Abstract
Non-invasive ventilation (NIV) or tracheotomy with invasive ventilation (TIV) are treatment options in ALS. However, a proportion of patients receiving long-term ventilation decide to have it withdrawn. The objective of this study was to analyse the clinical characteristics and palliative approaches in ALS patients withdrawing from long-term ventilation (WLTV).
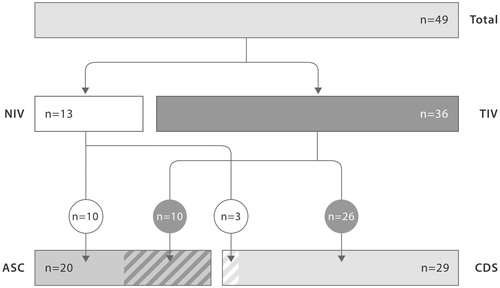
In a cohort study, two different palliative concepts in WLTV were studied: (1) augmented symptom control (ASC; sedation not intended) in patients with ventilator-free tolerance; (2) continuous deep sedation (CDS; sedation intended) in patients without ventilator-free tolerance. Results showed that WLTV was realised in 49 ALS patients (NIV = 13; TIV = 36). Mean daily ventilation was 23.4 h. The ALS Functional Rating Scale (ALSFRS-R) was low (5.6 of 48). Forty-one per cent of patients (n = 20) presented with ophthalmoplegia. ASC was performed in 20 patients, CDS in 29 patients. The mean time to death following disconnection was 32 (0.3–164) h during ASC and 0.3 (0.2–0.6) h in CDS. In conclusion, a low ALSFRS-R, high incidence of ophthalmoplegia and extended ventilator dependency were found before WLTV. The presence or absence of ventilator-free tolerance determined the approach to the management of symptoms, the setting for immediate end-of-life care and the course of dying in WLTV.
Introduction
Non-invasive ventilation (NIV) is the standard of care in ALS while tracheotomy with invasive ventilation (TIV) is realised in a smaller number of ALS patients (Citation1–3). In some countries including Germany, the frequency of TIV is on the increase; in our hospital, it is 8% (Citation4–6). The underlying reasons for the steady rise in life-prolonging treatment with NIV or TIV are improved home ventilation, availability of electronic communication systems and the availability of online participatory activities (Citation7,Citation8). Both forms of long-term ventilation can be associated with a substantial psychosocial strain for the patients and caregivers resulting in the wish of the patient to withdraw from ventilation therapy (Citation9–11). Typical factors contributing to the withdrawal of long-term ventilation (WLTV) are the burden of care, social deprivation or loss of the ability to communicate through an ALS-related ophthalmoplegia and locked-in syndrome (Citation11–14). Despite the increasing frequency of WLTV, there are still very few systematic investigations on the limitation or discontinuation of ventilation therapy in ALS patients (Citation14–16). Although there is variability among cases, WLTV is likely to lead to breathlessness and distress, which should be anticipated and managed proactively. For symptom management, two different groups of symptom control in WLTV have been distinguished: the ‘sedation’ group refers to those patients who are highly dependent on NIV or TIV and may become distressed within minutes of WLTV. These patients will require continuous deep sedation (CDS) before WLTV. The ‘augmented symptom control’ (ASC) group refers to patients who can tolerate longer periods of time without ventilation support. In this group, patients require medication that allows them to remain calm and comfortable without being deeply sedated. Only recently, the Association for Palliative Medicine of Great Britain and Ireland published a comprehensive professional guideline for WLTV elaborating on the concepts of sedation and ASC (Citation17). The present cohort study summarizes the experience of WLTV in 49 ALS patients. Here, the clinical characteristics of ALS patients before WLTV, our experiences with the two approaches of palliation (ASC and CDS) and the determinants of the dying process are presented.
Methods
Study design and participants
We performed a cohort study in a referral centre for patients with ALS in Berlin (Germany). The study patients fulfilled the diagnostic criteria for ALS. All patients were receiving long-term ventilation through NIV or TIV. Prior to WLTV, in all patients a minimum of two clinicians trained in assessing the patient’s decision making capacity were involved. Furthermore, for all patients feedback was obtained from the multi-professional team and the family regarding the consistency of the patients’ wishes. In one case, a psychiatrist was consulted additionally to exclude a mental health disorder affecting the decision-making capacity. In all patients including those with loss of the ability to communicate (tetraplegia in conjunction with ophthalmoplegia; n = 7), an advance directive had been obtained specifying the individual criteria and timing of WLTV. In principle, prior to WLTV two case conferences had been held (at least four weeks apart) attended by the patient, the patient’s relatives, friends, carers or other persons authorized by the patient. For the end-of-life decision conferences, the multidisciplinary ALS outpatient clinic team and representatives of the home care team were gathered. Persons authorized by the patient were offered to be present during WLTV including ‘rooming-in’ for longer courses of WLTV (mostly relevant in ASC).
