thirdly, the polymer bundles also promote hemolysis causing chronic anemia with Hb levels ranging from 6 to 11 g/dl. The severity of this anemia is dependent on primary genotype and genetic modifiers of fetal hemoglobin levels, the strongest known modifier of the SCD clinical expression. Patients with higher rates of hemolysis are more likely to develop vascular injury and multi-organ dysfunction. Finally, hemolysis by-products such as erythrocyte damage-associated molecular patterns (eDAMPS) along with ischemia-reperfusion injury caused by vaso-oclussion, promote sterile inflammation and oxidative stress. These events further amplify vaso-occlusion through a feedback loop by promoting adhesion of neutrophils, platelets, and endothelial cells. These molecular, cellular, and biophysical processes work in synergy to promote acute and chronic pain, ischemic reperfusion injury, and infarctions of vital organs, such as spleen, heart, kidneys, liver, muscle, brain, lung, and bone.
While in sub-Saharan Africa, without treatment, most babies born with SCD rarely live beyond 5 years of age [Citation5,Citation6] the life expectancy has improved drastically in high-income countries; This is mainly due to the widely implemented new-born screening, followed by a comprehensive care, including penicillin prophylaxis, pneumococcal immunization, availability of red cell transfusions, and use of the fetal hemoglobin-inducing therapy Hydroxyurea. Some patients have the potential to live well into their 7th decade [Citation7]. However, with improved life expectancy, cardiovascular complications become more common, due to persistent intravascular hemolysis [Citation8]. Cardiovascular complications such as proliferative systemic vasculopathy, left ventricular diastolic dysfunction and pulmonary hypertension have been reported. These factors are known predictors of mortality in SCD patients [Citation7,Citation9].
SCD patients commonly have lower diastolic, systolic, and mean blood pressure in comparison to the general population. Notably, the incidence of pulmonary hypertension and renal insufficiency at relatively normal BP (≥120/70 mmHg) have been reported in some SCD patients [Citation10]. Previous studies in SCD patients have labeled this phenomenon ‘relative systemic hypertension’ (RSH) [Citation10]. RSH was defined as Systolic BP (SBP) 120–139 mm Hg or diastolic BP (DBP) 70–89 mm Hg and systemic hypertension as SBP 140 mm Hg or DBP 90 mm Hg or higher.
BP is a potential modulator of clinical severity in SCD patients, recurrent deleterious and loss of function mutation with genes associated with lowering BP has been recently associated with long survival in SCD in Africa [Citation11]. Identifying factors associated with BP variation is key to controlling BP, as well as preventing associated causes of mortality in SCD patients. Herein, we present a systematic review of risk factors associated with BP variation in SCD patients.
2. Patients and methods
2.1. Protocol registration
This review was registered with the International Prospective Register of Systematic Reviews (PROSPERO), registration number CRD42020168798.
2.2. Search strategy and eligibility criteria
The Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) served as a template for reporting the present review [Citation12].
Two reviewers (AN and CO) with the help of an expert llibrariandeveloped a comprehensive literature search strategy () in the following databases:
MEDLINE/PubMed.
Scopus.
Web of Science.
The PubMed database search syntaxes are presented in Appendix 1. This syntax is a combination of MeSH terms, keywords, and tags and was adapted for other databases. AN and CO searched for studies using the following three concepts: SCD patients, risk factors, and blood pressure. The Boolean operators ‘OR’ were used with synonyms within each concept and then the search results for different concepts were combined with the ‘AND’ operator. In addition, AN and CO searched other sources using Google Scholar search engine and checked the reference lists of relevant studies. AN and CO completed the search process by manually searching Google. All the identified articles were imported into Mendeley (reference manager) software. Duplicate studies from the different electronic databases were removed through the Mendeley reference manager. Independently, AN and CO screened titles and abstracts of the search results for potentially eligible studies. Full texts of the remaining articles were retrieved and further assessed independently by AN and CO using eligibility criteria. Any discrepancies were resolved through consensus.
The following exclusion and inclusion eligibility criteria were used to screen full text:
Only observational studies addressing the risk factors of blood pressure variation among SCD patients were included.
