Abstract
Purpose: Evidence base to support the use of the effortful swallow in clinical populations with dysphagia is currently lacking. This study aims to quantify the effects of effortful swallowing on pharyngeal swallowing biomechanics in adults with dysphagia using pharyngeal high-resolution manometry (PHRM).
Method: ManoScan HRM equipment with a 4.2 mm pressure catheter was used. Participants completed duplicate 10ml baseline and 10ml effortful liquid (IDDSI Level 0) swallows in randomised order. PHRM data were analysed using a semi-automated online platform (www.swallowgateway.com).
Result: Fifteen adults (8 males; range 45-86 years) with mixed aetiology dysphagia (Functional Oral Intake Scale Level 2–5) were included. Median pharyngeal contractile (156.81 mmHg cm s; IQR 80.62) increased significantly (213.50 mmHg cm s; IQR 117.2) during effortful swallowing. Significant increases were also observed in velopharyngeal pressure, mesopharyngeal pressure, hypopharyngeal pressure and upper oesophageal sphincter (UOS) relaxation duration. UOS integrated relaxation pressure (IRP) was not significantly altered with effortful swallowing.
Conclusion: Effortful swallowing induced significant biomechanical changes to swallow in adults with dysphagia. Increases in global pharyngeal rigour, tongue base pressure and UOS opening duration were captured by PHRM during effortful swallowing. Further investigation in larger homogeneous clinical populations is needed to verify the physiological effects of this frequently employed intervention.
Introduction
Dysphagia management often involves the implementation of compensatory strategies and/or rehabilitation exercises to optimise a person’s swallow safety and efficiency (Easterling, Citation2017). Voluntary pharyngeal swallowing manoeuvres are commonly used to alter pharyngeal physiology and bolus flow (Logemann, Citation2008). The effortful swallow is frequently employed in clinical practice (Carnaby & Harenberg, Citation2013; Rumbach, Coombes, & Doeltgen, Citation2018). It was originally employed as a compensatory strategy to optimise tongue base contact with the posterior pharyngeal wall, increasing bolus pressure during swallowing (Witte, Huckabee, Doeltgen, Gumbley, & Robb, Citation2008). Although the effortful swallow has been considered a rehabilitative technique, there remains a lack of evidence to determine whether the swallow manoeuvre permanently alters swallowing physiology (Felix, Corrêa, & Soares, Citation2008). Despite this, recent research has demonstrated that the effortful swallow is the most frequently utilised dysphagia intervention in clinical practice across countries (Carnaby & Harenberg, Citation2013; Rumbach et al., Citation2018).
Despite the frequent use of effortful swallow, its evidence base remains limited. A recent systematic review elucidated the evidence base for the effortful swallow manoeuvre and found just two high-quality studies (Bahia & Lowell, Citation2020). Most research evaluating the impact of effortful swallowing has been conducted within healthy populations (Bahia & Lowell, Citation2020; Langmore & Pisegna, Citation2015). Findings include increased submental muscle activation and pharyngeal contractile strength (Doeltgen, Ong, Scholten, Cock, & Omari, Citation2017; Hoffman et al., Citation2012; Huckabee, Butler, Barclay, & Jit, Citation2005). Findings vary in terms of changes to upper oesophageal sphincter (UOS) opening with effortful swallowing in healthy adults (Bülow, Olsson, & Ekberg, Citation1999; Doeltgen et al., Citation2017). Of note, instructions on how to complete the effortful swallow differ across research studies (Bahia & Lowell, Citation2020).
Few studies have investigated the effects of effortful swallowing within clinical populations with dysphagia. Three studies have evaluated effortful swallowing in head and neck cancer, Parkinson’s disease and stroke populations, although participant groups were limited in size and one of these studies relied on a clinical examination (Bülow, Olsson, & Ekberg, Citation2001, Citation2002; Felix et al., Citation2008). The need to expand the evidence base for the effortful swallow is imperative to guide clinical practice. Further research to explore the effects of effortful swallowing in clinical populations has been recommended (Bahia & Lowell, Citation2020; Doeltgen et al., Citation2017).
Pharyngeal high-resolution manometry (PHRM) is an evaluation tool which is emerging into clinical dysphagia practice (Rogus-Pulia et al., Citation2020). PHRM can provide quantitative measures of physiological events that occur during swallowing which complement videofluoroscopy (VFS) and Fibreoptic Endoscopic Evaluation of Swallowing (FEES) findings and inform dysphagia treatment (Knigge, Thibeault, & McCulloch, Citation2014). PHRM has been used to evaluate the effects of rehabilitation and manoeuvres commonly used in dysphagia practice (Aoyagi et al., Citation2021; Hoffman et al., Citation2012; Regan, Citation2020). Using PHRM, these studies have been able to look beyond swallow safety and efficiency and identify subtle changes in swallowing physiology. To date, PHRM has been used with and without impedance to evaluate the effect of an effortful swallow on pharyngeal (Doeltgen et al., Citation2017; Hoffman et al., Citation2012) and oesophageal (O’Rourke et al., Citation2014) phases of swallowing in healthy adults. Interestingly, several pharyngeal and oesophageal metrics were not altered with effortful swallowing (Doeltgen et al., Citation2017; O’Rourke et al., Citation2014). This may be due to the young healthy participants in these studies who already present with optimal pressures during swallowing.
