ABSTRACT
Healthcare has been shifting toward individuals participating in decision-making and empowered to be active in their treatment, and health monitoring. The term “participatory health informatics” (PHI) started to appear in literature. A clear definition of PHI is missing, and facets of PHI still have to be shaped. The objective of this paper is to offer a definition of PHI considering themes and technologies that make healthcare participatory. We searched Pubmed, ACM Digital Library, IEEE Xplore, EMBASE, and conference proceedings for articles that reported about use of information technology or informatics in the context of PHI. We performed qualitative synthesis and reported summary statistics. 39 studies were eligible after screening 382 titles and abstracts and reviewing 82 full texts. The top 5 person-centered key themes related to PHI included empowerment, decision-making, informed patient, collaboration, and disease management. Finally, we propose to define PHI as multidisciplinary field that uses information technology as provided through the web, smartphones, or wearables to increase participation of individuals in their care process and to enable them in self-care and shared decision-making. Goals to be achieved through PHI include maintaining health and well-being; improving the healthcare system and health outcomes; sharing experiences; achieving life goals; and self-education.
Introduction
The health discipline and healthcare itself have been undergoing a paradigm shift. One in which informed and connected patients are altering the traditional course of health and wellbeing management through greater information availability, social connectedness and support, collaboration, choice, and autonomy over health decisions.Citation1,Citation2 This shift lies at the heart of participatory health or medicine, which inherently describes this transformation toward collaboration, empowerment, and shared decision-making about health.Citation2 However, it is still unclear what exactly shapes participatory health informatics (PHI), in which health conditions and patient-centered activities it is applied, and by what technologies it is undertaken. It is this notion that this paper seeks to examine.
Both providers of healthcare and health consumers are beginning to realize the value that a more tailored and individualized approach can bring.Citation2,Citation3 Greater person (or patient) centricity can enhance the self-management process.Citation3,Citation4 It has been widely published that positive health experiences lead to greater patient empowerment, activation, engagement, and adherence to positive health behaviors.Citation5,Citation6 Person-centredness advocates that healthcare be aligned with individualized goals, as well as biomedical causes of illness, and other aspects of psychosocial health. In this sense, the focus is on what is meaningful to the individual living with and managing the health condition.Citation6,Citation7 With this in mind, healthcare providers are being prompted to consider better accommodating patient-specific goals, wishes, and needs to ensure shared-decision making. With greater shared decision-making, communication improves, and so too patient autonomy, self-efficacy, and satisfaction.Citation3,,Citation7,,Citation8 Ultimately, the aim of these efforts is to support achieving optimal health outcomes.
Twenty-first century models of healthcare and self-management support the possibilities that various digital information technologies can bring to supporting participatory health.Citation2,Citation3 Particularly in reference to the underlying notions of participation, collaboration, and empowerment, various technologies are becoming increasingly recognized for their participatory health enabling effect; these include but are not limited to social media platforms, mobile health (apps and devices), self-quantification, remote monitoring and sensing, digital gaming solutions, personally controlled electronic health records, virtual and augmented reality devices, and telemedicine technologies.Citation2,Citation9
Over the last 20 years, there has been a steady increase in the amount of published literature framed around patient participation in health, from around 7,000 PubMed indexed articles in year 2000 to over 25,000 articles in 2019. However, despite increasing interest and recognition of the importance of participatory person-centric approaches in the realm of informatics, no formal definition exists for PHI. Therefore, the objective of this study is to both unpack and synthesize the paradigm in more depth, as well as offer the health informatics community a working definition for PHI. This brings the peripheral benefit of creating an enhanced way to catalog efforts and literature related to the discipline to support future health intervention and research endeavors.
Methods
This study follows an interpretivist approach (scoping review) underpinning secondary research to identify key facets and informatics themes within participatory health and medicine literature. Sub-questions driving this analysis include:
What are the key person-centered themes that make healthcare participatory? (i.e. empowerment, shared-decision making, institutional culture, etc.)
Which health conditions are most frequently reported in the PHI paradigm? What particular types of conditions lend themselves to participatory health?
