Abstract
Soft tissue defects around the ankle are common and must be covered with thin and pliable flaps. A regional flap, particularly from the dorsum of the foot was considered ideal. A neurocutaneous flap, based on the superficial peroneal nerve (SPN) and its branches was designed as a proximally based flap via cadaveric dissection. This study aimed to demonstrate the vascularity and characteristics of the superficial peroneal neurocutaneous (SPNC) flap. The SPNC flap was created in 11 lower limbs (seven cadavers) using a proximally based design. The skin flap was dissected at the dorsum of the foot, followed by injection of diluted methylene blue through the anterior tibial artery, to visualize the vascularity. The flap pedicle above the anterior ankle joint line was dissected along the SPN for anatomical study of perforating branches, paraneural vessels, and flap territory. The mean distances of the most proximal perforating branches were 1.51 ± 1.48 cm from the anterior ankle joint line, and 5.12 ± 1.78 cm from the lateral malleolus. The mean distances of the most distal perforating branches were 2.75 ± 1.54 cm from the anterior ankle joint line, and 5.90 ± 1.81 cm from the lateral malleolus. The mean number of perforating branches was 3.73 ± 1.49. The mean flap territories were 5.51 ± 0.59 cm in length, and 7.15 ± 0.64 cm in width. The SPNC flap is an alternative method for soft tissue reconstruction around the ankle with a proximally based flap design. The antegrade flow has been shown to offer effective vascularity in flaps prepared via cadaveric dissection.
Introduction
Skin and soft tissue defects around the ankle are common challenges in orthopedic surgery. Often, these defects involve exposure of vital structures, such as arteries, nerves, tendons, and bones, that require flap coverage. Although many useful local flaps have been described in this region, they present some limitations. For example, the dorsalis pedis-artery pedicle flap requires the sacrifice of the dorsalis pedis artery, which is an important vessel of the foot [Citation1,Citation2]. Similarly, other neurocutaneous flaps, such as the reversed sural flap or saphenous flap, have been used for lower limb reconstruction; however, they are not always suitable because injury near the ankle might have damaged the perforating vessels that supply these flaps. Moreover, the bulky flap contour results in limited function and aesthetic when wearing shoes. Likewise, free flaps provide excellent tissue coverage; however, they also require an experienced microsurgery team.
Masquelet et al. introduced a neurocutaneous island flap, supplied by the vascular axis of the sensitive superficial nerve of the leg [Citation3]. The concept of a neurocutaneous flap was developed based on the advantage of the paraneural vessels of the superficial cutaneous nerves called vasa nervorum, in supplying the overlying skin [Citation3–6]. Subsequently, several flaps have been reported to be popularly used in the lower extremities [Citation4,Citation7–10]. The vascular anatomy of all dorsal pedal cutaneous nerves has been studied, and a variety of neurocutaneous flap applications in the dorsum of the foot have been reported with favorable results in forefoot defect coverage and thin flap design [Citation11–13].
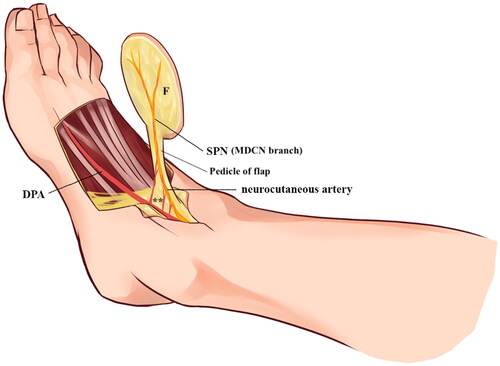
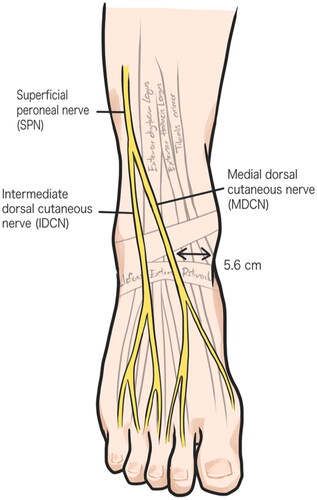
The superficial peroneal nerve (SPN) and its branches, the medial dorsal cutaneous nerve (MDCN), and intermediate dorsal cutaneous nerve (IDCN), supply a major portion of the dorsum of the foot, except for those regions supplied by the deep peroneal nerve (DPN) and sural nerve (SN). The MDCN is larger in size and less variable than the others () [Citation14–17]. This study involves the neurocutaneous flap that depends on SPN and MDCN, called the superficial peroneal neurocutaneous (SPNC) flap, that receives the most reliable blood supply from perforating branches of the dorsalis pedis artery, primarily supplying the dorsum of the foot.
