ABSTRACT
Background: High prevalence of sleep disturbance, which is associated with poor mental health, has been observed among non-treatment seeking refugees. However, no longitudinal research has investigated the chronicity of untreated sleep disturbance and its impact on refugees’ mental health.
Objective: This longitudinal study investigated associations between mental health (posttraumatic stress disorder, anxiety, depression), sleep symptoms (insomnia severity, pre-sleep arousal), and factors predicting mental health, over a 12-month period.
Method: Syrian refugees (N = 69) from a cross-sectional study (Time 1) participated in the current 12-month (Time 2) follow-up study. Participants completed a series of questionnaires examining sleep, trauma exposure, post-migration living difficulties, and mental health at both time points.
Results: When compared to Time 1, participants showed a significant increase in post-migration stress at Time 2. However, there was an improvement in their mental health and levels of sleep disturbance. Half of the participants met criteria for moderate (36%) or severe sleep disturbance (15%) at Time 2. Forty-two per cent of the participants had moderate to severe sleep disturbance at both Time 1 and Time 2. When predicting mental health at 12-month follow-up, only pre-sleep arousal at Time 1 uniquely predicted mental health at Time 2. Mediation analysis indicated that change in pre-sleep arousal (from Time 1 to Time 2) significantly mediated the relationship between change in post-migration stress and change in mental health symptoms.
Conclusions: This study demonstrated that sleep symptoms have an indirect and long-term impact on mental health among refugees. Understanding modifiable factors, such as sleep, mediating the relationship between trauma exposure and PTSD symptoms is important, as such factors can be targeted in psychological interventions for refugees.
HIGHLIGHTS:
• 42% of refugees residing in a high-income country continued to report insomnia at 12-months follow-up. • Pre-sleep arousal was a unique predictor of long-term PTSD, anxiety, and depression symptoms. • Sleep mediated the relationship between post-migration stress and mental health.
Antecedentes: Se ha observado en refugiados que no están en búsqueda de tratamiento una alta prevalencia de alteraciones del sueño, que se asocia con una salud mental pobre. Sin embargo, no existen estudios longitudinales que hayan investigado la cronicidad de las alteraciones del sueño no tratadas y su impacto en la salud mental de los refugiados.
Objetivo: Este estudio longitudinal investigó las asociaciones entre salud mental (trastorno de estrés postraumático, ansiedad, depresión), síntomas del sueño (severidad del insomnio, activación previa al sueño), y factores predictores de salud mental, a lo largo de un periodo de 12 meses.
Método: Refugiados sirios (N=69) de un estudio transversal (Momento 1) participó en el siguiente seguimiento a los 12 meses (Momento 2). Los participantes completaron una serie de cuestionarios examinando el sueño, la exposición al trauma, las dificultades vitales luego de la migración y la salud mental en ambos momentos de medición.
Resultados: En comparación al Momento 1, los participantes mostraron un aumento 2significativo del estrés posterior a la migración en el Momento 2. Sin embargo, hubo una mejora en su salud mental y los niveles de alteración del sueño. La mitad de los participantes cumplieron los criterios para alteraciones del sueño moderadas (36%) o severas (15%) al Momento 2. Cuarenta y dos por ciento de los participantes tuvieron alteraciones del sueño moderadas a severas en ambos Momentos 1 y 2. Al predecir la salud mental en el seguimiento a 12 meses, sólo la activación previa al sueño en el Momento 1 predijo únicamente la salud mental al Momento 2. Los análisis de mediación indicaron que el cambio en la activación previa al sueño (desde el Momento 1 al Momento 2) medió significativamente la relación entre cambio en el estrés posterior a la migración y cambio en los síntomas de salud mental.
Conclusiones: Este estudio demostró que los síntomas del sueño tienen un impacto indirecto y en el largo plazo en la salud mental de los refugiados. Es importante el entendimiento de los factores modificables, tales como el sueño, que mediaron la relación entre la exposición al trauma y los síntomas, dado que tales factores pueden ser abordados en las intervenciones psicológicas para refugiados.
背景: 在不寻求治疗的难民中, 睡眠障碍患病率很高, 这与精神健康状况不佳有关。但是, 没有纵向研究考查未经治疗的睡眠障碍的长期性及其对难民心理健康的影响。
目的: 本纵向研究考查了12个月期间心理健康 (创伤后应激障碍, 焦虑, 抑郁), 睡眠症状 (失眠严重程度, 睡前觉醒) 与心理健康预测因素之间的关系。
方法: 来自横断面研究 (时间点1) 的69名叙利亚难民参加了当前12个月 (时间点2) 的随访研究。参与者完成了考查两个时间点睡眠, 创伤暴露, 移民后生活困难和心理健康的一系列问卷。
结果: 与时间点1相比, 参与者在时间点2的移民后压力显著增加。但是, 他们的心理健康和睡眠障碍水平有所提升。一半的参与者在时间点2达到中度 (36%) 或严重睡眠障碍 (15%) 的标准。42%的参与者在时间点1和时间点2都有中度至严重的睡眠障碍。在12个月的随访中, 只有时间点1的睡前觉醒独立预测了时间点2的心理健康。中介分析表明, 睡前觉醒的变化 (从时间点1到时间点2) 显著中介了移民后压力和心理健康症状改变之间的关系。
结论: 本研究表明, 睡眠症状对难民的心理健康具有间接和长期的影响。了解睡眠等可调节因素并中介创伤暴露与PTSD症状之间的关系很重要, 因为这些因素可以作为难民心理干预措施的目标。
Syrians continue to be the world’s largest forcibly displaced population, with an estimated 11.7 million Syrians displaced and in need of humanitarian assistance (United Nations High Commissioner for Refugees [UNHCR], Citation2019). Experiences of conflict-related violence and ongoing concerns about the current situation in Syria are compounded by post-migration living difficulties in host countries, such as inadequate housing and health services, isolation and discrimination, loss of status, harsh socioeconomics, and uncertainty about the future (Hassan, Ventevogel, Jefee-Bahloul, Barkil-Oteo, & Kirmayer, Citation2016; Kaya, Kiliç, Karadağ Çaman, & Üner, Citation2019). These factors impact mental health, with prevalence rates of posttraumatic stress disorder (PTSD) being 33.5% and 27.2% in a sample of Syrians living in a refugee camp in Turkey (Alpak et al., Citation2015) and in Lebanon (Kazour et al., Citation2017), respectively. Most studies investigating the mental health of Syrian refugees, however, have been conducted in Syrian-bordering countries and are limited to cross-sectional designs. Little is known about the mental health of displaced Syrians residing in high-income countries and whether psychological disorders continue unabated or resolve over time.
