Abstract
Our research project computed the direct health costs of patients with amyotrophic lateral sclerosis (ALS) in a Spanish multidisciplinary unit and explored the main factors associated. Besides analyzing a context with universal health care provision, we used an administrative health care dataset from the most crucial center unit treating ALS in Catalonia (80% of total patients). Our results show that the direct health cost of caring for an ALS patient in our unit was 5,158€per patient/year. This cost was not influenced by the onset of the disease, sex or age, but it increased if the patient lived near our center since this facilitates the frequency of follow-up visits. Finally, the higher the educational level, the lower the direct health costs.
Introduction
Amyotrophic lateral sclerosis (ALS) is a fatal neurodegenerative disease characterized by degeneration of the upper and lower motor neurons. It is considered a rare disease (those whose prevalence is below 5 cases per 10,000 inhabitants in the European Community). Rare diseases are usually chronic and progressive, highly disabling, without curative treatment, and difficult to diagnose. They have high mortality and low prevalence. The only treatment approved in Spain is riluzole. This complexity has led to the creation of reference centers with multidisciplinary teams, allowing excellence in management and epidemiological knowledge. Multidisciplinary units for neuromuscular diseases are generally located in major academic centers or tertiary hospitals scattered throughout the territory. The concentration of large numbers of patients in these centers has resulted in clinical expertise, which facilitates appropriate management and improves either survival or quality of life (Citation1–5).
The economic burden of patients with ALS is high, both in terms of direct medical costs to health providers, non-medical costs incurred by patients and their caregivers, and indirect costs through loss of employment. Costs vary over the trajectory of the condition and depend on disease manifestation, progression, and survival duration. There are several studies regarding the costs generated by ALS at reference hospitals. Van der Steen (Citation6) has shown that the cost of specialized care provided and coordinated by ALS care centers was no more significant than the cost of ALS management through non-specialized services. Connolly (Citation7) quantified the health and social care costs of ALS in Ireland and found that the most significant proportion of costs (72%) was in community-based care. Seven per cent of all costs were attributable to assistive devices and appliances, and only 21% of costs were attributable to ALS clinical care services in Ireland. An economic analysis of ALS costs in Australia found that indirect costs exceeded direct health care costs (i.e. costs of care facilities and healthcare professionals) (Citation8). Boylan (Citation9) analyzed direct care costs in 18 centers with public and private care in the USA. The prominent patient cost was related to the professional's salary. It highlighted that the costs related to consultations outside the clinic (mail, SMS, telephone, etc.) involve hours of professional work. In a different context, Song (Citation10) evaluated the costs of the patient treated in Chinese military reference hospitals, which are approximately 1,800€per year, which increases with the evolution of the disease. These costs were related to pharmacy expenses.
We contribute to the scarce evidence of studies examining the health care cost of ALS in multidisciplinary units. Specifically, we calculated the direct health costs of a multidisciplinary ALS unit in a Spanish tertiary center and explored the main factors associated. This research constitutes a novelty in the context of universal health care provision. Additionally, we also contributed by using an administrative health care dataset from the most crucial center unit treating ALS in Catalonia (80% of total patients), including an inventory of costs, disease-specific factors, and socio-demographic information.
Patients and methods
The study design is a cost-of-illness analysis that relates to an inventory of costs for 425 individual patients with ALS treated at Hospital Universitari de Bellvitge using retrospective information for 2016–2019. We considered all patients diagnosed with ALS during this period irrespectively to their diagnosis phenotype and only those costs at the considered tertiary center that accounts for 80% of ALS patients in Catalonia. In Spain, the medical insurance system covers all costs of medical treatment. Then, we estimated associated factors with these direct health costs.
Variables of interest
Collected data corresponds to (i) socio-demographic characteristics (gender, age, nationality, educational levels, and working condition), (ii) direct healthcare costs, which included visits (emergency, nursing care, and medical specialists), laboratory tests, and medical procedures (e.g. capnography, individual respiratory kinesitherapy, spirometry, etc.), and; (iii) strictly related to the disease pharmacological expenditure. Rehabilitation costs were not considered since these costs are not related to the tertiary center. Compared to most previous studies that used survey information (the Spanish case was analyzed in López-Bastida (Citation11)), in 2019, we used analytical costs that the hospital provided. We also considered the date of death if the patient passed away during the considered period. Regarding visits, we accounted for all kinds of visits: initial and follow-up, consultation for hospitalization, palliative, phone consultation, and internal visits for evaluation or follow-up.
