 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Background
We aimed to evaluate the intra-rater reliability in 30-second chair stand test (30CST) as a self-test, and the inter-rater reliability comparing a self-test with a physiotherapist-assessed 30CST for patients with knee osteoarthritis (KOA). The second purpose was to evaluate the classification ability of the 30CST as self-test to distinguish between reduced physical function and normal function.
Methods
Patients with KOA performed two self-tests of 30CST at home and thereafter a physiotherapist assessed the patient. Absolute agreements were presented with intraclass correlation coefficient (ICC), 95% confidence interval (CI) and standard error of measurement (SEM). Post-hoc analyses were conducted to calculate minimal detectable change (MDC). The classification ability was analysed with receiver operating characteristic (ROC)-curves and area under the ROC-curve (AUC). The significance level was p < 0.05.
Results
In total, 114 followed the protocol. Intra-rater and inter-rater reliability were good (ICC 0.97, CI 0.95–0.99, SEM 0.89 and ICC 0.81, CI 0.72–0.87, SEM 2.29 respectively). MDC were 2.5 stands when comparing self-test results individually and 0.23 on a group level. The MDC between self-tests and physiotherapist assessment were 6.4 stands for individual comparison and 0.59 for group comparison. The self-test was 80% likely to detect reduced physical function compared to a physiotherapist assessing physical function with 30CST (AUC = 0.79–0.80).
Conclusions
The results indicate that 30CST can be a reliable self-assessment of physical function in lower extremities for patients with KOA. These findings can be useful in areas such as self-screening for reduced physical function, self-assessment in digital physiotherapy, and as measurement in research projects.
Introduction
Osteoarthritis (OA) symptoms are one of the main reasons for consulting primary healthcare [Citation1]. Globally, it is estimated that 23% of people aged 40 or over suffer from knee OA (KOA) [Citation2], and in Sweden, 14% of the population over 45 years old [Citation3]. Common symptoms are pain, joint stiffness, and impaired physical function [Citation4]. Patients with KOA tend to seek care when their physical function is getting worse [Citation5] or when the pain is unbearable [Citation6]. Pain-related avoidance of activities can lead to activity limitations among patients with KOA [Citation7–9]. A negative spiral of physical deconditioning could occur where pain avoidance leads to muscle weakness [Citation8,Citation10], which can lead to further activity limitations [Citation9,Citation10]. For patients with KOA, the pre-phase before contacting healthcare involves affected body function and impacts activities and participation according to the International Classification of Functioning, Disability and Health (ICF) [Citation11]. Most patients with OA (79%) had stopped or reduced their physical activities due to their OA [Citation6].
Today, physical function can be assessed with self-reported questionnaires or performance-based measurements [Citation12]. Performance-based tests are often used to measure how much the patients actually can perform as opposed to how much pain they experience during the activity [Citation13]. When comparing self-reporting scales with performance-based tests, the latter have been shown to better distinguish between pain and physical function [Citation14]. The performance-based tests are usually assessed in the clinic and supervised by healthcare personnel.
The 30-second chair stand test (30CST) is one of the recommended tests for assessing physical function for patients with KOA [Citation15]. The 30CST has an excellent intra-session reliability (intraclass correlation (ICC) > 0.9) for patients with KOA [Citation16–18], but is lacking in construct validity and responsiveness [Citation19]. This performance test is applicable for a wide range of physical function abilities [Citation20] and might be useful for patients to self-evaluate their level of physical function, for example, in digital healthcare and in research projects. Former research has evaluated the 30CST using technical devices for self-assessment, such as smartphone applications [Citation21,Citation22], accelerometer-derived metrics to detect falls [Citation23], and in videoconferencing [Citation24]. These studies were conducted in healthy individuals or patients with multiple sclerosis, cancer and OA [Citation21–24]. To the best of our knowledge, the research about 30CST as self-test without technical devices for patients with KOA appears to be limited.
