ABSTRACT
Purpose: Many youth and adults with Cerebral Palsy (CP) experience high levels of fatigue. This study aimed to compare three fatigue self-report questionnaires to guide clinicians. Method: Thirty youth and adults (age range 17–64) with CP were assessed with Danish versions of the Fatigue Impact and Severity Self-Assessment questionnaire, the Modified Mental Fatigue Scale, and the Multidimensional Fatigue Inventory. Psychometric properties were investigated. Rank order and classification models were compared across questionnaires. Results: The Reduced Motivation and Physical Fatigue subscales of the Multidimensional Fatigue Inventory showed inadequate internal consistency. Participants were frequently ranked differently with the questionnaires. There were issues related to the conceptualization of physical fatigue. Conclusion: The choice of assessment tool should be based on assessment purpose as the questionnaires assess different aspects of fatigue severity, impact, and management. Also, test selection can have important implications on the conclusions that are made about fatigue type and severity.
Introduction
Cerebral palsy (CP) is medically defined as “a group of permanent disorders of the development of movement and posture, causing activity limitation, which is attributed to non-progressive disturbances that occurred in the developing foetal or infant brain.”Citation1 In addition to motor impairments, CP can give cognitive difficulties, disturbances in sensation and perception, as well as communicative and behavioral problems.Citation1 While CP research traditionally has focused primarily on children with CP, there has been an increase in research focusing on adults with CP over the past decade. One of the themes that has received a lot of attention is fatigue. While there is no consensus on the definition of fatigue, it can be defined as “The awareness of a decreased capacity for physical and/or mental activity due to an imbalance in the availability, utilization, and/or restoration of resources needed to perform activity.”Citation2
Fatigue is a common complaint amongst youth and adults with CP, as it is in many other neurological patient populations.Citation3–5 It is estimated that between 30 and 60% of adults with CP experience high levels of fatigue.Citation6–9 As there is no consensus on the definition of fatigue or how to assess fatigue, estimations of prevalence must be interpreted cautiously. Youth and adults with CP report higher levels of fatigue than neurotypical individuals, suggesting that fatigue is more prominent in this population group.Citation6–12 Fatigue was also the third most commonly identified CP-related health problem by rehabilitation physicians.Citation13 Various studies have reported that the level of fatigue experienced in CP is associated with the severity of motor impairment. Indeed, at a group level, there seems to be an association between Gross Motor Function Classification System (GMFCS) level and reported fatigue severity.Citation6–9,Citation14–16 Results from some studies suggest, however, that the association may not be linear.Citation17,Citation18 Fatigue is commonly considered a multidimensional construct including physical and mental/cognitive components. Most studies investigating fatigue in CP have used tools that focus primarily on physical aspects of fatigue and have consistently reported high levels of fatigue. Only few studies have focused on mental components of fatigue in CP and results are inconsistent with one study reporting higher levels of mental fatigue in CP and another study not.Citation6,Citation9
Many individuals report having to limit daily activities due to fatigue and report having to take their fatigue into consideration when planning their everyday life.Citation19 In addition, fatigue has been associated with a reduced quality of life and general measures of health in this population.Citation7 As fatigue can have important consequences on everyday life, it should be addressed by health care professionals. This can however be challenging, as fatigue is a complex and multi-facetted phenomenon. Self-report assessment tools can help guide clinicians in identifying fatigue and in describing its expression when working with adults with CP.
There are many self-report assessment tools available for fatigue as it is a common complaint across many patient populations, including neurological patients. However, these tools usually ask participants to compare their current experience of fatigue to their experience of fatigue prior to their illness onset, questions that are not well suited for individuals with CP, who have had their diagnosis since the very early years of their life. Although many self-report assessment tools have been used in the adult CP population, there are only two tools that have been designed or modified specifically to be used in adults with CP and validated in this population: The Fatigue Impact and Severity Self-Assessment (FISSA) and the Modified Mental Fatigue Scale (m-MFS).Citation14,Citation20 As far as we know, no study has yet compared these measures of fatigue.
The overall aim of the current study was to compare fatigue self-report assessment tools in a CP population. Thirty adults with CP were assessed using the FISSA and m-MFS. Additionally, the Multidimensional Fatigue Inventory (MFI-20), a tool that is widely used for assessing fatigue in various neurological patient groups in Denmark, was administered.Citation21 Importantly, the MFI-20 does not require respondents to compare their experience to a pre-injury baseline. The specific objectives of the study were to: i) make fatigue self-report assessment tools, that are designed for an adult CP population, available in Danish, ii) investigate the internal consistency, item statistics, and scale score distribution (including floor and ceiling effects) for the FISSA, the m-MFS, and the MFI-20; iii) compare responses across the three scales, including their respective classification models for identifying positive and negative cases of fatigue; and iv) explore associations between fatigue severity and background variables. By accomplishing these objectives, the study aims to enhance the understanding and assessment of fatigue in individuals with CP, providing valuable guidance to clinicians when planning interventions and support strategies related to fatigue.
