Abstract
Background
Applying an appropriate physiotherapy intervention to a hospitalised patient can be challenging because the clinical status can change rapidly, affecting the patient’s physical capacity. Determining the appropriate type and dose of the physiotherapy intervention requires dynamic assessment of physical capacity and adequate clinical reasoning by the physiotherapist.
Purpose
To develop a framework for determining physical capacity to support physiotherapists in their clinical reasoning process when treating hospitalised patients.
Methods
A framework was developed using a multi-method approach. First, the scientific literature was searched for existing frameworks for clinical reasoning in physiotherapy. These methods were inventoried and relevant elements were extracted. Second, a first draft of the framework was developed by a group of experts. Third, the framework was tested in practice, leading to a final version.
Results
A total of 17 frameworks were identified from the literature. No framework was found for generic use in the hospital for the purpose of determining patient’s physical capacity. Relevant elements from the identified frameworks were: the use of ICF terminology, the use of a patient management model, and frequent monitoring of clinical parameters. Field testing of the first draft of the framework led to improvement of the framework for use in clinical practice.
Conclusion
A framework was developed to support physiotherapists in their clinical reasoning process when treating hospitalised patients. The framework can provide guidance for determining the patient’s physical capacity to allow for an adequate training stimulus.
Introduction
Early mobilisation and exercise training are important physiotherapy interventions for many hospitalised patients. They can reduce the risk of complications and length of stay, and increase the patient’s functional independence at discharge [Citation1–5]. However, applying these interventions is often challenging [Citation6,Citation7], because the patient may be medically unstable and exhibit rapid changes in clinical status. During hospitalisation, clinical factors including hemodynamic and respiratory stability, neurological status, and the patient’s mental and cognitive status, can change hourly and affect the patient’s physical capacity [Citation8]. Physical capacity, embodying concepts such as strength, range of motion, endurance and balance, is a key pathway through which individuals maintain their ability to carry out activities [Citation9].
A repetitive assessment of physical capacity and adequate clinical reasoning by the physiotherapist (PT) is necessary to determine the appropriate type and dose of the physiotherapy intervention during hospitalisation. In addition to clinical factors, environmental factors (the physical, social and attitudinal environment in which people live) and personal factors (e.g. age, coping style, level of education) are also important to include into the clinical reasoning process [Citation10,Citation11]. To support the clinical reasoning of hospital-based PTs, a framework that takes into account the various factors that influence a patient’s physical capacity could be useful in structuring the clinical reasoning process. Making the complex process of clinical reasoning transparent could help to reduce the variation between PT's and facilitate clearer communication between PTs and other healthcare professionals about a patient’s physical capacity and the resulting training options. In addition, such a framework could play a role in the educational and professional development of PTs [Citation7,Citation10].
To our current knowledge, there is no framework available that can be used by PTs for all admitted patients to determine the patient’s physical capacity in order to apply an appropriate training stimulus based on it. Well-known and widely used clinical reasoning models used by PTs in various settings are the Hypothesis-Oriented Algorithm for Clinicians (HOAC), the REHAB cycle, and a clinical reasoning model based on the International Classification of Functioning, Disability and Health (ICF) [Citation10,Citation12,Citation13]. These hypothesis-oriented models provide systematic guidance for treating patients and are designed for use in all settings [Citation14–16]. However, these models are comprehensive, making them less practical for use in a hospital setting. Because of the lack of specificity for the hospital setting, specific frameworks have been developed for clinical decision support regarding early mobilisation therapy in the intensive care unit [Citation1,Citation17] and for the physiotherapy management of COPD patients in the hospital [Citation6]. However, these frameworks are not applicable to other patient groups during hospitalisation. Since determining the patient’s physical capacity is a common part of physiotherapy practice in the hospital, it might be helpful for PTs to have a generic guidance for this.
Therefore, the purpose of this study was to develop a framework for determining physical capacity to support PTs in their clinical reasoning process when treating hospitalised patients. The framework should reflect the complex and dynamic physical capacity of the patient, facilitate uniform communication, and support professional education.
