ABSTRACT
Parents have important roles to play for adolescents to get the human papillomavirus (HPV) vaccine, an effective measure in the prevention of cervical and other HPV-related cancers. It is important to understand the intention of parents to have their adolescents vaccinated for optimal uptake of the vaccine in Nigeria. This study investigated the intention of parents in five selected communities to get their adolescents vaccinated with HPV vaccine in Ibadan, Nigeria using the Integrated Behavioral Model (IBM). Cross sectional study design was employed and 678 parents were interviewed. Pearson correlation, chi-square test and multiple regression were used for data analysis at α = 0.05. Mean age of the parents was 42.5 ± 10.0 years and 230(33.9%) were males. Almost all of the parents (96.8%) had the intention to vaccinate their adolescents with HPV vaccine. This intention was significantly correlated with experiential attitude (r = 0.74, p = <.01), instrumental attitude (r = 0.33, p = <.01), injunctive norm (r = 0.39, p = <.01), descriptive norm (r = 0.32, p = <.01), perceived control (r = 0.32, p = <.01) and self-efficacy (r = 0.46, p ≤ .01). A higher proportion of parents older than 65 years significantly had no intention to vaccinate their adolescents with HPV vaccine. Intention to vaccinate adolescents with HPV vaccine was predicted by experiential attitude (OR = 0.88, 95% CI: 0.80–0.95), personal agency (OR = 0.22, 95% CI: 0.15–0.29) and injunctive norm (OR = 0.08, 95% CI: 0.02–0.13). Parental intention to vaccinate adolescents with HPV vaccine was high among the parents in this study. The reluctance of older parents about HPV vaccine for adolescents requires further investigation.
Introduction
The human papillomavirus (HPV) vaccine has been shown to be effective in the prevention of cervical cancer, the second-leading women specific cancer in Nigeria and globally.Citation1–3 The HPV is responsible for almost all the cases of cervical cancerCitation4,Citation5 with the most common means of its transmission being through sexual activity.Citation6 The HPV vaccine is most effective for the prevention of cervical cancer when it is administered before sexual debut.Citation2,Citation7 This validates the recommendation for the administration of the vaccine in early adolescence before the onset of sexual activities.
Adolescents are expectedly still cared for by their parents, who also ensure they remain in good health.Citation6 This may entail taking important health care decisions on behalf of the adolescents at various times with or without their inputCitation8 such as decision about the uptake of the HPV vaccine. Parental involvement in this regard is important to facilitate access to HPV vaccine and it is also an ethical requirement because most adolescents are legal minors in many countries and parents are expected to act on their behalf.Citation9,Citation10 It is therefore apparent that parents have important roles to play for the HPV vaccination of adolescents to be a success.
The HPV vaccine is being introduced gradually in African countries which bear most of the burden of cervical cancer.Citation1 As at 2019, 11 African countries have included the vaccine in their routine vaccination schedule.Citation11 These countries are Botswana, Lesotho, Rwanda, Sao Tome and Principe, Senegal, Seychelles, South Africa, Uganda, Mauritius, Zimbabwe and Tanzania. Each of these countries have better infant vaccination coverage compared with NigeriaCitation12 and it is expected that the introduction of the HPV vaccine should be straightforward in these countries as they can build on their existing vaccination structures. However, despite the impressive to fair infant vaccination coverage, there have been some reports of difficulties in the introduction of the HPV vaccine in some of these countries as a result of misconceptions about the vaccine.Citation13–15 There have also been some concerns and hesitancy about the HPV vaccine in West African countries.Citation16 Nigeria has the highest population of adolescents in Africa, being the most populous country in AfricaCitation17 and has a strong history of vaccine hesitancy.Citation18 All of these factors make behavioral research about HPV vaccination to be important in Nigeria.
HPV vaccine is yet to be included in the routine immunization schedule in Nigeria, although, it was licensed in the country in 2008.Citation19 Only few adolescents have been vaccinated due to the high cost of the vaccine which is out of reach of the average Nigerian family.Citation20 The intention to perform a behavior has been shown to be a good predictor of the actual performance of that behavior.Citation21 Therefore, investigating the intention of Nigerian parents to vaccinate their adolescents with HPV vaccine can give insight into their perception about the vaccine and its acceptability for their adolescents. It can also provide useful information which can be used in the design of the HPV vaccination program with a target for a high uptake of the vaccine when it is rolled out in the future. Earlier research have examined parents’ knowledge and acceptability of the HPV vaccine for their adolescents using non-theory-based approaches.Citation8,Citation22,Citation23 The results obtained from such studies are usually difficult to use in the design of interventions to improve knowledge about the vaccine or improve the acceptability. A theory-based approach can delineate relevant concepts and give concise information that will make the design of interventions more focused and their evaluation easier.