Materials and Methods
Study Sample and Procedure
Thirty adults with CP were recruited for the study between July and September 2021. Participants were recruited via the Elsass Foundation, a private foundation in Denmark working to improve the quality of life of people with CP and their families. A recruitment ad was posted on the Elsass Foundation’s website, LinkedIn profile and Facebook page and shared by users of these platforms. Some individuals who were known to the foundation and who previously had expressed an interest in participating in research were contacted directly and informed about the project. Individuals who were interested in participating registered online after which they were contacted by telephone to check for eligibility. To be included, participants had to be formally diagnosed with CP, be ≥15 years old, have Danish as their mother tongue, and had to be able to fill in a questionnaire with a certain degree of independence (participants were allowed to receive verbal or physical support from the test administrator or from a helper to understand and answer the questions). Individuals with significant communicative challenges (levels IV and V based on the Communication Function Classification System, CFCS) or pronounced cognitive challenges (based on clinical impression) affecting their ability to understand and answer the questionnaires relevantly were excluded from the study.Citation22
Data collection was performed in-person at various locations across Denmark. Background information was collected from the participants through interview. The three questionnaires were then administered using paper-and-pencil. Participants were asked to fill out the questionnaires themselves but could get help from the test administrator in reading the questions and writing answers. The order in which the three questionnaires were filled out was counterbalanced. To provide a supportive environment, participants were encouraged to share their thoughts throughout the process. After having filled out the questionnaires, the participants were asked if they had any questions or comments related to the questionnaires themselves, to their experience of fatigue or to fatigue in general. This represented a form of debriefing for the participants. As research suggests that it can be overwhelming to reflect upon the influence that fatigue has on one’s life, participants were also given the opportunity to have a follow-up consultation with a qualified therapist from the Elsass Foundation.Citation14 Participants did not receive remuneration for participating in the study, but transportation expenses were covered.
Ethics
Both oral and written information was provided to the participants and informed consent was acquired in accordance with the Declaration of Helsinki.Citation23 The study was approved by The Institutional Ethical Review Board, Department of Psychology, University of Copenhagen, Denmark (IP-IRB/11052020).
Fatigue Questionnaires
Fatigue Impact and Severity Self-Assessment
The FISSA is a self-assessment tool that was specifically developed as a clinical tool.Citation14 As an introduction to completing the questionnaire, participants are asked to think of fatigue “in terms of physical tiredness, muscle soreness, exhaustion of muscles and body or any related feeling.”Citation14 Therefore, the tool focuses primarily on the more physical aspects of subjective fatigue. The tool includes 37 items. The first 31 items are used to create a total fatigue score ranging from 31 (low fatigue) to 157 (high fatigue). The last six items are qualitative questions investigating daily fatigue and management and are not included in the FISSA score. Most items are scored on a 5-point Likert scale ranging from Completely Disagree (1) to Completely Agree (5) and a higher score is related to greater fatigue. One item is scored from 1 to 7 and is related to the number of days a week fatigue is experienced. In addition to providing an overall fatigue score, the tool includes two subscales: an Impact Subscale that is related to impact and severity of fatigue (items 1–17; score range 17 to 87), as well as a Management and Activity Modification Subscale that is related to the management of fatigue (items 18–31, score range 14 to 70).Citation14 The FISSA has been validated in a group of 130 youth and adults with CP between 14 and 31 years of age and was shown to have adequate test – retest reliability.Citation14 At the time of the study, no cutoff had been provided to distinguish individuals with pathological levels of fatigue on the FISSA.
Modified Mental Fatigue Scale
The Mental Fatigue Scale (MFS) is a self-assessment tool designed to assess mental fatigue in people with acquired neurological diseases or injuries.Citation24,Citation25 The original MFS requires participants to compare before and after injury. The m-MFS is a modified version of the MFS designed to be appropriate for adults with CP. Instead of referring to perceived differences in fatigue before and after acquired brain injury, the items of the m-MFS relate to the experience of fatigue over the past four weeks.Citation20 The developers of the m-MFS define pathological mental fatigue as “mental exhaustion appearing during cognitive activity or sensory stimulation and having a disproportionately long recovery period.”Citation20 The m-MFS consists of 14 items which all contain one question and a choice between four descriptive rating possibilities (0 = no problem, 1 = slight problems, 2 = fairly serious problems and 3 = serious problems) including half-points between each option, giving the respondents seven response options for each question. Concrete examples are provided for each question.Citation20 The questionnaire yields a single total mental fatigue score ranging from 0 (low mental fatigue) to 42 (high mental fatigue). Construct validity of the m-MFS has been investigated in a group of 10 adults aged 20–56 years old at GMFCS levels I and II.Citation20 It was concluded that the participants perceived the tool as easy to read and understand, the structure of the tool was considered straightforward, the rating options were considered to help with identification of life situations, and there was very good agreement between the respondents’ interpretation and the designers’ intended meaning for the items.Citation20 The developers apply a cutoff of 10 in the validation study, which is the same cutoff suggested for the original MFS, where a score above 10 is considered to indicate fatigue related problems.Citation20,Citation24
Multidimensional Fatigue Inventory
The MFI-20 is a generic self-assessment tool designed to assess fatigue in healthy respondents and a broad range of patient groups.Citation21,Citation26 The tool has been used internationally to investigate fatigue in various neurological patient populations, including individuals with CP.Citation6,Citation27,Citation28 The developers of the tool considered fatigue to be a multi-dimensional concept and therefore designed the questionnaire to cover five dimensions: General Fatigue, Physical Fatigue, Reduced Activity, Reduced Motivation, and Mental Fatigue. The MFI-20 includes 20 items. Each item is a statement related to fatigue that is rated on a five-point Likert scale ranging from 1 (yes, that is true) to 5 (no, that is not true). Negatively worded items are reverse-scored, and items are summed in subscale scores that range from 4 (no fatigue) to 20 (maximum fatigue) with each subscale including four questions. The MFI-20 has been validated in various neurological populations (including Parkinson’s disease, multiple sclerosis and acquired brain injury). While the tool has been used to assess fatigue in CP, it has not been formally validated in this population.Citation6 A score of ≥ 12 on the General Fatigue subscale is usually considered as an indication of elevated fatigue.Citation29,Citation30 The MFI-20 has been available in Danish for many years and has been used to assess fatigue in patients with acquired brain injury in a Danish context.Citation29–32
Translation of the FISSA and M-MFS
The FISSA and m-MFS were not available in Danish prior to this study. The tools were therefore formally translated into Danish for the purpose of this study. The tools were translated following general translation guidelines provided by the World Health Organization.Citation33 Each tool was first translated from their original language (FISSA: English; m-MFS: Swedish) into Danish by two independent health care professionals with special expertise within the field of brain injury and fatigue and who were bilingual with Danish as their mother tongue. The forward translations were compared, and discrepancies were discussed and resolved between the two translators at meetings led by the project manager. This step resulted in a forward version of the test. Subsequently, a back-translation from Danish into each tool’s original language was made by a bilingual Danish-speaking health care professional with English as a mother tongue for the FISSA and a health care professional with Swedish as mother tongue for the m-MFS. The back-translations were compared to the original versions of the tool and discrepancies were discussed and resolved between the back-translators and the project manager. The original developers of the tools were given a report about the translation process and resolved discrepancies and asked to comment on the translations. The Danish versions of the tool were then piloted in five adults with CP to identify unclear formulations. Based on this, minor adjustments were made. After proofreading, final versions were sent for approval amongst the developers of the tools. The Danish versions of the FISSA and m-MFS used in the project are openly available (https://osf.io/qy7rj/files/osfstorage/662416599a61040db1bfa5e7 and https://osf.io/qy7rj/files/osfstorage/66241d3fea2b6313c2533061).