Which stakeholders are most frequently reported in PHI?
Which technologies are most frequently represented in the PHI-related literature?
What person-centered activities lie at the heart of PHI? (i.e. quantified-self, social networking, information seeking, shared-decision making, research, etc.)
Search strategy
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) criteria guided the conduct and reporting of the review.Citation10 The search was carried out between March 20th and 25th, 2020. The search strategy covered all articles published during the period 2010–2019 included in Pubmed; ACM Digital Library; IEEE Xplore; and EMBASE comprising the following text words: “Participatory health” or “Participatory medicine”. Additionally, we searched for gray literature in proceedings of selected conferences in the field of Health/Medical Informatics for the period 2010–2019:
International Medical Informatics Conference (MedInfo)
Medical Informatics Europe Conference (MIE)
European Federation for Medical Informatics Special Topics Conferences (EFMI STC)
Scandinavian Health Informatics conferences (SHI)
Inclusion and exclusion criteria
Articles were included in this review if: 1) they referred to informatics or included a “definition/explanation” of what informatics is in the context of participatory health; and 2) they were published in the following languages: English, German, or Spanish.
Eligibility and data extraction
All references captured by the search engines were uploaded to EndNote X9 and Rayyan QCRI. Duplicates were identified and removed. In order to assess the eligibility of the articles, all titles and abstracts were examined by two independent reviewers. In a second round, the full-text of the selected articles were extracted and carefully analyzed to confirm their eligibility by two independent reviewers. Eligibility doubts were discussed until reaching agreement. The selected articles were included in the qualitative synthesis.
Three reviewers extracted the data from the selected studies regarding: publication type; health condition(s) represented; stakeholders (participants/population); participatory health-enabling technologies utilized; and health-related activities associated. The data were abstracted into a Microsoft Excel spreadsheet standardized for this review. We also collected definitions of PHI in case the term was defined in a paper.
Results
Sample
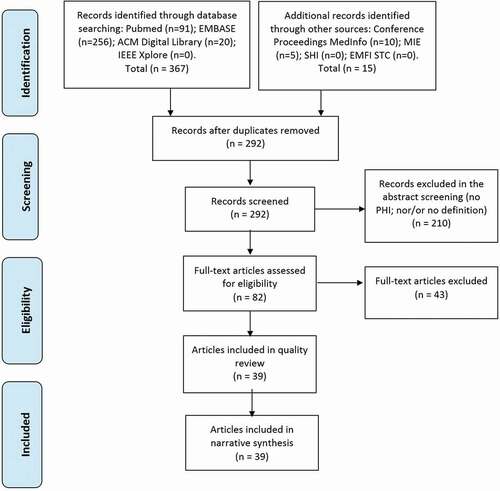
A total of 382 records were identified and 39 met the inclusion criteria, and therefore were included in the qualitative synthesis (see search strategy in Appendix 1; and flowchart of the selection procedure in ).
Publication type
Regarding the publication type of the included articles referring to PHI, we found a third of them were original articles, while the rest were classified as opinion papers, reviews, essays, abstracts or posters, and letters to the editor. See summary of publication types and references in each category in Table 1.
Table 1. Publication type
Health conditions and stakeholders
Regarding the health conditions that are reported in the participatory health paradigm: 18 among the 39 included papers did not refer to a specific health condition or medical specialty (46.1%). Among the 23 remaining papers 7 referred to medical specialties (17.9%), and 14 to specific health conditions (35.9%). The results are shown in Table 2.
Table 2: Health conditions represented in PHI literature
Regarding the represented stakeholders, most of the publications on PHI referred to patients (19/39, 48.7%),Citation1,Citation9,Citation11–27 healthcare professionals (9/39, 23%),Citation9,Citation11,Citation12,Citation16,Citation19,Citation20,Citation24,Citation28,Citation29 and citizens (7/39, 17.9%).Citation9,Citation13,Citation23,Citation28–31 A couple of publications also referred to researchers and other scientists (2/39, 5.1%).Citation18,Citation29
Technologies
We identified a broad range of technologies used in the reported research in the context of participatory health. Most prevalent was the use of social media, social networks, and discussion forums, reported in 56.4% of the articles. Wearables, self-care technologies, and self-tracking devices were the next most mentioned technology (23.1%). The mentioned technologies in PHI articles, as well as their references, are shown in Table 3.