The course of PTSD is complex and affected by several factors, such as the nature of precipitating events, characteristics of the trauma survivor, and nature of the recovery environment (Weine et al., Citation1998). The results of longitudinal studies in refugee mental health vary immensely. Several studies have found improvements in mental health over time, including those living in refugee camps (Mollica et al., Citation2001) and resettled in a host country (USA: Weine et al., Citation1998). In contrast, several studies have found an increase in PTSD symptoms among resettled refugees (Lie, Citation2002; Roth, Ekblad, & Agren, Citation2006), while other studies have found no change in symptoms (Australia: Cooper, Enticott, Shawyer, & Meadows, Citation2019; Germany: Kaltenbach, Schauer, Hermenau, Elbert, & Schalinski, Citation2018), even after a 7-year period (Netherlands: Lamkaddem et al., Citation2014). These seemingly contradictory results may reflect differing experiences in the home country or host country and refugee-specific characteristics. This demonstrates the need for further research investigating the relationships between individual and contextual factors and mental health outcomes over time.
Several theoretical models have been developed to better understand the factors contributing to refugee mental health (e.g. Miller & Rasmussen, Citation2010, Citation2016; Nickerson, Bryant, Silove, & Steel, Citation2011). These models acknowledge the role of pre- and post-migration stress. They also provide a comprehensive account of the integrated psychological trauma mechanisms underpinning the psychological reactions experienced by refugees in the aftermath of trauma (Miller & Rasmussen, Citation2010, Citation2016; Nickerson et al., Citation2011). However, these models do not specifically include or consider the role of sleep disturbance. The role of sleep in the psychological adjustment of refugees is essential to consider given the immense non-refugee research demonstrating the importance of sleep disturbance in perpetuating many of the mental health concerns (PTSD, anxiety, and depression) observed in refugee groups.
Sleep disturbance plays a crucial role in PTSD. Subjective sleep disturbance is highly comorbid with PTSD and is often considered a ‘hallmark’ feature of the disorder (Ross, Ball, Sullivan, & Caroff, Citation1989). In this paper, we define sleep disturbance as difficulty falling asleep, maintaining sleep, early awakening, or unrefreshing/nonrestorative sleep in an individual who has an adequate opportunity for sleep. Prospective studies have demonstrated that sleep disturbance, both prior to and following trauma, is an important predictor of the development of PTSD (Bryant, Creamer, O’Donnell, Silove, & McFarlane, Citation2010; Gehrman et al., Citation2013) and exacerbates the distress and dysfunction of those with PTSD (Belleville, Guay, & Marchand, Citation2009; Giosan et al., Citation2015). Indeed, several researchers have proposed that sleep disturbance may play a role in mediating the effect of trauma exposure on PTSD. In support of this, two studies have found sleep disturbance mediated the relationship between trauma exposure and PTSD symptoms among veterans (Picchioni et al., Citation2010) and military personnel (Steele, Germain, & Campbell, Citation2017). Sleep disturbance is also a predictor of PTSD treatment outcome and clinically addressing sleep disturbance can improve PTSD symptoms (Nappi, Drummond, & Hall, Citation2012; Walters et al., Citation2019). Wright et al. (Citation2011) longitudinally examined, among combat veterans, the relationship between sleep and PTSD symptoms. They found insomnia at 4 months post-trauma was a significant predictor of change in PTSD symptoms at 12 months post-trauma. However, there was no support for PTSD symptoms predicting insomnia, suggesting insomnia symptoms may be a driver of PTSD (Wright et al., Citation2011).
Pre-sleep arousal is strongly related to sleep disturbance and PTSD hyperarousal symptoms. Pre-sleep arousal is the heightened arousal that occurs during the sleep onset period, and it is comprised of cognitive arousal (i.e. excessive worry, rumination, ‘racing/overactive mind’) and somatic arousal (i.e. physiological responses like difficulty breathing, overall nervous or bodily tension, and rapid heart rate) (Nicassio, Mendlowitz, Fussell, & Petras, Citation1985). Pre-sleep arousal has been found to mediate the relationship between perceived daily stress and subjective sleep quality (Morin, Rodrigue, & Ivers, Citation2003; Winzeler et al., Citation2014). However, little research has investigated pre-sleep arousal as a mediating variable between daily post-migration stress experienced by refugees and mental health symptoms.
To date, little empirical work has considered the associations between trauma exposure, post-migration stress, sleep symptoms, and PTSD in refugee populations. Thus, there are several important gaps in the literature. While there are established findings from sleep literature on the relationship between sleep disturbance and major mental health conditions commonly reported in trauma-exposed populations, there are very few studies that have investigated these relationships within a refugee population. Specifically, within the field of psychotraumatology, hyperarousal is hypothesized to be a pivotal mechanism associating PTSD with sleep disturbance; (hyper)arousal is associated with sleep disturbance, which contributes to the maintenance of PTSD (Germain, Buysse, & Nofzinger, Citation2008). In the sleep field, pre-sleep arousal has been identified as one of the most significant perpetuating factors of chronic insomnia (Harvey, Citation2002), and life stress is proposed to be associated with pre-sleep arousal, which in turn is associated with sleep disturbance (Morin et al., Citation2003; Winzeler et al., Citation2014). While these advances have occurred in parallel, few empirical investigations have integrated these proposed associations. Therefore, the current study examined the associations between post-migration life stress, pre-sleep arousal/sleep disturbance, and PTSD.
Examining this relationship is of particular importance given sleep disturbance is common among refugees and associated with PTSD symptoms (Lies, Mellor, Jobson, & Drummond, Citation2019). Recently, we conducted a cross-sectional study investigating a) sleep disturbance amongst newly-arrived Syrian (n = 75) and Iraqi (n = 11) refugees living in Melbourne, Australia, b) psychosocial factors associated with greater sleep disturbance, and c) whether the relationship between trauma exposure and PTSD symptoms was mediated by post-migration stress and sleep symptoms in a sequential manner. We found that 65% of the sample had moderate to high levels of sleep disturbance, and pre-sleep arousal was the only factor predicting sleep disturbance (Lies, Jobson, Mascaro, Whyman, & Drummond, Citation2020). We also found the association between trauma exposure and PTSD symptoms was mediated by post-migration stress and sleep symptoms in a sequential order. When these two mediators were reversed, the models were no longer significant. These findings suggest that sleep symptoms may play a greater role in the clinical presentation of post-traumatic stress in refugees than is generally recognized. However, it is unclear to what extent these findings are unique to refugees recently resettled in a host country and how these findings change over time as refugees settle in the host country.