Indeed, in order to explore determinants of all healthcare costs run at the multidisciplinary unit plus pharmacological expenses related exclusively to ALS, we considered the following predictors: gender, age (quadratic specification), condition of immigrant status, a dummy variable identifying those patients that passed away during the period (exitus), patient's educational attainment level, working status and a variable representing the distance between the hospital where the unit of analysis is located and the reference hospital. Additionally, we computed and introduced as a covariate a dummy variable identifying those costs and distances to a reference hospital that was, statistically speaking, should be considered outliers (12 patients were identified using the Hadi methodology). The latter allowed us to control for extra tailored expenses in our variable of interest distribution. Then, we ran a further analysis introducing a variable that interacted with exitus status and time from ALS detection and exitus. Next, a patient's residential postcode was used to get a proxy of income in the specific location. In order to do that, we have matched the database with the microdata corresponding to a random sample of declarants of the 2013 income tax provided by the Fiscal Studies Institute. We calculated the average tax base in each postcode, using it as a proxy of income for the patients in that postcode.
Finally, some clinical variables were also considered, such as diagnosis phenotype (aggregated at three level: bulbar onset, spinal onset, and other motor neurone diseases that includes PSMA and PLS), a dummy variable indicating that a genetic analysis was carried out to confirm the disease and the delay in diagnosis (time distance between the date of ALS onset and the first time the patient went into the clinic).
Statistical analysis
We have estimated through regression analysis using a generalized linear model (GLM) that became the dominant strategy for modeling healthcare costs when there are unknown forms of heteroskedasticity (Citation12,Citation13). The log link function and the Gamma distribution are the most frequently used GLM specifications in healthcare cost studies are the log link function and the Gamma distribution (Citation13). We have also compared GLM to alternative specifications such as finite mixture models or a Tobit specification (since costs were censured at the left part of the distribution).
Results
shows the characteristics of the representative patients with ALS in Catalonia. 55% of patients were male, with a predominance of spinal onset forms (52.94%), with a mean diagnostic delay in days of 531.70. The mean distance to the referral center was 36 km. The cultural level of the patients evaluated through education showed that 12.24% had not completed primary education. Up to 41.18% of the patients were retired, and 36.94% were active at work. 86% of patients had a genetic test for c9. The average patient/year direct costs generated in the multidisciplinary unit of 425 patients was 5,158€, although these costs showed a significant variation (see disentangling the sample by educational levels).
Figure 1 Distribution of internal health direct costs by educational level. Note: dashed, solid, and dashed-dot lines refer to primary or less secondary and tertiary educational levels, respectively.
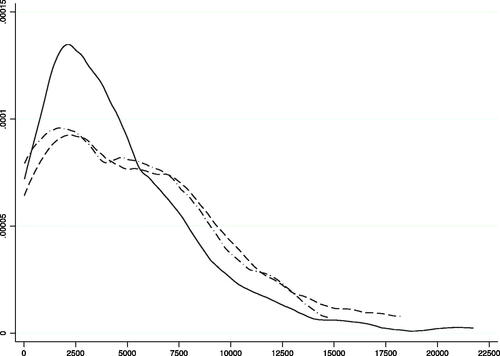
Table 1 Demographic and clinical characteristics.