Risk factors included but not limited to age, sex, demographic and genetic variants, epigenetic, socio-economic, psychological, anthropometric, biological, and disease-related factors.
We excluded review articles without original data, case reports and expert opinion commentaries, and studies whose main outcome was not BP in SCD patients.
Eligible studies were included regardless of language, year of publication or geographical location.
2.3. Assessment of the methodological quality
The Newcastle-Ottawa Scale (NOS) and Q-Genie were used to evaluate the methodological quality of observational and genetic studies included in this review, respectively. Since there was no validation study to provide a cutoff score for rating low-quality studies, we considered 0–4, 5–7, and 8–10 stars as indicative of high, moderate, and low risk of bias, respectively. Two investigators (AN and CO) independently assessed the study quality and disagreements were resolved by consensus.
2.4. Data extraction
The study inclusion criteria were the study population, the study design, the country, the outcomes. Relevant data were independently extracted by the two reviewers (AN and CO) using a standardized extraction form in Microsoft Excel. The data extracted included the citation, language of the paper, study period, study location, study objectives, study design, study period, characteristics of participants, sample size, and sampling technique, explanatory and outcome variables, and the major findings. Specific data such as demographic and socio-economic characteristics, any anthropometric measurements, and blood pressure measurement procedures were also extracted. The risk factors that are associated with BP variations were categorized into demographic, anthropometrical, biological, and genetic.
2.5. Data synthesis
We conducted as a metanalysis and a narrative synthesis where a meta-analysis was not possible and descriptive synthesis. The descriptive synthesis included (a) PRISMA Flow; (b) a quality assessment; (c) a description of the study characteristics and findings (); and (d) a narrative synthesis. Furthermore, the results of meta-analysis are presented as a forest plot (). Ninety-five-percent confidence intervals (CI) and the standardized mean difference (std Mean difference) were calculated for each study and used for the meta-analysis. We use inverse-variance weighted random effects meta-analysis to pool the study-specific estimates. The choice of a random effects model was made a priori to allow for inter-study heterogeneity of results. The inter-study heterogeneity was evaluated by the X2 test on Cochrane’s Q statistic and its magnitude estimated using the I2 values. These values represent a percentage of variation in effect size between studies that can be attributed to genuine variability rather than chance. The I2 values of 25%, 50%, and 75% represent low, medium, and high heterogeneity, respectively. Quantitative data was pooled in a statistical meta-analysis using Review Manager (RevMan) software.
Figure 2. BP indices in SCD patients versus controls, (a) = systolic BP, (b) = diastolic BP, (c) = mean arterial pressure; (d) = Pulse rate, (e) = Pulse pressure.
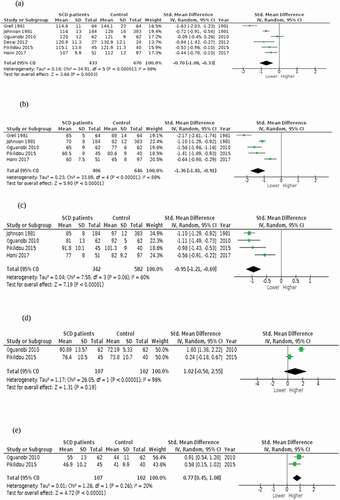
Table 2. Characteristics of included studies
3. Results
3.1. The review process
The database search yielded 2477 citations and further 30 articles were identified by manual screening of citations (). After the elimination of duplicates, 2420 records remained. After screening titles and abstracts, we found that 2325 records were irrelevant and excluded them. After assessing the full texts of the remaining 95 papers for eligibility, 77 of them were excluded. Sixteen studies were part of the qualitative synthesis, and seven studies were included in the meta-analysis ().
3.2. Assessment of risk of bias
All 16 studies included in the review were considered for critical appraisal. The results of the critical appraisal were used to generate a description of the risk of bias for each included study (). Studies were classified as having low (n = 2), moderate (n = 12) and high (n = 2) risk of bias. In most cases, the selection of non-representative samples was the source bias.