Methods
We used a multi-method approach, consisting of a literature search, discussions with experts and field-testing. The Medical Research Council (MRC) framework for complex interventions was used to guide the development of the framework by distinguishing between a theoretical phase, a modelling phase and an exploratory phase [Citation18]. The evaluation and implementation phase of the MRC framework are beyond the scope of the current study.
Theoretical phase: Comprehensive literature search
In order to provide a theoretical basis for the development of the physical capacity framework, this phase involves (1) a comprehensive review of the scientific literature on existing frameworks for clinical reasoning in physiotherapy and rehabilitation, and (2) the identification of key elements from these frameworks that could be relevant for the development of our physical capacity framework. Specific questions for the comprehensive literature search were:
Which frameworks are used to support clinical reasoning in physiotherapy and rehabilitation?
What are the key elements where these frameworks are based on?
To conduct the comprehensive literature review, we used the PRISMA statement as a guide [Citation19]. We did not perform a systematic review, but the PRISMA 2020 flow diagram and item checklist were used where applicable. A search was conducted in PubMed in June 2019 and updated in April 2021. The search strategy was determined by two members of the core team (ML and JB). The search included MESH terms as well as all field terms. The search as performed in PubMed is listed in Box 1. Additional literature was identified by citation searching.
Since the objectives of our literature search were not limited to in-hospital physiotherapy treatment, the search term ‘rehabilitation’ was incorporated. Rehabilitation refers to the process aimed at supporting patients recover from illness, injury or disability to attain the highest level of physical, mental, and social functioning possible. We included studies describing a method to support clinical reasoning or clinical decision-making in physiotherapy practice or in a rehabilitation setting involving physiotherapy. All types of adult patient groups were included regardless of their disease. The search was limited to English language papers. No books, theses and conference proceedings were used. The year of publication was not limited. The search was done by one reviewer (JB) by selecting literature on titles and abstracts that met the inclusion criteria. Full text screening was performed by two reviewers independently (JB and MEL). In case of uncertainty about inclusion, a third reviewer (ML) was consulted. We used a data extraction form, including the framework’s description, target population, the applied setting of the framework, users of the framework and purposes of the framework. Data extraction was independently performed by two reviewers (JB and MEL). In addition, key elements of the framework were extracted in a reflectivity meeting with the core team.
Box 1. Full search as performed in PubMed
(((clinical[All Fields] AND reasoning[All Fields]) OR "clinical decision-making"[MeSH Terms]) AND ("physical therapy modalities"[MeSH Terms] OR ("physical"[All Fields]) AND ("therapy"[All Fields] AND "modalities"[All Fields]) OR "physical therapy modalities"[All Fields] OR "physiotherapy"[All Fields] OR “rehabilitation” [All Fields]) AND (“tool" [All Fields] OR “model” [All Fields] OR “framework”[All Fields] OR “algorithm”[All Fields]))
Modelling phase: Development of the physical capacity framework
A core team of experts developed a draft version of the physical capacity framework. Key elements, which were extracted from the literature search, were discussed in a reflectivity meeting with the core team and were used to inform the first draft. Our core team consisted of four members working at the rehabilitation department of our academic teaching hospital: one senior researcher specialised in the field of development and evaluation of rehabilitation interventions (ML) and three PTs with a Master of Science degree (JB, RH, VV).
To obtain feedback on the first draft, three separate face-to-face meetings with PTs from the exercise physiology team, the neurology team and the acute team in our hospital were organised by one member (JB) of the core team, who works as a PT in the exercise physiology team. During these meetings, the purpose of the physical capacity framework, the results of the literature review and the preliminary version of the framework were presented and discussed. In addition, an example of a patient treated by the PTs of the respective team was presented to demonstrate how the physical capacity framework could serve as a clinical reasoning tool. PTs were then given the opportunity to reflect on the proposed framework. The feedback obtained from these meetings was noted and summarised by the researcher (JB) into categories: 1) the framework as an uniform method of communication between the different care providers 2) the experiences of the PTs and trainees with the framework as a learning tool 3) the comprehensibility of the framework 4) the usability of the framework as a tool for clinical reasoning and 5) the completeness of the framework (i.e. including relevant elements for the hospital setting). The results were discussed in a reflectivity meeting with the core team, upon which the framework was adapted to a semi-final version.
