ABSTRACT
Background
Augmentative and alternative communication (AAC) requires on-going support but few studies describing AAC training for healthcare professionals were found.
Method
We developed a short-term education program on amyotrophic lateral sclerosis communication support for undergraduate students in multiple healthcare disciplines. The program comprised lectures plus practice of three AAC methods. Participants were 58 students from four courses at four Japanese universities who completed the program twice, at 6-month intervals. Effects of the program on ‘Beginners’ (taking the program for the first time) and ‘Experienced’ (repeating the course 6 months later) were evaluated using pre-test/post-test scores, number of letters transmitted in 5 min, subjective burden indicated on visual analogue scale (VAS) before and after each AAC trial, and free-text comments.
Results
An increase in scores was shown from the first to the second pre-test. Number of letters generated in 5 min was higher for the Experienced group than for Beginners with the exception of one AAC device. VAS change rate for the Kuchimoji method was lower in the Experienced group than for Beginners. Text-mining of participants’ comments showed lower eyestrain reported in the Experienced group.
Conclusions
This study suggests that participants’ knowledge of AAC for communication support of people with ALS was retained 6 months after completing the short training program, and hands-on AAC experience helped them develop their skills and reduce the perceived subjective burden.
Introduction
Amyotrophic lateral sclerosis (ALS) is a neurodegenerative disease. Upper and lower motor neuron dysfunction causes progressive loss of voluntary muscle activity, including bulbar impairment (dysarthria and dysphagia) [Citation1]. The latest data indicate 9,636 registered patients with ALS in Japan in 2017 [Citation2]. ALS respiratory failure directly affects prognosis; most patients with ALS without ventilation support cannot live beyond 2–5 years from onset. In Japan, the percentage of tracheostomy and invasive ventilation (TIV) is higher (28%–33%) than in other countries (1%–17%) and there are some long-term survivors [Citation3,Citation4].
ALS involves symptoms that impair speaking, writing and physical expression. Communication is fundamental for patients, family, and healthcare professionals. The ability to communicate and understand affects patient participation in decision-making and symptom relief [Citation5,Citation6].
Augmentative and alternative communication (AAC) is any type of support for patients with spoken or written communication disorders, and involves communication strategies (e.g. hand gestures and signs) and/or devices to enhance or replace residual vocalization and communication functions in individuals with language and speech impairment [Citation7]. AAC use varies greatly depending on ALS functional state. AAC support is essential for patients with TIV because they cannot speak [Citation8]. TIV use in ALS is 1%–14% in the USA, 3% in Germany, 2%–5% in France and 11% in northern Italy. TIV is rarely used for ALS in the UK [Citation9]. An analysis of survival time until death/TIV for patients followed by a university hospital in Japan showed that 52 of 160 consecutive patients (33%) underwent TIV in 1990–2010 [Citation10].
In Japan, AAC has been used mainly for patients with ALS. The Rehabilitation Engineering Society of Japan conducted a survey in 2008 and 2009 on national communication support provision [Citation11]. ALS ranked first for dissemination of communication devices by disease (62%), followed by cerebrovascular disorders (10.6%) and cerebral palsy (7.6%). ALS accounted for 90.2% of requests for communication device repairs (i.e. replacing switches), reflecting voluntary motor function decline. Communication support was mostly associated with neurodegenerative disorders, especially ALS.
Makkonen et al. [Citation12] reported that 60% of Finnish patients with ALS retained adequate speech for an average of 18 months from the first bulbar symptoms. They recommended focusing on first bulbar symptom onset when assessing AAC need. Nakayama et al. [Citation8] examined communication status in 76 patients with TIV in Japan (17.2% were totally locked-in). Communication ability stage progression was associated with several factors, including TIV need and development of overt oculomotor limitation. Development of the latter within 24 months post-onset affected progression to Stage V (unable to communicate by any means) [Citation13]. However, some patients maintained communication >10 years after TIV. The authors emphasized that about 80% of patients with ALS using TIV can communicate with AAC devices [Citation8,Citation13].
Imura [Citation14] surveyed the Japanese ALS Association patients and family members who use AAC. The ‘stand-by group’, that did not yet use AAC, had little experience in using information technology (IT) such as personal computers. In addition, little support was available for the ‘aborted group’, which discontinued AAC use. The results suggested the need to provide incentives for the stand-by group to use IT devices, and support for the aborted group to use new AAC. The use of AAC in patients with ALS requires continuous support.