Statistical Analysis
Descriptive item statistics were performed, including means, SD, inter-item correlations, and item-total correlations (corrected for item overlap).Citation34 Item-total correlations below .30 were interpreted as inadequate. For each subscale, floor and ceiling effects were considered to be present if more than 15% of respondents achieved the lowest or highest score possible, respectively, and internal consistency was considered to be inadequate if Cronbach’s alpha was outside the range of .70 to .95.Citation35
The three fatigue questionnaires were compared with respect to rank order, and classification models were compared for the two tools that provide cutoffs (the MFI-20 and m-MFS). Frequencies of fatigue cases across MFI-20 and m-MFS were compared using Pearson’s χ2 test, and test agreement on classification of fatigue was evaluated using Cohen’s kappa. Characteristics were compared among congruent vs. incongruent classifications.
Construct validity concerning physical vs. mental fatigue was evaluated by testing the following hypotheses:
FISSA Impact Scale correlates more strongly with MFI-20 Physical Fatigue than MFI-20 Mental Fatigue
m-MFS correlates more strongly with MFI-20 Mental Fatigue than MFI-20 Physical Fatigue
Finally, associations of fatigue on the three questionnaires and demographic and clinical variables were investigated using correlational analyses and non-parametric tests. All correlations were computed using Spearman’s rank-order correlation coefficient (ρ). Correlation coefficients were interpreted using Cohen’s guidelines, i.e., .10 are “small,” .30 are “medium,” and .50 are “large” in terms of effect sizes.Citation36
Analyses were conducted in R version 4.2.0 using psych for descriptive statistics, ggplot2 (v. 3.4.0) for graphics, and vcd for kappa statistics.Citation37–40 There were no missing data.
Results
Demographics
Thirty adults were included in the project. The sample included individuals with a GMFCS level I to IV and with a CFCS level I to III (see for characteristics). Mean age was 40.5 years (SD = 13.43), ranging from 17 to 64 (median = 38, IQR = 21.75).
Statistics on Fatigue Measurement Tools
Scale score statistics on the three assessment tools and their subscales are available in . Scale score distributions (Figure S1), item descriptive statistics (Table S1–S3), and inter-item correlations (Tables S4–S11) are provided in online supplementary material. Two subscales on MFI-20 exhibited inadequate internal consistency, namely Reduced Motivation (α = .20) and Physical Fatigue (α = .62). For Reduced Motivation, three out of six item pairs were negatively correlated (Table S11). All items on Physical Fatigue were positively inter-correlated (Table S9), but Item 2 “Physically, I feel only able to do a little” was weakly correlated with the subscale score, ρ = .25 (see Table S3). Three subscales on MFI-20 exhibited floor effects, namely Reduced Activity, Reduced Motivation, and Mental Fatigue (see ). Item statistics on the FISSA were adequate, except for weak item-total correlations of Items 25 and 27 (Table S1). Regarding m-MFS, Items 13 and 14 were relatively weaker associated with the total score than the other items, and Item 13 “Do you sleep badly at night? If you are taking sleeping tablets and sleep normally, please place a circle around the ‘0’” exhibited an inadequate item-total correlation, ρ = .21 (see Table S2).
Table 1. Statistics on composite scores.
Classification of Fatigue
Cases of fatigue were classified using cutoff points on MFI-20 General Fatigue (≥12) and m-MFS (≥10). According to MFI-20 General Fatigue, 19 out of 30 (63.33%) met the criterion for fatigue. On m-MFS, 16 out of 30 (53.33%) were classified with fatigue. The frequencies of fatigue cases were not significantly different across the two instruments, χ2(1) = 0.27, p = .60, and there was a fair agreement beyond chance in case classification, Cohen’s κ = 0.39, 95% CI [0.06, 0.71], p = .02 (see ). Although statistically significant, this rate of agreement is not great, corresponding to 15% of data being reliable. Disagreement was associated with GMFCS, χ2(3) = 8.12, p = .04. Individuals with GMFCS level III were more likely to be classified differently on the two instruments (std. Z = 2.73). There was no effect of age, gender, or CFCS.