The objective of this study was to use PHRM to investigate the effect of effortful swallowing on pharyngeal swallowing physiology in adults with dysphagia. Based on previous findings, it is hypothesised that effortful swallows will induce pressure changes within the pharynx and UOS during swallowing in adults with dysphagia.
Method
Participants
This was a prospective study which obtained ethical approval from St. James’ Tallaght Research Ethics Committee (JREC). Each participant provided written informed consent. Participants were recruited consecutively from an outpatient dysphagia clinic in an acute hospital using convenience sampling. Inclusion criteria included the presence of dysphagia (minimum Functional Oral Intake Scale <6 (Crary, Mann, & Groher, Citation2005)) and a recent VFS (one-month maximum) to rule out a pharyngeal or oesophageal diverticulum. Exclusion criteria included the presence of pharyngeal or oesophageal diverticulum, head and neck cancer, tracheostomy, and recent nasal surgery.
High-resolution manometry (HRM) equipment
PHRM was completed using the ManoScan system (Medtronic, Atlanta, GA). A 4.2 mm diameter solid-state high-resolution catheter with 36 circumferential pressure sensors spaced 1 cm apart was used for all swallow trials (ManoScan, Medtronic, Atlanta, GA). The HRM catheter did not have multichannel intraluminal impedance sensors. Preparation for each PHRM examination involved calibrating the transducers at 0 and 300mmHg using externally applied pressure. Prior to catheter insertion, calibration of the equipment was completed in accordance with the manufacturer’s guidelines (Bredenoord & Hebbard, Citation2012).
Protocol
Prior to the PHRM examination, each participant was trained by a clinical specialist speech and language pathologist (CSSLP) to execute the effortful swallow. Information was provided and a demonstration of the effortful swallow was carried out by the CSSLP. The instruction provided was “squeeze hard with all your muscles as you swallow”. Once participants were observed completing the effortful swallow correctly, the PHRM examination commenced.
Participants fasted for a minimum of 4 hours prior to the PHRM examination. Each participant was seated upright on a chair with their head in a neutral position. The HRM equipment was situated next to the participant in a distraction-free clinic room. The PHRM protocol was completed by the CSSLP who received certified training in HRM and had over five years of clinical experience performing HRM examinations. Optilube was applied to the distal tip of the HRM catheter. Transnasal anaesthetic (TNA) was not applied to the nares of any participant to prevent the alteration of oropharyngeal sensation (Guiu Hernandez, Gozdzikowska, Apperley, & Huckabee, Citation2018).
The HRM catheter was inserted via the most patent nasal passage as reported by each participant (Lever et al., Citation2007). Prior to catheter insertion, participants were instructed to perform a chin tuck and sequentially swallow sips of water (IDDSI Level 0) using a straw until the catheter tip passed through the UOS into the proximal oesophagus (Doeltgen et al., Citation2017; Knigge et al., Citation2014). The HRM screen was monitored to ensure the pressure measurements from proximal velopharynx to UOS were captured. Adhesive tape was applied to the skin to fix the catheter in place. A 5-min accommodation period was permitted to normalise the pharyngeal pressure recordings.
Following the accommodation period, each participant swallowed duplicate 10 ml liquid boluses (IDDSI Level 0) under two swallow conditions. Each participant completed two non-effortful swallows (control) and two effortful swallows. The bolus consisted of a commercial still water beverage (Ballygowan® still water) which was 20–23 °C immediately prior to administration as measured by a handheld thermometer. Saline solution was not required due to the lack of impedance sensors on the catheter. As per High-Resolution Pharyngeal Manometry (HRPM) International Working Group’s recommendations, 10 ml bolus volumes were selected (Omari et al., Citation2020). A verbal cue was provided prior to each trial. Specific verbal instructions were provided immediately prior to each swallow trial. Participants were instructed to “swallow as normal” for non-effortful (control) trials. Prior to effortful swallow trials, participants were instructed to “squeeze hard with all your muscles as you swallow”. Participants were instructed to swallow the whole 10ml bolus in one swallow. Where piecemeal deglutition and coughing post-swallow were observed, the trial was repeated. The order of bolus administration was randomised using www.randomizer.org. Each bolus was administered via a 20 ml syringe. A syringe was used as the method of bolus delivery to ensure uniform bolus volume between trials (O’Rourke et al., Citation2014). A minimum thirty-second time period was enforced between each trial to prevent confounding inhibition of oesophageal peristalsis (Lever et al., Citation2007). Once all trials were completed, the catheter was removed and the PHRM examination was completed.