Table 1. Risk of bias in the included studies
3.3. Description of study characteristics
The studies’ sample sizes ranged from 38 to 3317 participants. Study participants’ mean age ranged from 6 to 81 years. Included studies were published between 1981 and 2018. Studies had a cross-sectional (n = 9), retrospective cohort (n = 6), and genome-wide meta-analysis (n = 1) design. The study settings included outpatient or in-hospital SCD participants. None of the studies included community-based recruitment of SCD participants. Studies were carried out in North America (n = 12), in Africa (=3) and Europe (n = 1). Details on the characteristics of the 16 included studies are reported in . Studies have described BP and risk factors associated with either SCD patients versus healthy controls or SCD patients only.
3.4. Meta-analysis
Due to limited data, we were only able to conduct a meta-analysis on seven studies that looked at BP in SCD patients versus controls. The meta-analysis results are presented in . From the pooled results systolic, diastolic, and mean arterial pressure were lower in SCD patients compared to control groups, whereas and pulse rate and pulse pressure were higher in SCD patients compared to control groups. Heterogeneity (I2) ranged from 20% to 96%, indicating substantial heterogeneity between studies (). In the sensitivity analysis, we identified outlier [Citation14]. The study substantially affected the heterogeneity of the pooled results. After excluding the study, the heterogeneity decreased from 96% to 60%. Furthermore, mean arterial pressure remained lower in SCD patients than in controls. We were unable to conduct a sensitivity/ subgroup analysis for pulse rate and pulse pressure, due to having fewer studies. The results that were not included in the meta-analysis are summarized in the narrative synthesis below.
3.5. Narrative synthesis
Although BP is a multifactorial condition, we present our results in categories of risk factors, namely demographic, anthropometric, biological, and genetic.
3.5.1. Demographic risk factors
Age was assessed in four studies. Studies have reported a lower BP in SCD patients than age- and sex-matched controls [Citation15–18]. However, a common finding was that age is associated with BP in SCD and that the BP increases rapidly with advancing age in SCD patients starting in their early twenties. Gender was assessed in five studies [Citation16,Citation18–21]. One study reported a significantly lower SBP in male compared to females SCD patients, but after adjusting for weight this difference disappeared (P = 0.050) [Citation21]. The expected DBP rise with advancing age was not present in male participants [Citation18]. Pulse pressure was higher in males of all ages [Citation6,Citation16,Citation22].
3.5.2. Anthropometric risk factors
BMI was assessed in five studies [Citation15,Citation17,Citation19,Citation20,Citation23]. Studies have found that, after controlling for other covariates, SBP was significantly associated with BMI (P < 0.0001) [Citation15]. BMI is independently associated with hypertension [Citation17,Citation20,Citation23]. In addition, SCD patients with elevated BP had significantly higher body weight, waist, and neck circumference (p < 0.050) [Citation19].
3.5.3. Biological risk factors
After controlling for other covariates, three studies found that DBP was independently associated with the level of hemoglobin [Citation15,Citation17,Citation23,Citation24]. DBP showed a positive correlation with age, body mass index in those over 17, hemoglobin concentration in women, blood urea nitrogen in males under 18, and a negative correlation with estimated glomerular filtration rate (eGFR) in patients under-age 18, SBP was negatively correlated with fetal hemoglobin in males over 17 [Citation23]. Triglycerides increased hematocrit and higher blood viscosity were independent risk factors for RSH in SCD patients [Citation24,Citation25]. Furthermore, pulse pressure and a history of blood transfusion were independently associated with systemic hypertension in SCD patients [Citation17]. Markers of hemolysis are associated with a higher pulse pressure in SCD patients [Citation25]. Augmentation index, a measure of arterial stiffness, was significantly higher in SCD patients compared with healthy controls (p < 0.050) [Citation22]. In the multivariate analysis, there was a significant correlation between SBP and age, BMI, history of hypertension, and absolute neutrophil count (estimate: 21.18, P = 0.023) [Citation15].