To determine if 30CST is feasible as a self-test when assessing physical function among patients with KOA, we conducted a reliability study with the primary aim to evaluate the intra-rater reliability, and the inter-rater reliability in self-tests compared to a physiotherapist assessing 30CST. The secondary aim was to analyse whether a self-test of 30CST could detect reduced physical function as well as physiotherapist assessment.
Material and methods
Study design
A reliability study was conducted between 27th February 2019 and 25th July 2023 in rehabilitation centres in primary healthcare in south-western Sweden. During 2022, two rehabilitation centres withdrew their participation in this study and two new rehabilitation centres were introduced to the study. All participants approved with written informed consent. The manuscript is reported according to COSMIN reporting guideline for measurement properties of patient-reported outcome measures [Citation25] and Guidelines for Reporting Reliability and Agreement Studies (GRRAS) [Citation26].
Sample size
The sample size was calculated with the statistical program Power Analysis and Sample Size (PASS), version 16 [Citation27]. For two observations per participant in respectively reliability analysis, i.e. comparing two self-tests for intra-rater reliability, or two observations including one self-test and one physiotherapist assessment for inter-rater reliability, 117 participants deemed necessary to achieve 80% power to detect an ICC of 0.8 with a significance level at p < 0.05. With an expected dropout rate of 20%, 147 patients were planned to be recruited to the study.
Eligibility criteria
Participants were recruited from five rehabilitation centres in primary healthcare in southwestern Sweden. Patients with KOA, regardless severity, with ongoing rehabilitation were asked to participate in this study. The KOA could have been diagnosed based on symptoms and did not have to be verified with radiography. Participants could have been diagnosed either by a physiotherapist or physician in primary care. Eligible participants were screened by the treating physiotherapist. The participants could have OA in other joints in the lower extremities, but the KOA needed to be the most troublesome. The participants had to be independent in walking (with or without walking aids) and understand Swedish orally and in written text. Exclusion criteria were neurological diseases, severe somatic or psychiatric disorders that negatively affected the physical function or balance, knee or hip arthroplasty the past six months, or other knee surgery that could result in reduced physical function.
Data collection
Self-assessment
Maximum 14 days prior to the physiotherapist assessment, the participants received an envelope containing questionnaires about demographic data, patient reported outcome measures (described below), and instructions for the self-test of 30CST. All questionnaires were answered at the participant’s home including the self-tests, and then brought back to the physiotherapist. Self-reported demographic data included age, gender, origin, and educational level. Health data included KOA duration, co-morbidities (OA in other joints, heart diseases, diabetes mellitus, rheumatic diseases, mental illness, or other disease), pain location, pain intensity, knee pain duration, pain experience and physical function in daily activities. Pain locations were measured with self-administrated pain drawing on 18 pre-specified body areas [Citation28]. To assess pain experience, the Swedish version of Intermittent and Constant OA Pain (ICOAP) knee questionnaire were used. The ICOAP consists of two subscales where one part is focused on intermittent pain and the other part on constant pain. The total score is ranging between 0–100 where 0 represents no pain and 100 extreme pain [Citation29]. The Swedish version of Knee Injury and Osteoarthritis Outcome Score – Physical function Short form (KOOS-PS) was used to capture how the participants experienced difficulties in physical function in knee related activities. The KOOS-PS score ranges between 0 and 100 where 0 represents severe difficulties and 100 no difficulties [Citation30].
The 30CST was performed on an approximately 45 cm high chair without arm support. The participant was encouraged to do as many stands as possible during 30 s of time. The start position was sitting on the chair. The stands were counted if the participant rose fully (straight hips and knees), and returned to sitting position. The arms were folded across the chest during the whole test [Citation16]. The pain intensity was measured before and directly after the tests (pain intensity during testing) using a numeric rating scale (NRS) 0–10, where 0 represents no pain and 10 worst imaginable pain [Citation31].
The test manual described how the 30CST should be performed, see Appendix 1, supplemental material. To minimise fall risk, participants were instructed to place the chair against a wall and have a table or similar in front of themselves. The participants were asked to do two measurements with maximum two days in between. No instructions were given regarding time of day. The second measurement (self-test 2) should be maximum one week prior to the physiotherapist assessment. The results of the self-tests were in a concealed envelope and brought to the physiotherapist at a scheduled follow-up appointment.
