ABSTRACT
Robust scientific evidence related to two rotavirus (RV) vaccines available worldwide demonstrates their significant impact on RV disease burden. Improving RV vaccination coverage may result in better RV disease control. To make RV vaccination accessible to all eligible children worldwide and improve vaccine effectiveness in high-mortality settings, research into new RV vaccines continues. Although current and in-development RV vaccines differ in vaccine design, their common goal is the reduction of RV disease risk in children <5 years old for whom disease burden is the most significant. Given the range of RV vaccines available, informed decision-making is essential regarding the choice of vaccine for immunization. This review aims to describe the landscape of current and new RV vaccines, providing context for the assessment of their similarities and differences. As data for new vaccines are limited, future investigations will be required to evaluate their performance/added value in a real-world setting.
PLAIN LANGUAGE SUMMARY
The disease
Rotaviruses are a leading cause of acute diarrhea, also called gastroenterities, among young children. They can lead to servere dehydration, hospitilization, and even death.
Several vaccines against rotavirus disease have been developed. Their design is based on:
weakened human rotavirus that mimic natural infection without causing disease, such as Rotarix, Rotavin-M1, Rotavac and RV3-BB (not yet marketed)
non-infective animal viruses such as RotaTeq, Rotasiil or LLR.
new concepts, such as inactivated vaccines
What is new?
We reviewed the current, recently launched and soon-to-be-launched rotavirus vaccines and found that:
Rotarix and RotaTeq have been used globally for more than a decade with demonstrated impact and favourable safety profile
Limited data on the impact and safety profile are available to date for:
Rotavin-M1 and LLR vaccines, locally marketed in Vietnam and China, respectively
Rotavac and Rotasiil, licensed in india
New vaccine concepts have been mainly investigated animal models with encouraging results
What is the impact?
Despite their different designs, the current rotavirus vaccines demonstrate effectiveness in protecting against rotairus gastroenterits.
Data for most recent vacciness are currently limited, for which additional data are needed to demonstrate how they will perform on a larger scale, their added value in a real setting and ther safety profile.
1 Introduction
Rotavirus (RV) gastroenteritis (RVGE) is a common disease that infects most children before the age of 5 years.Citation1,Citation2 Developing countries show a higher disease burden compared to developed countries, especially in very young children, due to higher comorbidity rates during childhood and inadequate access to preventive and treatment measures. As a result, the vast majority of RV-associated deaths occur in low-income countries.Citation2,Citation3 RV is highly contagious, spreading predominantly through a fecal-oral mode of transmission, and displays resistance to common disinfectants.Citation4 Upon ingestion, RVs replicate in the mature villous cells of the small intestine mucosa and cause fever, acute watery diarrhea, and vomiting. The resulting loss of body fluids may lead to severe dehydration, especially in the vulnerable age group of 3 months to 3 years, requiring timely hospitalization and treatment with oral rehydration and/or intravenous fluids.Citation2,Citation3 In 2016, RV infection was responsible for an estimated 1,537,000 (95% uncertainty interval [UI], 285,000 − 7,750,500) hospitalizations among children younger than 5 years, globally.Citation5
Vaccination has been identified as an efficient strategy to reduce the risk of RV infections and substantially reduce the disease burden. After the first recommendation in 2006, the World Health Organization (WHO) issued a reinforcement in 2009 supporting that RV vaccination should be offered to infants in all regions of the world, especially in regions with high diarrhea-related death rates.Citation6 The 2013 WHO position paper on rotavirus vaccines also states that the use of RV vaccines should be part of a comprehensive strategy to control diarrheal diseases using both prevention (e.g. promotion of basic hygienic measures, improved water supply and sanitation) and treatment packages (e.g. oral rehydration therapy).Citation2 For more than one decade, RV vaccines have substantially contributed to the global reduction of RV-associated mortality.Citation5,Citation7 However, due to unequal coverage of RV vaccines in different regions, RV was still responsible for 128,500 (95% UI, 104,500–155,600) deaths among children younger than 5 years in 2016, nearly all in low- and middle-income countries.Citation5
1.1 Understanding RV Biology
RV belongs to the genus Rotavirus (family Reoviridae) and is a wheel-shaped virus that has three concentric protein layers: an internal capsid (core), an intermediate capsid, and an outer capsid.Citation8 presents the structure of RV. The inner core contains the viral genome, which is composed of 11 segments of double-stranded RNA. The 12 proteins encoded by the 11 RNA segments of RV are divided into 6 structural viral proteins (VPs) and 6 non-structural proteins (NSPs).Citation8
Figure 1. Rotavirus structure and potential vaccine targets.
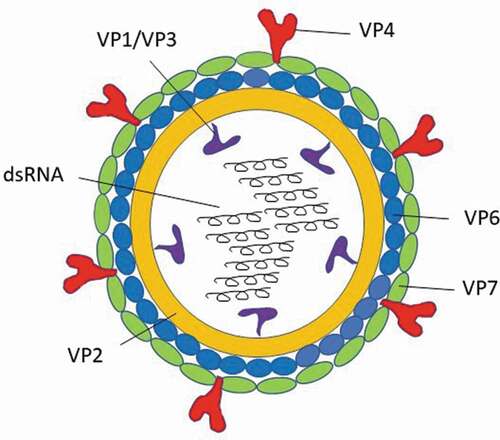
The amino acid sequence of the structural protein of the inner capsid layer, VP6, is used to classify RV into at least eight groups/species (referred to as RVA-RVH), of which groups A, B, C, and H have been found to infect humans and animals, and group A is the major cause of RV‐associated infections in humans.Citation9 Group A RVs are further categorized into genotypes based on differences in the RNA sequences that encode the two external proteins: VP4 and VP7. VP7 (a glycoprotein) determines the genotype G, whereas VP4 (a protease-cleaved protein) determines the genotype P.Citation8 More than 90% of group A RV genotypes correspond to one of the following strains: G1P[8], G2P[4], G3P[8], G4P[8], G9P[8], and G12P[8].Citation2,Citation10
Several RV proteins are involved in the immune response, including VP4 and VP7, which were shown to induce neutralizing RV-specific antibodies and enhance protective immunity. These proteins along with the highly immunogenic capsid-component VP6 have been crucial in RV vaccine development.Citation11,Citation12
However, to date, the immunological correlate of protection for RV remains to be firmly established.Citation11
1.2 RV vaccine development
Due to the substantial public health burden of RVGE, the need for effective prevention was critical. Following the discovery of RV, research into RV vaccines was initiated.Citation13,Citation14 The key observations and requirements for RV vaccine development included:
studies showed that a natural, early infection with RV prevented the development of clinically severe forms of the disease upon re-infection, and that repeated exposure to RV induced a broader heterotypic immune response;Citation12
due to the lack of a definite correlate of protection against RVGE, large efficacy trials to test RV vaccines would need to be based on clinical efficacy endpoints, e.g. moderate-to-severe RV-positive diarrheal disease;Citation15 and
an ideal RV vaccine should provide early and broad protection against the circulating and evolving RV strains.Citation16
These observations led to a first strategy for RV vaccine development using live-attenuated RV, which mimics natural infection and subsequent immune response, but without causing disease. Since interspecies infection is limited (this phenomenon being referred to as “host range restriction”), animal RVs are naturally attenuated for humans. Immunization with animal-based RV vaccines, called the “Jennerian” approach, was tested in the late 1980s but failed to achieve acceptable protection in infants.Citation17 Alternative approaches using either attenuated human RV strains or animal-human reassortant RV strains were therefore explored. The production of reassortant vaccines is based on the ability of RVs to combine with each other during mixed infections in vitro.Citation17 Such a vaccine formulation which consists of some genes from the animal RV parent and from the human RV parent − termed the “modified Jennerian” approach − resulted in the development of the first RV vaccine, Human Rhesus Rotavirus (HRRV; Rotashield, Wyeth-Lederle, USA), containing a mixture of four rhesus-human reassortant strains. Licensed in the United States of America (USA) in 1998, HRRV was withdrawn approximately one year later due to its association with intussusception (IS), an intestinal invagination that can result in life-threatening bowel obstruction.Citation18
Following the withdrawal of HRRV and 8 years of further research, two second-generation vaccines reached licensing stages in 2004 and 2006, respectively: 1) HRV, an oral human live-attenuated RV vaccine containing a single RV strain (Rotarix, GSK, Belgium)Citation19 and 2) HBRV, an oral bovine-human reassortant vaccine containing five reassortant strains (RotaTeq, Merck & Co., Inc, USA).Citation20 Both candidate vaccines published their landmark phase III trial results in the same issue of The New England Journal of Medicine in January 2006.Citation21,Citation22 They have since become the two most commonly used RV vaccines worldwide.Citation23 Their routine use in the National Immunization Program (NIP) is recommended by several national health authorities,Citation23 including the CDC (Centers for Disease Control and Prevention) in the USA,Citation24 where these two vaccines are available for use. Although differing in concept, HRV and HBRV have both had a tremendous impact on the burden of RV disease.Citation14
Other RV vaccines − following similar vaccine concepts to those employed for the two widely established vaccines − are either already locally marketed or in various development stages. Although several options are already available, research and development of new RV vaccines is ongoing with the aim of improving the global supply of RV vaccines, reducing vaccine cost, and improving vaccine effectiveness, in particular in developing countries.Citation17,Citation25 The early phase vaccines (pre-clinical stage) that are currently being developed provide novel approaches to promoting anti-RV immunity, such as inactivated virus, expression of viral recombinant proteins, or virus-like particles (VLPs).Citation25,Citation26 Thus, a unique vaccine landscape comprising several vaccine concepts is emerging in the field of protection against RV.
The different concepts of RV vaccines may result in different vaccine properties. Nevertheless, as licensed RV vaccines are able to provide broad protection against a variety of non-vaccine type RV strains,Citation27–29 the choice between these is often driven by programmatic considerations. To make the most appropriate choice for the implementation of RV vaccination, it is crucial for health authorities, healthcare practitioners, and other public health experts to understand the rationale, advantages, and limitations of the different RV vaccine options. While scientific evaluation of the currently available vaccines is well covered by published literature, our contribution emphasizes selection in private market in clinic use and programmatic issues in universal mass vaccination use, which could impact preferences among practitioners and recommending bodies. This literature review was conducted to gather and compare currently available information for established, recently licensed and in-development RV vaccines.
2 Methodology
This article is a non-systematic, comprehensive literature search carried out between the 1st of February 2017 and the 31st of August 2019 in PubMed and Embase with the aim of mapping the characteristics of RV vaccines (pre- and post-registration/licensure) according to their vaccine design, immunogenicity, efficacy, effectiveness, impact, and safety data for marketed and in-development RV vaccines. We subdivided the overall search into individual searches for each RV vaccine, with search terms including brand name, generic name, and manufacturer of the vaccine.
We complemented the literature search with a parallel search on Google and Google Scholar using the search terms mentioned above. The Google internet search enabled us to retrieve conference presentations and result summaries of products in clinical development or early stages of market launch for which the published data from journal articles retrieved via PubMed was limited. Additional sources of summarized data for the well-established HRV and HBRV vaccines, such as the summaries of product characteristics, were also identified through a Google search.