The introduction and continued use of AAC requires ongoing support from multidisciplinary healthcare teams [Citation15]; however, general undergraduate healthcare studies provide few opportunities to acquire AAC expertise in Japan. For example, the medical and nursing education model core curriculum presented by the Ministry of Education, Culture, Sports, Science and Technology in Japan only provides basic communication with patients and team communication, and does not mention support for patients with communication disorders [Citation16,Citation17]. Therefore, most healthcare professionals need to learn about AAC support after graduation, given their need to care for patients with ALS and the difficulties with communication experienced by these patients. Some institutes and patients’ associations in Japan have their own resources to support such learners [Citation18], but there are differences among individual healthcare professionals in terms of level of AAC support [Citation19]. It is therefore essential that undergraduate education in this field is effective even if limited, as it is a fundamental opportunity for students to gain exposure to AAC.
Nagayoshi et al. [Citation20] examined nursing students’ use of communication boards. They reported that time to transmit randomly set hiragana letters or numbers improved more for students with 10 days of training compared to students who practiced only two or three times, but there was no evaluation of long-term knowledge retention. Kavanaugh et al. [Citation21] assessed a 5-hour training program for young caregivers (8–18 years) of patients with ALS. Training comprised <1 h on communication support and did not address communication in patients with TIV. Evaluation involved participant impressions but not robust qualitative methods, such as text-mining.
In the intensive-care field, Radtke et al. [Citation22] reported the experience and perceptions of nurses regarding communication intervention: a basic communication skills training program and introduction of AAC strategies. While the nurses’ opinions about their experiences showed the benefits of training, they pointed out the small proportion of nurses trained or knowledgeable about best patient communication practices in the intensive care unit (ICU). Dithole et al. [Citation23] conducted a workshop with scenarios including communication during intubation, suctioning and tracheostomy care, especially focusing on assessment of a patient’s ability to communicate in order to check which AAC devices would be appropriate. The study indicated that AAC can improve nurse-patient communication in the ICU and the authors suggested the implementation of communication skills training for intensive-care nurses.
In other fields, Banfai et al. [Citation24] assessed a training program on knowledge and skills of automatic external defibrillators and basic life support (BLS) for 7–14-year-old students. Four months post-training, students retained some knowledge and skills. Kovács et al. [Citation25] examined the long-term effects of BLS training for medical students using different training conditions. Students who took a practical exam 3 months post-training showed greater skill retention after 5 months. Parikih et al. [Citation26] evaluated retention of palliative care communication skills training one year later in medical students using simulated patients. Although participants felt that communication skills training was important, there was no quantitative measure of knowledge and skill retention.
Previous research indicated educational effectiveness of training. However, few studies have evaluated the effects and retention of training programs on communication support for patients with ALS. We developed a short-term ALS communication support education program for undergraduate students in multiple healthcare disciplines: medicine, nursing, rehabilitation and education.
The research objective was to examine how AAC knowledge, skills and subjective burden were affected by a half-day education program, and to describe the change that occurred in these aspects over a 6-month period.
Methods
This study was conducted from March 2018 to September 2019. The Mie University Faculty of Medicine Research Ethics Committee approved the study (#3245).
Materials
The program content was adapted from Imura’s Guidebook for AAC, through discussions among the authors [Citation27]. The program comprised three 90-minute units of lectures plus practice of three AAC methods.
At the orientation session, we described the program, checked materials (guidebooks and worksheets) and explained how to complete the worksheets. After a pre-test, the program began ().
Table 1. Program outline.
Session 1 contained three lectures, the first of which was a 20-minute lecture on ALS, followed by a 9-minute video of a person with TIV, a group discussion on the need for communication, and an overview of AAC. Session 2 comprised AAC practice. Session 3 comprised five lectures on the AAC system for maximizing usage period, and subsequent group discussions. The program ended with a post-test and retrospective comments on the worksheets. Participants brought back the guidebooks and worksheets used in the program.
The pre-test/post-tests were the same. All topics were extracted from the guidebook summary. They comprised ten questions with participants selecting two of five choices [Citation28].
The practice exercises used a transparent flick-type communication board (Flick, ICT rescue team, Tokyo), the Kuchimoji communication method, and the Let’s Chat® (Panasonic Inc., Tokyo) communication device. The communication board presented a Japanese syllabary, allowing the patient to communicate with the caregiver using eye contact to select letters. The Kuchimoji method uses a combination of oral shapes and eye-blinking for communication [Citation28]. After a video explanation of how to use each AAC method, a 5-minute practice was performed. In the communication board and Kuchimoji sessions, participants were asked to practice three roles (patients, caregivers and observers), with the order rotated each time so that each participant was able to take on each role once.