The present study is an observational study about factors that are associated with a WLTV. The investigation includes a cohort study on two different approaches to palliative care. The determinants of the palliative approach and the process of dying are analysed. The study covers the time-period of September 2002 to June 2015. Data from 2002 to 2007 are analysed retrospectively; prospective analysis began in 2008. In the retrospective portion, patients were included who were already studied for other aspects (Citation16).
Data obtained
Baseline data and the neurological status were systematically documented. ALS severity was captured using the ALS Functional Rating Scale (ALSFRS-R) (Citation19). The type of ventilation (NIV, TIV), the duration of ventilation (months), the daily time of ventilation (hours) and the presence of ventilator-free breathing tolerance (minutes or hours) were documented. The duration of the process of dying was defined as the time between the disconnection from the ventilator (or the removal of the ventilation mask from the face) until asystolia.
Protocol approvals and registrations
The study protocol was approved by the Medical Ethics Committee of the Charité. According to their published ethical standards and guidelines, obtainment of a signed patient information and informed consent form was not required because reports were anonymized and there was no study intervention.
Data analysis
We determined the significant difference in the distribution of factors between patients cohorts using the Mann-Whitney U-test (age, disease duration, ALSFRS-R, ventilation time per day, duration of long-term ventilation, time to death after disconnection). A χ2 test was used to analyse the significance in the distribution of gender. To determine the significant differences in ALS-related ophthalmoplegia a Fisher’s exact test was used. All tests were two-tailed.
Results
Clinical characteristics
The clinical characteristics, the mode of ventilation and the course of dying are summarized in .
Table I. Clinical characteristics and course of dying in ALS patients withdrawing from long-term ventilation.
Approaches of palliation by medication
WLTV may lead to distressing symptoms that require anticipatory and timely treatment with appropriate doses of medications such as opioids and sedatives. The medication was intended to avoid or alleviate symptoms of discomfort or distress. The choice of medication for palliation of symptoms during WLTV was dependent on the severity and timing of symptoms anticipated upon removal of the mask or disconnection of the ventilator. Two different patient groups were distinguished (Citation17). One group of patients showed incomplete dependence on NIV or TIV with some ventilation-free breathing tolerance. In these patients a gradual increase of distress – if any – was anticipated. In this group medication for an augmented symptom control (ASC) was sufficient to avoid or ameliorate symptoms. Another group of patients showed complete dependence on NIV or TIV with no ventilation-free breathing tolerance. It was anticipated that removal of the mask or disconnection of the ventilator would lead to an immediate and high-grade distress. To avoid acute and severe distress a continuous deep sedation (CDS) was required.
Prior to WLTV, there was a decision between treatment regimens of ASC or CDS. The decision to use either ASC or CDS depended on whether or not patients had any ventilator-free breathing tolerance. The patients and the home care team were asked about ventilator-free breathing tolerance and anticipated distress while specifically differentiating between residual, minimal and lack of spontaneous breathing. In some individual cases, a trial disconnection was made, to determine the ventilation-free breathing tolerance. If ventilation-free time was verified, one could assume that ASC would be sufficient to avoid or alleviate WLTV-related symptoms. In the absence of ventilation-free breathing tolerance, it was assumed that CDS is required for the palliation of symptoms.
Augmented symptom control (ASC)
ASC was chosen in the presence of ventilation-free tolerance in NIV or TIV and an anticipated low degree of dyspnoea. To control possible symptoms such as distress, dyspnoea, anxiety or agitation, benzodiazepines (preferably lorazepam) or morphines were administered. Sedation was accepted although not intended. The use of ASC is summarized in .
Figure 1. Modes of ventilation and palliative approaches in patients with ALS withdrawing from long-term ventilation.
n: number of patients; Total: total number of patients in studied cohort; NIV: non-invasive ventilation; TIV: tracheotomy with invasive ventilation; ASC: augmented symptom control; CDS: continuous deep sedation.