Table 2. Diagnostic agreement in fatigue classification between the General Fatigue subscale of the Multidimensional Fatigue Inventory and the Modified Mental Fatigue Scale.
Associations Among Fatigue Scales
All fatigue scales and subscales, except for Reduced Motivation (MFI-20), were positively inter-correlated (please see ). The three main fatigue scales, FISSA Impact Scale, m-MFS, and General Fatigue (MFI-20), exhibited large inter-correlations. Despite being strongly correlated, individual participants were ranked differently across the three scales to a large extent ().
Figure 2. Individual rank comparisons across scales. Higher rank corresponds to higher score. FISSA Impact = Impact Scale of the Fatigue Impact and Severity Self-Assessment; m-MFS = Modified Mental Fatigue Scale; MFI-20 = Multidimensional Fatigue Inventory. Participants are color graded according to their FISSA rank as a reference.
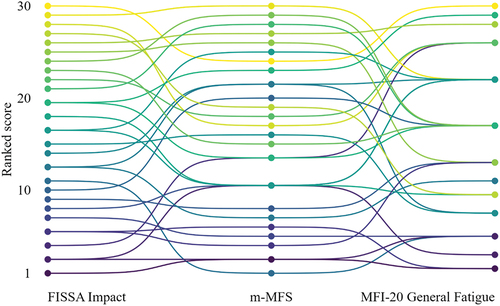
Table 3. Correlations among fatigue scales.
Regarding the distinction between physical and mental fatigue, we tested the two hypotheses concerning FISSA Impact Scale being a measure of physical fatigue (H1) and m-MFS being a measure of mental fatigue (H2). The correlation between MFI-20 subscales Mental Fatigue and Physical Fatigue was negligible (ρ = .05), although both were strongly associated with General Fatigue (MFI-20). H1 was not supported by the data, as the FISSA Impact Scale did not correlate more strongly with Physical Fatigue (ρ = .33) than Mental Fatigue (ρ = .50). H2 was supported, as m-MFS exhibited a large correlation with Mental Fatigue (ρ = .59), and a medium correlation with Physical Fatigue (ρ = .26).
Association Between Fatigue and Background Variables
Fatigue severity did not differ significantly between men and women (FISSA, W = 85, p = .30; m-MFS, W = 106, p = .87; MFI-20 GF, W = 109.5, p = .98), and there was only negligible or weak correlations with age (FISSA, ρ = .08, p = .67; m-MFS, ρ = −.18, p = .34; MFI-20 GF, ρ = .20, p = .29). By visual inspection, GMFCS level I and IV seemed to be associated with less severe fatigue, but there was no statistically significant difference among GMFCS levels (FISSA, χ2(3) = 6.18, p = .10; m-MFS, χ2(3) = 2.54, p = .47; MFI-20 GF, χ2(3) = 4.37, p = .22). illustrates the relation between fatigue and background variables.
Figure 3. Associations between fatigue vs. gender, age, and motor function. FISSA Impact = Impact Scale of the Fatigue Impact and Severity Self-Assessment; m-MFS = Modified Mental Fatigue Scale; MFI-20 GF = General Fatigue subscale of the Multidimensional Fatigue Inventory; GMFCS = General Motor Function Classification System. Highest and lowest possible scale score in brackets. Boxes extend to the first and third quartile, and the center line corresponds to the median. Whiskers extend to the largest and smallest value within 1.5 times the interquartile range. Dots represent individual values. Solid lines represent locally estimated scatterplot smoothing.
Discussion
The primary objective of this study was to compare three fatigue self-report assessment tools in adults with CP, in order to guide clinicians in their future practice. Thirty adults with CP were assessed using the MFI-20, the FISSA and the m-MFS. Before discussing the results of the study, it is worth describing some core differences between the tools. The first major difference is the populations that the tools were designed for. While FISSA and m-MFS both are designed to assess fatigue in individuals with CP, the MFI-20 is a generic tool to assess fatigue in a wide range of neurologic and non-neurologic patient populations, as well as non-patient populations.Citation21 The FISSA is the only tool that was designed from scratch specifically to assess fatigue in adults with CP. The tool was developed through a rigorous process including a high degree of user involvement.Citation14 The m-MFS is simply a modified version of a tool that was developed for patients with acquired brain injury.Citation24,Citation25 Another major difference between the tools is the dimensions of fatigue that are assessed. Indeed, while the MFI-20 covers five domains of fatigue (General Fatigue, Physical Fatigue, Reduced Activity, Reduced Motivation, and Mental Fatigue), the m-MFS, as its name suggests, is designed specifically to assess mental (not physical) aspects of fatigue, and the FISSA instructs respondents to consider fatigue in physical terms. Additionally, while all tools assess aspects related to the severity of fatigue and its consequences, the FISSA is the only tool that also evaluates coping and management of fatigue. Interestingly, the tools focus very little on how contextual factors influence the experience of fatigue, despite many individuals with CP stressing that their fatigue is strongly influenced by for example their physical environment and the type of support that they receive.
A comparison of scores across tools revealed that the three principal scales, FISSA Impact Scale, m-MFS, and MFI-20 General Fatigue, demonstrated significant positive inter-correlations, implying that they all assess a similar overreaching construct, namely fatigue. However, it is noteworthy that participants were frequently ranked differently across the three scales, suggesting that each scale captures distinct aspects of fatigue. In line with this finding, there was a relatively low level of agreement in classification between the two tools for which pathological cutoff values are used, namely the MFI-20 General Fatigue scale and the m-MFS total score. These findings hold significant clinical implications, as there is a considerable likelihood of a participant being identified as having pathological fatigue levels when using one scale but not the other. Notably, individuals with motor impairments corresponding to GMFCS level III were more likely to be classified differently on the two instruments. The differences in classification and ranking of participants across tools likely reflect that the tools are designed to assess different aspects of fatigue, as discussed above.