3.5.4. Genetic risk factors
We found limited data investigating the underlying genetic factors contributing to blood pressure variation, particularly in SCD patients. We found one study, which was a single genome-wide meta-analysis of SBP. The study included 1617 African-American SCD children and identified a suggestive candidate locus at rs7952106 in DRD2 gene and in MIR4301 gene [Citation26].
3.5.5. Clinical complications and blood pressure
Gordeuk et al. found that patients with SBP > 120 or DBP > 70 mm Hg may represent relative hypertension in SCD patients and identify patients at increased risk for pulmonary arterial hypertension and renal dysfunction. When they stratified patients by tricuspid regurgitant jet velocity (TRV) and serum creatinine concentration according to three blood pressure categories (Normal, RSH, systemic hypertension), TRV was 2.5 m/sec in 27% of the patients with normal BP, in 37% of the patients with RSH, and in 93% of the systemic patients with hypertension. Serum creatinine concentration was 1.0 mg/dL or higher in 7% of the patients with normal BP, in 17% with the patients with RSH and in 50% of the patients with systemic hypertension. During the two-year follow-up evaluation, systemic hypertension was observed in (16%) of those with RSH during the initial evaluation. Over 2 years of follow-up, there were trends for more frequent progression to elevated TRV or creatinine values in RSH and systemic hypertension groups [Citation10]. DeBaun et al., reported that higher baseline systolic blood pressure (P = 0.018) and male sex (P = 0.030) were statistically significantly associated with an increased risk of silent cerebral infarcts [Citation27]. Contrary to similar studies, Kuma et al., found a high prevalence of RSH and hypertension with a relatively low frequency of renal insufficiency, and no association between RSH and stroke [Citation16]. Novelli et al., found that higher pulse pressure was associated with markers of hemolysis, elevated serum creatinine and with proteinuria in SCD patients [Citation25]. Additionally, Kuma et al., found a higher pulse pressure in males of all ages compared to females [Citation10]. A recent cross-sectional study looking at the association between twenty-four-hour ambulatory BP monitoring and cerebrovascular outcomes found an association between nocturnal hypertension and a higher prevalence of silent cerebral infarcts (SCI), and stroke in children with SCD [Citation28].
4. Discussion
To our knowledge, this is the first reported systematic review and meta-analysis that provides information on a wide range of risk factors associated with BP variation among SCD patients. Advancing age, gender, BMI, higher body weight, waist, and neck circumference, hemoglobin, BUN, eGFR, triglycerides, greater hematocrit, higher blood viscosity, absolute neutrophil count, history of blood transfusion, and potentially variant in MIR4301 gene were independently associated with the risk of RSH or systemic hypertension in SCD patients. Furthermore, our pooled estimates illustrate that SBP, DBP, and mean arterial pressure were lower in SCD patients. Pulse pressure and pulse rate were higher in SCD patients compared to the general population, with heterogeneity ranging from low to high.
Previous studies have explained that lower BP in SCD patients may potentially be due to renal tubular defects or hyposthenuria, increased Sodium and water loss [Citation18,Citation23], lower BMI, and alterations in peripheral vascular resistance and vasodilation [Citation21] which affects cardiac parameters including cardiac output, cardiac index, ejection fraction, and stroke volume. It is well documented that SCD patients with RSH or Systemic hypertension are at increased risk of renal insufficiency, pulmonary hypertension, and silent cerebral infarction or stroke [Citation10,Citation16,Citation25,Citation27]. It has also been reported that the risk of occlusive stroke increases with SBP. No significant relationship between DBP and occlusive stroke was observed. No association was found between BP and a history of painful vaso-occlusive crisis. However, an association between increased triglycerides (a known risk factor for RSH and systemic hypertension) and the occurrence of vaso-occlusive crises was observed [Citation20]. In addition, pulse rate and pulse pressure being higher in SCD patients is a concern because pulse pressure is a well-documented predictor of sudden death [Citation29,Citation30]. Akingbola et al., reported that the history of stroke was associated with higher SBP and BMI on univariate analyze (p < 0.006) [Citation31]; however, Kuma et al., found a high prevalence of RSH and hypertension with a relatively low frequency of renal insufficiency, and no association between RSH and stroke. The study attributed these differences mostly to selection bias and under documentation of complications in their study design [Citation16].