Participants were asked to discuss improvements associated with their roles after each practice in the group. They did not have the opportunity for discussions with the other group as the groups were physically distanced. In the Let’s Chat® session, participants first used the set scanning speed (labeled ‘default’) of level 7 (scanning-speed range: 1 (slowest) – 13 (fastest)), then attempted the same text again using their preferred scanning speed (labeled ‘adjusted’). The contents to be transmitted were randomly changed and presented at each practice, so that the same message was not communicated twice.
Participants
Participants were a convenience sample of paid self-selected students recruited from the undergraduate faculties of medicine, nursing, rehabilitation and education (Clinical Psychology stream) at four Japanese universities. Inclusion criteria were 20–60 years old, able to participate in the program both initially and 6 months later, and no similar educational opportunities. All participants provided written informed consent.
Participants completed the same program twice, over a 6-month interval. Those taking the course for the first time were labeled ‘Beginners’ and those repeating the course 6 months later were labeled ‘Experienced’. The cohorts were kept away from each other so that there was no mixing between groups. A waiting-list control design with a 6-month delay interval was used to compare the two groups ().
Figure 1. Study design: a waiting-list control design.
Notes: This figure shows the flow of the study at one university. Here, implementation was conducted with one group of six participants at one university (The full study was conducted at four universities using the same flow). All participants, except for those in the last group, completed the same program twice at 6-month intervals. The effect of the education program was evaluated by comparing the outcomes between the first attendance (Beginners) and second attendance (Experienced).
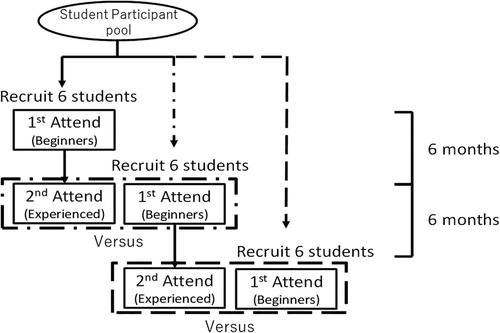
The number of participants was settled at 6 per group in each program of this trial due to the limited capacity of the research members at individual universities.
Analyses
Effects of the program were evaluated using four outcomes: pre-test/post-test scores; number of letters transmitted using each AAC in 5 min; subjective burden of AAC using visual analogue scale (VAS) values before and after each AAC trial; and free-text comments on impressions and awareness. Data were analysed using R version 3.5.0 (R Foundation for Statistical Computing, Vienna, Austria). Statistical significance was set at P < 0.05.
Participants were asked to mark their level of burden using VAS by marking a straight line with a highlighter pen at the subjective level perceived, where level 0 meant no burden and level 100 meant the highest burden. Just before the task, they were asked to mark the expected level of burden. Soon after the AAC trial, they were requested to do ratings again on another VAS with the same criteria, based on the actual burden experienced.
Free-text comments on the worksheets were processed using KH Coder® (https://khcoder.net/en/) text-mining software. In 2016, Higuchi proposed a two-step approach for quantitative content analysis of text data using KH Coder® [Citation29]. This two-step approach was used for analysis of the content of the free-text comments. First, KH Coder® extracted words from the comments and then ‘characteristic’ words used by Beginners and Experienced participants were compared. Coding rules were created for extracting words related to burden and ease of use, and finally KH Coder® compared the frequency with which these concepts occurred in Beginner and Experienced participant comments.
In KH Coder® analysis, ‘Token’ indicates the total number of words in the text. ‘In use’ indicates the number of words KH Coder® recognizes as analysis targets. KH Coder® created a co-occurrence network based on the frequency and pattern of the extracted words. Strongly related words were connected by lines. Degree of co-occurrence between words was indicated by the Jaccard coefficient.
Results
Of 58 students (16 males and 42 females) who participated in the program, 11 took the course only once owing to study period limitations, resulting in 105 total trials. All the participants were older than 19 years (mean ± standard deviation: 20.8 ± 1.6). There were 35 nursing students, 9 medical students, 9 rehabilitation students and 5 clinical psychology students.
Pre-test/post-test
shows percentage of correct answers for each question in each test. In questions 2, 7 and 8, the correct answer rate was accurately selected by less than half of the participants, with question 2 the lowest of them all. For most questions (except question 6) the percentage of correct answers increased or remained the same before and after the program. The percentage of correct answers decreased by about 20% for both the Beginner and Experienced group in question 6.
Table 2. Correct answer percentage for each question in the pre-test/post-test.