Integrated Behavioral Model
Integrated Behavioral Model (IBM) was developed from the Theory of Reasoned Action (TRA)Citation24and the Theory of Planned Behavior (TPB), with some constructs from the Health Belief Model, Social Cognition Theory and Theory of Interpersonal Behavior.Citation25,Citation26 In the IBM, intention is the most important determinant of behavior. Both TRA and TPB are relevant in many African settings as communal way of living is commonplace and social identity and cultural background have strong influence on behavior.Citation27 Attitude (divided into experiential and instrumental attitudes), perceived norm (made up of injunctive and descriptive norm) and personal agency (consisting of perceived control and self-efficacy) are used to determine the intention to perform a behavior in IBM. Experiential attitude is the feeling associated with the performance of a behavior while instrumental attitude is the attribute that is associated with the performance of a behavior.Citation26 Injunctive norm is what the people in one’s social circle expects of one’s behavior and descriptive norm is what the people in one’s social circle are doing.Citation28 Perceived control refers to the ability to carry out a behavior in the presence of challenges and barriers.Citation29 Personal agency is the self-confidence that one can perform a behavior in the presence of challenges and barriers.Citation30 All these constructs are based on background beliefs of individuals.
The intention to perform a behavior is a proxy for the actual performance of the behavior and it has been demonstrated in parental intention to vaccinate their daughters with HPV vaccine and the actual vaccination among Hispanics in the United States.Citation31 Since the HPV vaccine is yet to be included in the routine vaccination schedule in Nigeria, hence the choice of investigating the parental intention to allow adolescents to take HPV vaccine in this study as we assumed that this should closely predict the actual uptake of this vaccine when the vaccine becomes routine. This study therefore investigated the intention of parents of adolescents in selected communities in Ibadan to vaccinate their adolescents with HPV vaccine using the IBM.
Materials and methods
Study design
This is a part of a larger study that used mixed study design to investigate acceptability of the HPV vaccine for adolescents by stakeholders in Southwest Nigeria. However, the findings from the quantitative data are presented here.
Study site
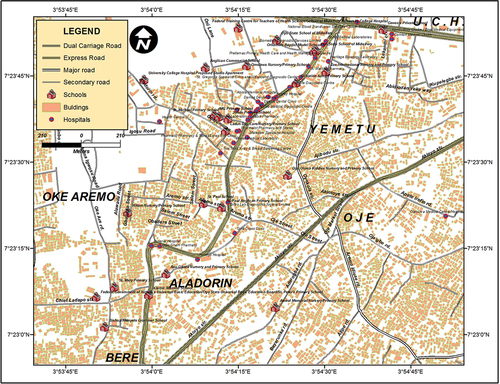
This study was conducted in five communities in Ibadan, a cosmopolitan city located in south western part of Nigeria. The communities are: Aláàádórin, Beere, Òje, Òkè Aremo and Yemetu as shown in . These communities have health development committees that consist of community members who are saddled with the responsibility of health promotion activities in the communities. The committees also liaise with the local government and health care facilities to facilitate health programs in the communites.
Study population
These were parents of adolescents who were residing in the selected communities in Ibadan.
Sample size and sampling
Four focus group discussions were conducted among 38 parents of adolescents to determine the relevant behavioral outcomes, important referents, environmental facilitators and barriers to vaccinating adolescents with HPV vaccine. This number exceeded the recommended minimum of 15 people with potential to perform the behavior of interest for elicitation interviews for the design of surveys using IBM.Citation26
For the household survey, the Kish and Leslie formulaCitation32 was used with 0.70 taken as the proportion of parents who accepted HPV vaccine for their adolescents in an earlier study,Citation22 degree of accuracy of 0.05 and z score of 1.96 at 95% confidence. The calculated sample size was multiplied by an effect factor of two due to the clustering nature of households in the communities and a total of 678 parents of adolescents were selected.
A four-stage sampling technique was used to select participants with the aid of the map of the communities (). The map was divided into four quadrants and seven streets were selected from each quadrant. Subsequently, a compound or household was selected, then a family with at least one adolescent, and lastly, a parent of an adolescent was selected. Only parents who had lived in the study communities for at least a year were eligible for selection. This was to capture the prevailing parental views about the HPV vaccine for adolescents within these communities with as little interference as possible from other communities.
Study questionnaire development
The elicitation interviews were conducted using interview guide based on findings from earlier research and the experiences of the researchers. The guide provided responses about the positive/negative feelings the parents would have if their adolescents get the HPV vaccine (experiential and instrumental attitude); the positive/negative outcomes of getting the vaccine (behavioral beliefs); the individuals who can influence the parents’ decisions to allow their adolescents to take the vaccine or do otherwise (normative referents); and environmental or individual factors that make vaccination of adolescents with HPV vaccine easy or difficult (perceived control and self-efficacy). The questionnaire was developed using the results from the content analysis of these interviews and the questions were designed to provide data about the sociodemographic characteristics and each construct of the IBM. The constructs of the IBM were measured on semantic differential scaleCitation33 to improve the clarity of the questions by clearly defining the connotative meanings of the bipolar adjectives which were used to describe the characteristics of each construct. The first question was about the parents’ intention to have their adolescents take the HPV vaccine. This was followed by questions to test for experiential (seven questions) and instrumental (eight questions) attitudes, injunctive and descriptive norms (12 questions each), perceived control (seven questions) and self-efficacy (seven questions) (Supplementary material). Both content and face validity of the questionnaire were conducted.