Figure 1. Illustration of superficial peroneal nerve anatomy and its branches, medial dorsal cutaneous and intermediate dorsal cutaneous nerves.
A proximally based or antegrade arterial flow flap design is an alternative flap coverage for soft tissue defects around the malleolar zone. This technique has the advantages of a thin subcutaneous flap and a rotatable design, thus permitting access to the defect area. The objective of this study was to demonstrate the versatility of the SPNC flap in terms of antegrade flow and vascular supply characteristics.
Methods
Fourteen lower limbs from seven soft cadavers, aged 18–85 years were enrolled in this anatomical study. Cadavers with a history of peripheral vascular disease, peripheral nerve neuritis, skin cancer, scarring, or anatomical distortion around the ankle or foot were excluded. This study was conducted at the Faculty of Medicine, Ramathibodi Hospital, from October 2020 to April 2021.
The number and location of the perforating branches that supplied the flap, its territories, the ankle and foot circumference, and foot length were measured. Ankle circumference was measured at the tip of the medial and lateral malleolus, while foot circumference was measured at the tarsometatarsal joint area; foot length was measured from the heel to the tip of the great toe on the plantar side. Statistical analyses were performed, and the results were expressed as mean and standard deviation. This study was approved by the ethics committee of the Ramathibodi Hospital.
Cadaveric dissection
After the cadaver subject was prepared, the course of the SPN was drawn based on the anatomical pathway of this nerve, that passed anteroinferior between the peroneus longus and brevis, and the extensor digitorum longus muscles, before piercing the deep fascia in the distal third of the leg, and dividing into the MDCN and IDCN branches. The MDCN was located approximately half the distance from the medial malleolus to the lateral malleolus [Citation17–19]. The axis of the flap was designed along the trajectory of SPN and MDCN. Subsequently, the skin paddle flap was outlined proximally by the midtarsal joint, and distally at the mid-length of the metatarsal bone. The lateral and medial margins were drawn at the most lateral and medial aspects of the dorsum of the foot. The 3 cm-wide flap pedicle, was outlined continuing from the proximal end of the skin flap, over the MDCN trajectory, to the anterior ankle joint line, thus ensuring the inclusion of paraneural vessels and superficial vein. The longitudinal skin incision was extended proximally to the ankle joint and distally to the first web space area. Before flap dissection, the SPN, MDCN, and anterior tibial artery (ATA) were identified proximal to the inferior extensor retinaculum, while the deep plantar artery was identified distal to the skin flap (). The catheter was inserted into the ATA and the deep plantar artery was cut and ligated at the distal site. Blood clots in the vessels of ATA, the dorsalis pedis artery, and its perforators along the dorsum of the foot were removed by irrigation with 200 ml of warm normal saline solution (60 °C) via the ATA until leakage of normal saline was observed at the deep plantar artery [Citation20,Citation21]. To verify that the neurocutaneous artery could provide vascularity to the flap in antegrade flow, the proximally based pedicle flap was created before injecting methylene blue. The proximally based antegrade-flow SPNC flap was dissected based on the SPN and MDCN trajectory, using a surgical loupe with 2.5× magnification. While the incision was made starting at the distal end of the flap and followed along the medial and lateral borders, the MDCN and superficial vein were cut and ligated to be included in the flap. Due to the variation of the cutaneous nerve of the foot, the cutaneous branch of deep peroneal nerve also including in this flap. The dissection of the flap over the extensor hallucis longus and extensor digitorum longus tendons preserved the paratenon. The pedicle was subdermally dissected at the anterior ankle joint line, along the trajectory of the MDCN, with a 3 cm-wide flap axis. The flap and pedicle were elevated, along with the fascia, MDCN, and superficial vein.
Figure 2. Illustration of SPNC flap designed and drawing. Skin flap was designed over the dorsalis pedis artery and the pedicle of flap was designed along the MDCN trajectory with 3 cm width (dotted line).