Among the results obtained, we considered information sources and articles with abstract and/or full text written in English. For the extensively studied HRV and HBRV vaccines, we selected recent informative articles that contained summarized data. For vaccines in late-stage development and locally marketed vaccines (including those recently prequalified by the WHO), we took into consideration all sources retrieved from PubMed, Google, Google Scholar, and Embase searches.
3 Results
The results of the literature search enabled us to gather the characteristics of the different RV vaccines including strains used, dosage, and presentation, clinical data on vaccine efficacy, effectiveness, and safety. We classified the vaccines and presented their data in tables as follows:
-: oral, live-attenuated, single-strain vaccines based on human RV strains (including neonatal strains): HRV (Rotarix), Rotavin-M1, 116E (Rotavac, a naturally occurring human-bovine reassortant) and RV3-BB;
Table 1. Characteristics of rotavirus single-strain vaccines based on neonatal or live-attenuated human RV strains
-: oral, live-attenuated, single-strain vaccine based on animal RV strains: Lanzhou lamb rotavirus vaccine (LLR);
Table 2. Characteristics of rotavirus single-strain vaccines based on live-attenuated animal RV strains
-: oral, live-attenuated, single- or multi-strain vaccines based on animal-human reassortant RV strains: HBRV (RotaTeq), Bovine Rotavirus Pentavalent BRV-PV (Rotasiil), tetravalent UK-BRV, hexavalent UK-BRV, and pentavalent UK-BRV;
Table 3. Characteristics of rotavirus multi-strain vaccines based on live-attenuated bovine-human reassortant RV strains
-: parenteral, non-live vaccines in early phase of development: inactivated RV vaccine, recombinant proteins, and VLPs.
Table 4. Characteristics of new rotavirus vaccines in early phase development
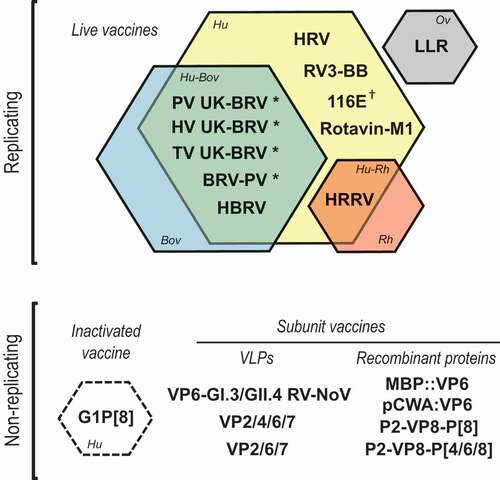
illustrates the landscape of RV vaccines included in this review, specifically vaccine concept and type of strain.
Figure 2. Overview of the rotavirus vaccines included in this review reflecting their vaccine concept and type of strain.
4 Discussion
A great variety of RV vaccines, using different approaches and concepts, have emerged over the last two decades with the common goal of preventing RVGE. As presented in the results section of this literature search (–), each vaccine concept and every vaccine within each concept show different biological properties (e.g. strain type and virus concentration) that may translate into different vaccine characteristics (e.g. dosing schedule, efficacy, effectiveness, and safety profile). A solid understanding of RV vaccine characteristics is therefore essential to support informed health policy decisions in individual countries and clinical practice.
4.1 Vaccine design – oral, live-attenuated, single- and multi-strains
RV vaccines can be of human or animal-human reassortant RV strain origin. In addition, the vaccine can be single-strain (if derived from a single RV strain) or multi-strain (if several strains are combined within a single vaccine). While vaccines designed on single live-attenuated RV strains are based on the observation that a first contact with RV prevents clinical symptoms in subsequent re-infections with the same or different wild-type strains, multi-strain reassorted RV vaccines’ design suggest that exposure to different strains of RV may confer protection against a broad range of circulating RV strains.Citation12,Citation16,Citation17 In this regard, both clinical data and real-world evidence derived from global studies with well-established vaccines have shown that both multi-strain (HBRV) and single-strain (HRV) RV vaccines can protect against several strains of RV.Citation27,Citation28 This broad protection is particularly relevant because RV strain distribution displays seasonal and geographical variations.Citation74,Citation75
Of note, the temporary predominance of the G2P4 strain in countries with high RV vaccination coverage (especially for Rotarix) − in the context of a substantial overall high vaccination coverage-related decrease in RV cases − has prompted scientific discussions regarding its potential emergence due to a link between RV vaccination and the prevalence of non-RV vaccine strains.Citation76,Citation77 However, data gathered so far from global RV surveillance networks support the occurrence of a natural cycling in RV strain distribution and dominant types. Moreover, similar unpredictable changes in strain fluctuations have been reported both in countries with and without routine RV vaccination.Citation78–80 There is therefore a lack of substantial evidence supporting the hypothesis of a shift in RV strain distribution driven by vaccine-induced pressure, and it seems likely that these changes reflect natural fluctuations in RV strains in time and space.Citation28,Citation81 Although these data are reassuring with regards to the circulation of non-vaccine RV strains, the risk of appearance of new RV strains arising from the segmented genome of RV is a strong argument for a continued and efficient epidemiological surveillance of RV strains.Citation82
4.1.1 Single-strain vaccines – neonatal naturally-occurring RV strains
Neonatal strains of RV appear to be naturally attenuated: it was observed that asymptomatically infected neonates had a reduced frequency and severity of RV-associated diarrhea in subsequent RV infections. This led to the exploration of RV neonatal strains as vaccine candidates.Citation17
Rotavac; a naturally occurring human-bovine reassortant neonatal strain
In the early 2000s, two RV strains obtained from asymptomatic-infected newborns in Delhi (strain 116E) and Bangalore (strain I321) were tested as vaccine candidates in India. Each strain appeared to be a naturally occurring human-bovine reassortant: 116E (genotype G9P[11]) is a human RV strain bearing a single gene segment derived from a bovine RV, while I321 (genotype G10P[11]) is a bovine strain with two gene segments derived from a human RV. In a phase I trial, 116E was able to induce a superior immune response compared to I321 and placebo, and was hence selected for further development.Citation83
In 2011, a phase III randomized, double-blind, placebo-controlled trial in India evaluated the safety and efficacy of 3 doses of 116E administered at 6, 10, and 14 weeks of age in more than 6,500 infants. The estimated efficacy of 116E against severe RVGE requiring hospitalization or supervised rehydration was 56% (95% confidence interval [CI] [37%–70%]) in the first year of life and 49% (95% CI [17%–68%]) in the second year of life ().Citation29,Citation31 The occurrence of adverse events was not significantly higher in the vaccine group compared to the placebo group; however, the study had insufficient power to conclude on the occurrence of IS between both groups.
Another study showed no interference of 116E in the immune response of co-administered vaccines routinely included in NIPs, such as oral polio vaccines (OPV) or pentavalent vaccines against diphtheria, pertussis, tetanus, hepatitis B, and Haemophilus influenzae type b.Citation34 The 116E vaccine was licensed in 2014 in India and recently obtained WHO prequalification.Citation35
RV3-BB (naturally attenuated human neonatal strain vaccine; in development)
The human neonatal G3P[6] strain RV3-BB, developed by Murdoch Children’s Research Institute in Australia, was found to replicate well in the newborn gut and to provide protection from severe RVGE.Citation84 These findings have led to a birth dose strategy with the goal of providing early protection against RV. After conclusive phase I results, a phase IIa trial reported RV3-BB to be immunogenic and well tolerated when given according to a 3-dose neonatal or infant schedule ().Citation32,Citation85 More recently, in a phase IIb, randomized, placebo-controlled trial in Indonesia conducted between 2013 and 2016, the vaccine efficacy against severe RVGE was 75% (95% CI [44%–91%]) for infants receiving the neonatal schedule (0 to 5 days, 8 weeks and 14 weeks of age), and 51% (7%–76%) for infants receiving the infant schedule (8 weeks, 14 weeks and 18 weeks of age).Citation37 In this study, a similar safety profile was observed across the neonatal schedule, infant schedule and placebo groups. A phase II dose-ranging study is ongoing in African neonates and infants.Citation86
4.1.2 Single-strain vaccines − human RV strain
HRV (Rotarix)
Rotarix (HRV) is a human RV vaccine composed of a G1P[8] strain obtained from the stool of an infant who experienced natural RV infection in the 1988–1989 RV season in the USA.Citation12 This vaccine was observed to provide protection against severe infections in subsequent RV seasons. The virus was attenuated by cell culture passages, and the final vaccine − obtained at GSK − underwent robust worldwide clinical development (RIX4414, HRV, Rotarix) (). HRV was first registered in Mexico in 2004 and its use has been characterized by extensive post-marketing studies to document safety, effectiveness, and impact.Citation17,Citation38,Citation87 HRV is currently registered worldwide in >100 countries and is WHO prequalified.Citation35,Citation88 The vaccine is administered in 2 doses between the ages of 6 and 24 weeks.Citation19
Rotavin-M1
Rotavin-M1 is a frozen oral vaccine containing a G1P[8] strain obtained from a Vietnamese child (). A dose-escalation study was primarily carried out in a small sample of Vietnamese infants to determine the vaccine dose and schedule. The vaccine formulation eliciting the highest immunoglobulin (Ig)A seroconversion rate (73%, 95%CI [58%‒88%]) was also shown to be well tolerated.Citation30 Although no efficacy results were released, the vaccine was licensed in Vietnam in 2012 based on the immunogenicity data. Since then, the vaccine has only been available on the private market with a 2-dose schedule at 2 and 4 months of age. However, the vaccine is currently being introduced into the Expanded Program on Immunization schedule of selected Vietnamese districts on a pilot basis.Citation26 A phase III immunogenicity trial of a liquid, nonfrozen formulation of the vaccine is also being planned.Citation25,Citation26,Citation30,Citation89
4.1.3 Single-strain RV Vaccines – animal strains
Lanzhou lamb rotavirus vaccine (LLR; lamb-derived RV vaccine)
LLR is a single RV strain G10P[15], lamb-derived, 3-dose vaccine developed and produced by the Lanzhou Institute of Biological Products ().Citation90 The vaccine is licensed in China since 2000, but since it is not part of a nationally funded program, the coverage is relatively low and geographically variable. The dosing schedule is one dose per year from age of 2 months to 3 years.Citation91 Since, to date, no placebo-controlled phase III trial has been conducted, few data are available on the vaccine’s safety, immunogenicity, and efficacy. However, estimates for vaccine effectiveness against RVGE have been provided by several case-control studies, ranging from 35% to 77%.Citation41–44 A recent ecological study conducted during nine seasons revealed an inverse relationship between vaccination coverage and RVGE incidence.Citation91
4.1.4 Multiple-strain RV Vaccines – licensed bovine-human reassortant
HBRV (RotaTeq; pentavalent, bovine-human reassortant, live-attenuated)
RotaTeq (HBRV) is a multi-strain bovine-human reassortant (WC3), developed by Merck & Co, Inc. (). Four reassortant RVs express the VP7 protein (G1, G2, G3, or G4) from the human RV parent strain, and the VP4 protein (P[5]) from the bovine RV parent strain. The fifth reassortant RV contained in the vaccine expresses the VP4 protein (P[8]) from the human RV parent strain and the outer capsid protein (G6) from the bovine RV parent strain.Citation20 As was the case for HRV, HBRV underwent extensive worldwide clinical development followed by large post-licensure studies reporting its positive impact and safety profile.Citation20,Citation39,Citation87 HBRV was licensed in February 2006 by the USA Food and Drug Administration and its administration is routinely recommended according to a 3-dose oral schedule at 2, 4, and 6 months of age. The first dose should be given between 6 and 12 weeks of age, with the two subsequent doses administered at 4–to–10-week intervals before the child reaches the age of 32 weeks.Citation20 Similar to HRV, HBRV is registered worldwide in >100 countries and has been prequalified by the WHO.Citation35,Citation92
BRV-PV (Rotasiil; pentavalent, bovine-human reassortant, live-attenuated)