Data collection
There were both English and Yoruba versions of the questionnaire and the version used was based on the preference of the participant. Data were collected by trained bilingual research assistants in the homes of the respondents. HPV was introduced as an infection that is mainly transmitted sexually which can result into cervical cancer decades after the infection. The symptomatology of cervical cancer was used to describe the disease instead of the word cervical cancer to ensure the parents understood the disease just as in an earlier study in the study environment.Citation34 The HPV vaccine was introduced as a vaccine that can prevent infection with most strains of HPV and is most effective when given in early adolescence before sexual debut. Parents were also informed that each adolescent will take two doses and each dose will cost 7,000 naira ($19.44) based on the exchange rate at the time of the study. The questionnaire was then administered by the research assistants. All the parents approached agreed to participate in the research but three could not complete the survey as they had to leave to attend to other matters.
Data analysis
Data was analyzed using Statistical Package for Social Sciences version 22.Citation35 Socioeconomic class for the family of the adolescents was determined using a method described by Oyedeji in Nigeria.Citation36 In this method, scores were allotted to the parents’ educational attainments and occupation and the mean of the scores for both parents determined the socioeconomic class with class I as the highest and class V the least. Class I and II were then categorized as high, class III as middle and IV and V as low socioeconomic classes. The differential sematic scale scores for each of the constructs of the IBM were summed and the means were generated to give the mean belief scores. These means were compared using student’s t test for those who had and those who did not have the intention to vaccinate their adolescents with HPV vaccine. Pearson’s correlation was used to determine the relationship between the total score of each component of IBM and intention to vaccinate adolescent with HPV vaccine. The parental factors associated with the intention to vaccinate adolescents with HPV vaccine was then determined by cross tabulating the proportion of parents with the intention to vaccinate or otherwise against selected parental characteristics using chi-square test. The sum of the scores for each construct of the IBM were categorized using the mean as the cut of and the scores that were at the mean and above were categorized as good experiential and instrumental attitudes, good descriptive and injunctive norms and good personal agency, perceived control and self-efficacy. The scores lower than the mean were categorized as poor for all the constructs. Multiple regression analysis was used to predict the intention to vaccinate adolescents using each component of the IBM because there were correlations among the independent variables. The level of significance for all statistical analysis was p < .05.
Ethical considerations
The study protocol was approved by the University of Ibadan/University College Hospital Ethics Commitee. All the study participants gave written informed consent before recruitment into the study. Only codes were used to identify each participant’s questionnaire and they were assured of the anonymity of their responses.
Results
Sociodemographic characteristics
There were 678 parents of adolescents in this study and 230(33.9%) were males. Their mean age was 42.5 ± 10.0 years and 21(3.1%) were more than 65 years old. The other sociodemographic characteristics is as shown in .
Table 1. Sociodemographic characteristics of the parents of adolescents in selected communities in Ibadan.
Intention to vaccinate adolescents with HPV vaccine and mean belief scores of IBM constructs
Among these parents, 656(96.8%) had the intention of getting HPV vaccine for their adolescents. All the sentences used to elicit experiential attitude strongly correlated with the intention to vaccinate adolescents with HPV vaccine except the sentence “I will be afraid if my adolescent is to have HPV vaccine” which had a weak correlation and a negative mean belief score for both parents who intended to, and those who had no intention to vaccinate their adolescents with HPV vaccine. The parents with intention to vaccinate their adolescents significantly had higher mean belief scores for experiential attitude than those who did not want to vaccinate their adolescents. Similar findings were seen in instrumental attitude but the mean belief score for “Adolescents will become infertile if they get HPV vaccine” and “Adolescents will become promiscuous if they get HPV vaccine” had negative mean belief scores for both group of parents. There was no difference in the mean belief of the parents with regard to the statement which stated that HPV vaccine would make adolescents promiscuous, but those who had the intention to vaccinate their adolescents significantly had negative mean belief regarding the statement about the vaccine causing infertility.
All the sentences used to elicit injunctive norm significantly correlated with intention to vaccinate the adolescents except the parental belief that traditional healers will approve the administration of HPV vaccine to their adolescents. This statement had low mean belief scores with no significant difference between either group of parents. Similar pattern was seen for descriptive norm among both parents with the statement which stated that traditional healers will allow their own adolescents to take HPV vaccine. Also, for descriptive norm, parents who did not have the intention to vaccinate their adolescents significantly did not believe that people in their social networks will vaccinate their own adolescents with the HPV vaccine. Overall, the correlation between the intention of the parents to vaccinate adolescents with HPV vaccine and the people in their social circle allowing their adolescents to get the vaccine was weak to moderate. There was a weak correlation between perceived control and the intention to vaccinate adolescents with HPV vaccine with the sentence about the administration of HPV vaccines in schools having the least mean belief score. For self-efficacy, the intention to vaccinate adolescents with HPV vaccine had weak to moderate correlations with the painted scenarios. There was a negative mean belief that parents will vaccinate their adolescents with HPV vaccine if the parents had to pay out of pocket for the vaccine and this was significantly worse for parents who did not have the intention to vaccinate their adolescents. The mean belief was however positive if the government will pay for the vaccine for both groups of parents.