Exploratory trial: Field testing
All PTs working in our hospital (n = 24) were asked to participate in field testing of the semi-final version of the physical capacity framework over a 6-month period. We briefed PTs to use the physical capacity framework as much as possible in daily practice and to organise case discussions with their team using the framework. If the PTs needed help or had questions about the case discussions, the researcher (JB) was available for consultation.
After the field testing period, four face-to-face meetings were organised by the researcher (JB). Three meetings were organised with the three PT teams that conducted the field tests. To improve the physical capacity framework for a final version, these three teams discussed, based on the previously identified topics in the modelling phase, with the researcher how the pilot phase had proceeded and what the physiotherapists would still like to add or change to the framework. Finally, we organised one meeting with occupational therapists and rehabilitation physicians from our department to get feedback from disciplines other than physiotherapy. This gave the researcher an impression of whether the framework could be used more broadly.
The feedback from these four expert meetings was summarised and categorised into topics by the researcher (JB). Based on these results, the framework was further modified by our core team, leading to the final version of the physical capacity framework.
Results
Comprehensive literature search
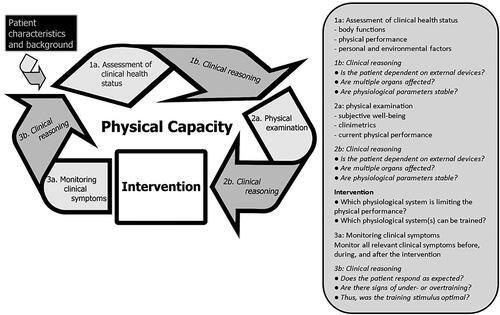
We identified a total of 311 papers of which 17 papers met the inclusion criteria. presents the flow of studies through the review. shows the extracted data of the included papers. The questions of the comprehensive literature search were answered through these data.
Figure 1. Flow of studies identified. Started with 302 records identified by Pubmed and nine additional records by searching for citations. Screened a total of 311 titles and abstracts and excluded 277 records. Thirty-four full-text papers were reviewed, after which 17 were excluded. Seventeen papers were finally included in the study.
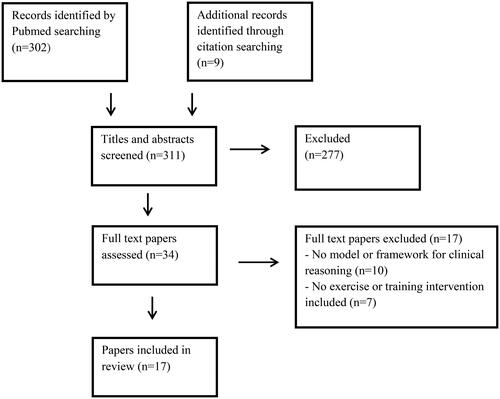
Table 1. Data extraction form.
1. Which frameworks are developed to support clinical reasoning in physiotherapy and rehabilitation?
A total of 17 frameworks were identified by the comprehensive literature search (see ). Of these frameworks, eight were developed for a specific patient group: patients with Parkinson Disease [Citation27], patients with COPD [Citation6], patients admitted to the Intensive Care Unit (ICU) [Citation17,Citation25], patients with low back pain [Citation28], patients with neurological diseases [Citation14], patients after stroke [Citation21] and patients with breast cancer undergoing chemotherapy [Citation22]. The other frameworks were developed for patients in general, i.e. independent of diagnosis [Citation7,Citation10,Citation12,Citation15,Citation16,Citation20,Citation23,Citation24,Citation26,Citation29–31]. A total of nine frameworks were specifically developed for PTs. [Citation7,Citation10,Citation15,Citation20,Citation24,Citation27–29,Citation31], whereas others were also developed for health professionals other than PTs [Citation6,Citation12,Citation14,Citation16,Citation17,Citation21,Citation22,Citation25,Citation26,Citation30]. Four frameworks were developed for clinical reasoning in the hospital setting, i.e. at a pulmonary unit [Citation6], an ICU [Citation17,Citation25] and for in-hospital use in general [Citation7]. This latter framework identified eight themes describing the core elements for clinical reasoning in acute hospital care, but this model was not specifically designed as a tool for use in practice [Citation7].