Rotasiil (BRV-PV) is a multi-strain bovine-human reassortant vaccine containing genotypes G1, G2, G3, G4, and G9 (). The lyophilized presentation is a thermostable vaccine and retains its stability at temperatures up to 25°C for up to 36 months, between 37°C and 40°C for 18 months, and for short time periods over 55°C.Citation50 Two randomized, double-blind, placebo-controlled trials were conducted in Niger and India to evaluate its efficacy. In both trials, healthy infants received three doses of the vaccine or placebo at 6, 10, and 14 weeks of age, along with routine vaccines. The primary efficacy analysis against severe RVGE highlighted a vaccine efficacy of 67% (95% CI [50%–78%]) in Niger and 36% (95% CI [12%–54%]) in India.Citation45,Citation49 Although there was no imbalance in the risk of adverse events across vaccine and placebo groups, these two studies were not powered to detect an increased incidence of rare events, such as IS. A study conducted in India reported that the vaccine does not interfere with the immunogenicity of concomitantly-administered routine pediatric vaccines.Citation93 A liquid formulation of BRV-PV has been developed and recently proved to be non-inferior to the lyophilized formulation.Citation94 The BRV-PV vaccine was licensed in 2017 in India and recently obtained WHO prequalification.Citation35
Multiple-strain RV Vaccines – additional bovine-human reassortant under clinical development
Tetravalent UK-BRV (bovine-human reassortant vaccine candidate)
This vaccine candidate, whose development was initiated by Shantha Biotechnics (India), contains RV strains with VP7 genotypes G1, G2, G3, and G4 (). Its safety and immunogenicity were evaluated in phase I and II studies, in which IgA seroconversion rates for the two highest vaccine titers (105.Citation8 and 106.Citation4 focus forming units [FFU]/mL) after administration of three doses ranged from 52.9% to 83.3%.Citation56 A phase III clinical trial was conducted involving 1,200 Indian infants aged 6–8-weeks to show non-inferiority against a currently licensed vaccine based on immunogenicity, but the study failed to achieve its main endpoint.Citation57 The development of this vaccine is not being pursued any further.Citation25
Pentavalent UK-BRV (bovine-human reassortant vaccine candidate)
Butantan Institute (Brazil) developed a vaccine candidate that contains RV strains with VP7 antigens G1, G2, G3, G4, and G9 (). This vaccine was found to be safe and immunogenic in a phase I trial conducted on 79 adult males.Citation48 However, the vaccine development has been hampered by difficulties to conduct further clinical trials in Brazil, where routinely used HRV has already demonstrated significant benefits with regards to the disease burden.Citation25
Hexavalent UK-BRV (bovine-human reassortant vaccine candidate)
This hexavalent vaccine candidate, currently in development at the Wuhan Institute of Biological Products (WIBP; China), contains the six reassortants developed by the National Institutes of Health (NIH), i.e. G1–4, G8, and G9 ().Citation47 Although a phase I safety trial has been initiated in 2016, no results have been publicly reported yet.Citation25,Citation33
Multiple-Strain RV Vaccines – Additional Lamb-Human Reassortant under Clinical Development (trivalent lamb-derived RV vaccine)
This trivalent genetic reassortant vaccine candidate developed at the WIBP, China, uses the lamb strain from the LLR as a backbone and contains the VP7 antigens G2, G3, and G4. A phase III trial has been underway since 2016 with planned disclosure of results in 2020.Citation25,Citation33
4.2 Vaccine design – parenteral, non-live, RV vaccines
Oral RV vaccines, although successful, display a reduced vaccine efficacy in low-income countries, that hinder their fulfillment worldwide.Citation95 This lower vaccine efficacy is thought to be associated − among other factors − with characteristics of the intestinal tract, including gut microbiota, maternal antibodies, and enteric co-infections, that are known to display population-specific variations.Citation92 By bypassing potential interferences with enteric environment, parenteral vaccines could offer a solution to overcoming the variable levels of vaccine efficacy observed in different target populations. In addition, due to their nature and mode of administration, these vaccines may eliminate risks of vaccine-associated increased IS risk. Moreover, parenteral vaccines have the added benefits that they can be used in combination with other injectable pediatric vaccines and can be produced at relatively low cost.Citation25,Citation26
A parenteral inactivated RV vaccine based on a G1P[8] strain is under development and has been tested in animal models with proven efficacy and heterotypic antibody response ().Citation59,Citation60 An alternative delivery approach using microneedles was also evaluated in mice and piglets.Citation63,Citation64 This preparation is also being considered for use as a combination vaccine with inactivated polio vaccine, and has proven to have no interference in the immune response to either component in mice studies.Citation25,Citation26,Citation96
The subunit vaccine P2-VP8-P[8] () is a parenteral RV vaccine candidate and consists of a truncated VP8 subunit of the rotavirus Wa strain G1P[8] fused with the P2 epitope from tetanus toxin (). After safety was demonstrated in adults,Citation61 the vaccine was assessed in South African toddlers and infants where it was found to be well tolerated, and displayed a strong IgG response (>98% seroconversion in vaccinated infants compared to 9% in infants receiving placebo).Citation62 These study results constituted the basis for a phase I/II trial aiming to assess the safety and immunogenicity of a trivalent subunit vaccine (P2-VP8-P[4]P[6]P[8]) in South African cohorts – the vaccine was shown to be well tolerated with promising anti-P2-VP8 IgG and neutralizing antibody responses among the three vaccine P types.Citation97 A multinational phase IIb/III efficacy trial with active comparator for prevention of severe gastroenteritis in healthy infants is currently under way (NCT04010448).Citation98
Research has also focused on the VP6 protein since it appears to be the most immunogenic and highly conserved protein in Group A RV ().Citation65 The VP6 subunit vaccine stemming from this research was shown to induce RV-specific antibodies and to prevent viral infection in a murine model of rotavirus infection.Citation66,Citation67 Finally, RV-like particles offer a new approach (RV-VLPs) for the development of a subunit RV vaccine. Similarly, a VP6 subunit vaccine, designed as a combination vaccine that incorporates norovirus VLPs (), has already been shown to elicit satisfactory immune responses in mice.Citation70
4.3 Dosing schedules
One notable difference between the vaccines reviewed in this article is the dosing schedule. While most of the RV vaccines (current and future) are administered according to a 3-dose schedule, HRV and Rotavin-M1 follow a 2-dose regimen.Citation33 For HRV, the use of a 2-dose schedule is supported by the dynamics of the immune response following natural infection.Citation99 In clinical trials, a high seroconversion rate was observed after the first dose of the vaccine, whereas the second dose showed a relatively modest additional increase in the seroconversion rate, suggesting that the benefit of a second dose is limited to a catch-up effect.Citation99
Of note, this immune response pattern is likely to correlate with the replication behavior of HRV, which is translated into vaccine antigen excretion ranging from 35% to 44%.Citation12 In contrast, bovine-human reassortant vaccines were shown to have a lower replication rate compared to HRV.Citation15 Based on available published data, bovine-human reassortant vaccines show the greatest increase in seroresponse rates after the third dose, highlighting the importance of a third dose in these vaccines.Citation56 Therefore, the first dose appears to be more important in eliciting a strong immune response for the 2-dose human live-attenuated vaccine than for bovine-human reassortant vaccines.Citation12 The RV3-BB and 116E vaccines are given according to a 3-dose schedule, in contrast with other human live-attenuated vaccines such as HRV and Rotavin-M1. Although all clinical studies of RV3-BB and 116E have been designed using the 3-dose schedule, to date, no rationale or explanation for this schedule have been published.Citation25,Citation26
Another aspect the vaccines differ on is the upper age limit of the vaccination schedule (–). The earliest age by which the vaccination schedule can be completed is 10 weeks of age with HRV.Citation19 This timeline is beneficial as it offers an early protection before the peak of naturally occurring RV infection.Citation100
In addition, early completion of the vaccination could also limit the potential overlap between the natural IS peak and the increased risk of IS following RV vaccination.Citation101,Citation102 However, the implementation of rigid time-restrictions may pose challenges for completion of the schedule, particularly in developing countries where delays in vaccination are common. Analysis of the benefit-risk profile of RV vaccination without age restrictions suggests that in low- and middle-income countries, the additional lives saved by removing age restrictions for RV vaccination would far outnumber the potential excess of vaccine-associated IS deaths.Citation103,Citation104 As a result, and while still promoting timely vaccination, the WHO removed the recommendation of age restriction for rotavirus vaccination in 2013 in order to improve vaccine coverage. However, as most severe cases of RVGE occur earlier in life, RV vaccination of children older than 24 months is not recommended by the WHO.Citation2
Vaccination scheduling is an important factor underlying compliance (adhering to the recommended immunization schedule) and completion (receiving all doses − not necessarily on schedule) of vaccination, which can greatly affect vaccine coverage. Coverage, in turn, has a substantial effect on the impact of RV vaccination, with greater reductions in the number of RV-positive samples and in RVGE hospitalizations in regions where coverage is higher.Citation105,Citation106 The LLR and BRV-PV vaccines have the broadest schedules, spread over 36 months for LLR, and with a maximum age of completion of 24 months for BRV-PV.Citation50 While these extended limits may help to ensure completion of the schedule and improve coverage, they need to be carefully evaluated in terms of benefit-risk profile and real value of vaccination. Interestingly, studies carried out based on databases report higher compliance and completion for 2-dose schedule compared to 3-dose regimen.Citation107,Citation108
4.4 Efficacy, effectiveness and impact
A correlate of protection for RVGE would facilitate timely evaluation of vaccination strategies and the next generation of RV vaccines.Citation109 There are no established correlates of protection for RV vaccines to date – only a surrogate marker of efficacy exists for HRV.Citation11,Citation110 Consequently, RV vaccines can only be licensed based on clinical efficacy data (see –). However, several studies have identified that post-vaccination anti-RV IgA seropositivity (i.e. antibody concentration ≥20 units/mL) may serve as a useful correlate of efficacy in clinical trials on the HRV (Rotarix) vaccine,Citation109,Citation111 with IgA seroconversion conferring substantial protection against any severe RVGE up to the age of one year.Citation112
The real-world use of the well-established HRV and HBRV vaccines has generated a great wealth of efficacy, effectiveness, and impact data. This includes data in pre-term, low birth weight infants, and other at-risk populations such as human immunodeficiency-virus (HIV)-infected or malnourished children.Citation13,Citation36,Citation38,Citation88,Citation95,Citation113–120 In contrast, to date, many of the locally marketed or recently launched vaccines have a limited record of efficacy and/or effectiveness data in global settings. Some of these vaccines with limited global experience data, namely 116E and BRV-PV (both locally manufactured), have received WHO prequalification, allowing accelerated introduction of RV vaccination in high-mortality countries (with the additional support of GAVI, PATH, and UNICEF). However, collection and analysis of post-licensure data through an active surveillance system will be critical to assess the safety and effectiveness of these vaccines. In the case of local vaccines in use for several years (e.g. LLR in China and Rotavin-M1 in Vietnam), the establishment and maintenance of national databases accurately recording health outcomes for RVGE following vaccine implementation would be beneficial in providing estimates of vaccine effectiveness in real-world settings and information about the safety profile of those vaccines (see safety section below).