Intention to vaccinate adolescents with HPV vaccine and correlation with IBM constructs
There was strong to moderate correlation between parental intention to vaccinate adolescents with HPV vaccine as shown in and experiential attitude had the strongest correlation (ρ = 0.74) while descriptive norm and perceived control had the least correlations (ρ = 0.32 in each case).
Table 2. Association of parental intention to immunize adolescents with HPV vaccine and each component of the Integrated Behavioural Model among parents of adolescents in selected communities in Ibadan.
Intention to vaccinate adolescents with HPV vaccine and parental characteristics
shows the association between the intention to vaccinate adolescents with HPV vaccine and parents’ sociodemographic characteristics. Significantly, a higher proportion of parents who were older than 65 years had no intention to vaccinate their adolescents compared to other age groups. In , good attitude, perceived norm, personal agency, perceived control and self-efficacy were significantly associated with the intention to vaccinate adolescents with HPV vaccine. The highest percentage of parents in this category were those with high experiential attitude 522(77.0%) then high perceived norm 412(60.8%) and injunctive norm 403(59.4%).
Table 3. Association between parental intention to vaccinate adolescents with HPV vaccine and selected parental sociodemographic characteristics of parents of adolescents in selected communities in Ibadan.
Table 4. Association between the components of the Integrated Behavioural Model and parental intention to vaccinate adolescents with HPV vaccine among parents of adolescents in selected communities in Ibadan.
Predictors of intention to vaccinate adolescents with HPV vaccine
shows the result of the multiple regression and the components that were included in the model were instrumental attitude, personal agency and injunctive norm. The first model showed that experiential attitude was a significant predictor of parental intention to vaccinate adolescent with HPV vaccine but the 95% confidence interval included 1. It however became a significant and true predictor of parental intention to vaccinate adolescents with HPV vaccine when personal agency, and subsequently injunctive norm were included in the models.
Table 5. Predictors of parental intention to vaccinate adolescents with HPV vaccine using components of Integrated Behavioural Model among parents of adolescents in selected communities in Ibadan.
Discussion
Almost all the parents in this survey had the intention to vaccinate their adolescents with HPV vaccine as shown by the contribution of each component of IBM. This intention was described in details with respect to their expected feeling, decision-making capacity and the external influences which may affect their decision-making process. However, there were concerns about the high cost of the vaccine which reduced the parents’ mean belief scores, and this was also evident if they were to pay for the vaccine out of pocket. The high proportion of parents who had the intention to vaccinate their adolescents with HPV vaccine is not only consistent with findings from earlier studiesCitation22–37–Citation39 but this proportion was higher than reports from most studies. Although the reason for this is not clear, it may be as a result of the fear associated with cancer as shown in an earlier study.Citation40 There is a high chance that the participants would have come in contact with someone who had cancer or died from cancer. The awareness of the mortality and morbidity associated with the disease is likely to make them accept anything that can prevent cancer among their adolescents. The high proportion of parents willing to get their adolescents vaccinated with HPV vaccine could also be as a result of the presence of community health development committees in each of these communities who have the responsibility of mobilizing community members for vaccination programs. These types of committees have been shown to have positive influence on vaccination coverage in Nigeria.Citation41 Also, the preliminary information they had about cervical cancer pathology and HPV vaccine before answering the survey questions could have enlightened them more about the role of the vaccine in cervical cancer prevention and increased their intention to get the vaccine for their adolescents. However, further investigations will be required to ascertain the real reasons for this high rate of intention to have adolescents vaccinated with HPV vaccine.
One of the differences between this study and earlier similar research is that the parents in the current study were given details about what HPV, HPV vaccine and cervical cancer before they were interviewed to avoid confusion with other disease conditions. This gave them a clear understanding about the questions they were being asked about the vaccine. Their responses were therefore a truer reflection of what they thought of the virus, the disease and the vaccine. This is because earlier studies have shown that there were misconceptions about these three in many countries.Citation13,Citation21,Citation34,Citation42,Citation43 Cancer of the cervix was being confused with cancer of the womb among women in South AfricaCitation43 and there was a lot of misconception about the cause of the disease in southwest Nigeria.Citation34 Also, HIV was being confused with HPV in South Africa.Citation21 It is important that a clear understanding about cervical cancer is established for its preventive measures like HPV vaccine to be acceptable. Otherwise, the output of research regarding cervical cancer and HPV vaccination may be misleading.