This longitudinal study aimed to conduct a follow-up (12-month) investigation of the associations between mental health, sleep disturbance, and living difficulties among the Syrian refugees in our initial study. Currently, there is no longitudinal study examining psychosocial stress, sleep, and mental health in Syrian refugees. A longitudinal follow-up study is warranted. This is because while there appears to be a high prevalence of mental health problems in the initial resettlement period among Syrian refugees (El Arnaout et al., Citation2019), over the longer-term prevalence of mental health symptoms is determined by the degree of trauma exposure and post-migration stress (Bogic, Njoku, & Priebe, Citation2015; von Haumeder, Ghafoori, & Retailleau, Citation2019). This study specifically aimed to (1) investigate the levels of post-migration stress, mental health (PTSD, anxiety, depression), and sleep symptoms in Syrian refugees at 12-month follow-up; (2) investigate which Time 1 variables predicted mental health symptoms at 12-month follow-up (Time 2); and (3) conduct exploratory analyses examining whether our cross-sectional findings (i.e. serial mediation model) were still evident when examined at 12 months.
1. Method
1.1. Participants and procedure
Syrian participants from our baseline study were invited to participate in the current study. The sample consisted of 69 (45% female) non-treatment seeking Syrian refugees living in Melbourne, Australia (92% retention from baseline study). Attrition analyses based on demographic profile and variable measures indicated no significant differences between those who remained in the study and those who did not (n = 7). Mean age of participants was 45.6 years old (SD = 15.9) and the average period of settlement in Australia was 29.7 months (SD = 6.4 months, range 18–53 months). The majority of participants were married (66.7%; 24.6% single; 8.7% widowed) and had completed at least secondary education (25% completed primary school; 47.50% completed secondary education; 27.5% completed tertiary education). Participants were representative of the larger report presented at the Public Seminar on Responses to Syrian-Conflict Refugee Settlement in Australia, Canada, Finland, Germany, New Zealand, Sweden, and the UK (Collins, Reid, Groutsis, Watson, & Ozkul, Citation2018) in terms of gender, age, marital status, and education distribution. demonstrates there were no significant differences in the proportion of health concerns, medication intake, and counselling uptake between Times 1 and 2, but there was a significant increase in those in employment at Time 2.
Table 1. Demographic profiles between two time points
To determine our target sample size, we examined the effect sizes observed in similar refugee (Steel, Silove, Bird, McGorry, & Mohan, Citation1999) and sleep studies (Steele et al., Citation2017), and adopted a conservative medium effect size (f2 =.15). With an alpha of .05 and power of 80%, the required sample to address Aims 1 and 2, for a linear multiple regression with two predictors, was 68 participants. Additionally, when we consulted guidelines for determining sample size for mediation of longitudinal data (Pan, Liu, Miao, & Yuan, Citation2018), we found that a similar number of participants were required. In order to address Aim 3 (3 predictors), we found that a total sample size of 77 was needed. Thus, the current sample appeared underpowered for Aim 3. Nevertheless, we decided to retain Aim 3, as we wanted to test the stability of model presented in our earlier cross-sectional study by conducting the serial mediation analyses with Time 2 data.
1.2. Measures
All measures used in the current study were identical to that used in the baseline study. A standard double-blind translation and back-translation procedure, in accordance with gold-standard translation practices (Bontempo, Citation1993), was used to develop Arabic versions of the questionnaires, unless adapted Arabic versions of questionnaires already existed.
1.2.1. Sleep diary
Based on the consensus sleep diary (Carney et al., Citation2012), our diary included subjective measures of bedtime, sleep latency, number, and duration of awakenings, wake time, time in bed after final awakening, and daytime naps; and calculated variables of total sleep time (TST) and sleep efficiency (SE). SE was calculated as the ratio of total time asleep to time in bed; ≥85% is generally considered ‘normal’ SE (Reed & Sacco, Citation2016).
1.2.2. Insomnia severity index (ISI)
ISI consists of 7-item scales used to assess the nature, severity, and impact of insomnia over a 1-week time interval (Morin, Citation1993). Total possible scores range from 0 to 28; a higher score indicating greater insomnia severity. A cut-off point of ISI≥10 is commonly used in community samples (Morin, Belleville, Bélanger, & Ivers, Citation2011). The ISI evidenced good internal consistency (α = .87) in the current study.
1.2.3. Pre-sleep arousal scale (PSAS)
PSAS is a 16-item self-report measuring cognitive and somatic arousal occurring during the pre-sleep period that can interfere with a person’s ability to initiate or maintain sleep (Nicassio et al., Citation1985). Items are rated on a 5-point scales; higher scores indicate increased arousal before falling asleep (Nicassio et al., Citation1985). Suggested cut-off scores for cognitive arousal are ≥20 and somatic arousal is ≥14 (Puzino, Amatrudo, Sullivan, Vgontzas, & Fernandez-Mendoza, Citation2019). In this study, the scale demonstrated strong internal consistency (α = .92).
1.2.4. Harvard trauma questionnaire (HTQ)
HTQ was developed specifically for trauma-affected refugees. This study used the trauma event section of the Iraqi (Arabic) version of the HTQ (Shoeb, Weinstein, & Mollica, Citation2007). Individuals responded ‘yes’ or ‘no’ to 40-items, indicating whether they had experienced the events directly. Total trauma exposure scores were calculated by a count of ‘yes’ responses. The measure evidenced good internal consistency (α = .86) in this study.
1.2.5. Post-migration living difficulties questionnaire (PMLD)
PMLD is a 23-item checklist assessing levels of stress due to post-migration stressors (Silove, Sinnerbrink, Field, Manicavasagar, & Steel, Citation1997). The PMLD consists of three domains: protection concerns, access to health and welfare, and stress related to resettlement. Participants rated the extent to which they considered each post-migration challenge to be a problem; only items rated ‘moderately serious problem’ and ‘very serious problem’ were considered positive. PMLD scores were calculated by summing living difficulties considered a problem. In this study, the PMLD showed excellent internal consistency (α = .95).