Data collection and analysis
Data from sixty swallows was exported to a semi-automated online analysis software (www.swallowgateway.com Flinders University, Adelaide, Australia). This software has been previously used to analyse HRM data (Regan, Citation2020; Winiker, Gillman, Hernandez, Huckabee, & Gozdzikowska, Citation2019). Research has shown that this software has excellent inter and intra-rater reliability (Omari et al., Citation2016; Singendonk et al., Citation2019). Data analysis was conducted by NH and JR. The PHRM examiner labelled each swallow. Each swallow was identified and analysed by manually identifying six landmarks within Swallow Gateway. The pharyngeal metrics were provided by the semi-automated analysis. Analysis was not blinded, but the bias was minimised by the semi-automated analysis. Once the semi-automated analysis was completed, the pressure metrics provided by Swallow Gateway were inputted into Microsoft Excel. Since participants completed two trials per swallow condition (baseline, effortful), the measures from both trials were averaged for statistical analysis.
Outcome measures
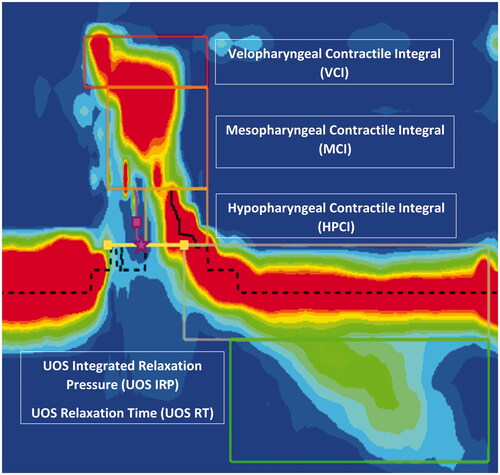
The pharyngeal outcome measures selected captured pressure and timing measurements in velopharyngeal, mesopharyngeal, hypopharyngeal and UOS regions. These measures aligned with core outcomes recommended by the HRPM International Working Group’s recommendations (Omari et al., Citation2020). Metrics are depicted in and they are defined in .
Table I. Pharyngeal high-resolution manometry metrics.
Statistical analysis
A statistical software IBM Statistical Package for the Social Sciences for Windows, Version 26.0 (IBM, Chicago, Illinois) was used to analyse PHRM metrics. Firstly, Shapiro-Wilk and Levene’s tests were completed to determine normality and equal variance, respectively (Hoffman et al., Citation2012). As data were not normally distributed, Wilcoxon signed-rank tests were used to compare median pharyngeal pressures between baseline and effortful swallow conditions. A probability of 5% (α = 0.05) determined a statistically significant difference and a 95% confidence interval was used in all tests.
Result
Participants
Fifteen participants (8 males: age range 45–86 years; mean age 63 years) with mixed aetiology dysphagia were recruited over a 3-month period. The cause and severity of dysphagia within the participant group are captured in . All participants tolerated intubation and the protocol completion rate was 100% (15 participants completed two 10ml liquid baseline swallows and two 10ml liquid effortful swallows. No adverse events (perforation, epistaxis, nausea, vomiting, vasovagal episode) were noted during the PHRM examinations.
Table II. Participant demographics.
Pharyngeal metrics
Effects on global pharyngeal pressure
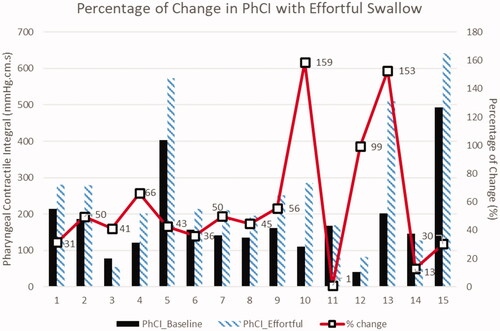
There was a statistically significant increase in median global pharyngeal rigour with effortful swallowing as measured by the pharyngeal contractile integral (PhCI) (Z = −3.124, p = 0.002) (). Effortful swallow increased the PhCI in 87% (13/15) participants on 10ml liquids ().
Table III. Pharyngeal metrics.
To identify who was benefiting from the effortful swallow, participants with a baseline PhCI below the median (156.81mmHg cm s) were identified and 71% (5/7) of those with reduced PhCI had increased PhCI with effortful swallowing. In contrast, PhCI was reduced in two of these seven participants with low baseline PhCI who had histories of unknown aetiology and stroke respectively. All (8/8) participants with a baseline PhCI at the median or above increased PhCI with effortful swallowing.