As previously mentioned, current RV vaccines (namely HRV and HBRV) show higher efficacy in high-income countries compared to low-income countries (–). Although this phenomenon is commonly observed for oral vaccines, such as cholera or polio vaccines, the exact causes underlying this trend remain unclear.Citation121 However, despite their lower efficacy, both HRV and HBRV vaccines have shown substantial real-world impact in developing countries where a high disease burden is present.Citation36 Candidate RV vaccines based on non-oral approaches (e.g. parenterally administered recombinant proteins and VLPs)Citation25,Citation26 provide potential pathways into increasing vaccine efficacy in developing countries.
While not yet reported for new vaccines, immunization with HRV and HBRV has shown to provide substantial indirect benefits (community or herd protection) in some high- and middle-income countries, where the RV-related hospitalization of children too old to receive the vaccine decreased by 24%–89% upon implementation of RV immunization programs.Citation88,Citation122–127 Community protection associated with RV vaccination is most prominent in the first 3 years of a child’s life, however, children who are too young to receive the vaccine may also benefit from this protection.
In addition, there is evidence for RV vaccination having a positive impact on nosocomial infections and providing benefits with regards to health economics outcomes, particularly HRV and HBRV.Citation113,Citation128–130 More recently, the possibly positive impact of RV vaccination on type 1 diabetes and celiac disease, as well as its contribution in reducing childhood seizure hospitalization risk, were documented.Citation131–133 In the context of new RV vaccines, evidence for such indirect effects should also be explored. Recent health economics analyses (cost-effectiveness evaluations) have been generated for 116E and BRV-PV.Citation134
4.5 Safety
The history of RV vaccine development has been greatly influenced by the withdrawal of the HRRV vaccine due to its association with IS, a naturally occurring rare event in infants mostly between 4 and 10 months of age.Citation18 As the increased risk of IS following RV vaccination is very low, it was not detected in pre-licensure studies but only after marketing authorization. Following this incident, a thorough safety evaluation − especially regarding IS − was required for all second-generation RV vaccines.Citation135 In addition, extensive post-marketing surveillance assessments of IS-related risks were also requested by regulatory bodies.Citation136
The background incidence of IS following RV vaccination in infants <1 year of age ranges from 25 to 101 per 100,000 infants per year in developed countries (data from USA and Australia), with a mean incidence of 74 per 100,000 infant per year (data from 35 studies).Citation137,Citation138 Although the risk of IS was not identified in large pre-licensure clinical trials with HRV and HBRV,Citation21,Citation22,Citation139 post-marketing surveillance studies have suggested the existence of a class effect for both vaccines, albeit much lower than for HRRV.Citation140–142 According to data from observational safety studies, administration of these vaccines can result in up to six additional cases of IS per 100,000 infants, especially during the 7 days following the first dose.Citation141
According to the 2018 updated WHO Global Advisory Committee on Vaccine Safety (GAVCS) report − despite the small risk of IS associated with RV vaccines − the safety profile of HRV and HBRV is acceptable, with the benefits of vaccination largely exceeding its risks. Moreover, for new vaccines such as BRV-PV and 116E, the benefit-risk profile remains in favor of RV vaccination although the need for further follow-up studies on newer vaccines was highlighted in this report.Citation143,Citation144
In this context and as mentioned above (see section 3. dosing schedule), the timing of vaccine administration remains an important feature to consider. Indeed, the earlier the vaccines are administered, the lower the expected risk of IS. Schedule compliance, and ensuring that doses are given as early as possible within the recommended timeframe, are therefore key to minimizing the overall risk of IS.Citation101,Citation102 Taking this into account, implementing neonatal or early schedules (when susceptibility to IS is low) for oral, live RV vaccines could potentially decrease the risk of IS associated with RV vaccination.
Mass administration of RV vaccines has not been associated with a general increase in the incidence of IS in countries where this has been monitored.Citation145–148 In addition, a non-significant decrease in IS has recently been documented during a 2-year follow-up of children who completed the RV vaccination.Citation146,Citation149,Citation150 If this trend on the overall incidence of IS in RV-vaccinated cohorts is confirmed by additional studies, the benefit-risk profile of RV vaccination may be even more positive.
While the safety profile with regards to IS and other adverse events (including real-world data) has been characterized in detail for the well-established vaccines HRV and HBRV, there are limited real-world safety data of recently licensed and currently unlicensed RV vaccines. The phase II trials of RV3-BB showed a similar safety profile (including the absence of increased frequencies of fever or gastrointestinal symptoms) in the vaccine groups compared with the placebo group.Citation32,Citation37 Rotavin-M1 demonstrated a similar adverse events profile to HRV in a phase I–II adaptative trial, with the most frequently reported adverse events being irritability and fever.Citation30 For LLR, available evidence is limited to effectiveness data, and no safety data in English-language peer-reviewed scientific journals have been released so far.Citation41–44 The incidence of adverse events and serious adverse events was comparable between 116E and placebo receivers in a key phase III trial,Citation29,Citation31 and an extensive analysis of IS cases from this trial did not suggest the existence of a link between 116E vaccination and increased IS incidence.Citation151 BRV-PV vaccination and placebo showed comparable adverse events and serious adverse events profiles in recent trials conducted in Niger and India, in which no confirmed IS cases IS were reported.Citation45,Citation49 In addition, studies investigating the immunogenicity and safety profile of new RV vaccines, 116E and BRV-PV, have revealed that these vaccines can be safely co-administered with childhood vaccines used in NIPs.Citation34,Citation93
Safety results derived from placebo-controlled trials need to be taken with caution as such studies are not powered to detect (and exclude) the potential risk of infrequent adverse events, such as IS. Large post-marketing studies and good-quality safety databases, such as the ones used to assess the safety of HRV and HBRV, are the most appropriate methods to detect rare events. Self-controlled case series are considered the gold standard to identify the risk of adverse events in a defined time frame with a very low incidence, such as IS.Citation152
Safety of HRV and HRBV has also been evaluated in special populations, in which the risk of wild-type RV infection is increased. While both vaccines have an established safety profile in pre-term infants,Citation120 one of the main concerns in pre-term infants and in immunocompromised children is the risk of vaccine virus shedding, which may lead to nosocomial transmission.Citation153 However, delaying vaccination until hospital discharge has its own risks, and hence opinions and guidelines on the optimal timing of vaccination is such populations differ.Citation154,Citation155 Both HRV and HBRV were found to be safe for use in HIV-infected children with asymptomatic/mildly symptomatic disease (clinical stages I and II according to WHO classification)Citation156 or under antiretroviral therapy, without any evidence for vaccine virus shedding.Citation157–159 HBRV was also well tolerated in children with congenital or acquired intestinal disease requiring resection, administration was well tolerated.Citation160 In infants with intestinal failure, rotavirus vaccination with HRV was also found to be safe and immunogenic.Citation161 Data for such population is not available any of the other vaccines licensed or in development.
In this context, introducing and maintaining high-quality post-licensure surveillance systems (for both vaccine safety and circulating strains) is a fundamental point with respect to safety monitoring, especially in certain developing countries.
5 Conclusion
More than a decade after HRV and HBRV were licensed, the current environment of RV vaccination shows an expanding and varied landscape, with new vaccines being licensed in local markets and other vaccine candidates being in preclinical or clinical stages of development. Despite the differences in RV vaccines, there is early evidence that they may all be effective in preventing and reducing the burden of RVGE. Healthcare professionals, National Immunization Technical Advisory Groups and public health authorities will play an important role in evaluating the overall benefits of each vaccine from the perspective of individual national vaccination programs and recommending the best choice depending upon their use i.e. in private clinic or NIP use. When implementing vaccination policies, it is crucial to look beyond affordability of the vaccine and to carefully consider other aspects, such as compliance, ease of administration, ease of scheduling with other routine pediatric vaccines and safety. In addition, it is crucial for new vaccines to demonstrate similar or improved profiles compared to existing vaccines, thereby establishing a favorable safety risk profile and improving the trust of the target population toward RV immunization programs. Furthermore, considering that RV vaccination coverage is relatively low at the moment in developing countries where it is the most needed, it is essential for new vaccines to increase their accessibility and affordability. More generally, promoting compliance and completion of vaccination schedules may also key be in improving coverage and boosting the impact of vaccines. Although the path to controlling RV disease is still paved with challenges, recent advances in the field of RV vaccination offer a promising stepping stone toward this ambitious goal.
Contributorship
All authors participated in the preparation of the article and have approved the final version of the manuscript.
Trademark statements
Rotarix is a trademark owned by or licensed to the GSK group of companies. RotaTeq is a trademark of Merck & Co., Inc. Rotavac is a trademark of Bharat Biotech. Rotavin-M1 is a trademark of Polyvac. Lanzhou lamb rotavirus vaccine is a trademark of Lanzhou Institute of Biomedical Products. Rotasiil is a trademark of Serum Institute of India. Rotashield is a trademark of Wyeth.
Acknowledgments
The authors thank the Modis platform (Modis, Wavre, Belgium c/o GSK) for providing medical writing services and Emmanuelle Ghys, PhD (Modis, Wavre, Belgium c/o GSK) for editorial support and publication management.
Disclosure of potential conflicts of interest
Bernd Benninghoff, Serge Debrus, Priya Pereira and Volker Vetter are employed by and hold shares in the GSK group of companies. Robert C. Gardner was employed by the GSK group of companies during the conduct of this study and has no non-financial interest to declare.
Additional information
Funding
References
- Chen S-C, Tan L-B, Huang L-M, Chen K-T. Rotavirus infection and the current status of rotavirus vaccines. Journal of the Formosan Medical Association. 2012;111(4):183–17. doi:10.1016/j.jfma.2011.09.024.
- World Health Organization. Rotavirus vaccines - WHO position paper – january 2013. Wkly Epidemiol Rec. 2013;88(5):49–64. doi:10.1016/j.jfma.2011.09.024.
- Crawford SE, Ramani S, Tate JE, Parashar UD, Svensson L, Hagbom M. Rotavirus infection. Nat Rev Dis Primers. 2017;3:17083. doi:10.1038/nrdp.2017.83.
- Sengupta P. Rotavirus: the challenges ahead. Indian J Community Med. 2009;34(4):279–82. doi:10.4103/0970-0218.58382.