1.2.6. Short posttraumatic stress disorder inventory (PTSD-8)
PTSD-8 is an 8-item screening questionnaire for PTSD (Hansen et al., Citation2010). It covers the three symptom clusters of the DSM-IV PTSD (four intrusion items, two avoidance items, two hypervigilance items), but excludes the diagnostically non-specific items (e.g. sleeping difficulty, difficulty concentrating). The PTSD-8 has been used in several large-scale refugee studies (Bryant et al., Citation2018; Nickerson et al., Citation2019). Items are scored on 4-point Likert scales and are summed to provide a symptom severity score. A cut-off point of 18 is indicative of probable PTSD (Hansen et al., Citation2010). In this study, the scale demonstrated sound internal consistency (α = .91).
1.3. Hopkins symptoms checklist (HSCL-25)
HSCL-25 is a 25-item checklist measuring anxiety/depression symptoms over the previous month and is widely used in refugee research (Mollica, Wyshak, de Marneffe, Khuon, & Lavelle, Citation1987). Items are scored on 4-point Likert scales and a cut-off of ≥1.75 for ‘clinically significant distress’ is recommended (Nettelbladt, Hansson, Stefansson, Borgquist, & Nordstrom, Citation1993). In this study, the scale demonstrated strong internal consistency (α = .95).
1.4. Procedure
Ethical approval was obtained from the Monash University Human Research Ethics Committee (MUHREC 11901). All participants provided informed consent in Arabic. Participants attended two appointments one-week apart. In Session 1, participants were instructed on how to complete the sleep diary at home for seven-nights. In Session 2, the sleep diary was collected and participants completed the questionnaires.
1.5. Data analysis plan
Data analyses were performed using SPSS version 21. There were no missing data. The sample included 14 sets of married couples. To determine if the inclusion of both members of the couple influenced the findings, we created a dummy variable (couple versus individual). When we included this variable as a covariate in the analyses, in each instance this variable was non-significant and did not alter the outcome of any analyses reported below. We categorised each individual according to their level of sleep disturbance using ISI≥10 and/or SE≤85. Individuals not exceeding cut-offs on either measure were considered as ‘normal’ sleepers, ‘moderate’ levels of sleep disturbance were defined as an ISI≥10 or SE≤85 and ‘severe’ levels of sleep disturbance as ISI≥10 and SE≤85. We chose to use both ISI and diary SE to classify levels of sleep disturbance, because we did not conduct a formal diagnostic interview and given this was a community sample not selected for any specific sleep features, utilization of two measures provided a more conservative estimate than use of a single measure.
To examine Aim 1, descriptive statistics, the percentage of participants meeting clinical cut-offs, and sleep disturbance categories were tabulated. We used ANOVA and t-tests to test differences between Time 1 (T1) and Time 2 (T2). We addressed Aim 2 in two ways. First, we performed a series of multiple regression analyses (method: enter) to explore which T1 variables (i.e. post-migration stress, mental health, insomnia severity, pre-sleep arousal) predicted each of the Time 2 mental health outcomes (i.e. T2 PTSD, anxiety, and depression). Second, we used simple mediation analysis PROCESS macro in SPSS (5000 bootstrapped resamples) to explore whether the relationship between changes in post-migration stress (i.e. T2 post-migration stress – T1 post-migration stress) and changes in PTSD symptoms (i.e. T2 PTSD symptoms – T1 PTSD symptoms) was mediated by changes in sleep symptoms, controlling for trauma exposure. To test Aim 3, we used serial multiple mediation analysis PROCESS macro in SPSS (Hayes, Citation2012), with 5000 bootstrapped resamples. We applied 95% confidence intervals to construct the indirect path and bias-corrected confidence intervals that did not contain zero were considered significant. Effect sizes were reported using standardized indirect effect size and interpreted as small (.01), medium (.09), and large (.25) (Preacher & Kelley, Citation2011).
2. Results
2.1. Aim 1: levels of post-migration stress, mental health and sleep disturbance
As shown in , participants showed significant reductions in symptoms of PTSD, anxiety/depression and insomnia, and a significant increase in post-migration stress at T2, when compared to T1. No significant change was found in pre-sleep arousal. At T2, 42% (n = 29) of participants met clinical cut-off for PTSD and 34.8% (n = 24) met cut-off for anxiety/depression, compared to 62.3% (n = 43; PTSD) and 55.1% (n = 38; anxiety/depression) of the sample at T1.
Table 2. Descriptive t-test to compare T1 – T2 study variables
At T2, 49.3% of the participants were normal sleepers, 36.2% had moderate sleep disturbance, and 14.5% had severe sleep disturbance. illustrates the movement of sleep categories between T1 and T2. Many of the normal sleepers at T1 remained normal sleepers at T2. A considerable number of participants showed improvement in their sleep at T2. However, a substantial number of participants who had moderate and severe sleep disturbance at T1 continued to have disturbed sleep, and an additional 10% (n = 7) experienced worsening sleep at T2. We found that 42% (n = 29) of Syrian refugees suffered from chronic sleep difficulties (i.e. had moderate to severe sleep disturbance both at T1 and T2).
Table 3. Trend of sleep categories between two time points
2.2. Aim 2: predicting mental health symptoms at 12-month follow-up
As shown in , when predicting PTSD symptoms at 12-month follow-up, the full model was significant. However, only T1 pre-sleep arousal was a significant predictor of PTSD symptoms at T2. The same pattern emerged when predicting anxiety/depression symptoms; only T1 pre-sleep arousal uniquely predicted anxiety/depression symptoms at follow-up.
Table 4. Multiple regression analyses predicting time 2 mental health symptoms
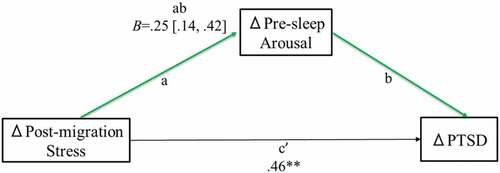
In terms of our second approach to addressing Aim 2, we first established that changes in post-migration stress were significantly related to changes in PTSD symptoms, B = .71, SE = .10, R2 = .45, F(2, 66) = 27.50, p < .001. When examining changes in pre-sleep arousal as a mediator of the relationship between change in post-migration stress and change in PTSD symptoms () the indirect effect (path ab) was significant, B = .25, SE = .07, 95% CI [.14, .42], R2 = .55, F(3, 65) = 26.32, p < .001. Change in post-migration stress remained a significant predictor of change in PTSD symptoms, B = .46, SE = .11, p < .001. When examining changes in insomnia as the mediator, the indirect effect was non-significant (path ab: B = .12, SE = .08, 95% CI [−.02, .32]).