Physiotherapist assessment
The physiotherapists were blinded to the self-test results during the assessment and used the same manual as for the self-test. They opened the closed envelope after the assessment to attach the physiotherapist assessment results. All physiotherapists were instructed and trained by the main author (CHH) regarding study protocol, 30CST and safety considerations regarding chair position before assessment. Weight and body length were measured by the physiotherapist to calculate a body mass index (BMI).
Statistical analyses
Demographic data is presented with mean and standard deviations (SD), median and 25th and 75th percentiles, or numbers and percentage. Median values were imputed for missing data about number of days between each test. Absolute agreement is presented with ICC, 95% confidence interval (CI) and standard error of measurement ()) for both intra- and inter-rater reliability. The SEM is calculated with the mean SD from the two tests included in the ICC analysis. Based on the SEM, post-hoc analyses of minimal detectable change (MDC) were calculated to present on an individual level (MDCind= 1.96 × √2 × SEM) and group level (MDCgroup= MDCind/√n) [Citation32]. Intra-rater reliability for the self-test (test 1 and test 2) were analysed with two-way mixed effects model and inter-rater reliability between the participant’s self-test (test 2) and the physiotherapist assessment were analysed with two-way random-effects model [Citation33]. ICC less than 0.5 was considered as poor reliability, 0.5–0.75 as moderate reliability, and ICC above 0.75 as good reliability [Citation34]. If more than 15% of participants should score zero on the test, the results would be interpreted as a floor effect [Citation32].
Classification ability of 30CST as self-test
The results of the 30CST, self-tests and physiotherapist assessment, were classified for each participant according to reference values of the 30CST for a healthy population, where values below the reference standards were classified as ‘reduced physical function’, see [Citation35,Citation36] and ‘normal physical function’ if equal or over the reference value. Logistic regression analyses were performed to evaluate whether the self-test (independent variable) could detect a reduced physical function as well as physiotherapist assessment (dependent variable). The analysis is adjusted for age and gender [Citation35,Citation36]. The sensitivity and specificity of the logistic regression models is illustrated with receiver operating characteristic (ROC)-curves and presented with areas under the ROC-curves (AUC) to distinguish between reduced physical function or not with a self-test. The AUC can range from 0 to 1 where values less than 0.5 are interpreted as equal to random classification, ≥ 0.5 fail, ≥ 0.6 poor, ≥ 0.7 fair, ≥0.8 good and ≥ 0.9 excellent classification ability [Citation37]. The ROC-curve illustrates the relationship between the sensitivity (y-axis) and 1-specificity (x-axis) of possible cut-off values, and suggested cut-off values for the self-tests together with its classification ability is presented. The analyses were applied with a significance level of p < 0.05 and conducted in Statistical Package for Social Sciences (SPSS) version 28 [Citation38].
Table 1. Reference values for 30 s chair stand test [Citation35,Citation36].
Results
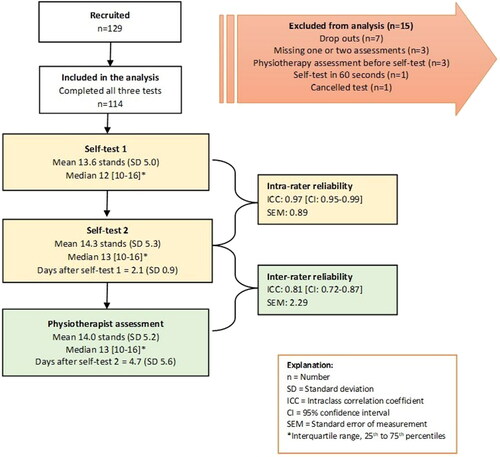
In total, 129 participants were recruited during 2019 to 2023, whereof 114 completed all three assessments. The mean age was 69 years (SD 8.7), the majority were overweight or obese (80%), and most participants were women (58%), born in Sweden (94%) and had finished high school (71%), see . Average pain duration was more than three years and nearly half had their KOA diagnosis longer than a year. Nearly a fifth had OA in other joints and 59% suffered from another disease. The ICOAP scores indicated mild symptoms. The participants’ knee related physical function was moderately affected, see . The most reported pain site was the right knee (69%), followed by the left knee (63%) and lumbar pain (41%). More than a third had bilateral knee pain (37%), 67% had three or more pain sites and 48% had at least four pain sites.