Continuous deep sedation (CDS)
CDS was elected in the absence of ventilation-free breathing tolerance. CDS was initiated before disconnection from the ventilator and realised with intravenous injections of morphines and propofol. Central venous access was used as peripheral venous punctures and ports were complicated or impossible to achieve due to the vasculature characteristics in this patient group. Patients choosing CDS had mostly endured a long disease course beyond the natural history of ALS. In these patients, we often found skin changes, lymphatic oedema and reduced venous visibility which hampered peripheral venous targeting. Sedation was not only accepted but intended to achieve the objective of shielding patients from dyspnoea and other distressing symptoms arising from acute deoxygenation. The use of CDS is summarized in .
Change of palliative concepts during WLTV
A switch of the previously planned medication regimen was necessary for two patients during the course of WLTV. One patient with TIV and anticipated high-grade distress (planned for CDS), showed unexpectedly residual spontaneous breathing while under sedation with propofol. In this case, sedation with propofol was tapered off and eventually stopped. During the tapering off, the patient was closely monitored for any clinical signs of dyspnoea or other distress. ASC using lorazepam and morphine proved sufficient to achieve symptom control. Another patient with intermittent NIV anticipated low-grade distress and planned ASC, but experienced the beginning of dyspnoea, which made CDS necessary to prevent distress and to control symptoms completely. In both cases, the unexpected necessity to alleviate symptoms was recognised instantly. Thus, unnecessary suffering from uncontrolled symptoms could be prevented (most particularly in the patient switching from ASC to CDS).
Symptom control
Adequate symptom control was defined as absence or alleviation of symptoms that may be related to the withdrawal of ventilation support. Target symptoms were distress or breathlessness including nasal flaring, sweating, increase in pulse rate or increase in respiratory rate (Citation17). The degree of sedation (in CDS) was confirmed by a reduced level of consciousness with no response to voice or pain stimulus. In most patients, primary symptom control was achieved. However, in some patients myoclonus (n = 6) was observed. Distress (n = 4) or dyspnoea (n = 1) was reported in a smaller subgroup of patients. However, in all patients symptoms were prevented or alleviated through titration of medication or by changing the palliative concept (planned ASC; switched to CDS).
Process of dying
With ASC, the mean time to death (time from disconnection to asystole) lasted 32.36 h (0.33–164 h). With CDS, the mean dying phase was much shorter and showed a mean latency to death of 0.31 h (0.15–0.63 h). The difference in the time-course of dying between ASC and CDS was highly significant (p < 0.05).
Discussion
The results show that WLTV is not realised early in ALS ventilation therapy. The patients’ wish for WLTV emerges more than one year into NIV. Apparently, WLTV in NIV occurs most frequently at a time when the treatment option of mask ventilation has been ‘exhausted’ and the decision between change to palliative care at the end of life and TIV may be needed to be taken. In patients with TIV, WLTV happens significantly later (mean 34 months after initiation of TIV). However, in some cases the decision for WLTV can arise a few days after the initiation of ventilation therapy or after several years of NIV or TIV (in this study, up to 12.5 years). Therefore, the ventilation period seems to be an uncertain factor in the decision for or against WLTV. Also, no clear pattern could be deduced from the patients’ age, gender and duration of disease.
Patients’ decisions for WLTV tend to arise in the setting of a more gradual decline in function that leads to a persistently unacceptable quality of life (Citation17). We found that patients who pursue WLTV have high ventilator dependency. It is well conceivable that WLTV in NIV was chosen in the face of the high burden associated with continuous NIV. Despite the high mean ventilation time, some patients opted for WLTV while still being on NIV for relatively short intervals (12 h/day). The reasons why individual patients chose certain points in time and situations to have WLTV initiated needs further research.
Forty-one per cent of patients before WLTV had complete or partial ophthalmoplegia. This is striking, since eye movement disorder is a very rare event during the natural course of ALS (Citation22). In this study, most of the patients with ophthalmoplegia (except one patient who had received NIV for 53 months) were invasively ventilated. Our observation corresponds to previous studies that ophthalmoplegia and locked-in syndrome may occur beyond the natural history of ALS during long-term ventilation (Citation15,Citation23). Ophthalmoplegia leads to a loss of the use of eye-controlled communication systems and thus to a further restriction of patient autonomy. Therefore, we discuss that ALS-related ophthalmoplegia is an important turning point in the patient’s decision-making process and may represent one of several factors associated with WLTV in ALS.