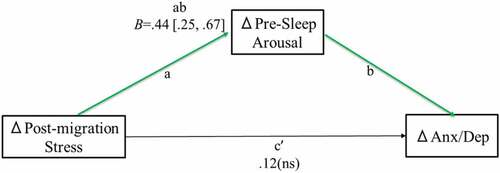
Figure 1. The effect of change in post-migration stress on change in PTSD through change in pre-sleep arousal
Change in post-migration stress was also significantly related to change in anxiety/depression symptoms, B = .71, SE = .10, R2 = .29, F(2, 66) = 13.44, p < .001. When examining change in pre-sleep arousal as the mediator (), the indirect effect was significant, B = .44, SE = .11, 95% CI [.25, .67], R2 = .57, F(3, 65) = 29.01, p < .001. When examining insomnia symptoms as the mediator, the indirect effect was significant, B = .27, SE = .11, 95% CI [.09, .51], R2 = .38, F(3, 65) = 11.12, p < .001. The direct effect of changes in post-migration stress on changes in anxiety/depression remained significant, B = .29, SE = .14, p < .05.
2.3. Aim 3: exploratory serial mediation models
2.3.1. Serial mediation model for PTSD
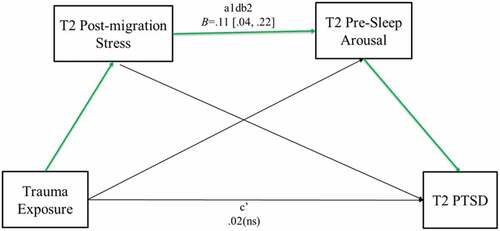
The total effect (path c) of trauma exposure on PTSD symptoms was significant (B = .38, SE = .13, p < .05) and the model accounted for 12% variance. As shown in , post-migration stress and pre-sleep arousal were significant sequential mediators of the relationship between trauma exposure and PTSD symptoms (path a1db2: B = .11, SE = .04, 95% CI [.04, .22]), with 64% of the effect coming indirectly through the two mediators. Furthermore, the direct effect (path c’) of trauma exposure was no longer a significant predictor of PTSD. When substituting insomnia symptoms as the sleep mediator, the sequential mediation path was again a significant predictor of PTSD symptoms (path a1db2: B = .07, SE = .04, 95% CI [.01, .17]), with 59% of the effect coming indirectly through the two mediators, and the direct effect (path c’) was no longer significant.
2.3.2. Serial mediation model for anxiety/depression
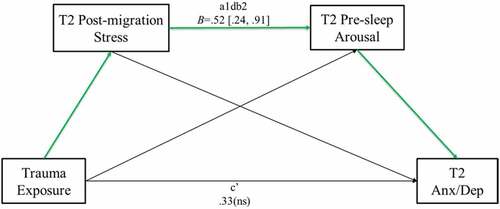
The total effect (path c) of trauma exposure on anxiety/depression was significant (B = 1.02, SE = .30, p = .001) and the model accounted for 15% variance. As shown in , current post-migration stress and current pre-sleep arousal sequentially mediated the relationship between trauma exposure and anxiety/depression (path a1db2: B = .52, SE = .17, 95% CI [.24, .91]), with 71% of the effect coming indirectly through the two mediators. The direct effect (path c’) of trauma exposure was no longer a significant predictor of T2 anxiety/depression. A comparable finding was observed when insomnia symptoms were included as the sleep mediator; the sequential mediation path significantly predicted T2 anxiety/depression symptoms (path a1db2: B = .38, SE = .17, 95% CI [.13, .81]), with 54% of the effect coming indirectly through the two mediators and the direct effect (path c’) was no longer significant.
3. Discussion
This study longitudinally examined mental health, sleep disturbance, and living difficulties in Syrian refugees. When compared to symptomatology at Time 1, we found significant reductions in symptoms of PTSD, anxiety/depression, and insomnia at Time 2 (i.e. 12 months later). However, we found an increase in post-migration stress and no significant change in pre-sleep arousal. Second, we found that changes in pre-sleep arousal significantly mediated the relationships between change in post-migration stress and change in mental health symptoms. Changes in insomnia significantly mediated the relationships between change in post-migration stress and change in anxiety/depression symptoms. Third, only pre-sleep arousal at Time 1 was a unique significant predictor of PTSD, anxiety/depression symptoms at Time 2. Finally, current post-migration stress and sleep symptoms (insomnia, pre-sleep arousal) mediated the relationship between trauma exposure and current mental health (PTSD, anxiety/depression) symptoms, replicating findings from the baseline study (Lies et al., Citation2020).
Our finding of significant reductions in mental health symptomatology aligns with previous research. For instance, Weine et al. (Citation1998) also found a reduction in PTSD symptoms at 12-month follow-up in Bosnian refugees who had resettled in the USA. Cooper et al. (Citation2019) found, in a longitudinal cohort study with newly arrived humanitarian refugees to Australia, clinically insignificant decrease in the prevalence of PTSD over 3 years. However, our finding was not consistent with the findings of Kaltenbach et al. (Citation2018) who found no change in symptomatology of refugees resettling in Germany over the course of 1 year or with longitudinal studies that have found a worsening of mental health symptoms over time (Lie, Citation2002; Roth et al., Citation2006). Thus, there is a need for further research examining the specific factors contributing to differing trajectories.
Accumulating research demonstrates that mental health and psychosocial problems are significantly associated with levels of sleep disturbance in refugees (Lies et al., Citation2020; Citation2019). The current study found, however, that over time sleep disturbance may reduce. Specifically, while only about one-third of the sample was considered normal sleepers at baseline, almost half of the sample was normal sleepers 12 months later. However, it is also worth highlighting that half of our participants still continued to report moderate to severe sleep disturbance at the 1 year follow-up, and 42% of our sample suffered from chronic sleep difficulties (i.e. moderate to severe sleep disturbance) across the 12-month period.
The sleep literature has demonstrated that various psychological factors, such as daily stress and pre-sleep arousal, play a fundamental role in the development and maintenance of insomnia (e.g. Winzeler et al., Citation2014). Trauma research highlights the well-established relationship between sleep disturbance and PTSD (e.g. Germain, McKeon, & Campbell, Citation2017). Despite improved understanding of the factors, little research has examined the impact of sleep disturbance on mental health in refugees. This current study aimed to examine theoretical models that account for the relationships between trauma exposure, post-migration stress, sleep symptoms, and mental health problems. These current longitudinal findings support our baseline findings (Lies et al., Citation2020); post-migration stress and sleep symptoms (insomnia, pre-sleep arousal) sequentially mediated the relationship between trauma exposure and mental health (PTSD, anxiety/depression symptoms).