As the three fatigue assessment tools were designed to assess different aspects of fatigue, the present study also examined the construct validity pertaining to physical and mental fatigue. Notably, as predicted, the scores obtained from the m-MFS, which specifically targets mental fatigue, demonstrated a stronger correlation with the Mental Fatigue subscale than the Physical Fatigue subscale of the MFI-20. Surprisingly, despite the FISSA Impact Scale’s emphasis on defining fatigue in physical terms, it did not correlate more strongly with the Physical Fatigue subscale compared to the Mental Fatigue subscale of the MFI-20. When investigating the scales at an item level, it becomes evident that they do not appear to assess the same construct, despite both scales emphasizing measuring physical aspects of fatigue. The MFI-20 Physical Fatigue subscale includes four items: “Physically I feel only able to do a little,” “Physically I can take on a lot,” “Physically I feel I am in bad condition,” and “Physically I feel I am in excellent condition.” While these items may reflect physical aspects of fatigue in neurotypical populations, they might predominantly reflect motor disabilities rather than fatigue in individuals with CP. In contrast, all items of the FISSA Impact Scale specify that respondents must consider how fatigue affects different aspects of their daily lives. The scale includes items such as “Fatigue interferes with my general everyday activities,” “Fatigue interferes with my ability to move around indoors,” “Fatigue interferes with my ability to do things on my own,” “Fatigue interferes with my participation in social activities,” “I use adaptive equipment to manage my fatigue (examples: a walker, manual wheelchair, power wheelchair etc.),” and “I have had to reduce my responsibilities at home because of fatigue.” It is worth noting that, while participants are instructed in the FISSA to consider fatigue “in terms of physical tiredness, muscle soreness, exhaustion of muscles and body or any related feeling,” the items within the Impact scale do not explicitly refer to physical fatigue.Citation14 In addition, they assess the impact of fatigue on a wide range of aspects of daily living. Some participants in this study mentioned while completing the questionnaire that they found it challenging to think of fatigue only in physical terms, as they also experience fatigue in nonphysical terms. This feedback challenges the assumption that the FISSA scores represent physical aspects of fatigue solely and not fatigue in more general terms, warranting further research on construct validity. Overall, when comparing the items across the tools, there appears to be a lack of agreement regarding how physical aspects of fatigue are conceptualized and operationalized, as reflected in the results.
An additional objective of the study was to explore certain psychometric properties of the three assessment tools in a sample of adults with CP. The Reduced Motivation subscale of the MFI-20 exhibited inadequate internal consistency, consistent with findings from studies examining other neurological populations, which have also reported low or inadequate internal consistency for this subscale.Citation21,Citation29,Citation41–44 In our study, the Reduced Motivation subscale included three pairs of negatively correlated items, rendering the scores on this subscale uninterpretable. These results may suggest that the items relate to different concepts or various aspects of motivation that do not align with one another. Possibly, the intended construct may be too complex to summarize in a single scale, or the items need to be refined to address the intended construct adequately. Furthermore, despite the positive inter-correlations among all items within the Physical Fatigue subscale of the MFI-20, several of them were small or negligible, and it also demonstrated inadequate internal consistency. Notably, item statistics for the FISSA Impact Scale and the m-MFS were generally satisfactory with minor exceptions. Two items specifically related to decreased and increased sleep within the m-MFS were negatively inter-correlated and showed weak associations with the total score. There appear to be some issues with these two items in the construction of the scale, as they do not seem to reflect the same underlying construct. For instance, participants who score high on Item 13 by indicating “I sleep less than 2–3 hours” are unlikely to score high on Item 14 by selecting “I sleep long or deep – At least 12 hours per day and night and in addition I need to take a nap during the day.” A plausible remedy to this issue would be to combine the items into one by using the highest item score of the two. Thus, a higher score represents a more abnormal (either increased or decreased) sleep duration. In this study, this combined item exhibits a stronger item-total correlation (ρ = .39) than Item 13 (ρ = .21) or 14 (ρ = .33) and improves the internal consistency of the scale (α = .87) by .01 point.
The relationship between fatigue and background factors was explored. While certain studies have reported a significant yet mild association between higher age and increased fatigue levels in adults with CP, several studies, including the current one, have not found a significant association.Citation8,Citation9,Citation12,Citation17 In the general population, some studies suggest higher self-reported fatigue levels among women compared to men, while others find no significant differences.Citation45,Citation46 Similarly, gender differences in fatigue levels have not consistently been reported in adults with CP either and no significant association was observed in the current study.Citation6,Citation8,Citation9,Citation11 When it comes to the association between fatigue levels and the severity of motor impairment in CP, results are more consistent. Indeed, many studies have found that higher levels of fatigue are associated with higher GMFCS classification.Citation6–9,Citation14,Citation15 Although this study did not find a statistical difference in fatigue levels across GMFCS levels, a visual examination of the data suggested a possible non-linear association, with GMFCS level I and IV potentially associated with lower levels of fatigue. The presence of a possible non-linear relationship has been reported previously in the literature and therefore warrants further investigation.Citation17,Citation18 Individuals who function at GMFCS level III typically use crutches and/or manual wheelchairs to assist mobility, and it has been suggested that this can lead to higher levels of fatigue than individuals who use physical assistance and/or powered mobility.Citation17,Citation18 It is possible that some individuals who function at GMFCS level III are overexerting themselves in order to live up to broader societal norms in relation to work, education and social engagements.