Table 3: Technologies used in participatory health literature
Key themes
Among the 39 articles reviewed as a part of this scoping review, 14 person-centered themes emerged, with 5 themes being mentioned by 6 or more of the articles. These top 5 themes included empowerment/autonomy (17/39, 43.6%), decision-making (12/39, 30.7%), informed patient/health literacy (9/39, 23.1%), disease management/self-management (6/39, 15.4%), and patient–provider relationship/collaboration (5/39, 12.8%). The remaining 10 themes were noted in 1 or 2 papers, and are listed in Table 4.
Table 4. Themes in articles involving a participatory health approach
Person-centered activities in PHI
At the heart of PHI are the activities in which stakeholders engage. Within the identified studies, a handful of discrete person-centered participatory health activities can be observed (e.g. social networking, quantified self, information seeking, etc.). Nearly half of the identified studies in this evolving space comment on the field of PHI in a general sense, i.e. not specifying in which activities stakeholders engage (17/39, 43.6%).
Of the final 39 included studies, the following activities could be more readily identified: patient-practitioner communication (10/39, 25.6%), social networking (9/39, 23.1%), and in equal numbers; self-quantification (6/39, 15.4%), shared decision-making (6/39, 15.4%), information seeking (6/39, 15.4%), and crowd-sourcing (6/39, 15.4%), as noted in Table 5.
Table 5: Person-centered activities in PHI
Discussion
Principal findings
The existing research in the PHI field is centered on social media, social networks, and discussion forums. Recent achievements including wearables, mHealth apps, and self-tracking devices, are starting to get included into this topic of PHI. Supported activities are mainly social networking/communication, self-quantification, information seeking, and shared decision-making. Accordingly, the role of the patient gets strengthened through PHI developments by delivering new opportunities to communicate, to get information, and to assess data.
What themes does PHI cover?
In our review, we found that the most common theme, patient empowerment and autonomy, was noted as a key theme in almost half of the manuscripts. Authors of the articles citing patient empowerment noted its importance both as an applied phenomenon (e.g., patients take control of their own health, patients can actively participate in democratized healthcare structures), as well as a general characteristic experienced by patients engaging in participatory health. One paperCitation32 noted that the empowerment experienced by patients involved in participatory health gave them the capability to act as primary providers of (their own) healthcare, an action that is clearly beyond the role patients play in non-participatory healthcare environments. The authors noted that the empowerment aspect of participatory health challenges the traditional healthcare paradigm, allowing patients to manage their health with greater autonomy.
The second most common theme among the articles was participatory health as a promoter of decision-making, both for one’s self and in conjunction with members of the healthcare team. Within this theme, authors referenced the evolution of patients from passive recipients of health information and proscribed response to active partners in decisions about priorities, goals, and treatment – even noting participation as equals in such discussions. Participatory health is driven by, and in-turn supports, synergies between social media and the individual needs of patients. The authors noted that the technology that facilitates participatory approaches to healthcare, such as self-trackers and mobile apps, supports sharing of decision-making. It was also suggested that participatory health should benefit healthcare systems in that patients who have a greater role in making decisions about their care are more likely to adhere to treatment plans.
Concepts related to being an informed patient and health literacy, cited by 9 papers,Citation9,Citation11,Citation19,Citation20,Citation26,Citation27,Citation33–35 were the third most common theme. The importance of high-quality patient education has long been recognized as a key element in motivated patients to act in the best interest of their health, so it is not surprising that literature on participatory health recognizes the centrality of health information and health literacy. The authors noted the importance of social media and the sharing of information among patients as a driver of participatory health. Too, being an informed patient is sometimes connected with patient empowerment, and availability of health information furthers empowerment by increasing knowledge.