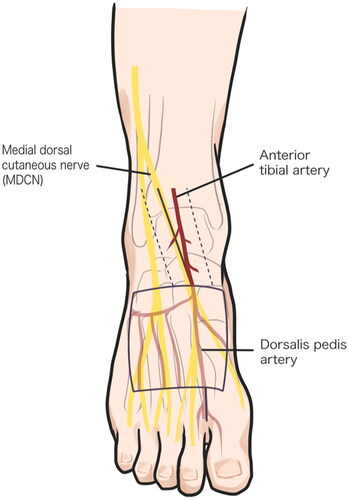
A warm diluted methylene blue solution (60 °C) was injected into the ATA until leakage was observed at the edge of the flap, to ensure that the paraneural vessel could vascularize the skin flap. Besides, the pedicle of the flap was dissected to identify the color-stained perforating branches of the dorsalis pedis artery (nutrient arteries), paraneural vessels, and their anastomosis. The location and number of perforating branches were recorded (). The distances from the anterior ankle joint line and lateral malleolus to the most distal and proximal perforating branches were measured using a Vernier caliper and measuring tape. The MDCN was explored underneath the flap to identify the paraneural vessels that run along the nerve and provide neurocutaneous perforators to the subcutaneous plexus (). The flap territory, defined by the boundary of methylene blue staining, was measured by width and length.
Figure 3. lateral side view of right foot shows colorized perforating branches of the dorsalis pedis artery under the pedicle of the flap (white asterisk). SPN, superficial peroneal nerve; P, pedicle of flap.
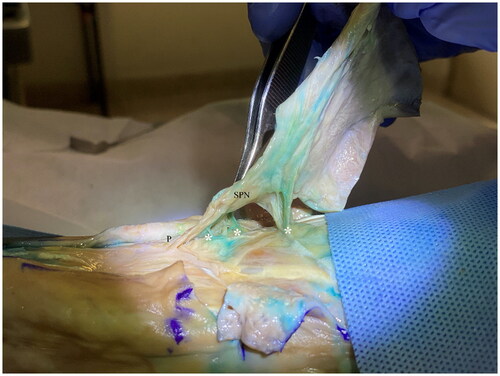
Figure 4. Exploration of superficial peroneal nerve underneath the flap shows the staining of paraneural vessels (asterisk) along the nerve and the neurocutaneous perforator (arrow) linking paraneural vessels and subcutaneous plexus.

After completion of flap dissection, the SPNC flap was raised as a pedicle flap that could be rotated and covered either the medial malleolus, lateral malleolus, or distal one-third of the leg ().
Results
Eleven lower limbs from seven soft cadavers were studied (three males and four females); three lower limbs were excluded due to abnormal anatomy (old wound scar over the dorsum of the foot). Seven and four lower limbs were from the left and right sides, respectively. The mean age of cadavers was 69.3 years. The baseline characteristics of cadavers were foot length of 20.5–26.0 cm (mean = 23.89 ± 1.74), foot circumference of 18.4–25.5 cm (mean = 23.19 ± 2.03), and ankle circumference of 21.5–26.4 cm (mean = 23.71 ± 1.77) ().
Table 1. cadaveric study results.
This study showed that the trajectory of the SPN was located subcutaneously, immediately anterior to the distal third of the leg, and the MDCN was located approximately half the distance from the medial to the lateral malleolus. The most proximal and distal perforating branches were −0.5–5.3 cm (mean = 1.51 ± 1.48) and 1.1–6.2 cm (mean = 2.75 ± 1.54) from anterior ankle joint line, and 0.2–7.1 cm (mean = 5.12 ± 1.78) and 1.4–8.6 cm (mean = 5.90 ± 1.81) from lateral malleolus, respectively. It implies that the pivot point of this flap would be not beyond 1.5 cm distal to the anterior ankle joint line and 5 cm from the lateral malleolus. The number of perforating branches along the pedicle ranged from one to six branches (mean = 3.73 ± 1.49). The flap territories were 4.5–6.4 cm (mean = 5.51 ± 0.62) in length, and 6.0–8.4 cm (mean = 7.22 ± 0.62) in width (). The ratio of the flap to foot length, and flap width to foot circumference were approximately 1:4 and 1:3, respectively. All flaps were elevated with a pedicle width of 3 cm.
Discussion
The neurocutaneous flaps have been used for several decades, and they remain beneficial for both upper- and lower-extremity defect coverage. The vascularity of the neurocutaneous flap based on the SPN, MDCN, and LDCN of the foot was studied in the lower extremities; MDCN has been exclusively studied for its rich nutrient artery network [Citation11,Citation12]. However, the visually assessed certainty of the vascular supply to the flap via antegrade flow, the flap territory, and the pivot point have never been investigated during cadaveric dissection.