The ALS multidisciplinary care clinic at hospital Universitari de Bellvitge was established in 2001 to ensure the delivery of continuing care through a dedicated team of specialists (neurologist, pulmonologist, nutritionist, endocrinologist, rehabilitation specialist, physical therapist, psychologist, social worker, nurse manager, speech therapist, and an administrative worker). Patients were seen every three months, with each visit including an assessment of pulmonary function (forced spirometry; home nocturnal pulse oximetry; and arterial blood gas levels) and nutritional status, with early NIMV and placement of a gastrostomy tube advocated as stated in the guidelines of the American Academy of Neurology and the European Federation of Neurological Societies. Out of the 40,865 registers, most frequent categories (above 1%) corresponded to the following specific visits or procedures in descending order of relevance: follow-up visits (22.6%), laboratory and microbiology (12.6%), nursing follow-up visits (8.6%), first visit (4.6%), health education (3.7%), gasometry (3.6%), spirometry (3.1%), phone consultations (3.0%), pulse oximetry (3.0%), urgency visit (2.9%), kinesitherapy (2.2%), pharmacy (1.6%), electromyography (1.5%) and consultations for hospitalization (1.4%).
shows the estimated marginal effects using GLM. The main predictors for direct health costs were if the patient passed away, which relates to end-of-life medical spending that is the main component of aggregate medical expenditure (Citation14) and the link between severity and cost of illness (Citation15). Likewise, another good predictor was the condition of being diagnosed utilizing a genetic test which showed a shorter delay in diagnosis. Finally, the costs increased if the patient lived near the analyzed health care center. The latter relies on the fact that closer distance facilitates the frequency of follow-up visits. Hence, direct health costs were not influenced by the onset of the disease or gender. Educational attainment levels were statistically significant. Indeed, compared to less advantaged patients, having secondary/tertiary education showed lower direct health costs (1,400€–1,500€) after adjusting for the rest of the variables and controlling for outliers.
Table 2 GLM results: marginal effects.
Discussion
Traditionally medicine always omitted evaluation of the socioeconomic factors from its sphere. It even came to consider that these questions opposed the excellent medical practice. Today such an assertion is unsustainable. For a health professional, the path to efficiency passes by assuring clinical effectiveness, in this way guaranteeing both the patient's interest and the suitable distribution of resources.
The socioeconomic burden of ALS on a healthcare system is high, but unfortunately, the available information is limited for all healthcare contexts. An intuitive and widely accepted dogma is that multidisciplinary care clinics cost more to deliver care than standard models. Our results showed that the direct health costs associated with an ALS patient in a multidisciplinary unit were 5,158€per patient/year in the Spanish universal healthcare context. This cost was not influenced by the onset of the disease, sex or age. Notwithstanding, it increased if the patient lived near our center since it facilitated the frequency of follow-up visits. Likewise, costs were associated with the patient's educational level. The more educated they were, compared to incomplete primary and primary, the lower the costs (around 1,400€). There are multiple mechanisms for the effect of socioeconomic status on health. The more educated in general had a healthier lifestyle, and people with better education have better employment opportunities, income, housing, and increasing rates of supplementary health insurance. We believe that people with a higher level of education facilitate health education to be co-responsible in self-care, reducing the number of visits to reference units or the consumption of health resources. Although more extensive studies are needed to confirm this.
The multidisciplinary clinical team consists of a core of health professionals who centralize care and streamline the multiple visits, providing a dynamic and individualized diagnosis and anticipating the orientation and plan of care. Studies have shown that the quality of care delivered in multidisciplinary care is high. Both qualities of life and survival are better in neuromuscular populations treated in multidisciplinary clinics than in isolated neurological clinics. International evidence (Citation16) suggests that multidisciplinary care should be available for ALS people; attending multidisciplinary clinics extends survival, enhances the quality of life, reduces emergency hospital admissions and enhances access to clinical professionals. Multidisciplinary care is an effective and efficient way of managing the disease. The team can recognize disease progression, initiate palliative care discussions, and perhaps even reduce the number of these emergent presentations to the hospital. The objective is to improve survival and be efficient, acceptably use resources, and achieve equal or better effectiveness at a lower cost.
In a healthcare system where the money would follow the patient (i.e. activity-based or capitated population-based funding models), the referral of a complex patient to a highly specialized center should not place an economic burden on the hospital.
Acknowledgements
We wish to thank Miquel Valls Foundation and IDIBELL for supporting us on this project. We thank CERCA Programme/Generalitat de Catalunya for institutional support.
Disclosure statement
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Correction Statement
This article has been republished with minor changes. These changes do not impact the academic content of the article.