2. What are key elements in these frameworks?
Since no framework appeared to be available for PTs that reflects the complex and dynamic physical capacity of hospitalised patients and can guide clinical reasoning, key elements deemed relevant were extracted from the identified frameworks as a basis for a new physical capacity framework to be developed.
First, the use of the ICF, which plays a role in the majority of frameworks identified, was considered a key element because it has been widely used as a structure for describing health and health status in physiotherapy and rehabilitation. It therefore ensures uniformity and unambiguous communication [Citation10,Citation24,Citation26,Citation28]. Second, the structure of the patient management model including patient history, examination, diagnosis/prognosis, intervention and evaluation, was considered useful in guiding the patient systematically through the patient journey [Citation7,Citation10,Citation12,Citation14,Citation15,Citation20,Citation28]. Some frameworks provided a specification of a component of the patient management model, for example by focusing on the intervention [Citation6,Citation17,Citation22,Citation24–27,Citation30] or determining a physiotherapeutic diagnosis [Citation29]. Finally, monitoring of clinical parameters (such as heart rate and oxygen saturation) was considered relevant to evaluate whether the appropriate training stimulus is being provided and to adjust the stimulus if necessary [Citation6,Citation30].
Development of the physical capacity framework
To develop a first draft and semi-final version of the physical capacity framework, the core team discussed the results of the literature search and feedback from the three PT specialist teams until consensus was reached.
The use of the ICF model as the basis for the physical capacity framework was considered important by both the PT teams and the core team. All teams agreed that the use of the ICF model could contribute to uniform communication. Body functions, activities and participation, environmental and personal factors of the ICF model were considered relevant to the physical capacity framework. Body functions were categorised into six internal body systems [Citation8], deemed important for PT practice in the hospital: cardiovascular status, respiratory status, musculoskeletal status, neurological status, internal status and psychological/cognitive status. Activities and participation in the hospital setting were specified as the physical performance of the patient, with an emphasis on mobility during hospitalisation. In the first draft of the framework, the core team introduced fixed functional performance categories (i.e. E: bedridden, D: bed-edge mobilisation, C: active transfer, B: assisted walking, A: independent walking). However, for the semi-final version, after feedback from the PTs, that these fixed categories are not complete enough to describe a patient’s functional performance, it was decided to let the PTs fill in the physical performance status themselves. Examples of environmental factors in a hospital setting include whether the patient is nursed in isolation because of an infection, whether a partner is present, or whether the patient has a urinary catheter or drain. Personal factors refer to a person’s coping style, behaviour and attitude.
With regard to the patient management model [Citation8], the core team felt it was important to include the elements examination, intervention and evaluation in our physical capacity framework. Feedback from the specialist teams revealed that a fixed core set of tests or measurements for examination was not desirable due to the diverse medical specialties (neurology, traumatology, pulmonology, cardiology, etc) targeted by the framework. For a description of the PT intervention, Frequency, Intensity, Type and Time principle (FITT factors) were recommended. All teams agreed on the relevant clinical parameters to be monitored during PT treatment for hospitalised patients (see ).
Table 2. Clinical parameters.
Field testing
The semi-final version of the framework was tested and evaluated in clinical practice. Of the 24 PTs and 3 trainees working at our hospital at the time, 18 PTs and all trainees were willing to participate in the field test. Six PTs did not consider themselves eligible for participating, because they were less involved in daily clinical practice. For collecting the feedback from the PTs after field testing the five topics as described in the method were used.