The SPNC flap described in this study may resemble the reported dorsalis pedis perforator flap [Citation22]. Although the location of the perforators and the course of the vascular axis are quite similar, their concepts may differ. The perforating branches of the dorsalis pedis artery or dorsal metatarsal artery supply both flaps. However, the dorsalis pedis perforator flap receives blood supply from septocutaneous perforators, while the SPNC flap follows the cutaneous nerve that receives blood supply from the perforator system, which links the vascular plexus between the subcutaneous and paraneural vessels.
To ensure that the vascularity of the flap was provided by the paraneural vessels, and the subcutaneous layer was nourished by neurocutaneous perforators that received blood supply from the perforating branches of the dorsalis pedis artery, the proximally based SPNC flap was harvested before methylene blue injection. The deep fascia was included while the paratenon was left intact during flap dissection. The advantage of deep fascia inclusion is that it helps to protect the neurovascular axis while facilitating dissection [Citation3]. The procedure correlates with that used in our previous study, performed on the upper extremities [Citation23]. In this study, while numerous proximally perforating branches of the dorsalis pedis artery were found 1 cm distal to the anterior ankle joint line, the average distance was calculated as 1.51 cm along the same direction. In addition, to increase the mobility of the flap, the extensor retinaculum was proximally dissected to identify the perforating branches of the anterior tibialis vessel to create the proximal pivot point and long pedicle to cover the lower leg area. These perforator findings are consistent with a previous study that reported branching, at approximately 4 cm proximal to the intermalleolar line [Citation11,Citation24]. However, in this study, we focused on the proximal perforating branch of the dorsalis pedis artery, to avoid injury to the extensor retinaculum. Usually, if the donor site defect is unable to primary closure, it would be cover by split thickness skin graft.
The advantages of the SPNC flap are as follows: (1) The flap has less subcutaneous fat, which provides the ideal thinness for soft tissue reconstruction, particularly around the ankle area and distal one-third of the leg that requires less bulky tissue; (2) The SPNC flap depends on the neurocutaneous artery and its anastomosis; therefore, the major vessels of the foot are preserved compared to the dorsalis pedis flap which is sacrificed the main vascular axis; (3) The flap has a cutaneous nerve, which preserves sensation and thus, could be a sensate flap; (4) The SPNC flap designed with the pedicle along neurocutaneous axis that provide more distance and mobility for cover the defect than the perforator flap which is rotate around perforator itself like a propeller flap.
There are some limitations to this study; the results of this cadaveric study of SPNC flap may have further obstacles to its clinical translation. Furthermore, the anatomy of the cutaneous nerves of the foot dorsum is highly variable [Citation14–17]. The cutaneous nerves, MDCN, LDCN, the cutaneous branch of the deep peroneal nerve, or all the above may be incorporated into the flap; thus, impairment of sensation due to cutaneous nerve sacrifice is to be considered.
Conclusion
The SPNC flap with a proximally based design is an alternative for soft tissue coverage around the malleolar area. This cadaveric study verified that antegrade flow via the neurocutaneous artery could offer sufficient vascularity to the SPNC flap. In addition, the SPNC flap is a sensate flap that preserves major blood vessels.
Author contributions
Thepparat Kanchanathepsak, M.D. (Conceptualization, Study design, Investigation, Manuscript writing & editing).
Katanyata Kunsook, M.D. (Investigation, Data collection, Data analysis, Manuscript writing).
Wasit Panoinont, M.D. (Research assistant, Investigation, Manuscript review).
Chinnawut Suriyonplengsaeng, M.D., Sorasak Suppaphol, M.D., Ittirat Watcharananan, M.D. and Panithan Tuntiyatorn, M.D. (Supervision, Manuscript review & editing).
Tulyapruek Tawonsawatruk, M.D., Ph.D. (Data analysis, Methodology, Manuscript review & editing).
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Krag C, Riegels-Nielsen P. The dorsalis pedis flap for lower leg reconstruction. Acta Orthop Scand. 1982;53(3):487–493.
- McCraw JB, Furlow LT. The dorsalis pedis arterialized flap. A clinical study. Plast Reconstr Surg. 1975;55(2):177–185.
- Masquelet AC, Romana MC, Wolf G. Skin island flaps supplied by the vascular axis of the sensitive superficial nerves: anatomic study and clinical experience in the leg. Plast Reconstr Surg. 1992;89(6):1115–1121.