The magnitude of change in PhCI with effortful swallow across participants is captured in . Amongst the 13/15 participants who had an increased PhCI with effortful swallowing, the median percentage increase was 50% (IQR 34–83%). In the two cases where PhCI reduced with effortful swallowing, the percentage of the PhCI decrease was 13% and 41% (participants 3 and 14) respectively.
Velopharyngeal pressure
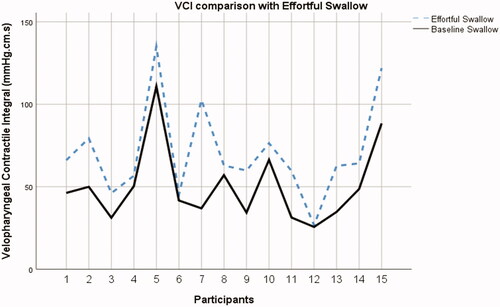
Velopharyngeal pressure was significantly increased with effortful swallowing as measured by the velopharyngeal contractile integral (VCI) (Z = −3.408, p = 0.001). Increases in VCI were observed in 100% (15/15) of participants during effortful swallows. Increases in VCI with effortful swallowing across the participant group are captured in .
Mesopharyngeal pressure
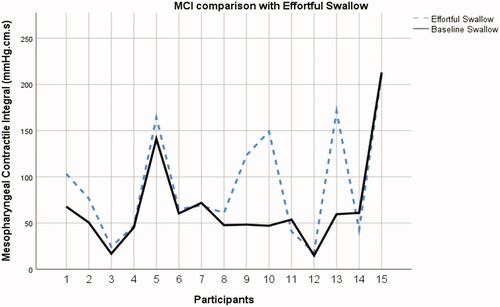
There was a statistically significant increase in tongue base to posterior pharyngeal wall pressure as measured by the mesopharyngeal contractile integral (MCI) during effortful swallows (Z = −2.215, p = 0.027) (). Increased MCI pressures were observed in 73% (11/15) during effortful swallows (). Participants with a baseline MCI below the median (53.79mmHg cm s) were identified and 100% (7/7) of those with reduced MCI at baseline had increased MCI with effortful swallowing. Decreases in MCI pressure were observed in participants with chronic obstructive pulmonary disease (COPD), auto-immune disease, unknown aetiology, and achalasia.
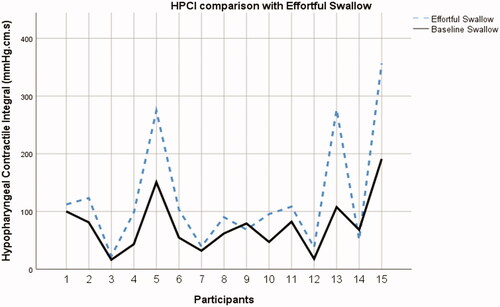
Hypopharyngeal pressure
The hypopharyngeal contractile integral (HPCI) increased significantly during effortful swallows (Z = −2.953, p = 0.003). Increases in HPCI were observed in 87% (13/15) during effortful swallows (). Participants with a baseline HPCI below the median (68.11mmHg cm s) were identified and 100% (7/7) had increased HPCI with effortful swallowing. Decreased HPCI pressure was observed in one participant with stroke and one with unknown aetiology.
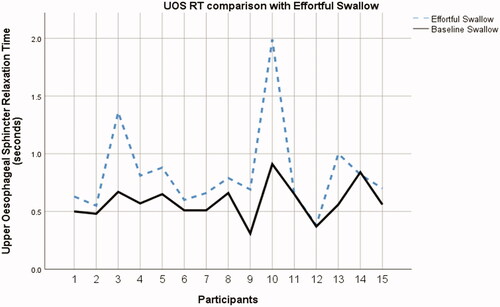
UOS relaxation time
Effortful swallowing resulted in a significant increase in UOS relaxation time (UOS RT) when compared with non-effortful swallows (Z = −3.171, p = 0.002). Increases in UOS RT were observed in 87% (13/15) during effortful swallows (). Participants with a baseline UOS RT below the median (0.56 secs) were identified and 100% (6/6) had increased UOS RT with effortful swallowing. A decrease in UOS RT was observed in one participant with an unknown aetiology of dysphagia. No change was observed in UOS RT in one participant with auto-immune disease.
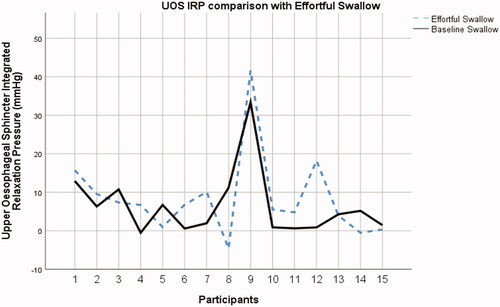
UOS integrated relaxation pressure
There was no significant alteration to UOS integrated relaxation pressure (UOS IRP) with effortful swallowing (Z = −1.193, p = 0.233). Decreases in UOS IRP were observed in 40% (6/15) during effortful swallows (). Participants with a baseline UOS IRP above the median (4.28mmHg) were identified and 66% (4/6) had decreased UOS IRP with effortful swallowing. A decrease in UOS IRP was observed in participants with stroke, lung cancer, multiple sclerosis, achalasia, and unknown aetiology.