Table 2. Patient characteristics (n = 114).
Twenty-one physiotherapists assessed the participants and they had varying levels of clinical experience (range < 1 to > 30 years). Mean chair stands for the first self-test were 13.6 (SD 5.0) stands, 14.3 (SD 5.3) for the second self-test and 14.0 (SD 5.2) when assessed by a physiotherapist. The mean chair height differed one cm between self-tests and physiotherapist assessment, 46 cm (SD 1.4) respectively 45 cm (SD 0.7). The self-tests were performed two days apart (SD 0.9), and five days (SD 5.6) elapsed between the second self-test and the physiotherapist assessment. Average pain intensity was lower when a physiotherapist asked about it before (2.3 (SD 2.2) vs. 2.9 (SD 2.1)), and during the test (3.1 (SD 2.5) vs. 3.8 (SD 2.4)) than self-reported in the self-tests. Most participants managed to perform the 30CST without arm support, and less than 1% cancelled the test. None performed 0 on the self-tests nor when supervised by a physiotherapist. The first self-test detected 73 (64%) participants with reduced physical function, while the second self-test resulted in 63 (55%), and the physiotherapist assessment detected 63 (55%). The ICCs were good, 0.97 (CI [0.95–0.99], SEM 0.89) for intra-rater reliability and 0.81 (CI [0.72–0.87], SEM 2.29) inter-rater reliability. See .
Figure 1. Flow chart of participants and analysis for intra- and inter-rater reliability of 30-second chair stand test (30CST).
Converting SEM into MDC, shows that the MDCind would be 6.4 and for MDCgroup 0.59 when comparing self-test results with physiotherapists’ results. The MDCind for intra-reliability of the self-tests was 2.5 and when interpreting on a group level the MDCgroup was 0.23. Mean change for self-tests were −0.73 stands (SD 1.5), and +0.33 (SD 4.3) comparing self-test with physiotherapist assessment. Further, 14% of the sample has a detectable change between the self-tests and 7% had a change between the self-test and physiotherapist assessment.
Classification ability of 30CST as self-test
The classification ability of the self-tests to distinguish between reduced or not reduced physical function as determined by a physiotherapist was fair to good (AUC: self-test 1: 0.79; self-test 2: 0.80, both p < 0.01) (). A cut-off value of 12.5 stands in 30CST had a 75% sensitivity and 74% specificity for self-test 1, respectively 13.5 stands for self-test 2 (75% sensitivity and 72% specificity).
Figure 2. (a,b) Receiver operating characteristic (ROC)-curve analysis of 30-second chair stand test (30CST) to classify reduced physical function. (A) self-test 1, (B) self-test 2. Reduced physical function was categorised through normative values [Citation35,Citation36].
![Figure 2. (a,b) Receiver operating characteristic (ROC)-curve analysis of 30-second chair stand test (30CST) to classify reduced physical function. (A) self-test 1, (B) self-test 2. Reduced physical function was categorised through normative values [Citation35,Citation36].](/cms/asset/5f39014e-8556-4e7f-a4a8-0cd544e1372c/iejp_a_2337419_f0002_b.jpg)
Discussion
Our results suggest that 30CST is a reliable test for self-assessment of physical function in patients with KOA. We showed that the self-test has good intra- and inter-reliability (ICC >0.80), and seem feasible to use in a home setting. The diagnostic ability of the self-test has fair to good classification ability to distinguish between reduced physical function and normal function (AUC > 0.79–0.80). Performance of less than 12 stands on 30CST could be classified in clinical situations as reduced physical function for patients with KOA regardless of age or gender. Our results support Bowman et al. [Citation24], who report that the 30CST is a safe test to perform without supervision, i.e. for people without balance insufficiencies. These results add to the evidence of using performance tests as self-tests [Citation24]. A reliable and safe to use self-test could be valuable in a digital setting, which would be helpful in the emerging new area of digital physiotherapy [Citation39].