References
- Traynor BJ, Alexander M, Corr B, et al. effect of a multidisciplinary amyotrophic lateral sclerosis (ALS) clinic on ALS survival: a population based study, 1996-2000. J Neurol Neurosurg Psychiatry. 2003;74:1258–61.
- Chiò A, Bottacchi E, Buffa C, Mutani R, Mora G. Positive positive effects of tertiary centres for amyotrophic lateral sclerosis on outcome and use of hospital facilities. J Neurol Neurosurg Psychiatry. 2006;77:948–50.
- Zoccolella S, Beghi E, Palagano G, Fraddosio A, Guerra V, Lepore V, et al. ALS multidisciplinary clinic and survival. Results from a population-based study in Southern Italy. J Neurol. 2007;254:1107–12.
- Miller RG, Jackson CE, Kasarskis EJ, England JD, Forshew D, Johnston W, et al. Practice parameter update: the care of the patient with amyotrophic lateral sclerosis: drug, nutritional, and respiratory therapies (an evidence-based review): report of the quality standards subcommittee of the American Academy of Neurology. Neurology 2009;73:1218–26.
- Andersen PM, Abrahams S, Borasio GD, de Carvalho M, Chio A, Van Damme P, et al. EFNS guidelines on the Clinical Management of Amyotrophic Lateral Sclerosis (MALS)-revised report of an EFNS task force. Eur J Neurol. 2012;19:360–75. Mar
- Steen IVD, Berg JPVD, Buskens E, Lindeman E, Van Den Berg LH. The costs of amyotrophic lateral sclerosis, according to type of care. Amyotroph Lateral Scler 2009;10:27–34.
- Connolly S, Heslin C, Mays I, Corr B, Normand C, Hardiman O. Health and social care costs of managing amyotrophic lateral sclerosis (ALS): an Irish perspective. Amyotroph Lateral Scler Frontotemporal Degener. 2015;16:58–62.
- Deloitte Access Economics. Economic analysis of motor neurone disease in Australia, report for Motor Neurone Disease Australia, Deloitte Access Economics, Canberra, November. 2015. Available at: http://www.mndaust.asn.au/Influencing-policy/Economic-analysis-of-MND-(1)/Economic-analysis-of-MND-in-Australia.aspx. Accessed March 30, 2017.
- Boylan K, Levine T, Lomen-Hoerth C, Lyon M, Maginnis K, Callas P, et al. Prospective study of cost of care at multidisciplinary ALS centers adhering to American Academy of Neurology (AAN) ALS practice parameters. Amyotrophic Lateral Sclerosis and Frontotemporal Degeneration. 2016;17:119–27.
- Song H, Liu JC, Cao ZP, Luo WJ, Chen JY. Medical cost and healthcare utilisation of amyotrophic lateral sclerosis in China: a cohort study based on hospital data from 2015 to 2018. Medicine. 2020;99:e23258.
- Lopez-Bastida J, Perestelo-Perez L, Monton-Alvarez F, Serrano-Aguilar P, Alfonso-Sanchez JL. Social economic costs and health-related quality of life in patients with amyotrophic lateral sclerosis in Spain. Amyotroph Lateral Scler 2009;10:237–43.
- Buntin MB, Zaslavsky AM. Too much ado about two-part models and transformation? Comparing methods of modeling Medicare expenditures. J Health Econ. 2004;23:525–42.
- Manning WG, Basu A, Mullahy J. Generalized modeling approaches to risk adjustment of skewed outcomes data. J Health Econ. 2005;24:465–88.
- French EB, McCauley J, Aragon M, Bakx P, Chalkley M, Chen SH, et al. End-of-life medical spending in last twelve months of life is lower than previously reported. Health Affairs. 2017;36:1211–7.
- Meng L, Bian A, Jordan S, Wolff A, Shefner JM, Andrews J. Profile of medical care costs in patients with amyotrophic lateral sclerosis in the Medicare programme and under commercial insurance. Amyotrophic Lateral Sclerosis and Frontotemporal Degeneration. 2018;19:134–42.
- Van den Berg JP, Kalmijn S, Lindeman E, Veldink JH, de Visser M, Van der Graaff MM, et al. Multidisciplinary ALS care improves quality of life in patients with ALS. Neurology 2005;65:1264–7.