Discussion
This study used PHRM to evaluate the physiological effects of the effortful swallow in adults with mixed aetiology dysphagia. Findings revealed effortful swallows significantly increased global pharyngeal contractility in adults with dysphagia on thin liquids. This finding supports the hypothesis that the effortful swallow manoeuvre generates greater pharyngeal pressure when compared with non-effortful swallowing.
Increased pressure with effortful swallowing was observed at the level of the velopharynx, mesopharynx and hypopharynx. This global pressure increase aligns with previous research (Takasaki, Umeki, Hara, Kumagami, & Takahashi, Citation2011) and indicates that effortful swallowing does not simply increase tongue base retraction, but increases contraction of the superior and inferior pharyngeal constrictor muscles. Effortful swallowing was found to significantly increase UOS RT when compared with non-effortful swallowing in adults with dysphagia. This finding is significant since the aim of the effortful swallow is to increase pharyngeal pressure to generate greater pharyngeal force to propel the bolus through the pharynx into the oesophagus (O’Rourke et al., Citation2014). Alongside greater pharyngeal force, prolonged UOS RT can assist with improving pharyngeal bolus clearance (Hind, Nicosia, Roecker, Carnes, & Robbins, Citation2001). These findings suggest that the effortful swallow does more than increase tongue base to posterior pharyngeal wall contact in people with dysphagia.
It was noteworthy that UOS IRP was not significantly altered with effortful swallowing in this clinical population. The extent of UOS opening may be more challenging to modify in dysphagia intervention due to neurological or age-related changes in physiology (Kendall & Leonard, Citation2002). However, another plausible theory for the lack of change in the extent of UOS opening is that the UOS IRP is not a suitable measure of UOS opening extent. Use of impedance measures such as maximum admittance or bolus presence time to capture the extent of UOS opening with effortful swallowing may be more suitable in future studies. It is notable, however, that UOS admittance did not increase with effortful swallowing in previous PHRM research in a healthy participant group (Doeltgen et al., Citation2017).
In comparison to normative data published in previous research, global pharyngeal rigour was low in this participant group at baseline (O’Rourke, Humphries, Lazar, & Martin‐Harris, Citation2017). Low global pharyngeal rigour has been associated with pharyngeal dysfunction and aspiration on VFS (O’Rourke et al., Citation2014). Identification of manoeuvres such as the effortful swallow which can increase global pharyngeal pressure during swallowing is of great value to clinical practice. Alteration of global pharyngeal pressure with effortful swallow in this study aligns with a previous study which measured PhCI in healthy participants during effortful swallows (Doeltgen et al., Citation2017).
The findings in this study revealed that effortful swallowing increased pressure in the velopharyngeal and mesopharyngeal regions. Differing results have been reported in respect of the physiological changes in pressure in the mesopharyngeal region during effortful swallowing (Hoffman et al., Citation2012; Takasaki et al., Citation2011). Hoffman and colleagues (Citation2012) revealed a slight decrease in mesopharyngeal pressure during effortful swallows in healthy adults. Having reported an increase in velopharyngeal pressure and a decrease in mesopharyngeal pressure, Hoffman and colleagues (Citation2012) posited that effortful swallowing is a floor of mouth event rather than a base of tongue event. However, the conclusion posed by Hoffman and colleagues (Citation2012) is not supported by the findings in this study since effortful swallowing resulted in an increase in both velopharyngeal and mesopharyngeal regions in adults with dysphagia.
In contrast to the findings posited by Hoffman and colleagues (Citation2012), Takasaki and colleagues (Citation2011) reported significant increases in velopharyngeal and meso-hypopharyngeal pressure during effortful swallowing in healthy adults. Of note, both studies (Hoffman et al., Citation2012; Takasaki et al., Citation2011) evaluated the effortful swallow manoeuvre on adults who had no history of dysphagia and reported contrasting findings. Different methods were used in this study when compared with previous PHRM studies (Doeltgen et al., Citation2017; Hoffman et al., Citation2012; Takasaki et al., Citation2011). Previous studies used 5 ml liquid boluses to evaluate the physiological changes in the pharynx during effortful swallows in young healthy adults. In contrast, 10 ml liquid boluses were used in this study to evaluate the effects of effortful swallowing in middle to old-aged patients with dysphagia. In previous studies, researchers applied TNA to the nares of each participant prior to the PHRM examination (Doeltgen et al., Citation2017; Hoffman et al., Citation2012; Takasaki et al., Citation2011). In contrast to previous studies, TNA was not applied to any participant in this study to avoid the potential alteration of oropharyngeal sensation. This may have contributed to the different findings between previous studies (Hoffman et al., Citation2012; Takasaki et al., Citation2011) and the present study. Hoffman and colleagues (Citation2012) acknowledged the use of TNA as a limitation in their study since the researchers could not rule out any potential impact on oropharyngeal sensation. In addition, research has revealed that TNA provides no additional comfort while negatively impacting the magnitude of pharyngeal pressures (Guiu Hernandez et al., Citation2018). The most significant difference in this study was the inclusion of participants with dysphagia of mixed aetiology. With the exception of three studies (Bülow et al., Citation2001, Citation2002; Felix et al., Citation2008), research evaluating the effects of effortful swallowing has only been conducted within healthy populations.