In the literature on WLTV in ALS, the focus had been on patients with TIV (Citation15,Citation18). Only recently, systematic data on WLTV in both NIV and TIV have been obtained (Citation11,Citation17). Rather than capturing the whole range of palliative concepts, our study compared ASC and CDS as being two distinct palliative approaches in WLTV (Citation17). For symptom control in patients with ventilation-free tolerance and mild anticipated symptoms after disconnection from the ventilator, ASC appears sufficient. The limitation with ASC is that not all patients, i.e. those without ventilation-free tolerance and with severe anticipated symptoms following disconnection, are actually suited to this approach. In these patients, CDS provides sufficient symptom control. The downside is the degree of invasiveness with this method (once a placement of central venous access is necessary) and the short latency to death (given that CDS is mostly performed in patients without ventilation-free tolerance). Thus, CDS may be perceived as distinct from a natural course of dying. A systematic survey of ethics and legal issues among physicians in the UK revealed anxieties about the ethics related to the use of medication in WLTV (Citation11). Some respondents (all experienced with WLTV in ALS) were concerned that they were not seen to hasten the patient’s death with sedative medication (Citation11). Independent of the method’s limitations (invasiveness and potential misperception), CDS is not ‘routinely’ used in all patients who decided for WLTV. CDS may be an overtreatment in patients who do not require a deep level of sedation for the control of WLTV related symptoms. In principle, it is conceivable that patients who show ventilator-free tolerance (qualifying for ASC) may wish to receive CDS in order to ‘escape’ from the more prolonged dying process by an immediate loss of consciousness in CDS. Interestingly, none of the patients with ventilator-free tolerance (n = 20; suggested for ASC) endorsed the alternative treatment option of CDS.
We found that ASC and CDS are equally relevant palliative concepts in WLTV (). As expected, CDS was the predominant palliative pathway for patients withdrawing from TIV. In contrast, ASC was sufficient in most of the patients with NIV. Nonetheless, CDS was performed in three NIV patients to control symptoms during WLTV. Our findings substantiate that the prime issue when choosing between ASC or CDS is not the actual withdrawal of NIV or TIV but rather if there is ventilator-free breathing tolerance before WLTV. Whenever possible (given ventilator-free tolerance) we assume that ASC is favourable over CDS. ASC may be seen as closer to the natural process of dying as the patient slowly deteriorates over 32 h. This may be less stressful for families and professionals, although it may also be considered by some as an unnecessary prolongation of the dying process. In contrast, CDS may be seen as less stressful as the process of dying occurs over a matter of only minutes, although this again may be seen by some as a source of stress as they fear they have caused the death through an active act, which may feel like euthanasia (Citation11). Both perspectives are reasonable and require systematic research and elucidation.
The distinction between ASC and CDS was of psychosocial relevance as these concepts stood for different clinical settings and expectations held by patients, relatives, physicians and nursing staff. ASC implied overnight hospital care (dying process of more than one day), whereas CDS meant a very short hospital stay for a few hours (course of dying of less than 1 h). Before starting WLTV, both the patient and the relatives present should be informed of the possibility of having to switch palliative concepts during WLTV (i.e. from ASC to CDS or vice versa). Another aspect that needs to be communicated is the strict distinction between CDS and euthanasia. The placement of a central venous catheter, deep sedation and the short dying phase may create the impression of being an ‘active’ intervention (Citation11,Citation18). This stresses the importance that patients, their families and health care professionals involved in WLTV should be advised that WLTV differs morally and legally from euthanasia or physician-assisted suicide. CDS should be perceived as sedation for the imminently dying patient, which is administered with the intent of relieving symptoms, not of hastening death (Citation24,Citation25).
This study has several limitations. Some of them are related to the mixed retrospective-prospective design. The reasons of the patients for stopping ventilation, the validation of quality of death and the judgement of the procedure by relatives cannot be explored retrospectively. Therefore, this study was not designed to systematically capture the psychological impact in WLTV. Previous reports addressed the psychological strain of WLTV making further studies on the quality of death and other psychological aspects in WLTV highly desirable (Citation9,Citation12,Citation15,Citation18).
