?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Background: Sugammadex is a selective relaxant binding agent for antagonism of prolonged rocuronium-induced neuromuscular blockade. The recommended dose is 2 mg/kg. Based on the pharmacological characteristics of sugammadex in obese patients, the calculated lean body mass (CLBM) should be used to determine the dose to reverse moderate neuromuscular blockade induced by rocuronium.
Objective: A study was undertaken to prove that sugammadex can be used according to CLBM to reverse moderate neuromuscular blockade in obese female patients.
Methods: This is a prospective, non-randomised, observational study. Sugammadex was used at the end of bariatric surgery on obese patients with a body mass index > 32 kg/m2. The dose was calculated according to the lean body mass. Muscle blockade was assessed using train-of-four monitoring.
Results: Twenty women were included in this study. All patients were female and ASA 2. The age of patients ranged between 20 and 50 years with a mean age of 35.74 (±10) years. The mean CLBM was 50 kg. The mean time from administration of sugammadex to reverse neuromuscular blockade from two responses of TOF to T4/T1 > 90% was 167.25 seconds (2.8 minutes) (60–285 seconds).
Conclusion: It is concluded that the calculated lean body mass can be used to calculate the dose of sugammadex for obese female patients to reverse moderate neuromuscular blockade induced by rocuronium.
Introduction
Muscle relaxants must be administered according to the calculated lean body mass (CLBM) and not to the real weight of the patient, particularly in the case of morbidly obese patients. Rocuronium used according to the ideal body weight has a shorter duration of action than when the real bodyweight is used.Citation1 Sugammadex is a molecule that reverses neuromuscular blockade induced by rocuronium and vecuronium.Citation2 We recruited obese female patients who were monitored during bariatric surgery with a train-of-four (TOF) monitoring and a measure of the single twitch before and after rocuronium administration. At the end of surgery, patients received 2 mg/kg of sugammadex according to the CLBM and we measured the recovery time from two to four responses of TOF, and the time to obtain a ratio T4/T1 equal to or greater than 90%. The aim of this study was to determine whether the CLBM can be used in obese female patients to determine the dose of sugammadex necessary to reverse rocuronium neuromuscular blockade in obese female patients.
Methods
A prospective, non-randomised, observational study was conducted between May 15 and August 3, 2009. Following ethical committee approval, we measured the recovery time (TOF—90%) of patients older than 18 years during bariatric surgery. The procedures included gastric bypasses, gastric sleeves or gastric bandings. The body mass index (BMI) was above 32 kg/m2. Twenty consecutive patients gave their informed consent to participate in the study. A recommended dose of sugammadex is 2 mg/kg weight.Citation3,Citation4
TOF and twitch were measured with a TOF-watch SX monitor 2.2 (Organon (Ireland) Ltd., Swords, Co. Dublin, Ireland) and electronically recorded every 15 seconds. A stimulus of 60 mA current over 200 µs was used.Citation3
The anaesthetic technique included propofol (2 mg/kg), sufentanil (0.2 µg/kg), rocuronium (1.2 mg/kg) and desflurane. Although a recommended rocuronium dose is 0.6–1.2 mg/kg weight,Citation3,Citation4 we used 1.2 mg/kg and used the CLBM as the weight factor. The twitch (100%) was measured before administration of the muscle relaxants but after induction of anaesthesia. At the end of the procedure, sugammadex (2 mg/kg CLBM) was administered when the TOF reached two responses out of four. The time between two and four twitches of TOF with a twitch above 90% of the initial one (T4/T1 ≥ 90%) was noted in seconds.
Lean body mass (LBM) was calculated using the formula of JamesCitation5 for females:We measured the mean time to recovery and the range. We determined the relationship between: (i) the BMI and recovery time, (ii) weight and recovery time, (iii) CLBM and recovery time and (iv) body temperature and recovery time. The statistical analysis included the covariance between each factor and the correlation coefficient of Pearson.
Exclusion criteria were patients with a history of allergic reaction on sugammadex, rocuronium or other neuromuscular blockers, hepatic or renal failure, patients with neuromuscular diseases and patients with any chronic medication having a myorelaxant effect such as benzodiazepines. All patients were older than 18 years.
Results
The study was carried out on 20 ASA 2 female patients. The patients ranged in age from 20 to 50 years with a mean age of 35.74 (±10) years. The patient demographic and surgical data are given in . For patient 12, we had to replace the accelerometer of the TOF-Watch at the beginning of anaesthesia to ensure calibration of the neuromuscular stimulation prior to neuromuscular relaxation. The automatic record of the TOF was corrected for the baseline twitch.