In this study, effortful swallowing increased UOS RT. However, previous studies investigated the effects of effortful swallowing on UOS RT and revealed differing results. Two studies reported no increase in UOS RT during effortful swallows (Bülow et al., Citation1999; Doeltgen et al., Citation2017). However, Doeltgen and colleagues (2017) posited that the lack of effects on UOS parameters may have resulted from the evaluation of effortful swallowing in young healthy adults with no history of swallowing difficulties. As such, this study highlighted the significant effects that effortful swallowing has on UOS RT in adults with dysphagia. Of note, it is important to acknowledge measurement differences of UOS RT. While UOS RT captures pressure changes, it could be argued that bolus presence time or maximum admittance, both of which rely on impedance data, maybe more accurate measures of UOS opening.
Previous research revealed that effortful swallowing significantly decreased UOS IRP when compared with non-effortful swallows (Witte et al., Citation2008). However, Witte and colleagues (Citation2008) investigated the effects of effortful swallowing in a healthy population. In contrast to this study, the researchers measured UOS IRP using one sensor located in the UOS (Witte et al., Citation2008). Using PHRM, Hoffman and colleagues (Citation2012) reported a slight increase in UOS IRP, a finding that is similar in this study. Having analysed the extent and duration of UOS relaxation during effortful swallows, it is evident that the swallow manoeuvre has the greatest impact on UOS RT. Although the swallow manoeuvre has been found to increase UOS RT, it is important to consider the impact on the extent of UOS opening. As outlined by Hoffman and colleagues (Citation2012), the effortful swallow aims to increase pharyngeal pressure and improve bolus passage. However, this can only occur through a patent UOS. Although the increase in UOS IRP was not significant, it is important to consider the impact that this may have on the extent of UOS opening in patients with dysphagia.
Limitations and future directions
Study limitations include the small sample size and heterogeneous clinical populations. In future studies, adequately powered participant groups with homogeneous clinical populations are needed to evaluate the effectiveness of the effortful swallow manoeuvre. The effects of age should be considered in future PHRM research. While this study was not adequately powered to investigate differences between oropharyngeal and oesophageal dysphagia, future research may consider exploring this. Confirmation of weak tongue base retraction or weak pharyngeal constriction during VFS or FEES within the participant group would be optimal. Participants in this study were provided with verbal instructions and a demonstration prior to completing the effortful swallow. Future studies should consider using floor-of-mouth surface electromyography (sEMG) simultaneously during PHRM examination to ensure accuracy and consistency of the swallow manoeuvre. Furthermore, the addition of impedance may have provided rich data on changes to bolus flow with effortful swallowing. Metrics such as maximum admittance and bolus presence time may have served as more appropriate metrics to capture the extent of UOS opening, compared to UOS IRP. In addition, it would be beneficial to capture oesophageal metrics to evaluate the effects of the effortful swallow on oesophageal physiology within a clinical population. Finally, duplicate 10ml fluid swallows of baseline and effortful swallowing were examined in this study. This was in an effort to limit the length of the HRM procedure for adults with dysphagia. In line with HRPM International Working Group guidelines, future studies should complete triplicate swallows of each bolus condition (Omari et al., Citation2020) and more than one bolus volume (i.e. 5ml and 10ml) should be included. In addition, completing more than one viscosity would be beneficial to determine the impact of the effortful swallow across bolus conditions (Ferris et al., Citation2021).
Conclusion
This study highlights the effects of the effortful swallow on pharyngeal pressure and UOS opening duration on thin liquids in adults with dysphagia using PHRM. Advanced understanding of the physiological effects of dysphagia interventions including the effortful swallow may inform candidacy and optimise treatment outcomes in clinical practice.