Similar to previous reliability studies, the intra-reliability was good [Citation17–19,Citation40] and SEM around one repetition [Citation18,Citation19]. The high ICC values might be biased by awareness of previous self-test results, and that the time period between the self-tests could be too short to forget about the results. Also, filling out the results digitally would minimise the risk of striving for the same or better results as before. Further, the pain levels reported before the tests indicated that the KOA symptoms were similar before the testing. There was slightly lower pain intensity at physiotherapist assessment compared to the self-tests, yet the number of stands were not affected.
The results of inter-reliability were lower than previous studies [Citation16,Citation40]. Our study was performed in a clinical environment, with a high number of assessors with a wide range of clinical experience, ranging from less than one year to more than 30 years of practice, which may contribute to the difference in results, but reflecting clinical practice. However, all assessors were instructed by CHH to reduce variability in assessment. Another possible factor affecting the ICC value might have been that 13% had the physiotherapist assessment more than seven days after the self-test, and some may have had treatment, i.e. home exercise, during this time. This might have affected the physical function of these patients. Despite the methodological limitations, we believe that it is unlikely that the short treatment period of two weeks could result in increased physical function, which is confirmed by the difference between self-test 2 and physiotherapist assessment (mean 14.3 respectively 14.0 stands). Slightly higher chair heights in the self-tests (range 43–50 cm; physiotherapist range 43–48 cm) and possible issues in how the self-test is performed such as feet position or leaning against the back of the chair, the type of chair used (soft or hard surface), counting (including or excluding last half stand) and timing alone may also have affected the results. Of practical reasons, the accuracy of the performance of self-tests were not checked. However, it can be assumed that the individual variations are similar for both performances of the self-test. Despite this, the inter-reliability was good, ICC >0.80.
To increase the generalisability of the study, we chose a pragmatic setting to reflect the daily primary care for patients with KOA. Recruited patients had a wide range of symptoms, from symptoms of KOA only to multiple pain sites, former surgery and comorbidities. This is in accordance with the clinical appearance. More than half (67%) had pain in more than three sites, one out of five had OA in another joint (21%), and 67% had at least one comorbidity, which is similar to previous study reporting 72% having one comorbidity or more, although a higher rate of multi-joint OA (92%) [Citation41].
When evaluating treatment effects with mixed assessment of 30CST, i.e. using both self-tests and physiotherapist assessment, our results indicate that a difference of at least six stands is needed to consider it a change in physical function. Using self-tests only require less stands to detect a change in physical function, which is in agreement with previous studies of patients with KOA and hip OA; 2.4–2.7 stands [Citation18,Citation19,Citation42].
The instructions for the self-tests were intended to be brief and easy to understand. Thus, we did not specify any time of the day that the tests were going to be performed. This might have affected the 30CST results since pain levels can vary during the day or worsen after a whole day of weight-bearing activities. However, the lowest mean level of pain intensity in this study was lower than that seen in other reliability studies [Citation18,Citation19,Citation40], and our results in 30CST did not differ from other studies [Citation16–19,Citation40].
The previously reported lack of construct validity in 30CST [Citation19], might affect the analyses of the classification ability. In this study, 15 participants (13%) were under the age of 60. Broad reference values for people below the age of 60 was used [Citation36], and we did not use specific reference values with 10-year intervals between 20-year-olds and 59-year-olds making the difference between reference values for 55–59-year-olds and 60–64-year-olds unreasonably large [Citation35,Citation36]. This may have resulted in some of the younger participants being compared to reference values which were too high [Citation35]. Hence, analyses based on reference values in 5–10-year intervals for patients between 35 and 60 years of age are needed. In this study, the reference values used might have affected the number of patients classified with reduced physical function, and the ROC-curves from this study should be interpreted with caution for patients under 60 years. Additional analyses excluding patients 59 years of age or younger increased the AUC slightly to 0.84, and the sensitivity of the cut-off values 12.5 respectively 13.5 of self-test 1 and 2 increased to 82–86% and the sensitivity decreased to 70–72%, see Appendix 2, supplemental material. Caution should also be applied for patients over 80 years since the number of patients in this age interval were few.