In SCD patients, elevated pulse pressure has been reported to be associated with hemolysis, proteinuria, and chronic kidney disease [Citation16,Citation25]. Elevated TRV and serum creatinine concentrations in RSH and systemic hypertension in SCD [Citation10] reinforces the importance of systemic blood pressure as a predictor of kidney deterioration in SCD and pulmonary arterial hypertension.
This review also highlights a wide range of risk factors associated with BP variation in SCD patients and subsequently leads to complications described above. Previous studies show that the risk of RSH and systemic hypertension in SCD patients increases with advancing age, with an onset in the early twenties [Citation23,Citation32]. In addition, gender-dependent factors, such as nitric oxide production, which is higher in females compared to males, may explain the higher pulse pressure observed among SCD male patients [Citation33]. Nitric oxide is thought to be important in maintaining vasomotor tone, limiting platelet aggregation, inhibiting ischemia-reperfusion injury, and modulating endothelial adhesion molecule expression [Citation34]. Therefore, being an adult and/or male SCD patient could potentially increase the risk of developing RSH and Systemic Hypertension. Furthermore, SCD patients with elevated BP have higher waist, neck circumference, elevated BMI, history of blood transfusion, and prior diagnosis [Citation17,Citation19,Citation35]. Elevated BP has been reported to be associated with a history of stroke [Citation31], higher prevalence of silent cerebral infarcts (SCI), and stroke in children with SCD [Citation28]. Therefore, the ability to identify individuals prior to the development of cardiovascular complications is of paramount importance, particularly in SCD patients [Citation35].
Further evidence shows a correlation between biological factors (hemoglobin, hematocrit, and triglycerides) and BP variation. However, this correlation varies among age and sex subgroups in SCD patients. In the RSH and systemic hypertension group, there is an increase in blood viscosity compared to SCD patients in the normal group [Citation20]. Increased blood viscosity in the RSH and systemic hypertension groups may be due to lower hemolytic rate, which leads to elevation of hematocrit and hemoglobin levels [Citation20]. As the viscosity increases, there is a negative impact on blood flow, which may worsen cardiovascular function [Citation36]. Interventions such as hydroxyurea known to modulate hemolytic rate and increase levels of hemoglobin do not increase blood viscosity in SCD patients and positively impacts the rheology properties of sickle red blood cells (RBC) [Citation2,Citation20]. However, these findings are generalizable to patients having a hemoglobin increase of around 1 g per deciliter (g/dl) under hydroxyurea [Citation2]. Therefore, blood flow may be an important factor for the diagnosis and management of RSH and systemic hypertension in SCD patients [Citation36]. The importance of rheology and vascular complications will require to be further investigated. Additionally, alpha-thalassemia can also modulate the hemolytic rate by decreasing the tendency of HbS to polymerize, which results in increased hemoglobin concentrations [Citation36]. The protective effect of alpha-thalassemia varies from reduced occurrence of stroke, gallstones, leg ulcers, and priapism [Citation2]. However, elevated hematocrit and blood viscosity may be associated with increased frequency of pain in patients with alpha-thalassemia [Citation2,Citation20,Citation37].
The findings on genetic factors relating to BP in SCD patients are consistent with a previous review [Citation38]. Since genetic factors were only investigated in one study, no solid inference can be drawn on whether the same genetic variants influence BP across different human populations. This highlights the urgent need for studies aimed at identifying specific SNPs associated with BP and cardiovascular complications in SCD patient populations, particularly in Africa.
Even though we conducted a comprehensive search and most of our included observation studies were low to moderate risk of bias, this review is not without limitations. When we pooled point estimates in a meta-analysis, we observed heterogeneity ranging from low to high, thus limiting our interpretation of pooled estimates. Contributors to this unexplained heterogeneity may be due to a wide range of study methodologies, study settings, populations, and periods studied in our included studies. Most of the included studies were from North America, which highlights a gap in comparable studies from lower-income countries, which carry the greatest burden of SCD. All the included studies recruited their study participants from SCD clinics or referral hospitals. Thus, these findings may not be generalizable to the whole SCD population. Nevertheless, the study still provides a comprehensive evaluation of risk factors associated with BP in an SCD clinic or hospital setting.