- Troeger C, Khalil IA, Rao PC, Cao S, Blacker BF, Ahmed T. Rotavirus vaccination and the global burden of rotavirus diarrhea among children younger than 5 years. JAMA Pediatr. 2018;172(10):958–65. doi:10.1001/jamapediatrics.2018.1960.
- World Health Organization. Rotavirus vaccines. WHO position paper – december 2009. Wkly Epidemiol Rec. 2009;84(50):533–40. doi:10.1001/jamapediatrics.2018.1960.
- Tate JE, Burton AH, Boschi-Pinto C, Parashar UD. World health organization-coordinated global rotavirus surveillance N. Global, regional, and national estimates of rotavirus mortality in children <5 years of age, 2000-2013. Clin Infect Dis. 2016;62(Suppl 2):S96–S105. doi:10.1093/cid/civ1013.
- Desselberger U. Rotaviruses. Virus Res. 2014;190:75–96. doi:10.1016/j.virusres.2014.06.016.
- Parashar UD. Rotavirus. Emerg Infect Dis. 1998;4(4):561–70. doi:10.3201/eid0404.980406.
- Gentsch JR, Laird AR, Bielfelt B, Griffin DD, Banyai K, Ramachandran M. Serotype diversity and reassortment between human and animal rotavirus strains: implications for rotavirus vaccine programs. J Infect Dis. 2005;192(Suppl 1):S146–159. doi:10.1086/431499.
- Desselberger U, Huppertz HI. Immune responses to rotavirus infection and vaccination and associated correlates of protection. J Infect Dis. 2011;203(2):188–95. doi:10.1093/infdis/jiq031.
- O’Ryan M. Rotarix (RIX4414): an oral human rotavirus vaccine. Expert Rev Vaccines. 2007;6(1):11–19. doi:10.1586/14760584.6.1.11.
- Tate JE, Patel MM, Steele AD, Gentsch JR, Payne DC, Cortese MM. Global impact of rotavirus vaccines. Expert Rev Vaccines. 2010;9(4):395–407. doi:10.1586/erv.10.17.
- Yen C, Tate JE, Hyde TB, Cortese MM, Lopman BA, Jiang B. Rotavirus vaccines: current status and future considerations. Hum Vaccin Immunother. 2014;10(6):1436–48. doi:10.4161/hv.28857.
- Angel J, Franco MA, Greenberg HB. Rotavirus vaccines: recent developments and future considerations. Nat Rev Microbiol. 2007;5(7):529–39. doi:10.1038/nrmicro1692.
- Velazquez FR, Matson DO, Calva JJ, Guerrero L, Morrow AL, Carter-Campbell S, Glass RI, Estes MK, Pickering LK, Ruiz-Palacios GM. Rotavirus infection in infants as protection against subsequent infections. N Engl J Med. 1996;335(14):1022–28. doi:10.1056/NEJM199610033351404.
- Dennehy PH. Rotavirus vaccines: an overview. Clin Microbiol Rev. 2008;21(1):198–208. doi:10.1128/CMR.00029-07.
- Delage G. Rotavirus vaccine withdrawal in the United states; the role of postmarketing surveillance. Can J Infect Dis. 2000;11(1):10–12. doi:10.1155/2000/414396.
- European Medicines Agency. Rotarix® Summary of product characteristics, 11/ 05/2017update. [ accessed November, 2020]. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000639/WC500054789.pdf
- European Medicines Agency. RotaTeq summary of product characteristics, 30/ 05/2017update. [ accessed November, 2020]. http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000669/WC500054185.pdf
- Ruiz-Palacios GM, Perez-Schael I, Velazquez FR, Abate H, Breuer T, Clemens SC. Safety and efficacy of an attenuated vaccine against severe rotavirus gastroenteritis. N Engl J Med. 2006;354(1):11–22. doi:10.1056/NEJMoa052434.
- Vesikari T, Matson DO, Dennehy P, Van Damme P, Santosham M, Rodriguez Z. Safety and efficacy of a pentavalent human-bovine (WC3) reassortant rotavirus vaccine. N Engl J Med. 2006;354(1):23–33. doi:10.1056/NEJMoa052664.
- International Vaccine Access Center (IVAC) JHBSoPH. VIEW-hub RV- Vaccine introduction: current dosing schedule. 2020.[ accessed December, 2019]. https://view-hub.org/map/?set=current-dosing-schedule&group=vaccine-introduction&category=rv
- Centers for Disease Control and Prevention. Vaccines and preventable diseases: routine vaccine recommendations. [ accessed November, 2020]. https://www.cdc.gov/vaccines/vpd/rotavirus/hcp/recommendations.html
- Kirkwood CD, Ma LF, Carey ME, Steele AD. The rotavirus vaccine development pipeline. Vaccine. 2019;37(50):7328–35. doi:10.1016/j.vaccine.2017.03.076.
- Burke RM, Tate JE, Kirkwood CD, Steele AD, Parashar UD. Current and new rotavirus vaccines. Curr Opin Infect Dis. 2019;32(5):435–44. doi:10.1097/QCO.0000000000000572.
- De Vos B, Han HH, Bouckenooghe A, Debrus S, Gillard P, Ward R. Live attenuated human rotavirus vaccine, RIX4414, provides clinical protection in infants against rotavirus strains with and without shared G and P genotypes: integrated analysis of randomized controlled trials. Pediatr Infect Dis J. 2009;28(4):261–66. doi:10.1097/INF.0b013e3181907177.
- Leshem E, Lopman B, Glass R, Gentsch J, Banyai K, Parashar U. Distribution of rotavirus strains and strain-specific effectiveness of the rotavirus vaccine after its introduction: a systematic review and meta-analysis. Lancet Infect Dis. 2014;14(9):847–56. doi:10.1016/s1473-3099(14)70832-1.
- Bhandari N, Rongsen-Chandola T, Bavdekar A, John J, Antony K, Taneja S. Efficacy of a monovalent human-bovine (116E) rotavirus vaccine in indian infants: a randomised, double-blind, placebo-controlled trial. Lancet. 2014;383(9935):2136–43. doi:10.1016/S0140-6736(13)62630-6.
- Dang DA, Nguyen VT, Vu DT, Nguyen TH, Nguyen DM, Yuhuan W. A dose-escalation safety and immunogenicity study of a new live attenuated human rotavirus vaccine (Rotavin-M1) in Vietnamese children. Vaccine. 2012;30(Suppl 1):A114–121. doi:10.1016/j.vaccine.2011.07.118.
- Bhandari N, Rongsen-Chandola T, Bavdekar A, John J, Antony K, Taneja S. Efficacy of a monovalent human-bovine (116E) rotavirus vaccine in indian children in the second year of life. Vaccine. 2014;32(Suppl 1):A110–116. doi:10.1016/j.vaccine.2014.04.079.
- Bines JE, Danchin M, Jackson P, Handley A, Watts E, Lee KJ. Safety and immunogenicity of RV3-BB human neonatal rotavirus vaccine administered at birth or in infancy: a randomised, double-blind, placebo-controlled trial. Lancet Infect Dis. 2015;15(12):1389–97. doi:10.1016/s1473-3099(15)00227-3.
- Deen J, Lopez AL, Kanungo S, Wang XY, Anh DD, Tapia M. Improving rotavirus vaccine coverage: can newer-generation and locally produced vaccines help? Hum Vaccin Immunother. 2018;14(2):495–99. doi:10.1080/21645515.2017.1403705.
- Chandola TR, Taneja S, Goyal N, Antony K, Bhatia K, More D. ROTAVAC® does not interfere with the immune response to childhood vaccines in indian infants: A randomized placebo controlled trial. Heliyon. 2017;3(5):e00302–e00302. doi:10.1016/j.heliyon.2017.e00302.
- World Health Organization. WHO prequalified vaccines. [ accessed November, 2020]. https://extranet.who.int/gavi/PQ_Web/Browse.aspx?nav=3
- Velazquez RF, Linhares AC, Munoz S, Seron P, Lorca P, DeAntonio R. Efficacy, safety and effectiveness of licensed rotavirus vaccines: a systematic review and meta-analysis for Latin America and the Caribbean. BMC Pediatr. 2017;17(1):14. doi:10.1186/s12887-016-0771-y.
- Bines JE, At Thobari J, Satria CD, Handley A, Watts E, Cowley D. Human neonatal rotavirus vaccine (RV3-BB) to target rotavirus from Birth. N Engl J Med. 2018;378(8):719–30. doi:10.1056/NEJMoa1706804.
- Willame C, Vonk Noordegraaf-Schouten M, Gvozdenovic E, Kochems K, Oordt-Speets A, Praet N. Effectiveness of the oral human attenuated rotavirus vaccine: A systematic review and meta-analysis-2006-2016. Open Forum Infect Dis. 2018;5(11):ofy292. doi:10.1093/ofid/ofy292.
- Jonesteller CL, Burnett E, Yen C, Tate JE, Parashar UD. Effectiveness of rotavirus vaccination: A systematic review of the first decade of global postlicensure data, 2006-2016. Clin Infect Dis. 2017;65(5):840–50. doi:10.1093/cid/cix369.
- Reddy S, Nair NP, Giri S, Mohan VR, Tate JE, Parashar UD. Safety monitoring of ROTAVAC vaccine and etiological investigation of intussusception in India: study protocol. BMC Public Health. 2018;18(1):898. doi:10.1186/s12889-018-5809-7.
- Fu C, He Q, Xu J, Xie H, Ding P, Hu W. Effectiveness of the Lanzhou lamb rotavirus vaccine against gastroenteritis among children. Vaccine. 2012;31(1):154–58. doi:10.1016/j.vaccine.2012.10.078.
- Fu C, Wang M, Liang J, He T, Wang D, Xu J. Effectiveness of Lanzhou lamb rotavirus vaccine against rotavirus gastroenteritis requiring hospitalization: a matched case-control study. Vaccine. 2007;25(52):8756–61. doi:10.1016/j.vaccine.2007.10.036.
- Fu C, Tate JE, Jiang B. Effectiveness of Lanzhou lamb rotavirus vaccine against hospitalized gastroenteritis: further analysis and update. Hum Vaccin. 2010;6(11):953. doi:10.4161/hv.6.11.12847.
- Zhen SS, Li Y, Wang SM, Zhang XJ, Hao ZY, Chen Y. Effectiveness of the live attenuated rotavirus vaccine produced by a domestic manufacturer in China studied using a population-based case-control design. Emerg Microbes Infect. 2015;4(1):e64. doi:10.1038/emi.2015.64.
- Isanaka S, Guindo O, Langendorf C, Matar Seck A, Plikaytis BD, Sayinzoga-Makombe N. Efficacy of a low-cost, heat-stable oral rotavirus vaccine in Niger. N Engl J Med. 2017;376(12):1121–30. doi:10.1056/NEJMoa1609462.
- Zade JK, Kulkarni PS, Desai SA, Sabale RN, Naik SP, Dhere RM. Bovine rotavirus pentavalent vaccine development in India. Vaccine. 2014;32(Suppl 1):A124–128. doi:10.1016/j.vaccine.2014.03.003.