PTs agreed that the physical capacity framework supports uniform communication. Both PTs and trainees were convinced that the physical capacity framework could be used as a learning tool. Most PTs found the physical capacity framework useful, provided the elements were well defined. Some PTs found the use of the physical capacity framework time-consuming. All participating groups of (PT) specialists felt that the physical capacity framework can provide adequate guidance for clinical reasoning in physiotherapy practice for the hospitalised patient. However, they mentioned that it was not clear at what point in the physical capacity framework clinical reasoning occurs and recommended that clinical reasoning moments be more clearly indicated in the framework. The PTs agreed that body functions, detailed information about the patients’ physical performance and FITT factors are important elements that need to be established in the physical capacity framework. However, they mentioned that they missed information about the patient, such as history and diagnosis, pre-existent physical functioning, treatment goals and the patient’s request for help. Also, several PTs indicated that they would like to add additional monitoring parameters relevant to their specialism.
Final version of the physical capacity framework
Based on the feedback, adjustments were made and a final version of the physical capacity framework was created (see ). Below the different elements of the framework are presented, with paragraph numbers corresponding to the numbers in . Appendix 1 provides an example of using the physical capacity framework to describe a patient case.
Patient characteristics and background
Before starting the iterative process of clinical reasoning, it is important to extract relevant (medical) information from the patient’s electronic health record, such as diagnosis, medical history and comorbidities, and level of functioning before admission.
1a. Assessment of clinical health status
First, the PT determines from the patient’s electronic health record, the patient’s current physical status based on relevant clinical information, differentiating between the various body functions, i.e. cardiovascular status, respiratory status, muscular/bone status, neurological status, internal status and psychological/cognitive status. In addition, the PT identifies information about the current physical performance and relevant personal and environmental factors.
1b. Clinical reasoning
Based on the established physical status, the PT makes an estimate of the patients’ physical capacity. This estimate depends on several factors, including dependence on external devices, degree of organ damage, and instability of one or more physiological parameters. In doing so, the PT may consider the following questions:
Is the patient dependent on external devices? (e.g. ventilator, intra-aortic balloon pump, chest drain, arterial line, Continuous Veno-Venous Hemofiltration)? Higher dependency is likely related to lower physical capacity.
Are multiple organs of the patient affected? It is assumed that the more organs affected, the worse the patient’s physical capacity.
Does the patient have stable physiological parameters (e.g. blood pressure, heart rate, saturation or respiratory rate)? Unstable physiological parameters are often associated with lower physical capacity.
The PT then translates the estimate of physical capacity into an expectation of the patient’s physical performance. The level of physical performance can range from being fully bedridden to functioning independently on the ward.
2a. Physical examination
To confirm or adjust the estimated level of physical capacity and performance, the PT should visit the patient at this step to assess the patient’s subjective well-being, observe the patient’s current physical performance, and perform physical examination. The choice of clinimetrics depends on the patient’s medical condition and the estimated capacity and performance. For example, in a patient with a neurological disorder (e.g. CVA) who is active in bed, the Trunk Control Test is recommended [Citation32].
2b. clinical reasoning
The results of the physical examination in step 2a are used to refine the estimate of physical capacity determined in step 1b. This leads to a final estimate of the patient’s physical capacity and performance. Once this step has been completed, the appropriate physiotherapy intervention can be determined.
Intervention
The next step is to provide an adequate intervention for the patient with an appropriate training stimulus. Based on the information from step 2a, the PT can determine one or more of the physiological systems that limit the physical performance of activities (e.g. cardiovascular function impairment, respiratory function impairment and/or muscle weakness). The PT then knows the type and level of limitation and can determine which systems can be trained and which FITT factors are applicable. Condition-specific PT treatment protocols serve as guidelines to determine FITT factors. For example, in postoperative oncology patients, there is a mobilisation protocol from day 1 after surgery, with walking distances of 50-100 metres, increasing to day 7 (1150 metres). Our physical capacity framework can be supportive to assess the patient’s physical capacity each day to ensure that this protocol matches their current level of capacity and to decide if adjustments to the protocol are needed.