In WLTV, the use of midazolam and opioids is the ‘standard of care’ for symptom control. However, there is increasing experience on the use of propofol in palliative sedation (Citation26). In our setting we used propofol for medication in CDS (not in ASC). In this situation propofol allowed the depth of sedation to be easily controlled from minute to minute (Citation27). We are aware that our preference for propofol was one of several factors in the considerable variations of how WLTV is performed. A multicentre, ideally international and transcultural, study on different palliative approaches is needed to address the limitations of this study and the many unanswered questions in WLTV.
In ALS, with the decision for WLTV, the patient may define his or her own date of death. The experiences of the patient before the WLTV and of the family and healthcare professionals before and after the WLTV, is mostly unknown. The emotional and psychosocial experience close to death is a field of research that has been little explored. WLTV among ALS patients opens an access to this important issue (Citation28,Citation29).
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
Acknowledgements
DK, AF, CM and TM were supported by the initiative ‘Hilfe für ALS-kranke Menschen’. DK was a fellow of the ‘Angelika-von-Hagen-Fonds für Palliativmedizin bei der ALS’. The authors’ work was also supported by the ‘Knut Marthiens Fonds für ALS-Therapieforschung’. TM and SS were supported by the Joint Programme - Neurodegenerative Disease Research (BMBF; 01ED1402A). The project is supported through the following funding organizations under the aegis of JPND (http://www.jpnd.eu): Agency for Innovation by Science and Technology and Research Foundation, Flanders region; Bundesministerium für Bildung und Forschung (BMBF), Germany; Economic and Social Research Council, United Kingdom; Health Research Board, Ireland; Ministry of Health and Ministry of Education, Universities and Research, Italy; The Netherlands Organization for Health Research and Development, The Netherlands (national regional organizations who are funding project, by country, in alphabetical order).
References
- Miller RG, Jackson CE, Kasarskis EJ, England JD, Forshew D, Johnston W, et al. Practice parameter update: the care of the patient with amyotrophic lateral sclerosis. Multidisciplinary care, symptom management, and cognitive/behavioural impairment (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2009;73:1227–33.
- Andersen PM, Abrahams S, Borasio GD, de Carvalho M, Chio A, van Damme P, et al. EFNS guidelines on the clinical management of amyotrophic lateral sclerosis - revised report of an EFNS task force. Eur J Neurol. 2012;19:360–75.
- Bourke SC, Tomlinson M, Williams TL, Bullock RE, Shaw PJ, Gibson GJ. Effects of non-invasive ventilation on survival and quality of life in patients with amyotrophic lateral sclerosis: a randomised controlled trial. Lancet Neurol. 2006;5:140–7.
- Rabkin J, Ogino M, Goetz R, McElhiney M, Hupf J, Heitzman D, et al. Japanese and American ALS patient preferences regarding TIV (tracheotomy with invasive ventilation): a cross-national survey. Amyotroph Lateral Scler Frontotemporal Degener. 2014;15:185–91.
- Fini N, Georgoulopoulou E, Vinceti M, Monelli M, Pinelli G, Vacondio P, et al. Non-invasive and invasive ventilation and enteral nutrition for ALS in Italy. Muscle Nerve. 2014;50:508–16.
- Dreyer P, Lorenzen CK, Schou L, Felding M. Survival in ALS with home mechanical ventilation non-invasively and invasively: a 15-year cohort study in west Denmark. Amyotroph Lateral Scler Frontotemporal Degener. 2014;15:62–7.
- Caligari M, Godi M, Guglielmetti S, Franchignoni F, Nardone A. Eye tracking communication devices in amyotrophic lateral sclerosis: impact on disability and quality of life. Amyotroph Lateral Scler Frontotemporal Degener. 2013;14:546–52.
- Londral A, Pinto A, Pinto S, Azevedo L, De Carvalho M. Quality of life in amyotrophic lateral sclerosis patients and caregivers: impact of assistive communication from early stages. Muscle Nerve. 2015;52:933–41.
- Martin NH, Landau S, Janssen A, Lyall R, Higginson I, Burman R, et al. Psychological as well as illness factors influence acceptance of non-invasive ventilation (NIV) and gastrostomy in amyotrophic lateral sclerosis (ALS): a prospective population study. Amyotroph Lateral Scler Frontotemporal Degener. 2014;15:376–87.
- Kaub-Wittemer D, Steinbüchel NV, Wasner M, Laier-Groeneveld G, Borasio GD. Quality of life and psychosocial issues in ventilated patients with amyotrophic lateral sclerosis and their caregivers. J Pain Symptom Manage. 2003;26:890–6.