- Kapikian AZ, Simonsen L, Vesikari T, Hoshino Y, Morens DM, Chanock RM. A hexavalent human rotavirus-bovine rotavirus (UK) reassortant vaccine designed for use in developing countries and delivered in a schedule with the potential to eliminate the risk of intussusception. J Infect Dis. 2005;192(Suppl 1):S22–29. doi:10.1086/431510.
- Luna EJ, Frazatti-Gallina NM, Timenetsky MC, Cardoso MR, Veras MA, Miraglia JL. A phase I clinical trial of a new 5-valent rotavirus vaccine. Vaccine. 2013;31(7):1100–05. doi:10.1016/j.vaccine.2012.12.020.
- Kulkarni PS, Desai S, Tewari T, Kawade A, Goyal N, Garg BS. A randomized Phase III clinical trial to assess the efficacy of a bovine-human reassortant pentavalent rotavirus vaccine in Indian infants. Vaccine. 2017;35(45):6228–37. doi:10.1016/j.vaccine.2017.09.014.
- Skansberg A, Sauer M, Tan M, Santosham M, Jennings MC. Product review of the rotavirus vaccines ROTASIIL, ROTAVAC, and Rotavin-M1. Hum Vaccin Immunother. 2020:1–12. doi:10.1080/21645515.2020.1804245.
- Armah GE, Sow SO, Breiman RF, Dallas MJ, Tapia MD, Feikin DR. Efficacy of pentavalent rotavirus vaccine against severe rotavirus gastroenteritis in infants in developing countries in sub-Saharan Africa: a randomised, double-blind, placebo-controlled trial. Lancet. 2010;376(9741):606–14. doi:10.1016/s0140-6736(10)60889-6.
- Breiman RF, Zaman K, Armah G, Sow SO, Anh DD, Victor JC. Analyses of health outcomes from the 5 sites participating in the Africa and Asia clinical efficacy trials of the oral pentavalent rotavirus vaccine. Vaccine. 2012;30(Suppl 1):A24–29. doi:10.1016/j.vaccine.2011.08.124.
- Zaman K, Dang DA, Victor JC, Shin S, Yunus M, Dallas MJ. Efficacy of pentavalent rotavirus vaccine against severe rotavirus gastroenteritis in infants in developing countries in Asia: a randomised, double-blind, placebo-controlled trial. Lancet. 2010;376(9741):615–23. doi:10.1016/s0140-6736(10)60755-6.
- Block SL, Vesikari T, Goveia MG, Rivers SB, Adeyi BA, Dallas MJ. Efficacy, immunogenicity, and safety of a pentavalent human-bovine (WC3) reassortant rotavirus vaccine at the end of shelf life. Pediatrics. 2007;119(1):11–18. doi:10.1542/peds.2006-2058.
- Vesikari T, Itzler R, Matson DO, Santosham M, Christie CD, Coia M. Efficacy of a pentavalent rotavirus vaccine in reducing rotavirus-associated health care utilization across three regions (11 countries). Int J Infect Dis. 2007;11(Suppl 2):S29–35. doi:10.1016/s1201-9712(07)60019-8.
- Dhingra MS, Kundu R, Gupta M, Kanungo S, Ganguly N, Singh MP. Evaluation of safety and immunogenicity of a live attenuated tetravalent (G1-G4) Bovine-Human Reassortant Rotavirus vaccine (BRV-TV) in healthy Indian adults and infants. Vaccine. 2014;32(Suppl 1):A117–123. doi:10.1016/j.vaccine.2014.03.069.
- Saluja T, Palkar S, Misra P, Gupta M, Venugopal P, Sood AK. Live attenuated tetravalent (G1-G4) bovine-human reassortant rotavirus vaccine (BRV-TV): randomized, controlled phase III study in Indian infants. Vaccine. 2017;35(28):3575–81. doi:10.1016/j.vaccine.2017.05.019.
- Belongia EA, Irving SA, Shui IM, Kulldorff M, Lewis E, Yin R. Real-time surveillance to assess risk of intussusception and other adverse events after pentavalent, bovine-derived rotavirus vaccine. Pediatr Infect Dis J. 2010;29(1):1–5. doi:10.1097/INF.0b013e3181af8605.
- Jiang B, Wang Y, Glass RI. Does a monovalent inactivated human rotavirus vaccine induce heterotypic immunity? evidence from animal studies. Hum Vaccin Immunother. 2013;9(8):1634–37. doi:10.4161/hv.24958.
- Wang Y, Azevedo M, Saif LJ, Gentsch JR, Glass RI, Jiang B. Inactivated rotavirus vaccine induces protective immunity in gnotobiotic piglets. Vaccine. 2010;28(33):5432–36. doi:10.1016/j.vaccine.2010.06.006.
- Fix AD, Harro C, McNeal M, Dally L, Flores J, Robertson G. Safety and immunogenicity of a parenterally administered rotavirus VP8 subunit vaccine in healthy adults. Vaccine. 2015;33(31):3766–72. doi:10.1016/j.vaccine.2015.05.024.
- Groome MJ, Koen A, Fix A, Page N, Jose L, Madhi SA. Safety and immunogenicity of a parenteral P2-VP8-P[8] subunit rotavirus vaccine in toddlers and infants in South Africa: a randomised, double-blind, placebo-controlled trial. Lancet Infect Dis. 2017;17(8):843–53. doi:10.1016/s1473-3099(17)30242-6.
- Resch TK, Wang Y, Moon -S-S, Joyce J, Li S, Prausnitz M. Inactivated rotavirus vaccine by parenteral administration induces mucosal immunity in mice. Sci Rep. 2018;8(1):561. doi:10.1038/s41598-017-18973-9.
- Wang Y, Vlasova A, Velasquez DE, Saif LJ, Kandasamy S, Kochba E. Skin vaccination against rotavirus using microneedles: proof of concept in gnotobiotic piglets. Plos One. 2016;11(11):e0166038. doi:10.1371/journal.pone.0166038.
- Ward RL, McNeal MM. VP6: A candidate rotavirus vaccine. J Infect Dis. 2010;202(S1):S101–107. doi:10.1086/653556.
- Esteban LE, Temprana CF, Arguelles MH, Glikmann G, Castello AA. Antigenicity and immunogenicity of rotavirus VP6 protein expressed on the surface of Lactococcus lactis. Biomed Res Int. 2013;2013:298598. doi:10.1155/2013/298598.
- Temprana CF, Arguelles MH, Gutierrez NM, Barril PA, Esteban LE, Silvestre D. Rotavirus VP6 protein mucosally delivered by cell wall-derived particles from Lactococcus lactis induces protection against infection in a murine model. PLoS One. 2018;13(9):e0203700. doi:10.1371/journal.pone.0203700.
- Changotra H, Vij A. Rotavirus virus-like particles (RV-VLPs) vaccines: an update. Rev Med Virol. 2017;(6)27. doi:10.1002/rmv.1954.
- Conner ME, Zarley CD, Hu B, Parsons S, Drabinski D, Greiner S. Virus-like particles as a rotavirus subunit vaccine. J Infect Dis. 1996;174(Suppl 1):S88–92. doi:10.1093/infdis/174.supplement_1.s88.
- Lappalainen S, Pastor AR, Malm M, Lopez-Guerrero V, Esquivel-Guadarrama F, Palomares LA. Protection against live rotavirus challenge in mice induced by parenteral and mucosal delivery of VP6 subunit rotavirus vaccine. Arch Virol. 2015;160(8):2075–78. doi:10.1007/s00705-015-2461-8.
- Lappalainen S, Pastor AR, Tamminen K, Lopez-Guerrero V, Esquivel-Guadarrama F, Palomares LA. Immune responses elicited against rotavirus middle layer protein VP6 inhibit viral replication in vitro and in vivo. Hum Vaccin Immunother. 2014;10(7):2039–47. doi:10.4161/hv.28858.
- Tamminen K, Lappalainen S, Huhti L, Vesikari T, Blazevic V. Trivalent combination vaccine induces broad heterologous immune responses to norovirus and rotavirus in mice. PLoS One. 2013;8(7):e70409. doi:10.1371/journal.pone.0070409.
- Azevedo MS, Gonzalez AM, Yuan L, Jeong KI, Iosef C, Van Nguyen T. An oral versus intranasal prime/boost regimen using attenuated human rotavirus or VP2 and VP6 virus-like particles with immunostimulating complexes influences protection and antibody-secreting cell responses to rotavirus in a neonatal gnotobiotic pig model. Clin Vaccine Immunol. 2010;17(3):420–28. doi:10.1128/CVI.00395-09.
- Banyai K, Laszlo B, Duque J, Steele AD, Nelson EA, Gentsch JR. Systematic review of regional and temporal trends in global rotavirus strain diversity in the pre rotavirus vaccine era: insights for understanding the impact of rotavirus vaccination programs. Vaccine. 2012;30(Suppl 1):A122–130. doi:10.1016/j.vaccine.2011.09.111.
- Santos N, Hoshino Y. Global distribution of rotavirus serotypes/genotypes and its implication for the development and implementation of an effective rotavirus vaccine. Rev Med Virol. 2005;15(1):29–56. doi:10.1002/rmv.448.
- Matthijnssens J, Nakagomi O, Kirkwood CD, Ciarlet M, Desselberger U, Van Ranst M. Group A rotavirus universal mass vaccination: how and to what extent will selective pressure influence prevalence of rotavirus genotypes? Expert Rev Vaccines. 2012;11(11):1347–54. doi:10.1586/erv.12.105.
- Kirkwood CD. Genetic and antigenic diversity of human rotaviruses: potential impact on vaccination programs. J Infect Dis. 2010;202(S1):S43–48. doi:10.1086/653548.
- EuroRotaNet Annual Report 2018. Publication of report dated Sept 2019. [ accessed November, 2020]. http://www.eurorotanet.com/wp-content/uploads/2019/09/EuroRotaNet_report-Sept_2019_v1.pdf
- Carvalho-Costa FA, Assis RMS de, Fialho AM, Araujo IT, Silva MF, Gomez MM. The evolving epidemiology of rotavirus A infection in Brazil a decade after the introduction of universal vaccination with Rotarix(R). BMC Pediatr. 2019;19(1):42. doi:10.1186/s12887-019-1415-9.
- Roczo-Farkas S, Cowley D, Bines JE. Australian rotavirus surveillance program: annual report, 2017. Commun Dis Intell. 2018;2019:43. doi:10.33321/cdi.2019.43.28.
- Doro R, Laszlo B, Martella V, Leshem E, Gentsch J, Parashar U. Review of global rotavirus strain prevalence data from six years post vaccine licensure surveillance: is there evidence of strain selection from vaccine pressure? Infect Genet Evol. 2014;28:446–61. doi:10.1016/j.meegid.2014.08.017.
- Usonis V, Ivaskeviciene I, Desselberger U, Rodrigo C. The unpredictable diversity of co-circulating rotavirus types in Europe and the possible impact of universal mass vaccination programmes on rotavirus genotype incidence. Vaccine. 2012;30(31):4596–605. doi:10.1016/j.vaccine.2012.04.097.