In examining whether trauma exposure and baseline mental health, post-migration stress, insomnia, and pre-sleep arousal predicted mental health symptoms at 12-month follow-up, we found that while the overall model was significant, only baseline pre-sleep arousal emerged as a unique significant predictor. This indicates that pre-sleep arousal may be an important factor related to PTSD, anxiety/depression symptoms in this population. Additionally, we found the relations between changes in post-migration stress and changes in PTSD, anxiety/depression symptoms were mediated by changes in sleep symptoms, after controlling for trauma exposure. These mediation models highlight that sleep symptoms may play a significant role in the clinical presentation of chronic PTSD, anxiety, and depression symptoms in refugee populations.
Establishing sleep symptoms as a mediator of mental health has both theoretical and clinical significance. The conceptual models tested in the current study advance existing models as we have incorporated, in a more comprehensive manner, the associations among trauma exposure, post-migration stress, sleep symptoms, and mental health. Our findings provide additional support for the theory that highlights the importance of sleep in PTSD (Germain et al., Citation2017) and anxiety/depression (Li, Wu, Gan, Qu, & Lu, Citation2016; Oh, Kim, Na, Cho, & Chu, Citation2019). The research focused on sleep disturbances and psychological adjustment has previously been overlooked in refugee studies. Concurrently, there remain significant gaps in understanding the role of cognitive and somatic pre-sleep arousal in refugee psychological adjustment. Our findings demonstrate that further investigations into the specific relationship between cognitive/somatic pre-sleep arousal and trauma-related symptoms are warranted in refugee samples.
Clinically, the findings first highlight that given pre-sleep arousal emerged as a distinct predictor and mediator of mental health, the PSAS questionnaire may have potential clinical utility in terms of screening and treatment evaluation in refugee populations. Second, our findings call for further investigation for the effectiveness of sleep-focused interventions in improving psychological outcomes among refugees. Mindfulness-based training has shown potential in reducing pre-sleep arousal and improving sleep quality (Hassirim, Lim, Lo, & Lim, Citation2019) and Cognitive Behavioural Therapy for Insomnia is effective in targeting sleep disturbance commonly seen in PTSD (Walters et al., Citation2019).
Third, there is often stigma concerning psychological problems amongst refugees (Summerfield, Citation2005; Valibhoy, Kaplan, & Szwarc, Citation2017). Amongst refugees, mental health concerns are often raised in primary care settings in the context of dealing with physical problems, such as headaches, fatigue, difficulty sleeping, and difficulty breathing (Summerfield, Citation1999, Citation2005). Therefore, targeting sleep, as part of the larger mental health intervention, may lessen the focus on psychological mental health and pathologizing responses to events that often have a social and political origin. Focusing on a culturally relevant physiological symptom, such as sleep, may increase treatment-seeking behaviour and treatment adherence among refugees. However, these hypotheses need further investigation.
There are several limitations worth noting. While the measures employed in this study have been validated for use with refugees from multiple cultures, they have not been specifically adapted for the Syrian community. Another potential limitation is the mental health measures were not diagnostic. Second, while we were able to replicate the serial mediation model again at 12 months, it was conducted using the same sample of participants. Thus, future replication research is still needed. Finally, it is difficult to ascertain a priori sample size estimates in longitudinal research, particularly as this area of research is novel. Thus, there was limited previous research available to guide sample size estimates. Consequently, our analyses may have been underpowered. Therefore, future research assessing our hypotheses needs to be conducted in a larger sample size in order to provide greater confidence and generalizability of our findings. Despite these limitations, the current study highlights the extent of chronic sleep disturbance among Syrian refugees resettling in a high-income country and establishes that such sleep symptoms are mediators of longer-term mental health in this population. Moreover, this study has bridged the divide between trauma-focused and sleep-focused frameworks in the study of refugee mental health.
Acknowledgments
Part of this publication was supported by the Monash University’s Faculty of Arts Postgraduate Publication Award (PPA).
Disclosure statement
No potential conflict of interest was reported by the authors.
Data available statement
The data file can be accessed at Open Science Framework (DOI 10.17605/OSF.IO/D3J7F).
References
- Alpak, G., Unal, A., Bulbul, F., Sagaltici, E., Bez, Y., Altindag, A., … Savas, H. A. (2015). Post-traumatic stress disorder among Syrian refugees in Turkey: A cross-sectional study. International Journal of Psychiatry in Clinical Practice, 19(1), 45–11.
- Belleville, G., Guay, S., & Marchand, A. (2009). Impact of sleep disturbances on PTSD symptoms and perceived health. Journal of Nervous & Mental Disease, 197(2), 126–132.
- Bogic, M., Njoku, A., & Priebe, S. (2015). Long-term mental health of war-refugees: A systematic literature review. BMC International Health and Human Rights, 15(29). doi:10.1186/s12914-015-0064-9
- Bontempo, R. (1993). Translation fidelity of psychological scales: An item response theory analysis of an individualism-collectivism scale. Journal of Cross-cultural Psychology, 24(2), 149–166.
- Bryant, R. A., Creamer, M., O’Donnell, M., Silove, D., & McFarlane, A. C. (2010). Sleep disturbance immediately prior to trauma predicts subsequent psychiatric disorder. Sleep, 33(1), 69–74.
- Bryant, R. A., Edwards, B., Creamer, M., O’Donnell, M., Forbes, D., Felmingham, K. L., … Hadzi-Pavlovic, D. (2018). The effect of post-traumatic stress disorder on refugees’ parenting and their children’s mental health: A cohort study. The Lancet Public Health, 3(5), e249–e258.
- Carney, C. E., Buysse, D. J., Ancoli-Israel, S., Edinger, J. D., Krystal, A. D., Lichstein, K. L., & Morin, C. M. (2012). The consensus sleep diary: Standardizing prospective sleep self-monitoring. Sleep, 35(2), 287–302.
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed. ed.). Hillsdale, NJ: Lawrence Erlbaum.