Limitations
Our calculated sample size of 147 was not reached. This study started in 2019, and the recruitment period lasted almost four years, where two years were affected by the COVID-19 pandemic. During the pandemic, patients over 60 years of age were not allowed to visit the rehabilitation centres. Therefore, the inflow of patients with KOA was very low. Based on the estimated sample size to attain 80% power, the data collection was closed when 117 patients had completed all three tests for the reliability analysis, i.e. two self-tests followed by a physiotherapist assessment. However, three participants were excluded from analysis because the physiotherapist assessments were performed before the self-tests. Further, the cut-off value of 12 stands may not be applicable for patients over 80 years of age as the reference values are below 12 stands, and future research with a larger sample size for this age group is needed.
Conclusion
This study shows a good intra- and inter-rater reliability for 30CST as a self-test for patients with KOA which adds to the previous evidence of 30CST as a reliable measurement. Our results indicate that 30CST can be a reliable method of self-assessment of physical function in lower extremities for patients with KOA and can be useful in many areas, such as self-screening for reduced physical function, self-assessment in digital physiotherapy, and as measurement in research projects.
Ethical approval
The Swedish Ethical Review Authority approved the study, reference number: 2019-00784/1236-18, and amendment 2022-05340-02, and the study was prospectively registered 27th February 2019 in clinicaltrials.gov: NCT03855813.
Supplemental Material
Download Zip (48.3 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Decoded data are available on reasonable request.
Additional information
Funding
References
- Finley CR, Chan DS, Garrison S, et al. What are the most common conditions in primary care? Systematic review. Can Fam Physician. 2018;64(11):832–840.
- Cui A, Li H, Wang D, et al. Global, regional prevalence, incidence and risk factors of knee osteoarthritis in population-based studies. eClinicalMedicine. 2020;29–30:100587. doi:10.1016/j.eclinm.2020.100587.
- Turkiewicz A, Petersson IF, Björk J, et al. Current and future impact of osteoarthritis on health care: a population-based study with projections to year 2032. Osteoarthritis Cartilage. 2014;22(11):1826–1832. doi:10.1016/j.joca.2014.07.015.
- National Board of Health and Welfare. National guidelines for musculoskeletal diseases. Rheumatoid arthrtis, axial spondylarthritis, psoriatic arthritis, osteoarthritis and osteoporosis. Support for governance and management 2021 [Nationella riktlinjer för rörelseorganens sjukdomar. Reumatoid artrit, axial spondylartrit, psoriasisartrit, artros och osteoporos. Stöd för styrning och ledning 2021] 2021. https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/nationella-riktlinjer/2021-1-7137.pdf
- Thorstensson CA, Gooberman-Hill R, Adamson J, et al. Help-seeking behaviour among people living with chronic hip or knee pain in the community. BMC Musculoskelet Disord. 2009;10(1):153. doi:10.1186/1471-2474-10-153.
- Conaghan PG, Porcheret M, Kingsbury SR, et al. Impact and therapy of osteoarthritis: the arthritis care OA nation 2012 survey. Clin Rheumatol. 2015;34(9):1581–1588. doi:10.1007/s10067-014-2692-1.
- Holla JFM, van der Leeden M, Heymans MW, et al. Three trajectories of activity limitations in early symptomatic knee osteoarthritis: a 5-year follow-up study. Ann Rheum Dis. 2014;73(7):1369–1375. doi:10.1136/annrheumdis-2012-202984.
- Holla JFM, van der Leeden M, Knol DL, et al. Avoidance of activities in early symptomatic knee osteoarthritis: results from the CHECK cohort. Ann Behav Med. 2012;44(1):33–42. doi:10.1007/s12160-012-9353-x.