- Bhandari N, Sharma P, Glass RI, Ray P, Greenberg H, Taneja S. Safety and immunogenicity of two live attenuated human rotavirus vaccine candidates, 116E and I321, in infants: results of a randomised controlled trial. Vaccine. 2006;24(31–32):5817–23. doi:10.1016/j.vaccine.2006.05.001.
- Bishop RF, Barnes GL, Cipriani E, Lund JS. Clinical immunity after neonatal rotavirus infection. A prospective longitudinal study in young children. N Engl J Med. 1983;309(2):72–76. doi:10.1056/NEJM198307143090203.
- Danchin M, Kirkwood CD, Lee KJ, Bishop RF, Watts E, Justice FA. Phase I trial of RV3-BB rotavirus vaccine: a human neonatal rotavirus vaccine. Vaccine. 2013;31(23):2610–16. doi:10.1016/j.vaccine.2013.04.008.
- A phase II dose-ranging study of oral RV3-BB rotavirus vaccine. [ accessed November, 2020]. https://clinicaltrials.gov/ct2/show/NCT03483116
- Soares-Weiser K, Bergman H, Henschke N, Pitan F, Cunliffe N. Vaccines for preventing rotavirus diarrhoea: vaccines in use. Cochrane Database Syst Rev. 2019:2019. doi:10.1002/14651858.CD008521.pub5.
- Pereira P, Vetter V, Standaert B, Benninghoff B. Fifteen years of experience with the oral live-attenuated human rotavirus vaccine: reflections on lessons learned. Expert Rev Vaccines. 2020;19(8):755–69. doi:10.1080/14760584.2020.1800459.
- ClinicalTrials.gov. Phase III study of liquid formulation of ROTAVIN. 2018.[ accessed November, 2020]. https://clinicaltrials.gov/ct2/show/NCT03703336
- Li D, Xu Z, Xie G, Wang H, Zhang Q, Sun X. [Genotype of rotavirus vaccine strain LLR in China is G10P[15]]. Bing Du Xue Bao. 2015;31(2):170–73. doi:10.1001/jamanetworkopen.2018.1382.
- Fu C, Dong Z, Shen J, Yang Z, Liao Y, Hu W. Rotavirus gastroenteritis infection among children vaccinated and unvaccinated with rotavirus vaccine in Southern China: A population-based assessment. JAMA Netw Open. 2018;1(4):e181382. doi:10.1001/jamanetworkopen.2018.1382.
- Desselberger U. Differences of rotavirus vaccine effectiveness by Country: likely causes and contributing factors. Pathogens. 2017;6(4):65. doi:10.3390/pathogens6040065.
- Desai S, Rathi N, Kawade A, Venkatramanan P, Kundu R, Lalwani SK. Non-interference of bovine-human reassortant pentavalent rotavirus vaccine ROTASIIL® with the immunogenicity of infant vaccines in comparison with a licensed rotavirus vaccine. Vaccine. 2018;36(37):5519–23. doi:10.1016/j.vaccine.2018.07.064.
- Kawade A, Babji S, Kamath V, Raut A, Kumar CM, Kundu R. Immunogenicity and lot-to-lot consistency of a ready to use liquid bovine-human reassortant pentavalent rotavirus vaccine (ROTASIIL - Liquid) in Indian infants. Vaccine. 2019;37(19):2554–60. doi:10.1016/j.vaccine.2019.03.067.
- Burnett E, Parashar U, Tate J. Rotavirus vaccines: effectiveness, safety, and future directions. Paediatr Drugs. 2018;20(3):223–33. doi:10.1007/s40272-018-0283-3.
- Wang Y, Zade J, Moon SS, Weldon W, Pisal SS, Glass RI. Lack of immune interference between inactivated polio vaccine and inactivated rotavirus vaccine co-administered by intramuscular injection in two animal species. Vaccine. 2019;37(5):698–704. doi:10.1016/j.vaccine.2018.12.043.
- Groome MJ, Fairlie L, Morrison J, Fix A, Koen A, Masenya M. Safety and immunogenicity of a parenteral trivalent P2-VP8 subunit rotavirus vaccine: a multisite, randomised, double-blind, placebo-controlled trial. Lancet Infect Dis. 2020;(7). doi:10.1016/s1473-3099(20)30001-3.
- Safety, immunogenicity and efficacy of a trivalent rotavirus P2-VP8 subunit vaccine in prevention of severe rotavirus gastroenteritis in healthy infants in Africa and India. [ accessed November, 2020]. https://www.clinicaltrials.gov/ct2/show/NCT04010448
- Vesikari T, Karvonen A, Korhonen T, Espo M, Lebacq E, Forster J. Safety and immunogenicity of RIX4414 live attenuated human rotavirus vaccine in adults, toddlers and previously uninfected infants. Vaccine. 2004;22(21–22):2836–42. doi:10.1016/j.vaccine.2004.01.044.
- Cunliffe N, Zaman K, Rodrigo C, Debrus S, Benninghoff B, Pemmaraju Venkata S. Early exposure of infants to natural rotavirus infection: a review of studies with human rotavirus vaccine RIX4414. BMC Pediatr. 2014;14(1):295. doi:10.1186/s12887-014-0295-2.
- Koch J, Harder T, von Kries R, Wichmann O. Risk of intussusception after rotavirus vaccination. Dtsch Arztebl Int. 2017;114(15):255–62. doi:10.3238/arztebl.2017.0255.
- Valcarcel Salamanca B, Hagerup-Jenssen ME, Flem E. Uptake and timeliness of rotavirus vaccination in Norway: the first year post-introduction. Vaccine. 2016;34(39):4684–89. doi:10.1016/j.vaccine.2016.08.017.
- Patel MM, Clark AD, Glass RI, Greenberg H, Tate J, Santosham M. Broadening the age restriction for initiating rotavirus vaccination in regions with high rotavirus mortality: benefits of mortality reduction versus risk of fatal intussusception. Vaccine. 2009;27(22):2916–22. doi:10.1016/j.vaccine.2009.03.016.
- Patel MM, Clark AD, Sanderson CF, Tate J, Parashar UD. Removing the age restrictions for rotavirus vaccination: a benefit-risk modeling analysis. PLoS Med. 2012;9(10):e1001330. doi:10.1371/journal.pmed.1001330.
- Dudareva-Vizule S, Koch J, An der Heiden M, Oberle D, Keller-Stanislawski B, Wichmann O. Impact of rotavirus vaccination in regions with low and moderate vaccine uptake in Germany. Hum Vaccin Immunother. 2012;8(10):1407–15. doi:10.4161/hv.21593.
- Steele AD, Groome MJ. Measuring rotavirus vaccine impact in Sub-Saharan Africa. Clin Infect Dis. 2020;70(11):2314–16. doi:10.1093/cid/ciz918.
- Luna-Casas G, Juliao P, Carreno-Manjarrez R, Castaneda-Prado A, Cervantes-Apolinar MY, Navarro-Rodriguez R. Vaccine coverage and compliance in Mexico with the two-dose and three-dose rotavirus vaccines. Hum Vaccin Immunother. 2019;15(6):1251–59. doi:10.1080/21645515.2018.1540827.
- Krishnarajah G, Landsman-Blumberg P, Eynullayeva E. Rotavirus vaccination compliance and completion in a Medicaid infant population. Vaccine. 2015;33(3):479–86. doi:10.1016/j.vaccine.2014.06.059.
- Cheuvart B, Neuzil KM, Steele AD, Cunliffe N, Madhi SA, Karkada N. Association of serum anti-rotavirus immunoglobulin A antibody seropositivity and protection against severe rotavirus gastroenteritis: analysis of clinical trials of human rotavirus vaccine. Hum Vaccin Immunother. 2014;10(2):505–11. doi:10.4161/hv.27097.
- Angel J, Steele AD, Franco MA. Correlates of protection for rotavirus vaccines: possible alternative trial endpoints, opportunities, and challenges. Hum Vaccin Immunother. 2014;10(12):3659–71. doi:10.4161/hv.34361.
- Patel M, Glass RI, Jiang B, Santosham M, Lopman B, Parashar U. A systematic review of anti-rotavirus serum IgA antibody titer as a potential correlate of rotavirus vaccine efficacy. J Infect Dis. 2013;208(2):284–94. doi:10.1093/infdis/jit166.
- Baker JM, Tate JE, Leon J, Haber MJ, Pitzer VE, Lopman BA. Postvaccination serum antirotavirus immunoglobulin A as a correlate of protection against rotavirus gastroenteritis across settings. J Infect Dis. 2020;222(2):309–18. doi:10.1093/infdis/jiaa068.
- Pindyck T, Tate JE, Parashar UD. A decade of experience with rotavirus vaccination in the United States - vaccine uptake, effectiveness, and impact. Expert Rev Vaccines. 2018;17(7):593–606. doi:10.1080/14760584.2018.1489724.
- Goveia MG, Rodriguez ZM, Dallas MJ, Itzler RF, Boslego JW, Heaton PM. Safety and efficacy of the pentavalent human-bovine (WC3) reassortant rotavirus vaccine in healthy premature infants. Pediatr Infect Dis J. 2007;26(12):1099–104. doi:10.1097/INF.0b013e31814521cb.
- Van der Wielen M, Van Damme P. Pentavalent human-bovine (WC3) reassortant rotavirus vaccine in special populations: a review of data from the rotavirus efficacy and safety trial. Eur J Clin Microbiol Infect Dis. 2008;27(7):495–501. doi:10.1007/s10096-008-0479-5.
- J-M R, Nowak E, Le Gal G, Lemaitre T, Oger E, Poulhazan E. Impact of rotavirus vaccine on premature infants. Clinical and Vaccine Immunology: CVI. 2014;21(10):1404–09. doi:10.1128/CVI.00265-14.
- Groome MJ, Zell ER, Solomon F, Nzenze S, Parashar UD, Izu A. Temporal association of rotavirus vaccine introduction and reduction in all-cause childhood diarrheal hospitalizations in South Africa. Clin Infect Dis. 2016;62(Suppl 2):S188–195. doi:10.1093/cid/civ1204.
- Madhi SA, Cunliffe NA, Steele D, Witte D, Kirsten M, Louw C. Effect of human rotavirus vaccine on severe diarrhea in African infants. Malawi Med J. 2016;28(3):108–14. doi:10.1093/cid/civ1204.
- Perez-Schael I, Salinas B, Tomat M, Linhares AC, Guerrero ML, Ruiz-Palacios GM. Efficacy of the human rotavirus vaccine RIX4414 in malnourished children. J Infect Dis. 2007;196(4):537–40. doi:10.1086/519687.
- Esposito S, Pugni L, Mosca F, Principi N. Rotarix® and RotaTeq® administration to preterm infants in the neonatal intensive care unit: review of available evidence. Vaccine. 2018;36(36):5430–34. doi:10.1016/j.vaccine.2017.10.013.
- Patel M, Shane AL, Parashar UD, Jiang B, Gentsch JR, Glass RI. Oral rotavirus vaccines: how well will they work where they are needed most? J Infect Dis. 2009;200(Suppl s1):S39–48. doi:10.1086/605035.
- Field EJ, Vally H, Grimwood K, Lambert SB. Pentavalent rotavirus vaccine and prevention of gastroenteritis hospitalizations in Australia. Pediatrics. 2010;126(3):e506–512. doi:10.1542/peds.2010-0443.