Test scores for each group were normally distributed as determined using the Shapiro–Wilk test. The Beginners’ pre-test and post-test scores were compared using the paired t-test (). Their mean post-test score was 1.79 points higher (P < 0.001 n = 58) than at pre-test.
Table 3. Mean pre-test/post-test scores for each group.
First attendance post-test scores and second attendance pre-test scores of the same student were compared using the paired t-test (excluding 11 participants who took the course only once). The mean second attendance pre-test score was 0.89 points lower than the first attendance post-test score (P = 0.028, n = 47). Pre-test scores of Beginners and post-test scores of Experienced students were compared using unpaired t-test. The mean Experienced group score was 2.04 points higher (P < 0.001, n = 47) than the mean score of the Beginners.
Pre-test scores of Beginners and Experienced students were compared using the unpaired t-test. The mean Experienced group score was 0.88 points higher (P = 0.031, Beginners: n = 58, Experienced: n = 47) than the mean score of the Beginners.
Number of letters
A scanning-speed adjustment in the Let’s Chat® session was introduced after researcher discussion following the first implementation in each university. No adjustment was made for participants of the first implementation (24 students). Therefore, 34 Beginners and 38 Experienced students used the adjustment.
The number of letters in each group was normally distributed based on results of the Shapiro–Wilk test. We compared the mean number of letters transmitted in 5 min using each AAC by the Beginners and Experienced groups using unpaired t-tests (). The number of letters used by the Experienced participants was higher than by the Beginners, except in the Let’s Chat® default condition. The Experienced students transmitted more letters in 5 min: 8.7 (Flick), 5.6 (Kuchimoji) and 6.8 (Let’s Chat with adjusted speed) letters than the Beginners did ().
Table 4. Number of letters transmitted in a 5-minute period for each AAC system by group.
The change in the number of letters from the default to the adjusted conditions was also compared between the Beginners and the Experienced using the paired t-test. In both groups, the number of letters increased with adjustment.
VAS
As subjective burden showed large individual variation, VAS values were compared using change rates. The change in VAS values before and after using each AAC method was expressed as the after/before score rate (). The data were non-normally distributed (Shapiro–Wilk test). The VAS score rates for Beginners and Experienced groups were compared using Mann–Whitney U tests. The change rate of Kuchimoji for the Experienced participants acting as patients was 0.6 lower than for the Beginners (P = 0.001).
Table 5. VAS change rates by AAC.
Free-text comments
KH Coder® extracted 15,287 Japanese words from the comments. Some words (mainly particles, adverbs and symbols) were excluded if they lacked any semantic content of their own. Words such as ‘think’ and ‘feel’ were also excluded, as these would have been meaningless in the analysis. This left 6,018 tokens in use. There were 1261 types of words in total and 1018 types of words in use. The frequency (mean ± standard deviation) of each word in use was 5.9 ± 18.0.
The co-occurrence network was created from the text by KH Coder® (). Co-occurrences of words related to ‘time burden’ (circle A, e.g. ‘time’ and ‘wait’), words related to ‘technical burden’ (circle B, e.g. ‘transmit’ and ‘difficult’), and words related to ‘eyestrain’ (circle C, e.g. ‘eye’, ‘tired’ and ‘blink’) were extracted as characteristic words and comprehensive burden on ‘speed’ was shown in the circle D.
Figure 2. Co-occurrence network.
Notes: The figure was created with KH Coder® based on the frequency and pattern of words in free-text comments, without consideration of the analysts’ intentions. Words with strong co-occurrence were arranged close together and connected with lines. Circle sizes corresponded to the frequency. The numbers on the lines indicated the Jaccard coefficients. Larger values suggest a stronger degree of co-occurrence. Words reflecting feelings of burden were separated into ‘time burden’ (circle A), ‘technical burden’ (circle B), and ‘eyestrain’ (circle C). The other group (circle D) directly reflected burden relating to ‘speed’.
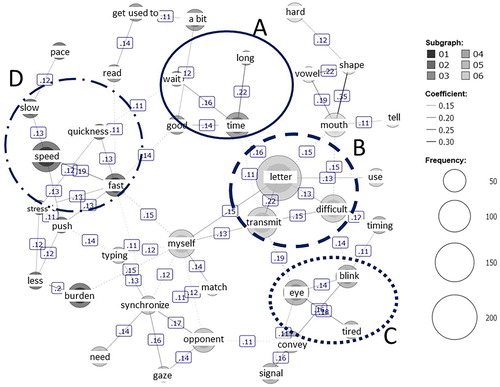
From the characteristic words via KH Coder®, four concepts emerged as ‘eyestrain’, ‘technical burden’, ‘time burden’ and ‘ease’ (). A coding rule was agreed whereby a combination of the particular expressions shown in the table should be regarded as an appearance of the concept of the heading. The number of occurrences of each code was compared between the Beginners and the Experienced (). A between-group difference was observed in the number of occurrences of ‘eyestrain’ (P = 0.036).