The strong correlation between experiential attitude (the feeling after performing a behavior) with the intention to vaccinate adolescent with HPV vaccine implies that the choice of the parents to vaccinate their adolescents was tied to the emotion they will have toward the process and this is similar to an earlier report by Robbins et al.Citation44 It was also a predictor of the intention to vaccinate adolescents. This construct can be targeted for behavioral change for parents who did not have the intention to vaccinate their adolescents in the study communities. Most parents desire to be in control of the events in the lives of their children and this can explain the reduction in the mean belief for perceived control if the HPV vaccination program is to be based in the school environment. This can be handled by allowing parents to provide consent for their adolescents to be vaccinated if Nigeria adopts the school-based program. The parents will then not see the vaccination program as a threat to their primary responsibility of decision-making about the health of their adolescents. Parents, as well as health-care workers have suggested this type of arrangement in earlier studies.Citation10,Citation45
The parents in this study also had unconventional views about the HPV vaccine compared with reports from earlier researchCitation13 which may be because of some paradigm shift from the traditional, conservative views of African parents as a result of urbanization and globalization. They wanted the vaccine for their adolescents despite being told that the HPV was sexually transmitted, and the mean belief that the vaccine will make their adolescents to become promiscuous was negative for both parents with the intention to vaccinate their adolescents and those who had no intention to vaccinate. This is a clear departure from the traditional African parents who believe their adolescents should abstain from all forms of sexual activity.Citation8 It is impressive that despite being informed that HPV was sexually transmitted, it did not deter them from having the intention to vaccinate their adolescents. Earlier studies have consistently shown that associating HPV vaccine with the prevention of sexually transmitted infections discouraged parents who either downplay the involvement of their adolescents’ sexual activitiesCitation44,Citation46 or hold the fear that the administration of the vaccine will promote indiscriminate sex.Citation38,Citation47 The reason for their departure from the conventional view require further research as earlier discussed to unravel the basis for their contrasting views about the sexuality of their adolescents.
The strong influence of the parents’ social circle in their decision about vaccinating their adolescents was shown by the strong correlation between their intention to vaccinate their adolescents with the HPV Vaccine and both injunctive and descriptive norms, similar to earlier reports.Citation31,Citation42,Citation48,Citation49 This further reiterates the importance of community behavioral change in this type of setting where communal living is the norm as individual health education have been shown not to be effective because of the external social influences that affect health-care decision-making.Citation50,Citation51 This type of scenario is seen in vaccine hesitancy which has been demonstrated to occur in clusters most times in the community.Citation52 Therefore, it is important to target the whole community for successful introduction of the HPV vaccine. It is important to note however that the mean belief that traditional healers will support adolescents to take the HPV vaccine or allow their adolescents to do the same was negative for both group of parents. It appears their influence on the decision of these parents to get HPV vaccine for adolescents is weak despite the fact that they patronize these healers, in contrast to an earlier finding from a study in South Africa where traditional healers supported the use of HPV vaccine to prevent cervical cancer.Citation53 The high cost of the HPV vaccine has been a consistent concern among stakeholdersCitation21,Citation46 and the parents in this study also had negative mean beliefs when they were to pay for HPV vaccine, but positive mean belief when the government was to pay for the vaccine. This high cost, relative to the economic status of the parents is one of the main reasons why HPV vaccine is yet to be routine in many developing countries. More effort is required to get cheaper and affordable vaccine in future to increase uptake of the vaccine.
Older people have been shown to be less likely to embrace new technology and this may explain why the older parents in this study significantly did not have the intention of vaccinating their adolescents with HPV vaccine. This was reported earlier by Ogilvie et al who studied parental intention to vaccinate their adolescents in Canada using the Theory of Planned behavior.Citation37 Appropriate and targeted intervention will be required to ensure they embrace the HPV vaccine through health education that demonstrate the relationship between HPV, cervical cancer and HPV vaccine. Peer educators within the same age category with the intention to vaccinate their own adolescents can also be employed, since the older parents would likely identify readily with others in their age group.
One of the strengths of this study is the fair representation of fathers (about a third of the parents) compared with most studies where fathers are either totally absent or are very few.Citation31,Citation54,Citation55 Most African countries are patriarchal, so, excluding men from HPV vaccination or cervical cancer research will be counterproductive because they are either the sole or main decision makers in their families.Citation56,Citation57 This will make outputs from such research irrelevant because the sociocultural context in which health-care decisions are being made were not considered in their design. Another strength is the use of elicitation interviews among the community members to develop the survey instruments based on the constructs of IBM. This made the content of the questionnaire to be familiar to the parents as their culture and beliefs were taken into consideration in contrast to the Health Belief Model that has a more individualistic basis.Citation42 The limitation of this study is the use of IBM which may make the extrapolation of the research findings to other settings difficult because the survey questions were based on findings from elicitation interviews conducted among community members and it is likely to depict their cultures and world view. However, most of the findings of the elicitation interview were similar to earlier research findings.Citation21,Citation23,Citation31
In conclusion, almost all the parents in the study communities had the intention to vaccinate their adolescents with HPV vaccine and experiential attitude was the strongest correlate and predictor of this intention. However, parents who were older than 65 years significantly did not have the intention to vaccinate their adolescents. These older parents will benefit from targeted interventions which will guide them to accept HPV vaccine and ensure the successful rollout of the HPV vaccination program for adolescents in Nigeria in the future.
Future direction
This study focused on intention to vaccinate adolescents with HPV vaccine. The actual uptake of the vaccine when it becomes routine can be explored and compared with the current findings. Also, the reasons for the reluctance of older parents to vaccinate their adolescents can be investigated so that interventions to increase their intention to vaccinate their adolescents can be designed based on the results of the investigation. The reasons for the high number of parents with the intention to vaccinate their adolescents with HPV vaccine also need to be explored. This may be a departure from the normal conservative views of parents about their adolescents’ sexuality or improved acceptance of vaccines.