- Pisters MF, Veenhof C, van Dijk GM, et al. The course of limitations in activities over 5 years in patients with knee and hip osteoarthritis with moderate functional limitations: risk factors for future functional decline. Osteoarthritis Cartilage. 2012;20(6):503–510. doi:10.1016/j.joca.2012.02.002.
- Dekker J, van Dijk GM, Veenhof C. Risk factors for functional decline in osteoarthritis of the hip or knee. Curr Opin Rheumatol. 2009;21(5):520–524. doi:10.1097/BOR.0b013e32832e6eaa.
- World Health Organization. International classification of functioning, disability, and health: ICF. 2001. https://www.who.int/classifications/international-classification-of-functioning-disability-and-health
- Jordan KP, Wilkie R, Muller S, Arthritis Research Campaign National Primary Care C., et al. Measurement of change in function and disability in osteoarthritis: current approaches and future challenges. Curr Opin Rheumatol. 2009;21(5):525–530. doi:10.1097/BOR.0b013e32832e45fc.
- Terwee CB, Mokkink LB, Steultjens MP, et al. Performance-based methods for measuring the physical function of patients with osteoarthritis of the hip or knee: a systematic review of measurement properties. Rheumatology. 2006;45(7):890–902. doi:10.1093/rheumatology/kei267.
- Stratford PW, Kennedy DM, Woodhouse LJ. Performance measures provide assessments of pain and function in people with advanced osteoarthritis of the hip or knee. Phys Ther. 2006;86(11):1489–1496. doi:10.2522/ptj.20060002.
- Dobson F, Hinman RS, Roos EM, et al. OARSI recommended performance-based tests to assess physical function in people diagnosed with hip or knee osteoarthritis. Osteoarthritis Cartilage. 2013;21(8):1042–1052. doi:10.1016/j.joca.2013.05.002.
- Gill SD, McBurney H. Reliability of performance-based measures in people awaiting joint replacement surgery of the hip or knee. Physiother Res Int. 2008;13(3):141–152. doi:10.1002/pri.411.
- Holm PM, Nyberg M, Wernbom M, et al. Intrarater reliability and agreement of recommended performance-based tests and common muscle function tests in knee osteoarthritis. J Geriatr Phys Ther. 2021;44(3):144–152. doi:10.1519/JPT.0000000000000266.
- Gill S, Hely R, Page RS, et al. Thirty second chair stand test: test-retest reliability, agreement and minimum detectable change in people with early-stage knee osteoarthritis. Physiother Res Int. 2022;27(3):e1957. doi:10.1002/pri.1957.
- Tolk JJ, Janssen RPA, Prinsen CAC, et al. The OARSI core set of performance-based measures for knee osteoarthritis is reliable but not valid and responsive. Knee Surg Sports Traumatol Arthrosc. 2019;27(9):2898–2909. doi:10.1007/s00167-017-4789-y.
- Jones CJ, Rikli RE, Beam WC. A 30-s chair-stand test as a measure of lower body strength in Community-Residing older adults. Res Q Exerc Sport. 1999;70(2):113–119. doi:10.1080/02701367.1999.10608028.
- Lein DH, Jr., Willig JH, Smith CR, et al. Assessing a novel way to measure three common rehabilitation outcome measures using a custom mobile phone application. Gait Posture. 2019;73:246–250. doi:10.1016/j.gaitpost.2019.07.251.
- Adusumilli G, Joseph SE, Samaan MA, et al. iPhone sensors in tracking outcome variables of the 30-Second chair stand test and stair climb test to evaluate disability: cross-Sectional pilot study. JMIR Mhealth Uhealth. 2017;5(10):e166. doi:10.2196/mhealth.8656.
- Tulipani LJ, Meyer B, Allen D, et al. Evaluation of unsupervised 30-second chair stand test performance assessed by wearable sensors to predict fall status in multiple sclerosis. Gait Posture. 2022;94:19–25. doi:10.1016/j.gaitpost.2022.02.016.
- Bowman A, Denehy L, Benjemaa A, et al. Feasibility and safety of the 30-second sit-to-stand test delivered via telehealth: an observational study. Pm R. 2023;15(1):31–40. doi:10.1002/pmrj.12783.