Table 6. Coding table of the four extracted concepts.
Table 7. Difference in the number of coded concepts between the groups.
Discussion
Pre-test/post-test scores
The participants had little knowledge related to some questions at the beginning of the program: ‘communication board (No. 2)’, ‘AAC support in accordance with trajectory of the disease (No. 7)’ and ‘the role of healthcare professionals (No. 8)’ at the first pre-test (). These scores increased through the program. In contrast, there was a question that showed no increase in correct answers (No. 6), suggesting that participants did not know when to introduce AAC and the nature of the team required to support it. Emphasis on the importance of AAC and the need to gain knowledge of AAC may have led to the misunderstanding that there is a need for specific healthcare professional support and early introduction regardless of stage. Lack of understanding of lecture content might have led to participants being confused about test items focusing on timing and support of AAC. In addition, they may have misunderstood items in the pre-test/post-test. This suggests a need to focus specifically on the topics of how and when AAC should be introduced. Ambiguous test items must also be revised for future training.
Beginners test scores increased after taking the program once, which may be an effect of single attendance (). The increase in the second pre-test scores compared to the first pre-test scores showed a slight retention of the learning effect. Taylor et al. [Citation30] examined the effects of pre-test/post-test scores on pre-class work and class recitation activities of biochemistry university students.
Students who performed these activities scored better than control participants who did not. However, the learning effect was not maintained after 8 months. In this study, participants’ knowledge was retained 6 months later, even though they had attended only a single program. The learning effect on the test score was statistically significant, although the difference between scores was very limited. It was difficult to evaluate actual effectiveness using only test scores. Therefore, other evidence of learning was considered including number of letters, VAS, and analysis of free comments.
Number of letters
The results suggested that even a single AAC practice was effective in maintaining the skills of participants in using AAC (). The meaningful transmissions at an average of more than 25 letters in 5 min using three types of AAC were shown in this study. The retention of skills supported the necessity of AAC experience in healthcare-education curricula.
There was no difference in the Let’s Chat® default condition, because the unified scanning speed was too slow for healthy persons to detect the difference in the number of transmitted letters. It was already reported that it is important to use AAC with suitable scanning speed for each patient [Citation31].
Morris et al. reported a qualitative study of adult AAC users’ experiences [Citation32]. The interview study with 12 patients revealed that AAC users felt ‘physicians were rushed and gave the impression that they did not have enough time to communicate’. The time barrier could be one of the factors that make healthcare professionals hesitate to communicate with patients: they are too busy for time-consuming communication. The speed at which letters are transmitted is important for communication with patients with communication disorders [Citation32]. Nagayoshi et al. reported that effective communication required communication partners to become accustomed to using AAC [Citation20]. In other words, it is necessary for healthcare professionals to acquire the skills to communicate efficiently with AAC so that they can be sensitive communication partners of people with ALS and know how best to provide practical support to those using AAC.
VAS
Contrary to the authors’ expectation that the AAC experience would reduce the subjective burden on participants, the results showed a decrease only in the Kuchimoji practice (). This may have reflected the small sample size and some sense of competition in the 5-minute practices of all the participants, even Experienced ones.
Andou [Citation33] described a relationship between social skill and burnout in nurses who care for patients in the neurological and neuromuscular ward. This study pointed out that caring for patients who have difficulty communicating was one of the stressors for young nurses. Decreasing the perceived burden of using AAC was thought to promote the communication of healthcare professionals with patients with communication disorders.
Decreases in Let’s Chat® VAS rates after adjustment to preferred scanning speed in both groups suggested that a speed suitable for each user reduced participant burden, as well as improving the number of letters. The perceived burden after adjustment was lower than the other results. This suggested that the participants realized how important to touch a device even once and to adjust it by each situation, even though all of them were young and very good at handling digital equipment and furthermore the communication device, Let’s Chat® has been recognized easy to use without special skills compared to other AAC.