- Safadi MA, Berezin EN, Munford V, Almeida FJ, de Moraes JC, Pinheiro CF. Hospital-based surveillance to evaluate the impact of rotavirus vaccination in Sao Paulo, Brazil. Pediatr Infect Dis J. 2010;29(11):1019–22. doi:10.1097/INF.0b013e3181e7886a.
- Hemming M, Rasanen S, Huhti L, Paloniemi M, Salminen M, Vesikari T. Major reduction of rotavirus, but not norovirus, gastroenteritis in children seen in hospital after the introduction of RotaTeq vaccine into the national immunization programme in Finland. Eur J Pediatr. 2013;172(6):739–46. doi:10.1007/s00431-013-1945-3.
- Paulke-Korinek M, Kundi M, Rendi-Wagner P, de Martin A, Eder G, Schmidle-Loss B. Herd immunity after two years of the universal mass vaccination program against rotavirus gastroenteritis in Austria. Vaccine. 2011;29(15):2791–96. doi:10.1016/j.vaccine.2011.01.104.
- Raes M, Strens D, Vergison A, Verghote M, Standaert B. Reduction in pediatric rotavirus-related hospitalizations after universal rotavirus vaccination in Belgium. Pediatr Infect Dis J. 2011;30(7):e120–125. doi:10.1097/INF.0b013e318214b811.
- Yen C, Armero Guardado JA, Alberto P, Rodriguez Araujo DS, Mena C, Cuellar E. Decline in rotavirus hospitalizations and health care visits for childhood diarrhea following rotavirus vaccination in El Salvador. Pediatr Infect Dis J. 2011;30:S6–S10. doi:10.1097/INF.0b013e3181fefa05.
- Standaert B, Strens D, Alwan A, Raes M. Medium- to long-term impact of rotavirus vaccination on hospital care in Belgium: A 7-year follow-up of the Rotavirus Belgium Impact Study (RotaBIS). Infect Dis Ther. 2016;5(1):31–44. doi:10.1007/s40121-015-0099-1.
- Standaert B, Strens D, Li X, Schecroun N, Raes M. The sustained rotavirus vaccination impact on nosocomial infection, duration of hospital stay, and age: the rotaBIS study (2005-2012). Infect Dis Ther. 2016;5(4):509–24. doi:10.1007/s40121-016-0131-0.
- Zlamy M, Kofler S, Orth D, Wurzner R, Heinz-Erian P, Streng A. The impact of rotavirus mass vaccination on hospitalization rates, nosocomial rotavirus gastroenteritis and secondary blood stream infections. BMC Infect Dis. 2013;13(1):112. doi:10.1186/1471-2334-13-112.
- Burke RM, Tate JE, Dahl RM, Aliabadi N, Parashar UD. Rotavirus vaccination is associated with reduced seizure hospitalization risk among commercially insured US children. Clin Infect Dis. 2018;67(10):1614–16. doi:10.1093/cid/ciy424.
- Hemming-Harlo M, Lahdeaho ML, Maki M, Vesikari T. Rotavirus vaccination does not increase Type 1 diabetes and may decrease celiac disease in children and adolescents. Pediatr Infect Dis J. 2019;38(5):539–41. doi:10.1097/INF.0000000000002281.
- Burke RM, Tate JE, Jiang B, Parashar UD. Rotavirus and Type 1 diabetes-is there a connection? A synthesis of the evidence. J Infect Dis. 2020;222(7):1076–83. doi:10.1093/infdis/jiaa168.
- Pecenka C, Debellut F, Bar-Zeev N, Anwari P, Nonvignon J, Shamsuzzaman M. Re-evaluating the cost and cost-effectiveness of rotavirus vaccination in Bangladesh, Ghana, and Malawi: A comparison of three rotavirus vaccines. Vaccine. 2018;36(49):7472–78. doi:10.1016/j.vaccine.2018.10.068.
- World Health Organization. Guidelines to assure the quality, safety and efficacy of live attenuated rotavirus vaccine. 2007.[ accessed November, 2017]. http://www.who.int/biologicals/publications/trs/areas/vaccines/rotavirus/Annex%203%20rotavirus%20vaccines.pdf
- Lopalco PL, DeStefano F. The complementary roles of Phase 3 trials and post-licensure surveillance in the evaluation of new vaccines. Vaccine. 2015;33(13):1541–48. doi:10.1016/j.vaccine.2014.10.047.
- Jiang J, Jiang B, Parashar U, Nguyen T, Bines J, Patel MM. Childhood intussusception: a literature review. PLoS One. 2013;8(7):e68482. doi:10.1371/journal.pone.0068482.
- Clark AD, Hasso-Agopsowicz M, Kraus MW, Stockdale LK, Sanderson CFB, Parashar UD. Update on the global epidemiology of intussusception: a systematic review of incidence rates, age distributions and case-fatality ratios among children aged <5 years, before the introduction of rotavirus vaccination. Int J Epidemiol. 2019;48(4):1316–26. doi:10.1093/ije/dyz028.
- Cheuvart B, Friedland LR, Abu-Elyazeed R, Han HH, Guerra Y, Verstraeten T. The human rotavirus vaccine RIX4414 in infants: a review of safety and tolerability. Pediatr Infect Dis J. 2009;28(3):225–32. doi:10.1097/INF.0b013e31819715fa.
- Dong R, Yang Y-F, Chen G, Shen Z, Zheng S. Risk of intussusception after rotavirus vaccination: a meta-analysis. Int J Clin Exp Med. 2016;9:1306–13. doi:10.1097/INF.0b013e31819715fa.
- Rosillon D, Buyse H, Friedland LR, Ng SP, Velazquez FR, Breuer T. Risk of intussusception after rotavirus vaccination: meta-analysis of postlicensure studies. Pediatr Infect Dis J. 2015;34(7):763–68. doi:10.1097/INF.0000000000000715.
- Kassim P, Eslick GD. Risk of intussusception following rotavirus vaccination: an evidence based meta-analysis of cohort and case-control studies. Vaccine. 2017;35(33):4276–86. doi:10.1016/j.vaccine.2017.05.064.
- Organization WH. Global advisory committee on vaccine safety, 6-7 December 2017. Wkly Epidemiol Rec. 2018;93(3):17–32.
- Organization WH. Global advisory committee on vaccine safety, 4-5 December 2019. Wkly Epidemiol Rec. 2020;95(4):25–36.
- Burke RM, Tate JE, Dahl RM, Aliabadi N, Parashar UD. Does rotavirus vaccination affect longer-term intussusception risk in US infants? J Pediatric Infect Dis Soc. 2019. doi:10.1093/jpids/piz035.
- Buttery JP, Danchin MH, Lee KJ, Carlin JB, McIntyre PB, Elliott EJ. Intussusception following rotavirus vaccine administration: post-marketing surveillance in the national immunization program in Australia. Vaccine. 2011;29(16):3061–66. doi:10.1016/j.vaccine.2011.01.088.
- Hawken S, Ducharme R, Rosella LC, Benchimol EI, Langley JM, Wilson K. Assessing the risk of intussusception and rotavirus vaccine safety in Canada. Hum Vaccin Immunother. 2017;13(3):703–10. doi:10.1080/21645515.2016.1240846.
- Yen C, Tate JE, Steiner CA, Cortese MM, Patel MM, Parashar UD. Trends in intussusception hospitalizations among US infants before and after implementation of the rotavirus vaccination program, 2000-2009. J Infect Dis. 2012;206(1):41–48. doi:10.1093/infdis/jis314.
- Cho H-K, Hwang SH, Nam HN, Han K, Kim B, Kong I. Incidence of intussusception before and after the introduction of rotavirus vaccine in Korea. PloS One. 2020;15(8):e0238185–e0238185. doi:10.1371/journal.pone.0238185.
- Yen C, Shih SM, Tate JE, Wu FT, Huang YC, Parashar UD. Intussusception-related hospitalizations among infants before and after private market licensure of rotavirus vaccines in Taiwan, 2001-2013. Pediatr Infect Dis J. 2017;36(10):e252–e257. doi:10.1097/INF.0000000000001644.
- John J, Kawade A, Rongsen-Chandola T, Bavdekar A, Bhandari N, Taneja S. Active surveillance for intussusception in a phase III efficacy trial of an oral monovalent rotavirus vaccine in India. Vaccine. 2014;32(Suppl 1):A104–109. doi:10.1016/j.vaccine.2014.03.036.
- Escolano S, Hill C, Tubert-Bitter P. A new self-controlled case series method for analyzing spontaneous reports of adverse events after vaccination. Am J Epidemiol. 2013;178(9):1496–504. doi:10.1093/aje/kwt128.
- Hofstetter AM, Lacombe K, Klein EJ, Jones C, Strelitz B, Jacobson E. Risk of rotavirus nosocomial spread after inpatient pentavalent rotavirus vaccination. Pediatrics. 2018;(1)141. doi:10.1542/peds.2017-1110.
- Pahud B, Pallotto EK. Rotavirus Immunization for hospitalized infants: are we there yet? Pediatrics. 2018;(1)141. doi:10.1542/peds.2017-3499.
- Kilich E, Sadarangani M. Use of rotavirus vaccines in preterm babies on the neonatal unit. Expert Rev Vaccines. 2016;15(12):1463–65. doi:10.1080/14760584.2016.1216318.
- World Health Organization. WHO case definitions of HIV for surveillance and revised clinical staging and immunological classification of HIV-related disease in adults and children. 2007. [ accessed November, 2020]. http://www.who.int/hiv/pub/guidelines/HIVstaging150307.pdf
- Steele AD, Madhi SA, Louw CE, Bos P, Tumbo JM, Werner CM. Safety, reactogenicity, and immunogenicity of human rotavirus vaccine RIX4414 in human immunodeficiency virus-positive infants in South Africa. Pediatr Infect Dis J. 2011;30(2):125–30. doi:10.1097/INF.0b013e3181f42db9.
- Steele AD, De Vos B, Tumbo J, Reynders J, Scholtz F, Bos P. Co-administration study in South African infants of a live-attenuated oral human rotavirus vaccine (RIX4414) and poliovirus vaccines. Vaccine. 2010;28(39):6542–48. doi:10.1016/j.vaccine.2008.08.034.
- Levin MJ, Lindsey JC, Kaplan SS, Schimana W, Lawrence J, McNeal MM. Safety and immunogenicity of a live attenuated pentavalent rotavirus vaccine in HIV-exposed infants with or without HIV infection in Africa. AIDS. 2017;31(1):49–59. doi:10.1097/qad.0000000000001258.
- McGrath EJ, Thomas R, Duggan C, Asmar BI. Pentavalent rotavirus vaccine in infants with surgical gastrointestinal disease. J Pediatr Gastroenterol Nutr. 2014;59(1):44–48. doi:10.1097/MPG.0000000000000361.
- Javid PJ, Sanchez SE, Jacob S, McNeal MM, Horslen SP, Englund JA. The Safety and Immunogenicity of rotavirus vaccination in infants with intestinal failure. J Pediatric Infect Dis Soc. 2014;3(1):57–65. doi:10.1093/jpids/pit060.