The study provides a comprehensive evaluation of risk factors associated with BP in an SCD clinic or hospital setting. Despite study limitations, our study updates current research on a range of factors that may contribute to the risk of RSH and systematic hypertension in SCD patients. Consequently, personalized early interventions aimed at lowering elevated BP may improve life expectancy among SCD patients by inhibiting progression to pulmonary arterial hypertension, advanced renal disease, and other vascular complications. However, high-quality evidence from clinical trials is needed to guide initiation of therapy and treatment goals in SCD patients. Similarly, public health interventions, such as population-based health education and lifestyle modification, within the cultural context, may play a role in preventing elevated BP in SCD patients. However, clinical trials and longitudinal studies should be conducted to confirm these hypotheses. Our systematic review identified methodological limitations and gaps in knowledge that should be addressed in future studies. Limited genetic studies have been done to identify SNPs associated with BP and cardiovascular complications in SCD patients, particularly in Africa. There is a gap in comparable studies from lower-income countries, which carry the greatest burden of SCD. Most importantly, there is a need for clinical trials that aim to determine whether BP interventions can reduce associated complications in SCD patients as they are in the general population. Lastly, the current proposed values for RSH are defined as Systolic BP 120–139 mm Hg or diastolic BP 70–89 mm Hg, whereas systemic hypertension is defined as Systolic BP ≥ 140 mm Hg or diastolic BP ≥ 90 mm Hg in all SCD patients. However, providing age-specific values for RSH and systemic hypertension would make it easier for readers and allow comparison across studies.
A combination of genetic and large longitudinal cohort studies may be able to identify SCD patients who are at highest risk of cardiovascular complications. Over the next 5 years, we will hopefully have more genetic studies looking at SNPs associated with BP and larger longitudinal cohort studies with scientifically rigorous methods for understanding risk factors associated with BP in SCD patients. The establishment of the Sickle In Africa consortium, which aims to facilitate research in SCD, may provide more prospective observational studies on BP and SCD, particularly in Africa. Additionally, there is a need to establish the optimal BP threshold above which to initiate therapy for patients with SCD and age-specific definition of BP based on BP centiles to facilitate comparison between SCD studies, as inclusion of children aged <18 years could have contributed to dilute some of the statistics reported.
5. Conclusions
Blood pressure is lower in SCD patients compared to the general population; however, SCD patients with RSH or systemic hypertension are at increased risk of morbidity and mortality. In addition, risk factors, such as age, gender, triglycerides, blood transfusion, and hemoglobin level are determinants of BP variation in SCD patients. Interventions that consider these risk factors may potentially lower BP pressure in SCD patients and prevent the development of severe complications.
Disclosure
The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or conflict with the subject matter or materials discussed in this manuscript apart from those disclosed.
Reviewer disclosures
Peer reviewers in this manuscript have no relevant financial or other relationships to disclose.
Acknowledgments
Gill Morgan, Health Science Library, University of Cape Town, who assisted with developing the search strategy.
Additional information
Funding
References
- Ware RE, de Montalembert M, Tshilolo L, et al. Sickle cell disease. Lancet. 2017;390(10091):311–323.
- Rees DC, Williams TN, Gladwin MT. Sickle-cell disease. Lancet. 2010;376(9757):2018–2031.
- Gladwin MT. Cardiovascular complications and risk of death in sickle-cell disease. Lancet. 2016;387(10037):2565–2574.
- Piel F, Patil AP, Howes R. Global epidemiology of sickle haemoglobin in neonates: a contemporary geostatistical model-based map and population estimates. Lancet. 2013;381(9861):142–151.