Free-text comments
Our analysis of characteristic words showed that the Experienced participants mentioned ‘eyestrain’ less frequently than the Beginners did, suggesting that participants retained the effect of AAC practice for 6 months and perceived AAC as less challenging, especially on the eyes (). The results were also considered to be related to the improvement in the number of letters in the AAC, when using the eyes, such as the Flick and the Kuchimoji. In contrast, the ‘time burden’ was still noted by the Experienced group. Huggins et al. reported patients with ALS expected to be able to transmit 15–19 letters/minute via AAC [Citation34]. Even the improved number of letters may not be as fast as students in the Experienced group expected. In addition, more AAC experience may be needed to improve ‘technical burden’ and ‘ease’.
Overall, these findings demonstrated the effectiveness of this communication-support program and indicate some retention of knowledge and skills. It was considered effective to have a program focusing on communication support for patients with ALS incorporated into medical and nursing curricula.
Limitations and future directions
This study was conducted with a limited sample size in four universities and four faculties. Participants were only those who voluntarily participated in this program. However, test scores increased slightly and participants were clearly able to acquire AAC skills through the program. It will be necessary to recruit a larger and more varied student sample in future to examine the learning effect.
Undoubtedly, further experience and training would be needed for healthcare professionals to provide a high level of personalized clinical support for AAC users. However, the program described in this paper provides an opportunity for participants to increase their awareness and familiarity with AAC, as a start to further development in this regard. We believe that this approach will contribute to supporting the younger generation, in other words, the next generation of clinical workers, supporting patients with communication disorders related to ALS.
Terry et al. [Citation35] reported that face-to-face instruction combined with online training was effective in the retention of learning effect among undergraduate nursing students. Having demonstrated the effectiveness of the program, the next strategy would be to provide the program in a more readily accessible format to a wider audience. One solution would be to deliver the training by e-learning, needless to say which should be investigated if it could provide the same effect of the face-to-face program. In the era of covid-19, the demand for e-learning is increasing. Whether e-learning is equivalent to face-to-face instruction requires further study. While the five-hour, face-to-face program provided the benefit of direct learning, participants were required to remain in the same location for an extended period of time, potentially leading to impact on attention spans.
Conclusion
We developed a half-day education program on communication support for patients with ALS and implemented it with students in healthcare disciplines at four universities. The study design over a 6-month interval suggested student knowledge was maintained and the AAC experience improved and helped develop students’ AAC skills and reduced some of the perceived burden. Communication support for patients with ALS should be included in the curriculum even if the training is limited to only half a day. The impact of this training may be significant for healthcare workers and the patients with ALS with whom they communicate.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Ethical approval statement
The Mie University Faculty of Medicine Research Ethics Committee approved the study (#3245).
Data availability statement
Ishikawa T, Narita Y, Fukuroku K, Takahashi E, Mizumoto C. Gross numbers of letters as the effect of a short-term training program for augmentative and alternative communication on health-care students after 6 months. Amyotroph Lateral Scler Frontotemporal Degener. 2019;20(sup.1):340.
Additional information
Funding
Notes on contributors
Takemasa Ishikawa
Takemasa Ishikawa is a nurse at Mie University Hospital, Japan. His interests are care for people with intractable neurological diseases, especially communication support.
Yugo Narita
Yugo Narita is a professor in the School of Nursing, Faculty of Medicine, Mie University, Japan. His interests are clinical neurology, geriatric medicine and care for people with intractable neurological diseases, especially to support communication difficulties.
Tamotsu Imura
Tamotsu Imura is a professor in the Faculty of Nursing and Rehabilitation, Chubu Gakuin University, Japan. His interests are rehabilitation engineering focused on communication aids, and multidisciplinary support for people with intractable neurological diseases.
Yuji Tanaka
Yuji Tanaka is a professor in the Health Service Centre, Aichi University of Education, Japan. His interests are clinical neurology, care for people with intractable neurological diseases and education of school health.
Michiko Nakai
Michiko Nakai is a professor in the Faculty of Nursing, Suzuka University of Medical Science, Japan. Her interests are care for people with intractable neurological diseases and fundamental nursing education.
Keiko Fukuroku
Keiko Fukuroku is an associate professor in the School of Nursing, Faculty of Medicine, Mie University, Japan. Her interests are care for people with musculoskeletal disorders and rehabilitation nursing.
References
- Yunusova Y, Plowman E, Green J, Barnett C, Bade P. Clinical measures of bulbar dysfunction in ALS. Front Neurol. 2019;10:106, doi:10.3389/fneur.2019.00106.