3a. monitoring of clinical symptoms
During the intervention, the PT should monitor relevant clinical symptoms (e.g. saturation and respiratory rate in case of a limited respiratory system) to objectively determine treatment tolerance. To make best use of these parameters, it is recommended to measure them before, during and after the intervention.
3b. Clinical reasoning
Using observation, recorded clinical symptoms and the patient’s subjective experience, the PT can determine whether the intervention provided a trainings stimulus as expected. In doing so, signs of under- or overtraining may be signalled and it can be determined whether the right training stimulus has been applied.
Discussion
Our article outlines a newly developed physical capacity framework to support PTs in their clinical reasoning process when mobilising or training hospitalised patients. The final framework seems helpful and feasible in guiding the steps to be taken during patient management to determine the patient’s physical capacity. During the hospital stay, patients are often treated by different PTs, due to varying schedules, weekend shifts, or other circumstances. Uniform communication about the patient’s physical capacity and training dose is therefore important.
Based on our literature review and discussions with experts, the first key element selected for its use in the framework was the ICF as a uniform language to describe health and health-related status [Citation11]. Second, the structure of the patient management model was found useful [Citation8]. Of specific importance to the hospital setting is that the steps to be taken are cyclical and iterative, especially because of the often rapidly changing health status of hospitalised patients [Citation7]. Monitoring clinical parameters is therefore another important element in the physical capacity framework, as PTs should be alert to changes in health status that may require further adjustments to FITT factors. Moreover, these parameters allow the PT to evaluate whether an adequate training stimulus has been applied and prevent under- or over-exertion of the patient.
It should be noted that the physical capacity framework presented here is intended to support clinical decision-making, but cannot replace the clinical expertise and skills of PTs [Citation22]. It is also important to note that the framework does not replace existing frameworks, but can be used as a specification of these frameworks to determine the physical capacity of a hospitalised patient. It is obviously very important not to lose sight of other factors relevant to patient-centred care, such as psychosocial factors, opinions, involvement, motivation and goals of the patient, as well as organisational factors, such as budget and availability of sufficient staff [Citation10,Citation12].
A methodological weakness of our study was the lack of a thorough qualitative research approach, which was not feasible due to time and budget constraints. Instead, we conducted a descriptive analysis of notes taken during meetings and interviews. To reduce the risk of researcher bias, we held reflectivity meetings with the core team to discuss findings from the literature review and feedback from the PTs. We used a process of co-creation to facilitate a collaborative process, which involves active participation, sharing of ideas, and contributions from healthcare professionals in the development of the framework. The steps we took had a natural flow, however we also worked in a structured and transparent way as much as possible, guided by the phases of the MRC framework for developing complex interventions.
Another potential weakness is that we did not systematically search other databases than Pubmed, so we cannot completely rule out the possibility that we missed relevant articles. However, since Pubmed covers most of the literature in our field and we conducted an additional snowball search using reference lists of identified articles, we are confident that we found most of the relevant literature. In addition, as only one reviewer made a selection on titles and abstracts of the initial search, this also increased the risk that relevant papers were missed.
The proposed physical capacity framework could serve as a starting point for further development of mobilisation and training tailored to hospitalised patients. In the future, an (international) multicentre working group consisting of health professionals from different disciplines, researchers and patients could be established, to conduct a qualitative study on the use and implementation of the framework in clinical practice. Then, the MRC cycle can be continued by testing the physical capacity framework for effectiveness in clinical practice (MRC phase 4) and implementing it if favourable (MRC phase 5) [Citation18]. Outcomes can be defined at the patient level (e.g. recovery of functional capacity and performance, length of hospital stay or discharge destination) or at the professional level (e.g. inter-professional communication and collaboration, student learning capacity). In terms of implementation, it may be helpful to build decision support for physical capacity and associated training dose into the electronic health record.
In conclusion, a physical capacity framework to support PTs in their clinical reasoning process when mobilising or training hospitalised patients was developed. The final physical capacity framework can guide the steps to be taken during patient management in order to determine the patients’ physical capacity and to achieve an adequate training stimulus, which can be adapted based on monitoring information.