- Phelps K, Regen E, Oliver D, McDermott C, Faull C. Withdrawal of ventilation at the patient's request in MND: a retrospective exploration of the ethics and legal issues that have arisen for doctors in the UK. Br Med J Support Palliat Care. 2015; Epub ahead of print. doi:10.1136/bmjspcare-2014-000826.
- Rousseau MC, Pietra S, Blaya J, Catala A. Quality of life of ALS and LIS patients with and without invasive mechanical ventilation. J Neurol. 2011;258:1801–4.
- Stutzki R, Weber M, Reiter-Theil S, Simmen U, Borasio GD, Jox RJ. Attitudes towards hastened death in ALS: a prospective study of patients and family caregivers. Amyotroph Lateral Scler Frontotemporal Degener. 2014;15:68–76.
- Maessen M, Veldink JH, Onwuteaka-Philipsen BD, Hendricks HT, Schelhaas HJ, Grupstra HF, et al. Trends and determinants of end-of-life practices in ALS in the Netherlands. Neurology. 2009;73:954–61.
- Dreyer PS, Felding M, Klitnæs CS, Lorenzen CK. Withdrawal of invasive home mechanical ventilation in patients with advanced amyotrophic lateral sclerosis: ten years of Danish experience. J Palliat Med. 2012;15:205–9.
- Meyer T, Dullinger JS, Münch C, Keil JP, Hempel E, Rosseau S, et al. Elective termination of ventilatory therapy in amyotrophic lateral sclerosis. Nervenarzt. 2008;79:684–90.
- Association for Palliative Medicine of Great Britain and Ireland (2015). Withdrawal of Assisted Ventilation at the Request of a Patient with Motor Neurone Disease: Guidance for Professionals. Available at http://apmonline.org/wp-content/uploads/2015/12/Guidance-with-logos-updated-020316.pdf (Accessed 21 March 2016).
- LeBon B, Fisher S. Case report: maintaining and withdrawing long-term invasive ventilation in a patient with MND/ALS in a home setting. Palliat Med. 2011;25:262–5.
- Cedarbaum JM, Stambler N, Malta E, Fuller C, Hilt D, Thurmond B, et al BDNF ALS Study Group (Phase III). The ALSFRS-R: a revised ALS functional rating scale that incorporates assessments of ventilatory function. J Neurol Sci. 1999;169:13–21.
- Bach JR. Amyotrophic lateral sclerosis: prolongation of life by non-invasive ventilatory aids. Chest. 2002;122:92–8.
- Sancho J, Servera E, Bañuls P, Marín J. Prolonging survival in amyotrophic lateral sclerosis: efficacy of non-invasive ventilation and uncuffed tracheotomy tubes. Am J Phys Med Rehabil. 2010;89:407–11.
- Donaghy CI, Thurtell MJ, Pioro EP, Gibson JM, Leigh RJ. Eye movements in amyotrophic lateral sclerosis and its mimics: a review with illustrative cases. J Neurol Neurosurg Psychiatry. 2011;82:110–16.
- Kawata A, Mizoguchi K, Hayashi H. A nationwide survey of ALS patients on trachoestomy positive pressure ventilation (TPPV) who developed a totally locked-in state (TLS) in Japan. Rinsho Shinkeigaku. 2008;48:476–80.
- Campbell ML. How to withdraw mechanical ventilation: a systematic review of the literature. AACN Adv Crit Care. 2007;18:397–403.
- Russell JA, Williams MA, Drogan O. Sedation for the imminently dying: survey results from the AAN Ethics Section. Neurology. 2010;74:1303–9.
- McWilliams K, Keeley PW, Waterhouse ET. Propofol for terminal sedation in palliative care: a systematic review. J Palliat Med. 2010;13:73–6.
- Morita T, Tsuneto S, Shima Y. Definition of sedation for symptom relief: a systematic literature review and a proposal of operational criteria. J Pain Symptom Manage. 2002;24:447–53.
- Borasio GD, Voltz R. Discontinuation of mechanical ventilation in patients with amyotrophic lateral sclerosis. J Neurol. 1998;245:717–22.
- Faull C, Rowe Haynes C, Oliver D. Issues for palliative medicine doctors surrounding the withdrawal of non-invasive ventilation at the request of a patient with motor neuron disease: a scoping study. Br Med J Support Palliat Care. 2014;4:43–9.