- Ministry of Health, Labour and Welfare. Tokutei iryouhi jukyuusyasyou syogaisyasuu taisyousikkannbetsu [Number of recipient certificates issued for specific disease treatment] (end of FY2017). [Article in Japanese]. [cited 2020 Jan 28]. Available from: https://www.mhlw.go.jp/toukei/youran/data30k/222.xls.
- Hirose T, Kimura F, Tani H, Ota S, Tsukahara A, Sano E, et al. Clinical characteristics of long-term survival with noninvasive ventilation and factors affecting the transition to invasive ventilation in amyotrophic lateral sclerosis. Muscle Nerve. 2018;58:770–6.
- Hayashi N, Atsuta N, Yokoi D, Nakamura R, Nakatochi M, Katsuno M, Izumi Y, Kanai K, Hattori N, Taniguchi A, et al. Prognosis of amyotrophic lateral sclerosis patients undergoing tracheostomy invasive ventilation therapy in Japan. J Neurol Neurosurg Psychiatry. Epub ahead of print. [cited 2020 Feb 3]. doi:10.1136/jnnp-2019-322213.2020.
- Fried-Oken M, Mooney A, Peters B. Supporting communication for patients with neurodegenerative disease. NeuroRehabilitation. 2015;37:69–87.
- Stans S, Dalemans R, Roentgen U, Smeets H, Beurskens A. Who said dialogue conversations are easy? The communication between communication vulnerable people and health-care professionals: a qualitative study. Health Expect. 2018;21:848–57.
- Light J. Toward a definition of communicative competence for individuals using augmentative and alternative communication systems. Augment Altern Commun. 1989;5:137–44.
- Nakayama Y, Shimizu T, Mochizuki Y, Hayashi K, Matsuda C, Nagao M, et al. Predictors of impaired communication in amyotrophic lateral sclerosis patients with tracheostomy-invasive ventilation. Amyotroph Lateral Scler Frontotemporal Degener. 2016;17:38–46.
- Magelssen M, Holmoy T, Horn M, Fondenaes O, Dybwik K. Ethical challenges in tracheostomy-assisted ventilation in amyotrophic lateral sclerosis. J Neurol. 2018;265:2730–6.
- Tagami M, Kimura F, Nakajima H, Ishida S, Fujiwara S, Doi Y, et al. Tracheostomy and invasive ventilation in Japanese ALS patients: decision-making and survival analysis: 1990–2010. J Neurol Sci. 2014;344:158–64.
- Imura T. Judosyougaisya ishidentatsusouchi no sikyu to riyoushien wo houkatsu suru komyunikeisyon sougousien no kakuritsu ni kansuru kenkyu [Survey for establishment of comprehensive communication supports with provision and facilitation of communication devices for severely disabled patients]. Comprehensive Research Report for MHLW Grant-in-Aid for Disabled Patients. Gifu (Japan). 2011;1:1–10. [Article in Japanese].
- Makkonen T, Ruottinen H, Puhto R, Helminen M, Palmio J. Speech deterioration in amyotrophic lateral sclerosis (ALS) after manifestation of bulbar symptoms. Int J Lang Commun Disord. 2018;53:385–92.
- Hayashi K, Mochizuki Y, Nakayama Y, Shimizu T, Kawata A, Nagao M, et al. Communication disorder in amyotrophic lateral sclerosis after ventilation – a proposal of staging and a study of predictive factor. Clinical Neurology. 2013;53:98–103. [Article in Japanese, Abstract in English].
- Imura T. Analysis of the situation and support for using communication aids in ALS patients. J Japan Intractable Illness Nursing Soc. 2015;20:125–38. [Article in Japanese, Abstract in English].
- Imura T. Analysis of the needs for introduction support of communication aids for ALS patients – an experiment of systematization of individual needs by text mining. J Chubu Gakuin Univ College. 2017;18:103–12. [Article in Japanese, Abstract in English].
- Ministry in Education, Culture, Sports, Science and Technology. Kango Kyouiku Moderu Koa Karikyuramu [The nursing education model core curriculum]. [Article in Japanese]. [cited 2020 May 11]. https://www.mext.go.jp/component/a_menu/education/detail/__icsFiles/afieldfile/2017/10/31/1217788_3.pdf.
- Ministry in Education, Culture, Sports, Science and Technology. Igaku Kyouiku Moderu Koa Karikyuramu [The education model core curriculum]. [Article in Japanese]. [cited 2020 May 11]. https://www.mext.go.jp/component/b_menu/shingi/toushin/__icsFiles/afieldfile/2017/06/28/1383961_01.pdf.