- Collins, J., Reid, C., Groutsis, D., Watson, K., & Ozkul, D. (2018). Syrian and Iraqi refugee settlement in Australia. Retrieved from https://www.uts.edu.au/sites/default/files/article/downloads/Collins.Reid_.Groutsis.Australia.Syrian-Conflict%20Refugee%20Settlement%20in%20Australia.pdf
- Cooper, S., Enticott, J. C., Shawyer, F., & Meadows, G. (2019). Determinants of mental illness among humanitarian migrants: Longitudinal analysis of findings from the first three waves of a large cohort study. Frontiers in Psychiatry, 10(545). doi:10.3389/fpsyt.2019.00545
- El Arnaout, N., Rutherford, S., Zreik, T., Nabulsi, D., Yassin, N., & Saleh, S. (2019). Assessment of the health needs of Syrian refugees in Lebanon and Syria’s neighboring countries. Conflict and Health, 13(1), 31.
- Gehrman, P., Seelig, A. D., Jacobson, I. G., Boyko, E. J., Hooper, T. I., Gackstetter, G. D., … Smith, T. C. (2013). Predeployment sleep duration and insomnia symptoms as risk factors for new-onset mental health disorders following military deployment. Sleep, 36(7), 1009–1018.
- Germain, A., Buysse, D. J., & Nofzinger, E. (2008). Sleep-specific mechanisms underlying posttraumatic stress disorder: Integrative review and neurobiological hypotheses. Sleep Medicine Reviews, 12(3), 185–195.
- Germain, A., McKeon, A. B., & Campbell, R. L. (2017). Sleep in PTSD: Conceptual model and novel directions in brain-based research and interventions. Current Opinion in Psychology, 14, 84–89.
- Giosan, C., Malta, L. S., Wyka, K., Jayasinghe, N., Evans, S., Difede, J., & Avram, E. (2015). Sleep disturbance, disability, and posttraumatic stress disorder in utility workers. Journal of Clinical Psychology, 71(1), 72–84.
- Hansen, M., Andersen, T. E., Armour, C., Elklit, A., Palic, S., & Mackrill, T. (2010). PTSD-8: A short PTSD inventory. Clinical Practice & Epidemiology in Mental Health, 6(1), 101–108.
- Harvey, A. G. (2002). A cognitive model of insomnia. Behaviour Research and Therapy, 40(8), 869–893.
- Hassan, G., Ventevogel, P., Jefee-Bahloul, H., Barkil-Oteo, A., & Kirmayer, L. J. (2016). Mental health and psychosocial wellbeing of Syrians affected by armed conflict. Epidemiology and Psychiatric Sciences, 25(2), 129–141.
- Hassirim, Z., Lim, E. C. J., Lo, J. C., & Lim, J. (2019). Pre-sleep cognitive arousal decreases following a 4-week introductory mindfulness course. Mindfulness, 10(11), 2429–2438.
- Hayes, A. F. (2012). PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling. Retrieved from http://www.afhayes.com/public/process2012.pdf
- Kaltenbach, E., Schauer, M., Hermenau, K., Elbert, T., & Schalinski, I. (2018). Course of mental health in refugees-a one year panel survey. Frontiers in Psychiatry, 9, 352.
- Kaya, E., Kiliç, C., Karadağ Çaman, Ö., & Üner, S. (2019). Posttraumatic stress and depression among syrian refugees living in Turkey: Findings from an urban sample. The Journal of Nervous and Mental Disease, 207(12), 995–1000.
- Kazour, F., Zahreddine, N. R., Maragel, M. G., Almustafa, M. A., Soufia, M., Haddad, R., & Richa, S. (2017). Post-traumatic stress disorder in a sample of Syrian refugees in Lebanon. Comprehensive Psychiatry, 72, 41–47.
- Lamkaddem, M., Stronks, K., Deville, W. D., Olff, M., Gerritsen, A. A., & Essink-Bot, M. L. (2014). Course of post-traumatic stress disorder and health care utilisation among resettled refugees in the Netherlands. BMC Psychiatry, 14, 90.
- Li, L., Wu, C., Gan, Y., Qu, X., & Lu, Z. (2016). Insomnia and the risk of depression: A meta-analysis of prospective cohort studies. BMC Psychiatry, 16(1), 375.
- Lie, B. (2002). A 3-year follow-up study of psychosocial functioning and general symptoms in settled refugees. Acta Psychiatrica Scandinavica, 106(6), 415–425.
- Lies, J., Jobson, L., Mascaro, L., Whyman, T., & Drummond, S. P. A. (2020). Post-migration stress and sleep disturbances mediate the relationship between trauma exposure and post-traumatic stress symptoms among Syrian and Iraqi refugees. The Journal of Clinical Sleep Medicine. doi: https://doi.org/10.5664/jcsm.8972.
- Lies, J., Mellor, A., Jobson, L., & Drummond, S. P. A. (2019). Prevalence of sleep disturbance and its relationships with mental health and psychosocial issues in refugees and asylum seekers attending psychological services in Australia. Sleep Health: Journal of the National Sleep Foundation, 5(4), 335–343.
- Miller, K. E., & Rasmussen, A. (2010). War exposure, daily stressors, and mental health in conflict and post-conflict settings: Bridging the divide between trauma-focused and psychosocial frameworks. Social Science & Medicine, 70(1), 7–16.
- Miller, K. E., & Rasmussen, A. (2016). The mental health of civilians displaced by armed conflict: An ecological model of refugee distress. Epidemiology and Psychiatric Sciences, 26(2), 129–138.
- Mollica, R. F., Sarajlic, N., Chernoff, M., Lavelle, J., Sarajlic, I. V., & Massagli, M. P. (2001). Longitudinal study of psychiatric symptoms, disability, mortality, and emigration among Bosnian refugees. JAMA, 286(5), 546.
- Mollica, R. F., Wyshak, G., de Marneffe, D., Khuon, F., & Lavelle, J. (1987). Indochinese versions of the Hopkins symptom checklist-25: A screening instrument for the psychiatric care of refugees. The American Journal of Psychiatry, 144(4), 497–500.
- Morin, C. M. (1993). Insomnia:. Psychological assessment and management. New York: Guilford Press.
- Morin, C. M., Belleville, G., Bélanger, L., & Ivers, H. (2011). The insomnia severity index: Psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep, 34(5), 601–608.
- Morin, C. M., Rodrigue, S., & Ivers, H. (2003). Role of stress, arousal, and coping skills in primary Insomnia. Psychosomatic Medicine, 65(2), 259–267.
- Nappi, C. M., Drummond, S. P. A., & Hall, J. M. H. (2012). Treating nightmares and insomnia in posttraumatic stress disorder: A review of current evidence. Neuropharmacology, 62(2), 576–585.