- Nakajima H, Imanishi N, Fukuzumi S, et al. Accompanying arteries of the cutaneous veins and cutaneous nerves in the extremities: anatomical study and a concept of the venoadipofascial and/or neuroadipofascial pedicled fasciocutaneous flap. Plast Reconstr Surg. 1998;102(3):779–791.
- Bertelli JA, Khoury Z. Neurocutaneous island flaps in the hand: anatomical basis and preliminary results. Br J Plast Surg. 1992;45(8):586–590.
- Bertelli JA. Neurocutaneous axial island flaps in the forearm: anatomical, experimental and preliminary clinical results. Br J Plast Surg. 1993;46(6):489–496.
- Zhong W, Lu S, Chai Y. Distally based saphenous neurocutaneous perforator flap: a versatile donor site for reconstruction of soft tissue defects of the medial malleolar region. J Foot Ankle Surg. 2016;55(2):391–396.
- Vergara-Amador E. Distally-based superficial sural neurocutaneous flap for reconstruction of the ankle and foot in children. J Plast Reconstr Aesthet Surg. 2009;62(8):1087–1093.
- Mak KH. Distally based sural neurocutaneous flaps for ankle and heel ulcers. Hong Kong Med J. 2001;7(3):291–295.
- Goil P, Choudhary GM, Jain R, et al. Versatile distally based neurocutaneous saphenous flap in the era of microsurgery. Eur J Plastic Surg. 2018;41(2):165–172.
- Xu Y-Q, Zhu Y-L, Wu N-X, et al. Distal foot coverage with reverse dorsal pedal neurocutaneous flaps. J Plast Reconstr Aesthet Surg. 2010;63(1):164–169.
- Hu D, Hong X, Wei X, et al. Anatomical basis and clinical application of the first metatarsal proximal perforator‐based neurocutaneous vascular flap. Clin Anat. 2020;33(5):653–660.
- Huang L, Pafitanis G, Song D, et al. Anatomical basis of the intermediate dorsal pedal neurocutaneous perforator pedicled propeller flap: a cadaveric dissection. Clin Anat. 2018;31(7):1077–1084.
- Solomon L, Ferris L, Tedman R, et al. Surgical anatomy of the sural and superficial fibular nerves with an emphasis on the approach to the lateral malleolus. J Anat. 2001;199(Pt 6):717–723.
- Nayak VS, Bhat N, Nayak SS, et al. Anatomical variations in the cutaneous innervation on the dorsum of the foot. Anat Cell Biol. 2019;52(1):34–37.
- Kg RM, Sn S, Koshy S, et al. Clinically important anatomical variation of cutaneous branches of superficial peroneal nerve in the foot. The Open Anatomy J. 2010;2(1):1–4.
- Blair JM, Botte MJ. Surgical anatomy of the superficial peroneal nerve in the ankle and foot. Clin Orthop Relat Res. 1994;(305):229–238.
- Canella C, Demondion X, Guillin R, et al. Anatomic study of the superficial peroneal nerve using sonography. AJR Am J Roentgenol. 2009;193(1):174–179.
- Apaydin N, Bozkurt M. Chapter 10 – surgical exposures for nerves of the lower limb. In: Tubbs RS, Rizk E, Shoja MM, Loukas M, Barbaro N, Spinner RJ, editors. Nerves and nerve injuries. San Diego: Academic Press; 2015. p. 139–153.
- Heymans OY, Nélissen XP, Peters S, et al. New approach to vascular injection in fresh cadaver dissection. J Reconstr Microsurg. 2004;20(4):311–315.
- Doomernik DE, Kruse RR, Reijnen MM, et al. A comparative study of vascular injection fluids in fresh-frozen and embalmed human cadaver forearms. J Anat. 2016;229(4):582–590.
- Zheng H-P, Xu Y-Q, Lin J, et al. Dorsal pedis perforator flap. In: Zheng H-P, Lin J, Xu Y-Q, Hu D-Q, editors. Atlas of perforator flap and wound healing: microsurgical reconstruction and cases. Singapore: Springer Singapore; 2019. p. 391–403.
- Kanchanathepsak T, Rojpitipongsakorn C, Tawonsawatruk T, et al. The lateral antebrachial neurocutaneous flap: a cadaveric study and clinical applications. J Reconstruct Microsurg. 2020;36(7):541–548.
- Low OW, Sebastin SJ, Cheah AEJ. A review of pedicled perforator flaps for reconstruction of the soft tissue defects of the leg and foot. Ind J Plast Surg. 2019;52(1):26–36.