- JALSA. ALS Toujisya Ni Yoru Dennshikiki Ya IT Kiki Wo Mochinai Komyunikeisyon Shienhouhou Kobetsu Kousyukai. [Seminar about Communication support without electronic devices and IT deviced by ALS patients]. [Article in Japanese] [cited 2020 Jul 5].
- Hidaka T, Mizuki S, Sato T, Matsubara Y. What are the Technology and knowledge for the lives of ALS patients?: focusing on the case exam;le of peer support. Ritsumeikan J Human Sci. 2009;18:33–47.
- Nagayoshi M, Abe Y, Satou C, Ichikawa K, Kitajima M, Fuyubuchi R, et al. Toumei mojiban No shiyou No nare To komyunikeisyon kaisuu niyoru ishidentatu sokudo Ni chigai Ga aruka [Whether there is a difference in the communication speed based on the experience of using the transparent dial and the communication frequency]. Japanese J Nursing Sci. 2017;42:68–73. [Article in Japanese].
- Kavanaugh M, Howard M, Banker-Horner L. Feasibility of a multidisciplinary caregiving training protocol for young caregivers in families with ALS. Soc Work Health Care. 2018;57:1–12.
- Radtke J, Tate J, Happ M. Nuerses’ perceptions of communication training in the ICU. Intensive Crit Care Nurs. 2012;28(1):16–25.
- Dithole KS, Thupayagale-Tshweneagae G, Akpor OA, Moleki MM. Communication skills intervention: promoting effective communication between nurses and mechanically ventilated patients. BMC Nurs. 2017;16(1):doi:10.1186/s12912-017-0268-5
- Banfai B, Pek E, Pandur A, Betlehem J. ‘The year of first aid’: effectiveness of a 3-day first aid program for 7-14-year-old primary school children. Emerg Med J. 2017;34:526–32.
- Kovács E, Jenei Z, Csordás K, Fritúz G, Hauser B, Gyarmathy A, Zima E, Gál J. The timing of testing influences skill retention after basic life support training: a prospective quasi-experimental study. BMC Med Educ. 2019;19. [cited 2020 May 11]. doi:10.1186/s12909-019-1881-7
- Parikh P, White M, Buckingham L, Tchorz K. Evaluation of palliative care training and skills retention by medical students. J Surg Res. 2017;211:172–7.
- Imura T. Shinkei kin shikkan kanja ni taisuru komyunikeisyon kiki dounyuu shien gaidobukku [The guidebook to assist introduction of AAC for patients with neuromuscular disorders]. [Article in Japanese]. [cited 2020 Feb 3]. https://rel.chubu-gu.ac.jp/files/2016-rep/guidebook-all.pdf.
- Narita Y, Nakai M. Imura t Tanaka Y Ishikawa T Fukuroku K. education program for students in multiple health-care fields to support communication with patients with amyotrophic lateral sclerosis - Can a Pre-/post-test evaluate knowledge gained through education sessions? Int J Affect Eng. 2019;18(3):161–70.
- Higuchi K. A two-step approach to quantitative content analysis: KH Coder tutorial using anne of Green gables (part I). Ritsumeikan Social Sci Rev. 2016;52:77–91.
- Taylor A, Olofson E, Novak W. Enhancing student retention of prerequisite knowledge through pre-class activities and in-class reinforcement. Biochem Mol Biol Educ. 2017;45:97–104.
- Ghedira S, Pino P, Bourhis G. Conception and experimentation of a communication device with adaptive scanning. ACM Trans Access Comput. 2009;1(3):1–23.
- Morris MA, Dudgeon BJ, Yorkston K. A qualitative study of adult AAC users’ experiences communication with medical providers. Disab Rehab Assist Technol. 2013;8(6):472–81.
- Andou Y. The relationship between Social skill and burnout in nurses who care for patients with neurological intractable illness. Japan Intractable Ill Nursing Soc. 2007;12(2):101–12.
- Huggins JE, Wren PA, Guis KL. What would brain-computer interface users want? opinions and priorities of potential users with amyotrophic lateral sclerosis. Amyotroph Later Scler. 2011;12(5):318–24.
- Terry VR, Terry PC, Moloney C, Bowtell L. Face-to-face instruction combined with online resources
- improves retention of clinical skills among undergraduate nursing students. Nurse Educ Today. 2018;61:15–19.
Appendix 1. Pre-test/post-test
All topics were extracted from the guidebook summary (28). They comprised ten questions with participants selecting two of five choices. Each asterisk showed correct answers. Participants answered the test at the beginning and end of the program in 10 min. The pre-test/post-tests were the same.