- Enyuma COA, Anah M, Pousson A, et al. Patterns of paediatric emergency admissions and predictors of prolonged hospital stay at the children emergency room, University of Calabar teaching hospital, Calabar, Nigeria. Afr Health Sci. 2019;19(2):1910–1923.
- Adam MA, Adam NK, Mohamed BA. Prevalence of sickle cell disease and sickle cell trait among children admitted to al fashir teaching hospital North Darfur State, Sudan. BMC Res. 2019;12:659.
- Gladwin MT. Cardiovascular Abnormalities in Sickle Cell Disease. J Am Coll Cardiol 59. 2012;13:1123–1133.
- Vichinsky EP. Pulmonary Hypertension in Sickle Cell Disease. N Engl J Med. 2004;350(9):857–859.
- Sachdev V, Machado F, Shizukuda Y, et al. Diastolic dysfunction is an independent risk factor for death in patients with sickle cell disease. J Am Coll Cardiol. 2007;49(4):472–479.
- Gordeuk VR, Sachdev V, Taylor G, et al. Relative systemic hypertension in patients with sickle cell disease is associated with risk of pulmonary hypertension and renal insufficiency. Am J Hematol. 2008;83(1):15–18.
- Wonkam A, Chimusa E, Mnika K, et al. Genetic modifiers of long-term survival in sickle cell anemia. Clin Transl Med. 2020;10(4):e152.
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009).6(7):e1000097.
- Campbell K, Asnani M, Cumming V, et al. Determinants of blood pressure in adults with sickle cell disease. West Indian Med J. 2007;56(95). DOI:https://doi.org/10.1590/S0043-31442007000300029.
- Grell G, Alleyne G, Serjeant R. Blood pressure in adults with homozygous sickle cell disease. Lancet. 1981;318(8256):1166.
- Desai P, Deal A, Brittain J, et al. Decades after the cooperative study: a re-examination of systemic blood pressure in sickle cell disease. Am J Hematol. 2012;87(10):65–68.
- Kuma AB-A, Owusu-Ansah AT, and Sey F, et al. Prevalence of relative systemic hypertension in adults with sickle cell disease in Ghana. PLoS One. 2018;13(1):e0190347.
- Makubi A, Mmbando B, Novelli E, et al. Rates and risk factors of hypertension in adolescents and adults with sickle cell anaemia in Tanzania: 10 years’ experience. Br J Haematol. 2017;177(6):930–937.
- Johnson S, Giorgio J. Arterial blood pressure in adults with sickle cell disease. Arch Intern Med. 1981;141(7):891–893.
- Oguanobi I, Onwubere C, Ibegbulam G, et al. Arterial blood pressure in adult Nigerians with sickle cell anemia. J Cardiol. 2010;56(3):326–331.
- Lamarre Y, Lalanne-Mistrich M, Romana M, et al. Male gender, increased blood viscosity, body mass index and triglyceride levels are independently associated with systemic relative hypertension in sickle cell anemia. PLoS One. (2013).8(6):e66004.
- Homi J, Homi-levee L. Adolescent blood. ArchIntern Med. 2017;153:3–6.
- Pikilidou M, Yavropoulo M, Antonio M, et al. Arterial stiffness and peripheral and central blood pressure in patients with sickle cell disease. J Clin Hypertens. 2015;17(9):726–731.
- Pegelow H, Colangelo L, Steinberg M, et al. Natural history of blood pressure in sickle cell disease: risks for stroke and death associated with relative hypertension in sickle cell anemia. Am J Med. 1997;102(2):171–177.
- Lemonne N, Romana M, Lamarre Y, et al. Association between relative systemic hypertension and otologic disorders in patients with sickle cell-hemoglobin C disorder. Am J Hematol. 2014;89(6):7–667.
- Novelli E, Hildesheim M, Rosano C, et al. Elevated pulse pressure is associated with hemolysis, proteinuria and chronic kidney disease in sickle cell disease. PLoS One. (2014).9(12):e114309.
- Bhatnagar P, Barro-Casella E, Bean J, et al. Genome-wide meta-analysis of systolic blood pressure in children with sickle cell disease. PLoS One. 2013;8(9):e74193.
