ABSTRACT
Loperamide is a widely available, over-the-counter medication. The advent of the opioid epidemic has seen cases of loperamide overdose being reported. The common side effects of the medication can be relatively benign, but at high doses, loperamide can precipitate life-threatening arrhythmias. Our case highlights rare side effects of loperamide overdose inducing ventricular tachycardia, with unfavorable consequences. This case emphasizes that the distribution and availability of this medication should be restricted, to be a prescription drug, to prevent overdose and adverse outcomes.
1. Introduction
Loperamide is a commonly used and widely available over the counter anti-motility agent, generally considered to be safe without serious side effects. The rise of the opioid epidemic has seen increasing number of overdose cases being reported. Acting as an agonist on μ-opioid receptors, it can mimic the effects of prescription opioids. Excessive ingestion may precipitate arrhythmias with untoward outcomes. Diagnosis and management of overdose associated with life-threatening arrhythmia can be a challenge.
2. Case Presentation
We present a case of a 36-year-old male with a remote history of opiate abuse, brought to the hospital after being found unresponsive at his workplace. He was last seen by a colleague at work, a few minutes before being found down.
Cardiopulmonary resuscitation (CPR) was initiated at the site. Emergency medical services reported his initial rhythm to be asystole, followed by ventricular tachycardia (VT). CPR and defibrillation were followed by the return of spontaneous circulation ROSC) after 25 minutes. Post-ROSC electrocardiogram (EKG) was suggestive of a wide complex idioventricular rhythm. He was intubated at the site and brought to the hospital for evaluation. He was found to have multiple bottles of loperamide in his pocket. On questioning the patient’s family revealed that he had abused opioids in the past however, they were unaware of recent opiate misuse. No recent diarrheal illness was reported. No family history of sudden cardiac death was noted.
On presentation to the emergency room (ER), the patient’s vital signs were blood pressure 135/77 mm/hg, Pulse: 68 bpm, with oxygen saturation 99% on the ventilator.
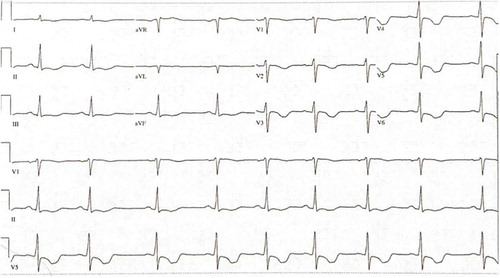
The initial 12 lead EKG obtained in the emergency room demonstrated sinus rhythm with complete heart block and wide complex ventricular escape rhythm at a rate of 96 beats per minute, the PR interval was undetectable, QRS duration was 166 ms, and the QTC interval was 645 ms.
Pertinent investigations obtained post-resuscitation, upon arrival to the hospital are as shown below:
Serum and urine drug toxicology screen was negative. Initial imaging including a chest x-ray, CT scan of the head and neck were unrevealing. An echocardiogram was suggestive of severely reduced ejection fraction of 25–30%, with global hypokinesis. Cardiac catheterization did not reveal any obstructive coronary artery disease.
Therapeutic hypothermia was initiated to achieve a target core body temperature of between 32–34°C for 24 hours. During the course of the first 48 hours of hospitalization, he continued to have multiple episodes of VT, torsades, and bradycardia requiring lidocaine, and magnesium infusions.
Successful targeted temperature management was followed by re-warming, with reassessment of his neurological status at regular intervals. The patient had limited neurological recovery and underwent a repeat CT without the contrast of his head on day 3 of his hospitalization, which was concerning for cerebral edema. He underwent treatment with therapeutic hypertonic saline.
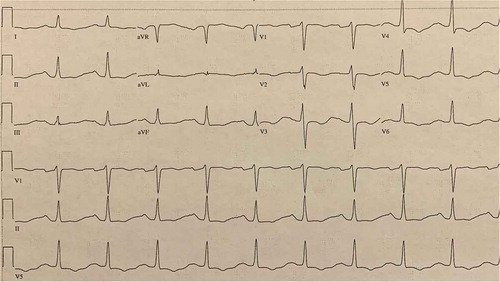
Hospitalization was further complicated by fevers on day 4 of his hospital stay, with chest x-ray demonstrating right upper lobe pneumonia. Methicillin-sensitive Staphylococcus aureus was cultured on bronchoscopy washings. Antibiotics were initiated and a 14-day regimen was completed. A repeat echocardiogram on day 10 showed improvement of ejection fraction to 50–55% with no regional wall motion abnormalities. Through the hospitalization, the patient’s EKG changes evolved with progressive shortening and normalization of the QTC and QRS intervals. The patient did not exhibit any significant neurological recovery, with serial CT scans of the head showing worsening edema. An MRI of the brain suggested anoxic brain injury. The patient was extubated on hospitalization day 20. The available options were discussed with the family, they opted to proceed with comfort directed care, with transfer to a hospice facility.