- Gagnier JJ, Lai J, Mokkink LB, et al. COSMIN reporting guideline for studies on measurement properties of patient-reported outcome measures. Qual Life Res. 2021;30(8):2197–2218. doi:10.1007/s11136-021-02822-4.
- Kottner J, Audigé L, Brorson S, et al. Guidelines for reporting reliability and agreement studies (GRRAS) were proposed. J Clin Epidemiol. 2011;64(1):96–106. doi:10.1016/j.jclinepi.2010.03.002.
- NCCS LLC. PASS 16 power analysis and sample size software. 16th ed. Kaysville, Utah: NCCS LLC; 2018.
- Bergman S, Herrström P, Högström K, et al. Chronic musculoskeletal pain, prevalence rates, and sociodemographic associations in a swedish population study. J Rheumatol. 2001;28:1369–1377.
- Hawker GA, Davis AM, French MR, et al. Development and preliminary psychometric testing of a new OA pain measure–an OARSI/OMERACT initiative. Osteoarthritis Cartilage. 2008;16(4):409–414. doi:10.1016/j.joca.2007.12.015.
- Perruccio AV, Stefan Lohmander L, Canizares M, et al. The development of a short measure of physical function for knee OA KOOS-Physical function shortform (KOOS-PS) - an OARSI/OMERACT initiative. Osteoarthritis Cartilage. 16(5):542–550. doi:10.1016/j.joca.2007.12.014.
- Downie WW, Leatham PA, Rhind VM, et al. Studies with pain rating scales. Ann Rheum Dis. 1978;37(4):378–381. doi:10.1136/ard.37.4.378.
- Terwee CB, Bot SDM, de Boer MR, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60(1):34–42. doi:10.1016/j.jclinepi.2006.03.012.
- Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15(2):155–163. doi:10.1016/j.jcm.2016.02.012.
- Portney LG, Watkins MP. Foundations of clinical research: applications to practice. 3rd ed. New York, NY: mcGraw-Hill Education; 2009.
- Rikli RE, Jones CJ. Development and validation of criterion-referenced clinically relevant fitness standards for maintaining physical independence in later years. Gerontologist. 2013;53(2):255–267. doi:10.1093/geront/gns071.
- McKay MJ, Baldwin JN, Ferreira P, et al. Reference values for developing responsive functional outcome measures across the lifespan. Neurology. 2017;88(16):1512–1519. doi:10.1212/WNL.0000000000003847.
- Nahm FS. Receiver operating characteristic curve: overview and practical use for clinicians. Korean J Anesthesiol. 2022;75(1):25–36. doi:10.4097/kja.21209.
- IBM Corp. IBM SPSS statistics for windows. 22.0 ed. Armonk, NY: IBM Corp.; 2013.
- Bernhardsson S, Larsson A, Bergenheim A, et al. Digital physiotherapy assessment vs conventional face-to-face physiotherapy assessment of patients with musculoskeletal disorders: a systematic review. PLoS One. 2023;18(3):e0283013. doi:10.1371/journal.pone.0283013.
- Suwit A, Rungtiwa K, Nipaporn T. Reliability and validity of the osteoarthritis research society international minimal core set of recommended performance-based tests of physical function in knee osteoarthritis in Community-Dwelling adults. Malays J Med Sci. 2020;27(2):77–89. doi:10.21315/mjms2020.27.2.9.
- Gay C, Guiguet-Auclair C, Mourgues C, et al. Physical activity level and association with behavioral factors in knee osteoarthritis. Ann Phys Rehabil Med. 2019;62(1):14–20. doi:10.1016/j.rehab.2018.09.005.
- Tolk JJ, Janssen RPA, Prinsen C, et al. Measurement properties of the OARSI core set of performance-based measures for hip osteoarthritis: a prospective cohort study on reliability, construct validity and responsiveness in 90 hip osteo-arthritis patients. Acta Orthop. 2019;90(1):15–20. doi:10.1080/17453674.2018.1539567.