Participatory health supports and, potentially, extends the patient–provider relationship. Through greater shared knowledge, increasingly proactive efforts by patients, and online tools that support collaboration, relationships between patients and members of their care team are strengthened and promoted. Participatory health enables greater communication among patients and providers, as well as supports the information sharing that can lead to trust and confidence in relationships. Not only are patients empowered in participatory health, but their connections to healthcare systems also are strengthened. Disease management and self-management of health conditions, also commonly cited in articles about participatory health, has long been recognized as a recurring strategy among patients for personal health improvement.
The most common themes covered by PHI (i.e., patient empowerment and autonomy, decision-making, concepts related to informed patient and health literacy, as well as patient–provider relationship) are also the main focus of participatory medicine field.Citation2 The difference between these two closely related fields would lie on the use of participatory health technologies to enable them.
Which stakeholders and health conditions are represented in PHI?
The participatory health model refers to the involvement of patients in health by taking a central role and participating in decisions that affect their health.Citation1 This model is becoming more popular and replacing the traditional and paternalistic top-down approach in healthcare. Participatory health also refers to engaging with citizens to take an active interest in health, and making healthy choices, which additionally contributes to reducing health inequities.Citation36,Citation37
In PHI articles, the most commonly mentioned stakeholders are also patients, healthcare professionals, and citizens in general. PHI involves technologies that enhance participation and engagement, and favors better decision-makingCitation38 Therefore, additional stakeholders, such as health informaticians or service developers, could be represented.
Regarding the targeted health conditions, in our review we have found that almost half of the articles dealt with health issues in general, and were not targeting specific diseases. Although we found diversity in the targeted health conditions or medical specialties, there are still a lot of conditions and well-being-related issues that could also be represented in PHI articles.
Patients, healthcare professionals and all citizens in general are the involved stakeholders in participatory medicine field and in PHI too. However, the participatory medicine field would refer to different stakeholders involvement in general, and mostly happening during the traditional communication arenas (i.e., in face-to-face medical consultations).Citation2 In PHI, participatory health technologies would specifically be the enablers of the different stakeholders involvement.
Which technologies are involved in PHI?
Among the technologies reported in the context of PHI, we can distinguish three types of support that is offered by the different technologies:
Web (2.0) tools (blogs, forums, social networks, etc.) for community support,
Wearables, self-tracking technologies, etc., as self-care support,
mHealth apps, eHealth tools, etc., for supporting healthcare provision.
Technologies for community support marked the beginning of PHICitation39 and still dominate the field of PHI as the results show. These technologies enable patients to exchange information and experiences on diseases or treatments, to get mental support by the community, to relieve themselves by writing about health or treatment experiences. Social media channels provide efficient, ubiquitous and user-friendly platforms that can encourage participation, engagement and action.Citation28 However, there are several issues that hamper the application of social media in practice, which are privacy, security and misinformation.Citation40 Social media information may provide manipulated and false content, as it has been demonstrated in the recent COVID-19 outbreak.Citation41 As well as a false sense of privacy, as demonstrated by the finding that Facebook data can be used to predict personal attributes such as ethnicity, sexual orientation, and substance use.Citation42 In addition, we can recognize the trend that technologies gain in interest in the context of PHI that rather focus on the individual patient–physician relationship as it is realized by mHealth apps or eHealth tools. These technologies can be integrated in healthcare provision, and have potential in supporting communication and data collection to be used in the achievement of personal health goals. Patient involvement and engagement as it is in the center of PHI can be well realized with such technologies enabling data monitoring and even 24/7 support which could be relevant in mental diseases.Citation43 Artificial intelligence, conversational user interfaces, gamification or medical avatars are started to be used in mHealth apps, for facilitating interaction, increasing user engagement and adapting to individual health goals and preferences. A third trend regarding technologies, is self-care and self-tracking technologies that even without interaction with a healthcare provider, can be applied by a patient to achieve certain health and wellness goals. In summary, we can see the various facets of individual needs and within healthcare treatment reflected in the PHI research developments: From communities, we move to support of the individual in self-care and patient–physician relationship and actual intervention through mHealth.
How could PHI be defined?