Ethical statement
Under Dutch law, we are allowed to use the physiotherapists’ data in accordance with the General Data Protection Regulation (GDPR). All procedures applied for this study were conform the declaration of Helsinki.
Supplemental Material
Download Zip (29.3 KB)Acknowledgement
We would like to acknowledge Dr. J. Runhaar for creating the illustration of our physical capacity framework.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Schaller SJ, Anstey M, Blobner M, et al. Early, goal-directed mobilisation in the surgical intensive care unit: a randomised controlled trial. Lancet. 2016;388(10052):1377–1388. doi: 10.1016/S0140-6736(16)31637-3.
- Ramos Dos Santos PM, Aquaroni Ricci N, Aparecida Bordignon Suster É, et al. Effects of early mobilisation in patients after cardiac surgery: a systematic review. Physiotherapy. 2017;103(1):1–12. doi: 10.1016/j.physio.2016.08.003.
- van der Leeden M, Balland C, Geleijn E, et al. In-hospital mobilization, physical fitness, and physical functioning after lung cancer surgery. Ann Thorac Surg. 2019;107(6):1639–1646. doi: 10.1016/j.athoracsur.2018.12.045.
- Moyer M, Young B, Wilensky EM, et al. Implementation of an early mobility pathway in neurointensive care unit patients with external ventricular devices. J Neurosci Nurs. 2017;49(2):102–107. doi: 10.1097/JNN.0000000000000258.
- Martínez-Velilla N, Casas-Herrero A, Zambom-Ferraresi F, et al. Effect of exercise intervention on functional decline in very elderly patients during acute hospitalization: a randomized clinical trial. JAMA Intern Med. 2019;179(1):28–36. doi: 10.1001/jamainternmed.2018.4869.
- Camp PG, Reid WD, Chung F, et al. Clinical decision-making tool for safe and effective prescription of exercise in acute exacerbations of chronic obstructive pulmonary disease: results from an interdisciplinary delphi survey and focus groups. Phys Ther. 2015;95(10):1387–1396. doi: 10.2522/ptj.20140542.
- Masley PM, Havrilko C-L, Mahnensmith MR, et al. Physical therapist practice in the acute care setting: a qualitative study. Phys Ther. 2011;91(6):906–919. doi: 10.2522/ptj.20100296.
- Guide to physical therapy practice 3.0. 2014, Alexandria, VA: American Physical Therapy Association (APTA).
- Kasper JD, Chan KS, Freedman VA. Measuring physical capacity. J Aging Health. 2017;29(2):289–309. doi: 10.1177/0898264316635566.
- Atkinson HL, Nixon-Cave K. A tool for clinical reasoning and reflection using the international classification of functioning, disability and health (ICF) framework and patient management model. Phys Ther. 2011;91(3):416–430. doi: 10.2522/ptj.20090226.
- International Classification of Functioning, Disability and Health. [cited 2022 May 3]; Available from: https://www.who.int/standards/classifications/international-classification-of-functioning-disability-and-health
- Rothstein JM, Echternach JL, Riddle DL. The hypothesis-oriented algorithm for clinicians II (HOAC II): a guide for patient management. Phys Ther. 2003;83(5):455–470. doi: 10.1093/ptj/83.5.455.
- Stucki G, Sangha O. Principle of rehabilitation. 2nd. ed. 1998, London, England: Mosby.
- Schenkman M, Deutsch JE, Gill-Body KM. An integrated framework for decision making in neurologic physical therapist practice. Phys Ther. 2006;86(12):1681–1702. doi: 10.2522/ptj.20050260.
- Baker SE, Painter EE, Morgan BC, et al. Systematic clinical reasoning in physical therapy (SCRIPT): tool for the purposeful practice of clinical reasoning in orthopedic manual physical therapy. Phys Ther. 2017;97(1):61–70. doi: 10.2522/ptj.20150482.