3. Discussion
Loperamide is a phenylpiperidine derivative structurally similar to diphenoxylate and haloperidol [Citation1]. It is a commonly used over the counter anti-diarrheal medication. Antidiarrheal effects of loperamide are mediated through direct agonism at the circular and longitudinal intestinal muscles via activation of peripheral mu-opioid receptors [Citation2]
At high doses, Loperamide can induce opioid-like euphoric effects on the central nervous system. Given the poor oral bioavailability coupled with limited brain penetration, studies suggest cardiotoxicity to be associated with doses 10–30 times higher than the maximum therapeutic dose [Citation3].
The opioid epidemic has seen a rise in the use of loperamide as an opioid alternative to relieve symptoms of narcotic withdrawal [Citation4]. Presentations of loperamide intoxication manifesting as recurrent syncope in conjunction with ECG abnormalities and cardiac arrest have been accounted for in literature [Citation5].
Loperamide overdose may lead to cardiac conduction disturbances which range in severity from QRS widening to QT prolongation, and the development of the potentially lethal polymorphic and monomorphic ventricular tachycardia [Citation6,Citation7].
The Inhibition of NaV1.5, a voltage-gated sodium channel subunit the cardiac muscle, has been shown to contribute to QRS prolongation [Citation3]. Recent in vitro studies have shown that loperamide is a potent inhibitor of the human ether-a-go-go-related gene K+ channel (hERG) and this activity potentiates QT prolongation and torsades de pointes [Citation7,Citation8].
We propose that our patient’s ventricular tachycardia may have been potentially preceded by QT prolongation by these mechanisms and precipitated the ventricular arrhythmia.
Loperamide was approved for use by the FDA in 1976. Effects seem to be limited to the gut at maximal recommended doses of 16 mg/day. At high doses however the euphoric effects, have led to overuse to help with opiate withdrawal symptoms and for recreational use as an opiate substitute [Citation9]. The pharmacokinetic half-life of loperamide is approximately 9–13 h, although longer half-lives have been reported with very high doses [Citation10]. This seems to be consistent with our patient’s EKG manifestations, with episodes of ventricular tachycardia becoming less frequent by day 2 of his hospitalization. The QRS and QTC intervals exhibited progressive regression through the hospital stay with QRS and QTC being 104 ms and 502 ms respectively at discharge.
Though toxicological laboratory studies routinely screen for opioid, loperamide levels are not routinely available in a commercial laboratory, being limited to specialized centers. History of opiate abuse and clinical suspicion help in establishing the diagnosis.
Treatment of overdose is mainly supportive, including providing cardiopulmonary life support. Therapeutic interventions tried in the treatment of loperamide induced cardiotoxicity include atropine, amiodarone, lidocaine, magnesium and sodium bicarbonate. In addition, pharmacological and electric pacing have been necessary in some cases to achieve heart rate overdrive for arrhythmia control [Citation1].
4. Conclusion
The opiate abuse epidemic continues to be a major concern. Individuals with opiate dependence use various remedies to help ameliorate withdrawal symptoms of opiates. Recent cases have reported the use of Loperamide in very high quantities, to mimic the effects of opiates. Our case highlights the importance of a potentially deadly side effect of this very widely available medication that can be purchased in bulk quantities of several hundred milligrams per bottle. With increasing cases of an overdose being reported, regulations on the purchase of this over the counter medication should be considered.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Akel T, Bekheit S. Loperamide cardiotoxicity: “A brief review”. Ann Noninvasive Electrocardiol. 2018 Mar;23(2):e12505.
- Sobczak M, Sałaga M, Storr MA, et al. Physiology, signaling, and pharmacology of opioid receptors and their ligands in the gastrointestinal tract: current concepts and future perspectives. J Gastroenterol. 2014 Jan 1;49(1):24–45.
- Kang J, Compton DR, Vaz RJ, et al. Proarrhythmic mechanisms of the common anti-diarrheal medication loperamide: revelations from the opioid abuse epidemic. Naunyn-Schmiedeberg’s Arch Pharmacol. 2016 Oct 1;389(10):1133–1137.
- Miller H, Panahi L, Tapia D, et al. Loperamide misuse and abuse. J Am Pharm Assoc. 2017 Mar 1;57(2):S45–50.
- Wu PE, Juurlink DN. Clinical review: loperamide toxicity. Ann Emerg Med. 2017 Aug 1;70(2):245–252.
- Marraffa JM, Holland MG, Sullivan RW, et al. Cardiac conduction disturbance after loperamide abuse. Clin Toxicol. 2014 Nov 1;52(9):952–957.
- Vaz RJ, Kang J, Luo Y, et al. Molecular determinants of loperamide and N-desmethyl loperamide binding in the hERG cardiac K+ channel. Bioorg Med Chem Lett. 2018 Feb 1;28(3):446–451.
- Klein MG, Haigney MC, Mehler PS, et al. Potent inhibition of hERG channels by the over-the-counter antidiarrheal agent loperamide. JACC: Clin Electrophys. 2016 Dec 1; 2(7):784–789.
- Vaughn P, Solik MM, Bagga S, et al. Electrocardiographic abnormalities, malignant ventricular arrhythmias, and cardiomyopathy associated with loperamide abuse. J Cardiovasc Electrophysiol. 2016 Oct;27(10):1230–1233.
- Eggleston W, Nacca N, Marraffa JM. Loperamide toxicokinetics: serum concentrations in the overdose setting. Clin Toxicol. 2015 May 28;53(5):495–496.