Because we could not identify a concrete definition of PHI in the reviewed literature, we use these findings to offer a definition:
“PHI is a multidisciplinary field closely related to participatory medicine. PHI uses information technology as provided through the web, smartphones, or wearables to increase participation of individuals in their care process, and to enable them in self-care and decision-making. PHI deals with the resources, devices, and methods required to support active participation and engagement of the stakeholders. It has been applied in the context of various medical conditions requiring long-term disease management. The individual is placed in the center of decision-making processes, the care process, and/or the self-care or self-management process, and has to communicate with the care team. PHI delivers the tools – information, software, and community – for this work. PHI also studies the effects of the use of such tools on the patient, care process, or physician–patient relationship, including ethical issues. The goals to be achieved through PHI include maintaining health and well-being; improving the healthcare system; improving health outcomes; sharing experiences; achieving life goals; and self-education”.
Strengths and limitations
This scoping review was conducted to identify the facets of PHI, in particular the themes, medical conditions, technologies, medical conditions, and person-centered activities involved. To the best of our knowledge, this study is the first attempt to formally shape PHI and to offer a concrete definition of this emerging research topic. This study helped us formulate a working definition of PHI to be used in future discussions and shapes of this research topic. To retrieve as many relevant articles as possible, the most commonly used databases in health and information technology fields were searched. As two reviewers independently selected the articles and three reviewers extracted the data, the selection bias in this review was minimal.
Due to practical constraints, we could not search interdisciplinary databases (e.g., Web of Science and ProQuest), conduct manual search across additional conference proceedings and other sources, and contact experts. Further, the search in the current review was restricted to English, German, and Spanish articles. Accordingly, it is likely that this review missed some publications. Additionally, we restricted the search to papers that include the terms “participatory health” or “participatory medicine”. We might have missed relevant papers that did not used explicitly those keywords but deal with a relevant topic. Several terms can be related to PHI, but these were too broad for conducting a review. However, the results of our study may help to define future studies seeking to examine PHI by uncovering key terms, phrases, and themes.
Conclusion
The breadth of technologies and themes which have been applied within PHI and continues to be applied to-date suggests that this remains an active field of research. Starting with social media starting around 2003, newly upcoming technologies became more and more involved as this study showed. New technologies as well as benefits that were recognized helped move forward the research and implementation of PHI in daily practice. However, several questions, in particular regarding the implementation of PHI in daily practice remain open: i.e. What are the implications of PHI for people living with life-long health conditions? Few publications have examined how the “therapeutic” effect persists or wanes over time, or whether there is a risk of overreliance on technology?
One of the first uses of the idea of PHI was in 2008, where it was used interchangeably with Health 2.0, Medicine 2.0, and eHealth. The term concerned the “use of a specific set of Web (2.0) tools (blogs, podcasts, tagging, search, wikis, etc.) by actors in health care including doctors, patients, and scientists, … in order to personalize health care, collaborate, and promote health education.”.Citation39 Since then, a wide ecosystem of pa rticipatory health efforts has emerged, offering individuals diverse technologies that support their participation. Such participatory health efforts include social media, health applications on mobile phones, or p ersonally controlled electronic health records. Other research on PHI already lists additional technologies that were not detected in our review, but will probably become more apparent in future, including direct-to-consumer tests such as genomic and blood tests, and crowdsourced health collaboration and experimentation communities.*Citation2,Citation18,Citation44–52
Declaration of interest
The authors report no conflicts of interest.
References
- deBronkart D. The patient’s voice in the emerging era of participatory medicine. Int J Psychiatry Med. 2018;53 (5–6):350–60. doi:https://doi.org/10.1177/0091217418791461.
- Swan M. Health 2050: the realization of personalized medicine through crowdsourcing, the quantified self, and the participatory biocitizen. Journal of Personalized Medicine. 2012;2 (3):93–118. doi:https://doi.org/10.3390/jpm2030093.
- Martin-Sanchez FJ, Lopez-Campos GH. The new role of biomedical informatics in the age of digital medicine. Methods Inf Med. 2016;55 (5):392–402. doi:https://doi.org/10.3414/ME15-02-0005.