Supplemental Material
Download MS Word (21.6 KB)Acknowledgments
We appreciate the support of the Chairman of Ward four, Ibadan North Local Government Area during the data collection phase. We also appreciate all the parents who accepted to participate in this study.
Disclosure statement
No potential conflict of interest was reported by the authors.
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2022.2069959.
Additional information
Funding
References
- Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–9. doi:10.3322/caac.21660.
- Gertig DM, Brotherton JM, Budd AC, Drennan K, Chappell G, Saville AM. Impact of a population-based HPV vaccination program on cervical abnormalities: a data linkage study. BMC Med. 2013;11(1):227. doi:10.1186/1741-7015-11-227.
- Bruni L, Albero G, Serrano B, Mena M, Gómez D, Muñoz J, Bosch FX, de Sanjose S. The human papillomavirus and related diseases in Nigeria. ICO/IARC Information Centre on HPV and Cancer (HPV Information Centre). 2019.
- Durst M, Gissmann L, Ikenberg H, zur Hausen H. A papillomavirus DNA from a cervical carcinoma and its prevalence in cancer biopsy samples from different geographic regions. Proc Natl Acad Sci U S a. 1983;80(12):3812–15. doi:10.1073/pnas.80.12.3812.
- Boshart M, Gissmann L, Ikenberg H, Kleinheinz A, Scheurlen W, zur Hausen H. A new type of papillomavirus DNA, its presence in genital cancer biopsies and in cell lines derived from cervical cancer. Embo J. 1984;3(5):1151–57. doi:10.1002/j.1460-2075.1984.tb01944.x.
- Barbot B, Heinz SL, Luthar SS. Perceived parental reactions to adolescent distress: development and validation of a brief measure. Attachment Hum Dev. 2014;16(1):1–21. doi:10.1080/14616734.2013.804328.
- Jit M, Choi YH, Edmunds WJ. Economic evaluation of human papillomavirus vaccination in the United Kingdom. BMJ (Clinical Research Ed). 2008;337:a769. doi:10.1136/bmj.a769.
- Dairo MD, Adeleke MO, Salawu AT, Adewole AD. Parental support for human papilloma virus vaccination by adolescents in Ibadan North Local Government Area, Ibadan, Nigeria. Int J Adolesc Med Health. 2016;30(2). doi:10.1515/ijamh-2016-0034.
- Brabin L, Roberts SA, Kitchener HC. A semi-qualitative study of attitudes to vaccinating adolescents against human papillomavirus without parental consent. BMC Public Health. 2007;7(1):20. doi:10.1186/1471-2458-7-20.
- Gottvall M, Grandahl M, Hoglund AT, Larsson M, Stenhammar C, Andrae B, Tydén T. Trust versus concerns—how parents reason when they accept HPV vaccination for their young daughter. Ups J Med Sci. 2013;118(4):263–70. doi:10.3109/03009734.2013.809039.
- Abdullahi LH, Hussey GD, Wiysonge CS, Kagina BM. Lessons learnt during the national introduction of human papillomavirus (HPV) vaccination programmes in 6 African countries: stakeholders’ perspectives. S Afr Med J = Suid-Afrikaanse Tydskrif Vir Geneeskunde. 2020;110(6):525–31. doi:10.7196/SAMJ.2020.v110i6.14332.
- Bobo FT, Asante A, Woldie M, Dawson A, Hayen A. Child vaccination in sub-Saharan Africa: increasing coverage addresses inequalities. Vaccine. 2022;40(1):141–50. doi:10.1016/j.vaccine.2021.11.005.
- Harries J, Moodley J, Barone MA, Mall S, Sinanovic E. Preparing for HPV vaccination in South Africa: key challenges and opinions. Vaccine. 2009;27(1):38–44. doi:10.1016/j.vaccine.2008.10.033.
- Turiho AK, Okello ES, Muhwezi WW, Katahoire AR. Perceptions of human papillomavirus vaccination of adolescent schoolgirls in western Uganda and their implications for acceptability of HPV vaccination: a qualitative study. BMC Res Notes. 2017;10(1):431. doi:10.1186/s13104-017-2749-8.
- Milondzo T, Meyer JC, Dochez C, Burnett RJ. Misinformation drives low human papillomavirus vaccination coverage in South African Girls Attending Private Schools. Front Public Health. 2021;9. doi:10.3389/fpubh.2021.598625.
- Wilson R. HPV vaccine acceptance in West Africa: a systematic literature review. Vaccine. 2021;39:5277–84.
- UNICEF. The state of the world’s children 2011: adolescence, an age of opportunity. New York (NY): United Nations Children’s Fund (UNICEF); 2011.
- Jegede AS. What led to the Nigerian boycott of the polio vaccination campaign? PLoS Med. 2007;4(3):e73. doi:10.1371/journal.pmed.0040073.