Acknowledgement
Thank you to members of the speech and language therapy department in Tallaght University Hospital where data collection took place.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Aoyagi, Y., Ohashi, M., Ando, S., Inamoto, Y., Aihara, K., Matsuura, Y., … Saitoh, E. (2021). Effect of tongue-hold swallow on pharyngeal contractile properties in healthy individuals. Dysphagia, 1–8. doi:https://doi.org/10.1007/s00455-020-10217-9
- Bahia, M.M., & Lowell, S.Y. (2020). A systematic review of the physiological effects of the effortful swallow maneuver in adults with normal and disordered swallowing. American Journal of Speech-Language Pathology, 29, 1655–1673. doi:https://doi.org/10.1044/2020_AJSLP-19-00132
- Bredenoord, A.J., & Hebbard, G.S. (2012). Technical aspects of clinical high-resolution manometry studies. Neurogastroenterology & Motility, 24 Suppl 1, 5–10. doi:https://doi.org/10.1111/j.1365-2982.2011.01830.x
- Bülow, M., Olsson, R., & Ekberg, O. (1999). Videomanometric analysis of supraglottic swallow, effortful swallow, and chin tuck in healthy volunteers. Dysphagia, 14, 67–72. doi:https://doi.org/10.1007/PL00009589
- Bülow, M., Olsson, R., & Ekberg, O. (2001). Videomanometric analysis of supraglottic swallow, effortful swallow, and chin tuck in patients with pharyngeal dysfunction. Dysphagia, 16, 190–195. doi:https://doi.org/10.1007/s00455-001-0065-9
- Bülow, M., Olsson, R., & Ekberg, O. (2002). Supraglottic swallow, effortful swallow, and chin tuck did not alter hypopharyngeal intrabolus pressure in patients with pharyngeal dysfunction. Dysphagia, 17, 197–201. doi:https://doi.org/10.1007/s00455-002-0050-y
- Carnaby, G.D., & Harenberg, L. (2013). What is “usual care” in dysphagia rehabilitation: A survey of USA dysphagia practice patterns. Dysphagia, 28, 567–574. doi:https://doi.org/10.1007/s00455-013-9467-8
- Crary, M.A., Mann, G.D.C., & Groher, M.E. (2005). Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Archives of Physical Medicine and Rehabilitation, 86, 1516–1520. doi:https://doi.org/10.1016/j.apmr.2004.11.049
- Doeltgen, S.H., Ong, E., Scholten, I., Cock, C., & Omari, T. (2017). Biomechanical quantification of mendelsohn maneuver and effortful swallowing on pharyngoesophageal function. Otolaryngology–Head and Neck Surgery, 157, 816–823. doi:https://doi.org/10.1177/0194599817708173
- Easterling, C. (2017). 25 Years of dysphagia rehabilitation: What have we done, what are we doing, and where are we going? Dysphagia, 32, 50–54. doi:https://doi.org/10.1007/s00455-016-9769-8
- Felix, V.N., Corrêa, S.M.A., & Soares, R.J. (2008). A therapeutic maneuver for oropharyngeal dysphagia in patients with Parkinson’s disease. Clinics, 63, 661–666. doi:https://doi.org/10.1590/S1807-59322008000500015
- Ferris, L., Doeltgen, S., Cock, C., Rommel, N., Schar, M., Carrión, S., … Omari, T. (2021). Modulation of pharyngeal swallowing by bolus volume and viscosity. American Journal of Physiology-Gastrointestinal and Liver Physiology, 320, G43–G53. doi:https://doi.org/10.1152/ajpgi.00270.2020
- Guiu Hernandez, E., Gozdzikowska, K., Apperley, O., & Huckabee, M.L. (2018). Effect of topical nasal anesthetic on swallowing in healthy adults: A double-blind, high-resolution manometry study. Laryngoscope, 128, 1335–1339. doi:https://doi.org/10.1002/lary.26996
- Hind, J.A., Nicosia, M.A., Roecker, E.B., Carnes, M.L., & Robbins, J. (2001). Comparison of effortful and noneffortful swallows in healthy middle-aged and older adults. Archives of Physical Medicine and Rehabilitation, 82, 1661–1665. doi:https://doi.org/10.1053/apmr.2001.28006
- Hoffman, M.R., Mielens, J.D., Ciucci, M.R., Jones, C.A., Jiang, J.J., & McCulloch, T.M. (2012). High-resolution manometry of pharyngeal swallow pressure events associated with effortful swallow and the Mendelsohn maneuver. Dysphagia, 27, 418–426. doi:https://doi.org/10.1007/s00455-011-9385-6
- Huckabee, M.-L., Butler, S.G., Barclay, M., & Jit, S. (2005). Submental surface electromyographic measurement and pharyngeal pressures during normal and effortful swallowing. Archives of Physical Medicine and Rehabilitation, 86, 2144–2149. doi:https://doi.org/10.1016/j.apmr.2005.05.005