Table 1: Demographic and surgical patient data
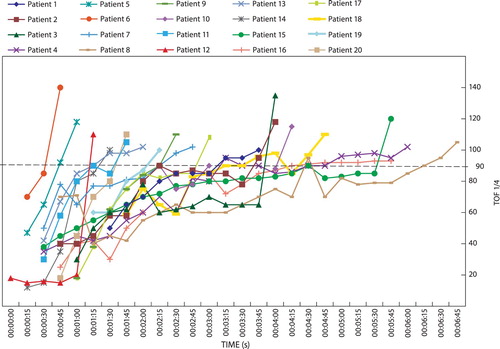
The characteristics of the neuromuscular blockade and sugammadex reversal are summarised in . The mean BMI was 41.43 kg/m2 (37.42–47.25). The weight range was 90 kg to 130 kg, with a height of 154 cm to 182 cm. The mean weight was 110.32 kg. The mean CLBM was 50 kg (42.96 kg–64.24 kg). The mean dose of sugammadex was 100 mg (90 mg–130 mg). In , the recovery curves for each patient are shown. Patients 8 and 16, following a recovery to above 90%, showed a lower value during the subsequent minute. All values were above 90% within 360 seconds (6 minutes).
Table 2: Study results
The time to four twitch responses and 90% of the initial twitch is given in . The mean time was 167.25 seconds (2.8 minutes) (116.25–213.75 [60–285]) and a median time of 150 seconds (2.5 minutes).
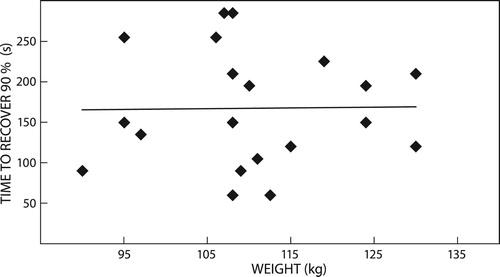
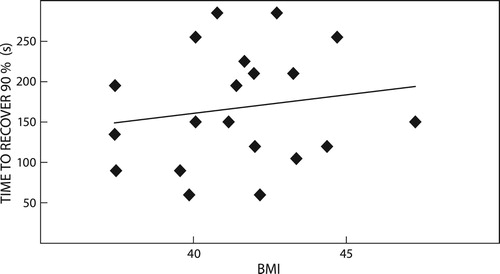
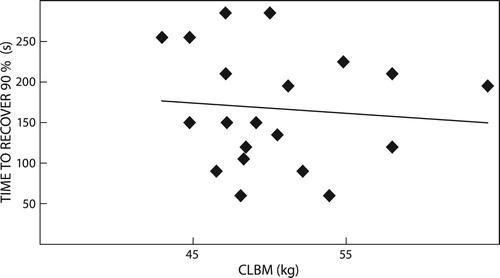
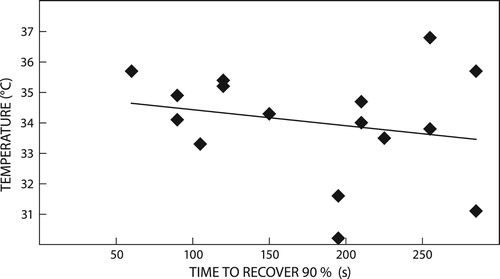
The regression curves between weight (), BMI (), LBM (), body temperature () and recovery time showed no direct relationship with recovery. The covariance was low.
Discussion
We obtained only a small sample and during the short period of study we were unable to include men that met the inclusion criteria of the study. These are limitations of our study.
Sugammadex forms very tight 1:1 complexes with amino-steroid-based relaxants.Citation2 It reverses rocuronium or vecuronium-induced neuromuscular blockade.Citation2–4 It is a selective relaxant binding agent. The dose of sugammadex is related to the dose of the neuromuscular agent.Citation3,Citation6–8
Leykin et al. statedCitation1 that the dose of rocuronium should be assessed on the basis of the ideal rather the real bodyweight in clinical practice. In obese patients, Meyhoff et al.Citation9 recommend using the ideal bodyweight (IBW) for dosing of rocuronium. The IBW dosage provides a shorter duration of action, without a difference in onset time or tracheal intubation conditions. Pühringer et al.Citation10 showed that obesity did not alter pharmacodynamics or pharmacokinetics in female patients.
In our study the dose of rocuronium (1.2 mg/kg) was based on the calculated lean body mass. Intubation of our patients was accomplished with ease. During anaesthesia, we followed the neuromuscular blockade with a TOF-Watch SX, to maintain a full block during the procedure. Murphy et al.Citation11 and othersCitation12 validated the TOF-Watch SX monitor as a safe quantitative technique to assess the neuromuscular blockade and the residual curarisation. According to Kopman et al.Citation2,Citation12: ‘there is now general agreement that return to TOF ratio of 90% or greater at the end of surgery should be our goal after the administration of nondepolarizing relaxants’. In our study, a TOF-Watch monitor was used and all the values were electronically registered every 15 seconds.