- Nettelbladt, P., Hansson, L., Stefansson, C. G., Borgquist, L., & Nordstrom, G. (1993). Test characteristics of the Hopkins symptom check list-25 (HSCL-25) in Sweden, using the present state examination (PSE-9) as a caseness criterion. Social Psychiatry and Psychiatric Epidemiology, 28(3), 130–133.
- Nicassio, P. M., Mendlowitz, D. R., Fussell, J. J., & Petras, L. (1985). The phenomenology of the pre-sleep state: The development of the pre-sleep arousal scale. Behaviour Research and Therapy, 23(3), 263–271.
- Nickerson, A., Bryant, R. A., Silove, D., & Steel, Z. (2011). A critical review of psychological treatments of posttraumatic stress disorder in refugees. Clinical Psychology Review, 31(3), 399–417.
- Nickerson, A., Hadzi-Pavlovic, D., Edwards, B., O’Donnell, M., Creamer, M., Felmingham, K. L., … Bryant, R. A. (2019). Identifying distinctive psychological symptom profiles among a nationally representative sample of refugees resettled in Australia. Australian & New Zealand Journal of Psychiatry, 53(9), 908–919.
- Oh, C.-M., Kim, H. Y., Na, H. K., Cho, K. H., & Chu, M. K. (2019). The effect of anxiety and depression on sleep quality of individuals with high risk for insomnia: A population-based study. Frontiers in Neurology, 10(849). doi:10.3389/fneur.2019.00849
- Pan, H., Liu, S., Miao, D., & Yuan, Y. (2018). Sample size determination for mediation analysis of longitudinal data. BMC Medical Research Methodology, 18(1), 32.
- Picchioni, D., Cabrera, O. A., McGurk, D., Thomas, J. L., Castro, C. A., Balkin, T. J., … Hoge, C. W. (2010). Sleep symptoms as a partial mediator between combat stressors and other mental health symptoms in Iraq war veterans. Military Psychology, 22(3), 340–355.
- Preacher, K. J., & Kelley, K. (2011). Effect size measures for mediation models: Quantitative strategies for communicating indirect effects. Psychological Methods, 16(2), 93.
- Puzino, K., Amatrudo, G., Sullivan, A., Vgontzas, A., & Fernandez-Mendoza, J. (2019). Clinical significance and cut-off scores for the pre-sleep arousal scale in chronic insomnia disorder: A replication in a clinical sample. Behavioral Sleep Medicine, 1–14. doi:10.1080/15402002.2019.1669604
- Reed, D. L., & Sacco, W. P. (2016). Measuring sleep efficiency: What should the denominator be? Journal of Clinical Sleep Medicine, 12(2), 263–266.
- Ross, R. J., Ball, W. A., Sullivan, K. A., & Caroff, S. N. (1989). Sleep disturbance as the hallmark of posttraumatic stress disorder. American Journal of Psychiatry, 146(6), 697–707.
- Roth, G., Ekblad, S., & Agren, H. (2006). A longitudinal study of PTSD in a sample of adult mass-evacuated Kosovars, some of whom returned to their home country. European Psychiatry, 21(3), 152–159.
- Shoeb, M., Weinstein, H., & Mollica, R. (2007). The harvard trauma questionnaire: Adapting a cross-cultural instrument for measuring torture, trauma and posttraumatic stress disorder in Iraqi refugees. International Journal of Social Psychiatry, 53(5), 447–463.
- Silove, D., Sinnerbrink, I., Field, A., Manicavasagar, V., & Steel, Z. (1997). Anxiety, depression and PTSD in asylum-seekers: Associations with pre-migration trauma and post-migration stressors. The British Journal of Psychiatry, 170(4), 351–357.
- Steel, Z., Silove, D., Bird, K., McGorry, P., & Mohan, P. (1999). Pathways from war trauma to posttraumatic stress symptoms among Tamil asylum seekers, refugees, and immigrants. Journal of Traumatic Stress, 12(3), 421–435.
- Steele, M., Germain, A., & Campbell, J. S. (2017). Mediation and moderation of the relationship between combat experiences and post-traumatic stress symptoms in active duty military personnel. Military Medicine, 182(5–6), e1632–e1639.
- Summerfield, D. (1999). A critique of seven assumptions behind psychological trauma programmes in war-affected areas. Social Science & Medicine, 48(10), 1449–1462.
- Summerfield, D. (2005). “My whole body is sick … my life is not good”: A Rwandan asylum seeker attends a psychiatric clinic in London. In D. Ingleby (Ed.), Forced migration and mental health: Rethinking the care of refugees and displaced persons (pp. 97–114). New York: Springer US.
- United Nations High Commissioner for Refugees (UNHCR). (2019). Figures at a glance. Retrieved from https://www.unhcr.org/ph/figures-at-a-glance
- Valibhoy, M. C., Kaplan, I., & Szwarc, J. (2017). “It comes down to just how human someone can be”: A qualitative study with young people from refugee backgrounds about their experiences of Australian mental health services. Transcultural Psychiatry, 54(1), 23–45.
- von Haumeder, A., Ghafoori, B., & Retailleau, J. (2019). Psychological adaptation and posttraumatic stress disorder among Syrian refugees in Germany: A mixed-methods study investigating environmental factors. European Journal of Psychotraumatology, 10(1), 1686801.
- Walters, E. M., Jenkins, M. M., Nappi, C. M., Clark, J., Lies, J., Norman, S. B., & Drummond, S. P. A. (2019). The impact of prolonged exposure on sleep and enhancing treatment outcomes with evidence-based sleep interventions: A pilot study. Psychological Trauma: Theory, Research, Practice, and Policy, 11(8), 811–937.
- Weine, S. M., Vojvoda, D., Becker, D. F., McGlashan, T. H., Hodzic, E., Laub, D., … Lazrove, S. (1998). PTSD symptoms in Bosnian refugees 1 year after resettlement in the USA. American Journal of Psychiatry, 155(4), 562–564.
- Winzeler, K., Voellmin, A., Schäfer, V., Meyer, A. H., Cajochen, C., Wilhelm, F. H., & Bader, K. (2014). Daily stress, presleep arousal, and sleep in healthy young women: A daily life computerized sleep diary and actigraphy study. Sleep Medicine, 15(3), 359–366.
- Wright, K. M., Britt, T. W., Bliese, P. D., Adler, A. B., Picchioni, D., & Moore, D. (2011). Insomnia as predictor versus outcome of PTSD and depression among Iraq combat veterans. Journal of Clinical Psychology, 67(12), 1240–1258.