- Morhason-Bello IO, Adesina OA, Adedokun BO, Awolude O, Okolo CA, Aimakhu CO, Akinwunmi BO, Oladokun A, Adewole IF. Knowledge of the human papilloma virus vaccines, and opinions of gynaecologists on its implementation in Nigeria. Afr J Reprod Health. 2013;17:150–56.
- Azuogu B, Umeokonkwo C, Azuogu V, Onwe O, Okedo-Alex I, Egbuji C. Appraisal of willingness to vaccinate daughters with human papilloma virus vaccine and cervical cancer screening uptake among mothers of adolescent students in Abakaliki, Nigeria. Niger J Clin Pract. 2019;22(9):1286. doi:10.4103/njcp.njcp_452_18.
- Head KJ, Cohen EL. Young women’s perspectives on cervical cancer prevention in Appalachian Kentucky. Qual Health Res. 2011;22:476–87. doi:10.1177/1049732311425053.
- Ezeanochie MC, Olagbuji BN. Human papilloma virus vaccine: determinants of acceptability by mothers for adolescents in Nigeria. Afr J Reprod Health. 2014;18:154–58.
- Rabiu KA, Alausa TG, Akinlusi FM, Davies NO, Shittu KA, Akinola OI. Parental acceptance of human papillomavirus vaccination for adolescent girls in Lagos, Nigeria. J Family Med Prim Care. 2020;9(6):2950–57. doi:10.4103/jfmpc.jfmpc_102_20.
- Fishbein M. A reasoned action approach: some issues, questions, and clarifications. In: Ajzen I, Al-barracin D, and Hornik R, editors. Prediction and change of health behavior: applying the reasoned action approach. Hillsdale, N.J.: Erlbaum; 2007. p. 281–95.
- Fishbein M, Bandura A, Triandis HC, Kanfer FH, Becker MH, Middlestadt S. Factors influencing behavior and behavior change. Bethesda, MD: National Institute of Mental Health; 1992.
- Glanz K, Rimer BK, Viswanath K. Health behavior and health education: theory, research, and practice. San Francisco: CAJohn Wiley & Sons; 2008.
- Katz IT, Ware NC, Gray G, Haberer JE, Mellins CA, Bangsberg DR. Scaling up human papillomavirus vaccination: a conceptual framework of vaccine adherence. Sex Health. 2010;7(3):279–86. doi:10.1071/SH09130.
- Rimal RN, Real K. How behaviors are influenced by perceived norms: a test of the theory of normative social behavior. Communic Res. 2005;32(3):389–414. doi:10.1177/0093650205275385.
- Kasprzyk D, Montaño DE, Fishbein M. Application of an integrated behavioral model to predict condom use: a prospective study among high HIV risk Groups1. J Appl Soc Psychol. 1998;28(17):1557–83. doi:10.1111/j.1559-1816.1998.tb01690.x.
- Bandura A. Toward a psychology of human agency. Perspect Psychol Sci. 2006;1(2):164–80. doi:10.1111/j.1745-6916.2006.00011.x.
- Rodriguez SA, Savas LS, Baumler E, Nyitray AG, Mullen PD, Vernon SW, Fernandez ME. Parental predictors of HPV vaccine initiation among low-income Hispanic females aged 11–17 years. Vaccine. 2018;36(33):5084–90. doi:10.1016/j.vaccine.2018.06.071.
- Kish L. Survey sampling. New York (NY): John Wiley and Sons, Inc; 1965.
- Osgood CE. Studies on the generality of affective meaning systems. Am Psychol. 1962;17(1):10–28. doi:10.1037/h0045146.
- Balogun F, Omotade O, Maree J. “She must have been sleeping around”: contextual interpretations of cervical cancer and views regarding HPV vaccination for adolescents in selected communities in Ibadan, Nigeria. PloS One. 2018;13(9):e0203950. doi:10.1371/journal.pone.0203950.
- Statistical package for social sciences for windows. Version 22.0. Armonk, NY. IBM Corp.;2013.
- Oyedeji G. Socioeconomic and cultural background of hospitalised children in Ilesa. Nig J Paed. 1985;12:111–17.
- Ogilvie GS, Remple VP, Marra F, McNeil SA, Naus M, Pielak KL, Ehlen TG, Dobson SR, Money DM, Patrick DM, et al. Parental intention to have daughters receive the human papillomavirus vaccine. Can Med Assoc J = Journal de L’Association Medicale Canadienne. 2007;177(12):1506–12. doi:10.1503/cmaj.071022.
- Marlow LA, Waller J, Wardle J. Parental attitudes to pre-pubertal HPV vaccination. Vaccine. 2007;25:1945–52. doi:10.1016/j.vaccine.2007.01.059.
- Degarege A, Krupp K, Fennie K, Srinivas V, Li T, Stephens DP, Madhivanan P. An integrative behavior theory derived model to assess factors affecting HPV vaccine acceptance using structural equation modeling. Vaccine. 2019;37(7):945–55. doi:10.1016/j.vaccine.2019.01.012.