Stout et al.Citation13 and Wulf et al.Citation14 found that desflurane did not significantly alter the time to recovery from rocuronium. However, desflurane anaesthesia significantly prolonged the duration of action of rocuronium at 0.9 mg/kg single bolus dose, when compared with sevoflurane or propofol anaesthesia maintenance regimens.Citation15 In our study, all the anaesthesia procedures were done with desflurane and rocuronium 1.2 mg/kg. Desflurane can change the time to recovery, but should the effect of sugammadex be influenced by the inhalational anaesthetic? Reversal of rocuronium-induced block by sugammadex did not differ between anaesthesia with propofol or sevoflurane.Citation16
Most patients (except patient 3) became hypothermic but sugammadex (2 mg/kg), given based on the CLBM, was effective at quickly reversing neuromuscular blockade for all. This was true even though it has been demonstrated that hypothermia prolongs the duration of action of rocuronium.Citation17 We did not observe inadequate ventilation after extubation of patients and transfer to recovery room where the hypothermia was treated.
Debaene and MeistelmanCitation4 propose using sugammadex at the end of the procedure when the TOF indicates a second twitch of 4, at a dosage of 2 mg/kg in order to obtain recovery in a time period shorter than 5 minutes. MirakhurCitation18 recommends 2 mg/kg for a shallow block and 4 mg/kg for a deep block. Groudine et al.Citation7 showed that with a dosage of 2 mg/kg there was a great variability in recovery time, reported to be between 1.8 and 15.2 minutes, but with higher dosages (8 mg/kg) the mean recovery time narrows to 0.8 to 2.1 minutes. Plaud et al.,Citation3 in a multicentre randomised dose-finding study with patients aged from 28 days to 65 years, found that the mean time was less than 2 miutes, except in children and adolescents where it was longer. When 0.6 mg/kg rocuronium was used, the neuromuscular blockade was reversed with 2 mg/kg of sugammadex in a time shorter than 3 minutes. This was dose dependent. In our study, the mean time is 167.25 seconds (2.8 minutes) (116.25–213.75 [60–285]) and the median is 150 seconds (2.5 minutes).
These results are comparable to the results of the literature. But in the literature the dosage is calculated according to bodyweight,Citation19 IBWCitation20 or IBW + 40%Citation21 and not the CLBM. The effect of sugammadex is dose dependent. If we use the bodyweight for the dosage, sugammadex would be very effective. The mean weight of our population is more than twice (2.24) the CLBM. For each patient, one ampoule of sugammadex was sufficient to reverse neuromuscular blockade. Conversely, as the drug is expensive, its economically justified use would be good practice.Citation22,Citation23 If we transfer the ratio to the cost, on average we would overspend by 125%. This is based on the cost and the volume of one ampoule of the drug. It may be better practice to use the CLBM to calculate the dose of sugammadex, instead of the total bodyweight. We recommend a similar study on similarly obese patients which includes a larger sample of both men and women who remain normothermic during surgery.
Conclusion
Our results show that the calculated lean body mass can be used for the dosage of sugammadex to reverse moderate neuromuscular blockade at the end of the procedure. The dosage of 2 mg/kg in a population of obese female patients allows a recovery time comparable to the general population of adults. We recommend the use of 2 mg/kg based on the calculated lean body mass. Monitoring of the neuromuscular blockade is important to detect any residual curarisation.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Leykin Y, Pellis T, Lucca M, et al. The pharmacodynamic effects of rocuronium when dosed according to real body weight or ideal body weight in morbidly obese patients. Anesth Analg. 2004;99(4):1086–1089. doi: 10.1213/01.ANE.0000120081.99080.C2
- Kopman A. Sugammadex: a revolutionary approach to neuromuscular antagonism. Anesthesiology. 2006;104:631–633. doi: 10.1097/00000542-200604000-00003
- Plaud B, Meretoja O, Hofmockel R, et al. Reversal of rocuronium-induced neuromuscular blockade with sugammadex in pediatric and adult surgical patients. Anesthesiology. 2009;110(2):284–294.
- Debaene B, Meistelman C. Indications et utilisation clinique du sugammadex. Annales Françaises D'Anesthésie et de Réanimation. 2009;28:S57–S63. doi: 10.1016/S0750-7658(09)72489-X
- De Baerdemaeker LEC, Mortier EP, Struys MMRF. Pharmacokinetics in obese patients. Continuing Education in anaesthesia. Crit Care Pain. 2004;4(5):152–155.