- Kendall, K.A., & Leonard, R.J. (2002). Videofluoroscopic upper esophageal sphincter function in elderly dysphagic patients. Laryngoscope, 112, 332–337. doi:https://doi.org/10.1097/00005537-200202000-00024
- Knigge, M.A., Thibeault, S., & McCulloch, T.M. (2014). Implementation of high-resolution manometry in the clinical practice of speech language pathology. Dysphagia, 29, 2–16. doi:https://doi.org/10.1007/s00455-013-9494-5
- Langmore, S.E., & Pisegna, J.M. (2015). Efficacy of exercises to rehabilitate dysphagia: A critique of the literature. International Journal of Speech-Language Pathology, 17, 222–229. doi:https://doi.org/10.3109/17549507.2015.1024171
- Lever, T.E., Cox, K.T., Holbert, D., Shahrier, M., Hough, M., & Kelley-Salamon, K. (2007). The effect of an effortful swallow on the normal adult esophagus. Dysphagia, 22, 312–325. doi:https://doi.org/10.1007/s00455-007-9107-2
- Logemann, J.A. (2008). Treatment of oral and pharyngeal dysphagia. Physical Medicine and Rehabilitation Clinics of North America, 19, 803–816. doi:https://doi.org/10.1016/j.pmr.2008.06.003
- Omari, T.I., Ciucci, M., Gozdzikowska, K., Hernández, E., Hutcheson, K., Jones, C., … O’Rourke, A. (2020). High-resolution pharyngeal manometry and impedance: Protocols and metrics-recommendations of a high-resolution pharyngeal manometry international working group . Dysphagia, 35, 281–295. doi:https://doi.org/10.1007/s00455-019-10023-y
- Omari, T.I., Savilampi, J., Kokkinn, K., Schar, M., Lamvik, K., Doeltgen, S., & Cock, C. (2016). The reliability of pharyngeal high resolution manometry with impedance for derivation of measures of swallowing function in healthy volunteers. International Journal of Otolaryngology, 2016, 2718482–2718488. doi:https://doi.org/10.1155/2016/2718482
- O’Rourke, A., Humphries, K., Lazar, A., & Martin‐Harris, B. (2017). The pharyngeal contractile integral is a useful indicator of pharyngeal swallowing impairment. Neurogastroenterology & Motility, 29, e13144. doi:https://doi.org/10.1111/nmo.13144
- O’Rourke, A., Morgan, L.B., Coss-Adame, E., Morrison, M., Weinberger, P., & Postma, G. (2014). The effect of voluntary pharyngeal swallowing maneuvers on esophageal swallowing physiology. Dysphagia, 29, 262–268. doi:https://doi.org/10.1007/s00455-013-9505-6
- Regan, J. (2020). Impact of sensory stimulation on pharyngo-esophageal swallowing biomechanics in adults with dysphagia: A high-resolution manometry study. Dysphagia, 35, 825–833. doi:https://doi.org/10.1007/s00455-019-10088-9
- Rogus-Pulia, N.M., Jones, C.A., Forgues, A.L., Orne, J., Macdonald, C.L., Connor, N.P., & McCulloch, T.M. (2020). Perceived professional and institutional factors influencing clinical adoption of pharyngeal high-resolution manometry. American Journal of Speech-Language Pathology, 29, 1550–1562. doi:https://doi.org/10.1044/2020_AJSLP-19-00134
- Rumbach, A., Coombes, C., & Doeltgen, S. (2018). A survey of Australian dysphagia practice patterns. Dysphagia, 33, 216–226. doi:https://doi.org/10.1007/s00455-017-9849-4
- Singendonk, M., Cock, C., Bieckmann, L., Szczesniak, M., Ferris, L., Benninga, M., & Omari, T. (2019). Reliability of an online analysis platform for pharyngeal high-resolution impedance manometry recordings. Speech, Language and Hearing, 22, 195–203. doi:https://doi.org/10.1080/2050571X.2018.1535564
- Takasaki, K., Umeki, H., Hara, M., Kumagami, H., & Takahashi, H. (2011). Influence of effortful swallow on pharyngeal pressure: evaluation using a high-resolution manometry. Otolaryngology–Head and Neck Surgery, 144, 16–20. doi:https://doi.org/10.1177/0194599810390885
- Winiker, K., Gillman, A., Hernandez, E.G., Huckabee, M.-L., & Gozdzikowska, K. (2019). A systematic review of current methodology of high-resolution pharyngeal manometry with and without impedance. European Archives of Oto-Rhino-Laryngology, 276, 631–645. doi:https://doi.org/10.1007/s00405-018-5240-9
- Witte, U., Huckabee, M.-L., Doeltgen, S.H., Gumbley, F., & Robb, M. (2008). The effect of effortful swallow on pharyngeal manometric measurements during saliva and water swallowing in healthy participants. Archives of Physical Medicine and Rehabilitation, 89, 822–828. doi:https://doi.org/10.1016/j.apmr.2007.08.167