- Kuitto K, Pickel S, Neumann H, Jahn D, Metelmann H-R. Attitudinal and socio-structural determinants of cervical cancer screening and HPV vaccination uptake: a quantitative multivariate analysis. J Public Health (Bangkok). 2010;18(2):179–88. doi:10.1007/s10389-009-0308-z.
- Itimi K, Dienye PO, Ordinioha B. Community participation and childhood immunization coverage: a comparative study of rural and urban communities of Bayelsa State, south-south Nigeria. Niger Med J. 2012;53(1):21–25. doi:10.4103/0300-1652.99826.
- Katz IT, Nkala B, Dietrich J, Wallace M, Bekker LG, Pollenz K, Bogart LM, Wright AA, Tsai AC, Bangsberg DR, et al. A qualitative analysis of factors influencing HPV vaccine uptake in Soweto, South Africa among adolescents and their caregivers. PloS One. 2013;8(8):e72094. doi:10.1371/journal.pone.0072094.
- Francis SA, Battle-Fisher M, Liverpool J, Hipple L, Mosavel M, Soogun S, Mofammere N. A qualitative analysis of South African women’s knowledge, attitudes, and beliefs about HPV and cervical cancer prevention, vaccine awareness and acceptance, and maternal-child communication about sexual health. Vaccine. 2011;29(47):8760–65. doi:10.1016/j.vaccine.2011.07.116.
- Robbins SCC, Bernard D, McCaffery K, Brotherton JML, Skinner SR. “I just signed”: factors influencing decision-making for school-based HPV vaccination of adolescent girls. Health Psychol. 2010;29(6):618–25. doi:10.1037/a0021449.
- Stretch R, McCann R, Roberts SA, Elton P, Baxter D, Brabin L. A qualitative study to assess school nurses’ views on vaccinating 12-13 year old school girls against human papillomavirus without parental consent. BMC Public Health. 2009;9:254. doi:10.1186/1471-2458-9-254.
- Holman DM, Benard V, Roland KB, Watson M, Liddon N, Stokley S. Barriers to human papillomavirus vaccination among US adolescents: a systematic review of the literature. JAMA Pediatr. 2014;168(1):76–82. doi:10.1001/jamapediatrics.2013.2752.
- Mupandawana ET, Cross R. Attitudes towards human papillomavirus vaccination among African parents in a city in the north of England: a qualitative study. Reprod Health. 2016;13(1):97. doi:10.1186/s12978-016-0209-x.
- Cheruvu VK, Bhatta MP, Drinkard LN. Factors associated with parental reasons for “no-intent” to vaccinate female adolescents with human papillomavirus vaccine: national immunization survey - Teen 2008–2012. BMC Pediatr. 2017;17(1):52. doi:10.1186/s12887-017-0804-1.
- Britt RK, Hatten KN, Chappuis SO. Perceived behavioral control, intention to get vaccinated, and usage of online information about the human papillomavirus vaccine. Health Psychol Behav Med. 2014;2(1):52–65. doi:10.1080/21642850.2013.869175.
- Poole DN, Tracy JK, Levitz L, Rochas M, Sangare K, Yekta S, Tounkara K, Aboubacar B, Koita O, Lurie M, et al. A cross-sectional study to assess HPV knowledge and HPV vaccine acceptability in Mali. PloS One. 2013;8(2):e56402. doi:10.1371/journal.pone.0056402.
- Ruijs WL, Hautvast JL, Kerrar S, van der Velden K, Hulscher ME. The role of religious leaders in promoting acceptance of vaccination within a minority group: a qualitative study. BMC Public Health. 2013;13(1):511. doi:10.1186/1471-2458-13-511.
- Leask J, Willaby HW, Kaufman J. The big picture in addressing vaccine hesitancy. Hum Vaccines Immunother. 2014;10(9):2600–02. doi:10.4161/hv.29725.
- Nelson JA, Francis SA, Liverpool J, Soogun S, Mofammere N. Healers in a non-traditional role; a focus group study of Sangoma’s knowledge of and attitudes to cervical cancer prevention and screening in Johannesburg, South Africa. Sexual Reprod Healthcare. 2010;1(4):195–96. doi:10.1016/j.srhc.2010.07.004.
- Omondi-Ogutu M, Imunya JM. Parental acceptance of human papillomavirus vaccine for their pre-pubertal and teenage daughters. East Afr Med J. 2011;88:163–70.
- Ngorsuraches S, Nawanukool K, Petcharamanee K, Poopantrakool U. Parents’ preferences and willingness-to-pay for human papilloma virus vaccines in Thailand. J Pharm Policy Pract. 2015;8(1):20. doi:10.1186/s40545-015-0040-8.
- Osamor P, Grady C. Factors associated with women’s health care decision-making autonomy: empirical evidence from Nigeria. J Biosoc Sci. 2018;50(1):70–85. doi:10.1017/S0021932017000037.
- Tokhi M, Comrie-Thomson L, Davis J, Portela A, Chersich M, Luchters S, van Wouwe JP. Involving men to improve maternal and newborn health: a systematic review of the effectiveness of interventions. PloS One. 2018;13(1): e0191620-e. doi:10.1371/journal.pone.0191620.