According to prior research, individuals with CP tend to experience higher levels of fatigue than the neurotypical population,Citation6–9 Consistent with this, a substantial proportion of the participants in this study exhibited scores above the standard cutoff values established for the m-MFS and the MFI-20. However, it is important to exercise caution when comparing levels of fatigue between individuals with CP and norms based on fatigue in neurotypical individuals, as well as when cutoff values are derived from populations of patients with acquired conditions. While individuals with acquired conditions may be assumed to possess a similar pre-morbid baseline as neurotypicals in terms of what can be considered high or low levels of fatigue, individuals who have lived most of their lives with CP cannot be expected to share the same reference point. Furthermore, it is crucial to stress that the sample of this study is not representative of the entire CP population, making it inappropriate to generalize the results to estimate the prevalence of fatigue in all adults with CP.
The study has several important limitations. Firstly, the sample size was relatively small meaning that the findings should be interpreted with caution. Additionally, there was an uneven distribution of participants across GMFCS levels within the sample with a stronger representation of participants with lower GMFCS levels and no participants with GMFCS level V. This disparity cannot solely be attributed to the recruitment strategy but likely also reflects that individuals with more severe motor impairments have fewer resources available to participate in research. Furthermore, due to the recruitment strategy employed, it is possible that individuals who volunteered to participate in the study exhibit a particularly pronounced experience of fatigue. Although this is unlikely to significantly impact the comparisons of scores across tools, the conclusions drawn regarding psychometric properties, and associations of fatigue levels with background variables, it likely has implications for the generalizability of the findings related to fatigue levels to the broader populations of individuals with CP.
Taken together, the study provides useful insights that can be used to guide clinicians when selecting fatigue self-report assessment tools. The FISSA, the m-MFS and the MFI-20 are designed to assess different aspects of fatigue severity, impact, and management. Therefore, depending on the purpose of an assessment, a clinician might want to select one tool rather than another. For example, if a clinician is working on developing new coping strategies in relation to fatigue with a client who primarily experiences fatigue in physical terms, they might want to use the FISSA as it can facilitate discussions between clinicians and people with CP regarding fatigue and management strategies.Citation10 If, however, the aim is to evaluate which dimensions of fatigue are most pronounced in an individual, the MFI-20 might be more appropriate. In addition, based on findings related to internal consistency, clinicians should avoid interpreting scores of the Reduced Motivation subscale and be cautious when interpreting scores on the Physical Fatigue subscale of the MFI-20 in adults with CP. Reduced Motivation, Reduced Activity, and Mental Fatigue also exhibited floor effects and are thus not well equipped to differentiate among individuals with low levels of fatigue.
The study has demonstrated that choices made by clinicians regarding which fatigue self-report assessment tools to use, can have important implications on the conclusions that are likely to be made with regards to the extent to which an individual is considered to be affected by fatigue. Based on the differences in classification across tools and the discussion above regarding the limitations of using normative cutoffs in participants with CP, it can be argued that pathological fatigue in CP should be diagnosed on the basis of formal diagnostic criteria rather than based on the score on single self-report fatigue tools. Self-report tools should not stand alone but be interpreted in the context of a clinical interview that focuses on the specific individual. In addition, self-report questionnaires only provide a retrospective and summative account of perceived fatigue. Recent studies have employed ecological momentary assessment techniques, involving repetitive real-time measurements of self-reported fatigue as people go about their day, to assess how the experience of fatigue fluctuates and interacts with environmental factors in everyday life.Citation47 This approach reduces risks of response bias and provides additional details about fatigue that may be helpful for the clinician working with individuals with CP to identify when and how fatigue worsens during the day and what can be done to improve self-management.
Supplemental Material
Download MS Word (592.2 KB)Acknowledgments
We would like to thank all the participants for their generosity in participating in the study. We would also like to thank Moa Anna Kristina Gustafsson, Susanne Hansen, Ann-Marie Agerbo Low, Katrine Arnkjær, Jenniefer Drude Borup for helping with the translations of the m-MFS and the FISSA-D. Finally, we would like to thank Olivia Dahl for her contributions throughout the project.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data for this paper cannot be made publicly available due to GDPR regulations as the combined background data at an individual level is considered personally attributable.
Supplementary material
Supplemental data for this article can be accessed online at https://doi.org/10.1080/17518423.2024.2347989
Additional information
Funding
References
- Rosenbaum P, Paneth N, Leviton A, Goldstein, M, Bax, M, Damiano, D, Dan, B, Jacobsson, B. A report: the definition and classification of cerebral palsy April 2006. Dev Med Child Neurol Suppl. 2007;109:8–14.
- Aaronson LS, Teel CS, Cassmeyer V, Neuberger GB, Pallikkathayil L, Pierce J, Press AN, Williams PD, Wingate A. Defining and measuring fatigue. Image: J Nurs Scholarsh. 1999;31(1):45–50. doi:10.1111/j.1547-5069.1999.tb00420.x.
- Alghamdi I, Ariti C, Williams A, Wood E, Hewitt J. Prevalence of fatigue after stroke: a systematic review and meta-analysis. Eur Stroke J. 2021 Dec;6(4):319–32. doi:10.1177/23969873211047681.
- Mollayeva T, Kendzerska T, Mollayeva S, Shapiro CM, Colantonio A, Cassidy JD. A systematic review of fatigue in patients with traumatic brain injury: the course, predictors and consequences. Neurosci Biobehav Rev. 2014;47:684–716. doi:10.1016/j.neubiorev.2014.10.024.