- DeBaun R, Sarnaik A, Rodeghier J, et al. Associated risk factors for silent cerebral infarcts in sickle cell anemia: low baseline hemoglobin, sex, and relative high systolic blood pressure. Blood. 2012;119(16):3684–3690.
- Strumph K, Benitez S, Hafeman M, et al. Noctrunal hypertension associated with stroke and silent cerebral infarcts in children with sickle cell disease. Pediatr Blood Cancer. 2021;68(5):1–7.
- Benetos A, Safar M, Rudnichi A, et al. Pulse pressure: a predictor of long-term cardiovascular mortality in a French male population. Hypertension. 1997;30(6):1410–1415.
- Gladwin MT. Cardiovascular complications in patients with sickle cell disease. Hematology. 2017;2017(1):423–430.
- Akingbola T, Tayo B, Salako B, et al. Comparison of patients from Nigeria and the USA highlights modifiable risk factors for sickle cell anemia complications. Hemoglobin. 2014;38(4):236–243.
- Bosu K, Aheto K, Zucchelli E, et al. Determinants of systemic hypertension in older adults in Africa: a systematic review. BMC Cardiovasc Disord. 2019;19(1). DOI:https://doi.org/10.1186/s12872-019-1147-7.
- Gladwin MT, Schechter AN, Ognibene FP. Sickle Cell Disease. Circulation. 2003;107(2):271–278.
- Ceglie G, DiMauro M, Tarisi De Jacobis I, et al. Gender-related differences in sickle cell disease in a pediatric cohort: a single-center retrospective study. Front Mol Biosci. 2019;6:1–5.
- Olatunji L, Olabode O, Akinlade O, et al. Neck circumference is independently associated with relative systemic hypertension in young adults with sickle cell anaemia. Clin Hypertens. 2018;24(3). DOI:https://doi.org/10.1186/s40885-018-0088-2.
- Johnson J, CS. Arterial blood pressure and hyperviscosity in sickle cell disease. Hematol Oncol Clin North Am. 2005;19(5):827–837.
- Lamarre Y, Romana M, Lemonne N, et al. Alpha thalassemia protects sickle cell anemia patients from macro-albuminuria through its effects on red blood cell rheological properties. Clin Hemorheol Microcirc. 2014;57(1):63–72.
- Geard A, Pule G, Chelo D, et al. Genetics of sickle cell-associated cardiovascular disease: an expert review with lessons learned in Africa. Omi J Integr Biol. 2016;20(10):581–592.
Appendix 1
The PubMed database search strategy
Search ((((((((((((((‘risk factors’[MeSH Terms] OR risk factors[Text Word])) OR ((determinant OR determinants OR exposure OR exposures)))) OR (‘genome-wide association study’[MeSH Terms] OR genome wide association studies[Text Word])) OR ((‘Genetic Loci’[Mesh]) OR ‘Genetic Association Studies’[Mesh] OR genetic loci[Text Word] OR Genetic Association Studies[Text Word])) OR (‘epidemiology’[Subheading] OR ‘epidemiology’[MeSH Terms] OR epidemiology[Text Word])) OR (‘epigenomics’[MeSH Terms] OR Epigenetics[Text Word])) OR (‘dna copy number variations’[MeSH Terms] OR copy number variation[Text Word])) OR (‘polymorphism, genetic’[MeSH Terms] OR polymorphism[Text Word]))) OR (‘polymorphism, single nucleotide’[MeSH Terms] OR snps[Text Word]))) AND ((((‘blood pressure’[MeSH Terms] OR ‘blood pressure determination’[MeSH Terms] OR ‘arterial pressure’[MeSH Terms] OR blood pressure[Text Word])) OR ((pulse pressure OR diastolic OR systolic))) OR ((variation OR variations OR irregularity OR irregularities OR variability OR variabilities OR difference OR differences)))) AND (((‘anemia, sickle cell’[MeSH Terms] OR sickle cell disease[Text Word])) OR ((hemoglobin s disease OR hemoglobin s diseases OR hbs disease OR hbs diseases)))