- Steiner WA, Ryser L, Huber E, et al. Use of the ICF model as a clinical problem-solving tool in physical therapy and rehabilitation medicine. Phys Ther. 2002;82(11):1098–1107. doi: 10.1093/ptj/82.11.1098.
- Hanekom S, Gosselink R, Dean E, et al. The development of a clinical management algorithm for early physical activity and mobilization of critically ill patients: synthesis of evidence and expert opinion and its translation into practice. Clin Rehabil. 2011;25(9):771–787. doi: 10.1177/0269215510397677.
- Craig P, Dieppe P, Macintyre S, et al. Developing and evaluating complex interventions: the new medical research council guidance. Int J Nurs Stud. 2013;50(5):587–592. doi: 10.1016/j.ijnurstu.2012.09.010.
- Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71.
- Jones MA. Clinical reasoning in manual therapy. Phys Ther. 1992;72(12):875–884. doi: 10.1093/ptj/72.12.875.
- Tempest S, McIntyre A. Using the ICF to clarify team roles and demonstrate clinical reasoning in stroke rehabilitation. Disabil Rehabil. 2006;28(10):663–667. doi: 10.1080/09638280500276992.
- van der Leeden M, Huijsmans RJ, Geleijn E, et al. Tailoring exercise interventions to comorbidities and treatment-induced adverse effects in patients with early stage breast cancer undergoing chemotherapy: a framework to support clinical decisions. Disabil Rehabil. 2018;40(4):486–496. doi: 10.1080/09638288.2016.1260647.
- Donaghy M, Morss K. An evaluation of a framework for facilitating and assessing physiotherapy students’ reflection on practice. Physiother Theory Pract. 2007;23(2):83–94. doi: 10.1080/09593980701211952.
- Elvén M, Hochwälder J, Dean E, et al. A clinical reasoning model focused on clients’ behaviour change with reference to physiotherapists: its multiphase development and validation. Physiother Theory Pract. 2015;31(4):231–243. doi: 10.3109/09593985.2014.994250.
- Laurent H, Aubreton S, Vallat A, et al. Very early exercise tailored by decisional algorithm helps relieve discomfort in ICU patients: an open-label pilot study. Eur J Phys Rehabil Med. 2020;56(6):756–763. doi: 10.23736/S1973-9087.20.06274-7.
- Hart T, Dijkers MP, Whyte J, et al. A theory-driven system for the specification of rehabilitation treatments. Arch Phys Med Rehabil. 2019;100(1):172–180. doi: 10.1016/j.apmr.2018.09.109.
- Borchers EE, McIsaac TL, Bazan-Wigle JK, et al. A physical therapy decision-making tool for stratifying persons with parkinson’s disease into community exercise classes. Neurodegener Dis Manag. 2019;9(6):331–346. doi: 10.2217/nmt-2019-0019.
- Rundell SD, Davenport TE, Wagner T. Physical therapist management of acute and chronic low back pain using the world health organization’s international classification of functioning, disability and health. Phys Ther. 2009;89(1):82–90. doi: 10.2522/ptj.20080113.
- Rushton A, Rivett D, Carlesso L, et al. International framework for examination of the cervical region for potential of cervical arterial dysfunction prior to orthopaedic manual therapy intervention. Man Ther. 2014;19(3):222–228. doi: 10.1016/j.math.2013.11.005.
- van der Leeden M, Stuiver MM, Huijsmans R, et al. Structured clinical reasoning for exercise prescription in patients with comorbidity. Disabil Rehabil. 2020;42(10):1474–1479. doi: 10.1080/09638288.2018.1527953.
- Donaghy ME, Morss K. Guided reflection: a framework to facilitate and assess reflective practice within the discipline of physiotherapy. Physiother Theory Pract. 2000;16(1):3–14. doi: 10.1080/095939800307566.
- Veerbeek JM. KNGF Richtlijn Beroerte – Update klinimetrie. 2017. Available from: https://www.kngf.nl/binaries/content/assets/kennisplatform/onbeveiligd/richtlijnen/beroerte/downloads/beroerte-verantwoording-en-toelichting