- Ramirez AO, Keenan A, Kalau O, Worthington E, Cohen L, Singh S. Prevalence and burden of multiple sclerosis-related fatigue: a systematic literature review. BMC Neurol. 2021 Dec 02;21(1):468. doi:10.1186/s12883-021-02396-1.
- van der Slot WMA, Nieuwenhuijsen C, van den Berg-Emons RJG, Bergen MP, Hilberink SR, Stam HJ, Roebroeck ME. Chronic pain, fatigue, and depressive symptoms in adults with spastic bilateral cerebral palsy. Develop Med Child Neuro. 2012;54(9):836–42. doi:10.1111/j.1469-8749.2012.04371.x.
- Benner JL, Hilberink SR, Veenis T, Stam HJ, van der Slot WM, Roebroeck ME. Long-term deterioration of perceived health and functioning in adults with cerebral palsy. Arch Phys Med Rehab. 2017;98(11):2196–205.e1. doi:10.1016/j.apmr.2017.03.013.
- Russchen HA, Slaman J, Stam HJ, Van Markus-Doornbosch F, VanDen Berg-Emons RJ, Roebroeck ME. Focus on fatigue amongst young adults with spastic cerebral palsy. J Neuro Eng Rehabil. 2014;11(1):1–7. doi:10.1186/1743-0003-11-161.
- Jahnsen R, Villien L, Stanghelle JK, Holm I. Fatigue in adults with cerebral palsy in Norway compared with the general population. Develop Med Child Neuro. 2003;45(5):296–303. doi:10.1017/S0012162203000562.
- Brunton LK, Condliffe EG, Kuntze G, Janzen L, Esau S, Toomey CM, Emery CA. More than just adolescence: differences in fatigue between youth with cerebral palsy and typically developing peers. Ann Rehabil Med. 2021 Jun;45(3):197–203. doi:10.5535/arm.20250.
- Nieuwenhuijsen C, van der Slot WMA, Dallmeijer AJ, Janssens PJ, Stam HJ, Roebroeck ME, van den Berg‐Emons HJG. Physical fitness, everyday physical activity, and fatigue in ambulatory adults with bilateral spastic cerebral palsy. Scand J Med Sci Sports. 2011;21(4):535–42. doi:10.1111/j.1600-0838.2009.01086.x.
- Opheim A, Jahnsen R, Olsson E, Stanghelle JK. Walking function, pain, and fatigue in adults with cerebral palsy: a 7-year follow-up study. Develop Med Child Neuro. 2009;51(5):381–88. doi:10.1111/j.1469-8749.2008.03250.x.
- Hilberink SR, Roebroeck ME, Nieuwstraten W, Jalink L, Verheijden JMA, Stam HJ. Health issues in young adults with cerebral palsy: towards a life-span perspective. Acta Derm Venereol. 2007;39(8):605–11. doi:10.2340/16501977-0103.
- Brunton LK, Bartlett DJ. Construction and validation of the fatigue impact and severity self-assessment for youth and young adults with cerebral palsy. Dev Neurorehabil. 2017;20(5):274–79. doi:10.1080/17518423.2016.1189974.
- van Gorp M, Dallmeijer AJ, van Wely L, de Groot V, Terwee CB, Flens G, Stam HJ, van der Slot W, Roebroeck ME. Pain, fatigue, depressive symptoms and sleep disturbance in young adults with cerebral palsy. Disabil Rehabil. 2021 Jul;43(15):2164–71. doi:10.1080/09638288.2019.1694998.
- Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Develop Med Child Neuro. 1997 Apr 01;39(4):214–23. doi:10.1111/j.1469-8749.1997.tb07414.x.
- McPhee PG, Brunton LK, Timmons BW, Bentley T, Gorter JW. Fatigue and its relationship with physical activity, age, and body composition in adults with cerebral palsy. Develop Med Child Neuro. 2017;59(4):367–73. doi:10.1111/dmcn.13306.
- Oude Lansink ILB, McPhee PG, Brunton LK, Gorter JW. Fatigue in adults with cerebral palsy: a three-year follow-up study. J Rehabil Med. 2018;50(10):886–91. doi:10.2340/16501977-2493.
- Brunton LK, Bartlett DJ. The bodily experience of cerebral palsy: a journey to self-awareness. Disabil Rehabil. 2013;35(23):1981–90. doi:10.3109/09638288.2013.770080.
- Bergqvist L, Öhrvall A-M, Rönnbäck L, Johansson B, Himmelmann K, Peny-Dahlstrand M. Evidence of construct validity for the modified mental fatigue scale when used in persons with cerebral palsy. Dev Neurorehabil. 2019;1–13. doi:10.1080/17518423.2019.1645227.
- Smets EMA, Garssen B, Bonke B, De Haes JCJM. The multidimensional fatigue inventory (MFI) psychometric qualities of an instrument to assess fatigue. J Psychosom Res. 1995;39(3):315–25. doi:10.1016/0022-3999(94)00125-O.
- Hidecker MJC, Paneth N, Rosenbaum PL, Kent RD, Lillie J, Eulenberg JB, Chester K JR, Johnson B, Michalsen L, Evatt M. et al. Developing and validating the communication function classification system for individuals with cerebral palsy. Dev Med Child Neurol. 2011;53(8):704–10. doi: 10.1111/j.1469-8749.2011.03996.x.
- World Medical Association. World medical association declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–94. doi:10.1001/jama.2013.281053.
- Johansson B, Starmark A, Berglund P, Rödholm M, Rönnbäck L. A self-assessment questionnaire for mental fatigue and related symptoms after neurological disorders and injuries. Brain Inj. 2010;24(1):2–12. doi:10.3109/02699050903452961.