- Suy K, Morias K, Cammu G. Effective reversal of moderate rocuronium or vecuronium-induced neuromuscular block with sugammadex, a selective relaxant binding agent. Anesthesiology. 2007;106:283–288. doi: 10.1097/00000542-200702000-00016
- Groudine SB, Soto R, Lien C, et al. A randomized, dose-finding, Phase II study of the selective relaxant binding drug, sugammadex, Capable of Safely reversing Profound rocuronium-induced neuromuscular block. Anesth Analg. 2007;104(3):555–562. doi: 10.1213/01.ane.0000260135.46070.c3
- Sorgenfrei IF, Norrid K, Larsen PB. Reversal of rocuronium-induced neuromuscular block by the selective relaxant binding agent sugammadex: a dose-finding and safety study. Anesthesiology. 2006;104:667–674. doi: 10.1097/00000542-200604000-00009
- Meyhoff C.S, Lund J, Jenshup MT, et al. Should dosing of rocuronium in obese patients Be based on ideal or corrected body weight? Anesth Analg. 2009;109(3):787–792. doi: 10.1213/ane.0b013e3181b0826a
- Püringer FK, Keller C, Kleinasser A, et al. Pharmacokinetics of rocuronium bromide in obese female patients. Eur J Anaesthesiol. 1999;16(8):507–510. doi: 10.1046/j.1365-2346.1999.00523.x
- Murphy G, Szokol J, Marymont J, et al. Intraoperative Acceleromyographic monitoring Reduces the Risk of residual neuromuscular blockade and Adverse Respiratory Events in the Postanesthesia Care Unit. Anesthesiology. 2008;109(3):389–398. doi: 10.1097/ALN.0b013e318182af3b
- Kopman A, Yee P, Neuman G. Relationship of the train-of-four Fade ratio to clinical Signs and Symptoms of residual Paralysis in Awake Volunteers. Anesthesiology. 1997;86:765–771. doi: 10.1097/00000542-199704000-00005
- Stout RG, Gan TJ, Glass PS, et al. The effect of desflurane on rocuronium onset, clinical duration and maintenance requirements. Acta Anaesthesiol Belg. 2006;57(4):349–353.
- Wulf H, Ledowski T, Linstedt U, et al. Neuromuscular blocking effects of rocuronium during desflurane, isoflurane, and sevoflurane anaesthesia. Can J Anaesth. 1998;45(6):526–532. doi: 10.1007/BF03012702
- Maidatsi PG, Zaralidou AT, Gorgias NK, et al. Rocuronium duration of action under sevoflurane, desflurane or propofol anaesthesia. Eur J Anaesth. 2004 Oct;21(10):781–786. doi: 10.1097/00003643-200410000-00005
- Vanacker B, Vermyen K, Struys M, et al. Reversal of rocuronium-induced neuromuscular block with the Novel drug sugammadex Is Equally effective Under maintenance Anesthesia with propofol or sevoflurane. Anaesth Analg. 2007;104:563–568. doi: 10.1213/01.ane.0000231829.29177.8e
- Beaufort AM, Wierda JM, Belopavlovic M, et al. The influence of hypothermia (surface cooling) on the time-course of action and on the pharmacokinetics of rocuronium in humans. Eur J Anaesthesiol. Supplement. 01 Sep 1995;11:95–106.
- Mirakhur RK. Sugammadex in clinical practice. Anaesthesia. 2009;64(suppl 1):45–54. doi: 10.1111/j.1365-2044.2008.05870.x
- Monk TG, Rietbergen H, Woo T, et al. Use of sugammadex in patients With obesity: A Pooled analysis. Am J Ther. 2017 Sep/Oct;24(5):e507–e516. doi: 10.1097/MJT.0000000000000305
- Duarte NMDC, Caetano AMM, Neto SDSC, et al. Sugammadex by ideal body weight versus 20% and 40% corrected weight in bariatric surgery – double-blind randomized clinical trial. Brazil J Anesth. May–June 2018;68(3):219–224. doi: 10.1016/j.bjan.2017.10.010
- Van Lancker P, Dillemans B, Bogaert T, et al. Ideal versus corrected body weight for dosage of sugammadex in morbidly obese patients. Anaesthesia. 2011;66(8):721–725. doi: 10.1111/j.1365-2044.2011.06782.x
- Sperry R. Principles of economic analysis. Anesthesiology. 1997;86:1197–1205. doi: 10.1097/00000542-199705000-00022
- Johnstone RE, Jozefczyk KG. Cost of anesthetic drugs. Experience with a cost education trial. Anesth Analg. 1994;76:766–771.