- Glasziou P. The paths from research to improved health outcomes. Evid Based Nurs. 2005;8 (2):36–38. doi:https://doi.org/10.1136/ebn.8.2.36.
- Battersby M, Von Korff M, Schaefer J, Davies C, Ludman E, Greene SM, Parkerton M, Wagner EH. Twelve evidence-based principles for implementing self-management support in primary care. Joint Commission Journal on Quality and Patient Safety. 2010;36 (12):561–70. doi:https://doi.org/10.1016/S1553-7250(10)36084-3.
- Finset A. Patient participation, engagement and activation: increased emphasis on the role of patients in healthcare. Patient Educ Couns. 2017;100 (7):1245–46. doi:https://doi.org/10.1016/j.pec.2017.05.011.
- Reuben DB, Tinetti ME. Goal-oriented patient care–an alternative health outcomes paradigm. N Engl J Med. 2012;366 (9):777–79. doi:https://doi.org/10.1056/NEJMp1113631.
- De Bronkart D. From patient centred to people powered: autonomy on the rise. BMJ (Online). 2015;350:h148.
- Hood L, Flores M. A personal view on systems medicine and the emergence of proactive P4 medicine: predictive, preventive, personalized and participatory. N Biotechnol. 2012;29 (6):613–24. doi:https://doi.org/10.1016/j.nbt.2012.03.004.
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6 (7):e1000097. doi:https://doi.org/10.1371/journal.pmed.1000097.
- Con D, Jackson B, Gray K, De Cruz P. eHealth for inflammatory bowel disease self-management - the patient perspective. Scand J Gastroenterol. 2017;52 (9):973–80. doi:https://doi.org/10.1080/00365521.2017.1333625.
- Kuziemsky C, Astaraky D, Wilk S, Michalowski W, Andreev P A Framework for incorporating patient preferences to deliver participatory medicine via interdisciplinary healthcare teams. Framework for incorporating patient preferences to deliver participatory medicine via interdisciplinary healthcare teams. AMIA Annual Symposium proceedings/AMIA Symposium AMIA Symposium. 2014; 2014: 835–44.
- Maier M, Takano T, Sapir-Pichhadze R. Changing paradigms in the management of rejection in kidney transplantation: evolving from protocol-based care to the era of P4 medicine. Canadian Journal of Kidney Health and Disease. 2017;4:2054358116688227. doi:https://doi.org/10.1177/2054358116688227.
- Merolli M, Gray K, Martin Sanchez F. TASoMe: validating a framework to generate evidence bout health outcomes from social media use. Building continents of knowledge in oceans of data: the future of co-created ehealth – proceedings of MIE 2018. Studies in health technology and informatics. 2018. 606–610.
- Merolli M, Gray K, Martin-Sanchez F. Patient participation in chronic pain management through social media: a clinical study. Stud Health Technol Inform. 2016; 225:577–81.
- Merolli M, Marshall C, Pranata A, Paay J, Sterling L. User-centered valuespecifications for technologies supporting chronic low-back pain management. MEDINFO 2019. Studies in health technology and informatics. 2019. 1288–1292. doi: https://doi.org/10.3233/SHTI190434.
- Storni C. Design challenges for ubiquitous and personal computing in chronic disease care and patient empowerment: a case study rethinking diabetes self-monitoring. Personal Ubiquitous Comput. 2014;18 (5):1277–90. doi:https://doi.org/10.1007/s00779-013-0707-6.
- Swan M. Crowdsourced health research studies: an important emerging complement to clinical trials in the public health research ecosystem. J Med Internet Res. 2012;14 (2):e46. doi:https://doi.org/10.2196/jmir.1988.
- Yellowlees P, Nafiz N. The psychiatrist-patient relationship of the future: anytime, anywhere. Harv Rev Psychiatry. 2010;18 (2):96–102. doi:https://doi.org/10.3109/10673221003683952.
- Denecke K, Gabarron E, Grainger R, Konstantinidis ST, Lau A, Rivera-Romero O, Miron-Shatz T, Merolli M. Artificial intelligence for participatory health: applications, impact, and future implications. Yearb Med Inform. 2019;28 (1):165–73. doi:https://doi.org/10.1055/s-0039-1677902.