- Johansson B, Rönnbäck L. Long-lasting mental fatigue after traumatic brain injury – a major problem most often neglected diagnostic criteria, assessment, relation to emotional and cognitive problems, cellular background, and aspects on treatment. 2014.
- Smets EMA, Garssen B, Cull A, De Haes JCJM. Application of the multidimensional fatigue inventory (MFI-20) in cancer patients receiving radiotherapy. Br J Cancer. 1996;73(2):241–45. doi:10.1038/bjc.1996.42.
- Cantor JB, Ashman T, Gordon W, Ginsberg A, Engmann C, Egan M, Spielman L, Dijkers M, Flanagan S. Fatigue after traumatic brain injury and its impact on participation and quality of life. J Head Trauma Rehabil. 2008;23(1):41–51. doi:10.1097/01.HTR.0000308720.70288.af.
- Mulligan H, Wilkinson A, Barclay A, Whiting H, Heynike C, Snowdon J. Evaluation of a fatigue self-management program for people with multiple sclerosis. Int J MS Care. 2016;18(3):116–21. doi:10.7224/1537-2073.2015-019.
- Norup A, Svendsen SW, Doser K, Ryttersgaard T, Frandsen N, Gade L, Forchhammer H. Prevalence and severity of fatigue in adolescents and young adults with acquired brain injury: a nationwide study. Neuropsychol Rehabil. 2019;29(7):1113–28. doi:10.1080/09602011.2017.1371045.
- Poulsen MB, Damgaard B, Zerahn B, Overgaard K, Rasmussen RS. Modafinil May alleviate poststroke fatigue: a randomized, placebo-controlled, double-blinded trial. Stroke. 2015 Dec;46(12):3470–77. doi:10.1161/STROKEAHA.115.010860.
- Dornonville de la Cour FL, Baerentzen MB, Forchhammer B, Tibaek S, Norup A. Reducing fatigue following acquired brain injury: a feasibility study of high intensity interval training for young adults. Dev Neurorehabil. 2022 Jul;25(5):349–60. doi:10.1080/17518423.2022.2052374.
- Christensen D, Johnsen SP, Watt T, Harder I, Kirkevold M, Andersen G. Dimensions of post-stroke fatigue: a two-year follow-up study. Cerebrovasc Dis. 2008;26(2):134–41. doi:10.1159/000139660.
- World Health Organisation. Process of translation and adaptation of instruments. World Health Organisation. 2020 Feb 27. https://www.who.int/substance_abuse/research_tools/translation/en/
- DeVellis RF. Scale development: theory and applications. 4th ed. Thousand Oaks: Sage; 2017.
- Terwee CB, Bot SDM, de Boer MR, van der Windt DAWM, Knol DL, Dekker J, Bouter LM, de Vet HCW. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007 Jan 01;60(1):34–42. doi:10.1016/j.jclinepi.2006.03.012.
- Cohen JW. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988.
- R Core Team. R: a language and environment for statistical computing. R Foundation for Statistical Computing. https://www.R-project.org/
- Psych: Procedures for Personality and Psychological Research. Version 1.9.12. Northwestern University. 2019. https://CRAN.R-project.org/package=psych.
- Wickham H. ggplot2: elegant graphics for data analysis. New York: Springer-Verlag; 2016.
- _vcd: Visualizing Categorical Data_. R package. Version1.4–11. 2023. https://CRAN.R-project.org/package=vcd
- Elbers RG, van Wegen EEH, Verhoef J, Kwakkel G. Reliability and structural validity of the multidimensional fatigue inventory (MFI) in patients with idiopathic Parkinson’s disease. Parkinsonism Relat Disord. 2012 Jun 01;18(5):532–36. doi:10.1016/j.parkreldis.2012.01.024.
- Fieo RA, Mortensen EL, Lund R, Avlund K. Assessing fatigue in late-midlife: increased scrutiny of the multiple fatigue inventory-20 for community-dwelling subjects. Assessment. 2014 Dec 01;21(6):706–12. doi:10.1177/1073191114541143.
- Wintermann G-B, Rosendahl J, Weidner K, Strauß B, Hinz A, Petrowski K. Fatigue in chronically critically ill patients following intensive care - reliability and validity of the multidimensional fatigue inventory (MFI-20). Health Qual Life Outcomes. 2018 Feb 20;16(1):37. doi:10.1186/s12955-018-0862-6.
- Fredriksson-Larsson U, Brink E, Alsén P, Falk K, Lundgren-Nilsson Å. Psychometric analysis of the multidimensional fatigue inventory in a sample of persons treated for myocardial infarction. J Nurs Meas. 2015;23(1):154–67. doi:10.1891/1061-3749.23.1.154.
- Watt T, Groenvold M, Bjorner JB, Noerholm V, Rasmussen N-A, Bech P. Fatigue in the Danish general population. Influence of sociodemographic factors and disease. J Epidemiol Commun H. 2000;54(11):827. doi:10.1136/jech.54.11.827.
- Lin JMS, Brimmer DJ, Maloney EM, Nyarko E, BeLue R, Reeves WC. Further validation of the multidimensional fatigue inventory in a US adult population sample. Popul Health Metri. 2009;7(1):1–12. doi:10.1186/1478-7954-7-18.
- Verschuren O, Benner JL, Balemans ACJ, Horemans H, Van Den Berg-Emons RJG, Van Der Slot WMA. Real-time daily fatigue, sleep, physical activity, and health-related fitness in adults with cerebral palsy. Develop Med Child Neuro. 2023 Sep 26;65(4):509–16. doi:10.1111/dmcn.15421.