- Househ M, Grainger R, Petersen C, Bamidis P, Merolli M. Balancing between privacy and patient needs for health information in the age of participatory health and social media: a scoping review. Yearb Med Inform. 2018;27 (1):29–36. doi:https://doi.org/10.1055/s-0038-1641197.
- deBronkart D, Gimme EG. My damn data (and let patients help!): the #GimmeMyDamnData manifesto. J Med Internet Res. 2019;21 (11):e17045. doi:https://doi.org/10.2196/17045.
- Graedon T, Graedon J. Let patients help with diagnosis. Diagnosis (Berlin, Germany). 2014;1 (1):49–51. doi:https://doi.org/10.1515/dx-2013-0006.
- Haridy J, Iyngkaran G, Tse E. An eHealth model of care for community hepatitis c management: the Health Elink project. Journal of Gastroenterology and Hepatology (Australia). 2017;32:70–71.
- Muscat M. Blackgammon: a grounded participatory design of a preconception health promotion “alternate reality game” for adolescent indigenous australian women. In: CHI ’13 extended abstracts on human factors in computing systems. Paris (France): Association for Computing Machinery; NY, USA, 2013, 1949–1952. https://doi.org/https://doi.org/10.1145/2468356.2468708.
- Rubenstein EL Crowdsourcing health literacy: the case of an online community. Proceedings of the 76th ASIS&T Annual Meeting: Beyond the Cloud: Rethinking Information Boundaries. Montreal (Quebec, Canada): American Society for Information Science, 2013.
- Riva S, Pravettoni G. Web as a new shortcut in patient-doctor communication and medical care relationship. Australasian Medical Journal. 2017;10:69.
- Gabarron E, Bradway M, Fernandez-Luque L, Chomutare T, Hansen AH, Wynn R, Årsand E. Social media for health promotion in diabetes: study protocol for a participatory public health intervention design. BMC Health Serv Res. 2018;18 (1):414. doi:https://doi.org/10.1186/s12913-018-3178-7.
- Koldkjaer Sølling I, Carøe P, Lindgren K, Siggaard Mathiesen K. Online communication and chronic obstructive pulmonary disease (COPD). MEDINFO 2015. Studies in health technology and informatics. 2015; 216:910.
- Nieto-Riveiro L, Groba B, Miranda MC, Concheiro P, Pazos A, Pousada T, Pereira J. Technologies for participatory medicine and health promotion in the elderly population. Medicine. 2018;97 (20):e10791. doi:https://doi.org/10.1097/MD.0000000000010791.
- Svedberg P, Arvidsson S, Larsson I, Carlsson IM, Nygren JM. Barriers and enablers affecting successful implementation of the electronic health service sisom: multicenter study of child participation in pediatric care. J Med Internet Res. 2019;21 (11):e14271. doi:https://doi.org/10.2196/14271.
- Al-Shorbaji N, Bellazzi R, Gonzalez Bernaldo de Quiros F, Koch S, Kulikowski CA, Lovell NH, Maojo V, Park H-A, Sanz F, Sarkar IN. Discussion of “The new role of biomedical informatics in the age of digital Medicine”. Methods Inf Med. 2016;55 (5):403–21. doi:https://doi.org/10.3414/ME15-12-0005.
- Kantor D, Bright JR, Burtchell J. Perspectives from the patient and the healthcare professional in multiple sclerosis: social media and participatory medicine. Neurology and Therapy. 2018;7 (1):37–49. doi:https://doi.org/10.1007/s40120-017-0088-2.
- Lopez-Campos G, Merolli M, Martin Sanchez F. Biomedical informatics and the digital component of the exposome. MEDINFO 2017. studies in health technology and informatics. 2017;245:496–500.
- Schmietow B, Marckmann G. Mobile health ethics and the expanding role of autonomy. Medicine, Health Care and Philosophy. 2019;22 (4):623–30. doi:https://doi.org/10.1007/s11019-019-09900-y.
- Boyce T, Brown C. Engagement and participation for health equity. planners rhipfp-ma. editor. World Health Organization regional Office, Copenhagen, Denmark;2017
- Frances F, La Parra-Casado D. 2019. Participation as a driver of health equity. World health organization The WHO Regional Office for Europe, Copenhagen, Denmark.
- Coughlin S, Roberts D, O’Neill K, Brooks P. Looking to tomorrow’s healthcare today: a participatory health perspective. Intern Med J. 2018;48 (1):92–96. doi:https://doi.org/10.1111/imj.13661.
- Hughes B, Joshi I, Wareham J. Health 2.0 and medicine 2.0: tensions and controversies in the field. J Med Internet Res. 2008;10 (3):e23. doi:https://doi.org/10.2196/jmir.1056.
- Petersen C, Lehmann CU. Social media in health care: time for transparent privacy policies and consent for data use and disclosure. Appl Clin Inform. 2018;9 (4):856–59. doi:https://doi.org/10.1055/s-0038-1676332.
- Duraisamy B, Rathinaswamy J, Sengottaiyan K. Social media reigned by information or misinformation about COVID-19: a phenomenological study. SSRN Electronic Journal. 2020;09:585–602.
- Kosinski M, Stillwell D, Graepel T Private traits and attributes are predictable from digital records of human behavior. Proceedings of the National Academy of Sciences of the United States of America. 2013; 110 (15): 5802–05.doi: https://doi.org/10.1073/pnas.1218772110.
- Kumar A, Wang M, Riehm A, Yu E, Smith T, Kaplin A. An automated mobile mood tracking technology (mood 24/7): validation study. JMIR Mental Health. 2020;7 (5):e16237. doi:https://doi.org/10.2196/16237.
- Van de Belt TH, Berben SA, Samsom M, Engelen LJ, Schoonhoven L. Use of social media by Western European hospitals: longitudinal study. J Med Internet Res. 2012;14 (3):e61. doi:https://doi.org/10.2196/jmir.1992.
- Nair S QS x NUI: towards natural user interfaces for personal health information. Proceedings of the 2016 ACM International Joint Conference on Pervasive and Ubiquitous Computing: Adjunct. Heidelberg, Germany: Association for Computing Machinery, 2016.
- Alonso SG, de la Torre Diez I, Zapirain BG. Predictive, personalized, preventive and participatory (4P) medicine applied to telemedicine and eHealth in the literature. J Med Syst. 2019;43 (5):140. doi:https://doi.org/10.1007/s10916-019-1279-4.
- Gray K, Martin-Sanchez FJ, Lopez-Campos GH, Almalki M, Merolli M. Person-generated data in self-quantification. A health informatics research program. Methods Inf Med. 2017;56 (1):40–45. doi:https://doi.org/10.3414/ME15-02-0006.
- Parish MB, Fazio S, Chan S, Yellowlees PM. Managing psychiatrist-patient relationships in the digital age: a summary review of the impact of technology-enabled care on clinical processes and rapport. Current psychiatry reports. 2017. 19 (11):90. doi: https://doi.org/10.1007/s11920-017-0839-x.
- Quattri F. Pharmacovigilance and participatory medicine through social media-we are still not there. BMJ Evidence-Based Medicine. 2018;23:A30.
- Bradley WG, Golding SG, Herold CJ, Hricak H, Krestin GP, Lewin JS, Miller JC, Ringertz HG, Thrall JH Globalization of P4 medicine: predictive, personalized, preemptive, and participatory - Summary of the Proceedings of the Eighth International Symposium of the International Society for Strategic Studies in Radiology, August 27– 29,2009. Radiology. 2011; 258: 571–82.
- Erikainen S, Pickersgill M, Cunningham-Burley S, Chan S. Patienthood and participation in the digital era. Digital Health. 2019;5:2055207619845546. doi:https://doi.org/10.1177/2055207619845546.
- Borda A, Molnar A, Kostkova P Serious games and participatory research in public health. Proceedings of the 9th International Conference on Digital Public Health. Marseille (France): Association for Computing Machinery 2019. Palais des Congrès et des Expositions. Marseille, France, November 20, 2019.