Abstract
There is limited research on the perceptions of substance use (SU) and treatment goals among patients with substance use disorders (SUD) and attention deficit hyperactivity disorder (ADHD). We investigate whether SU perceptions and treatment goals were different among SUD patients with (SUD+ADHD) and without (SUD-ADHD) ADHD. Twelve SUD+ADHD patients (39.5 ± 8.5 years, 10 men), and 10 age- and substance severity matched SUD-ADHD patients (34.0 ± 10.0 years, six men), consecutively recruited between February 2010 and July 2012 were interviewed during the course of their SUD treatment. Interview data were analyzed using content analysis. The perceived positive aspects of SU were self-regulation of physical health, behavior, feelings, reasoning/thoughts, and the rewarding effects. The perceived negative aspects of SU included consequences on physical health, behavior, feelings, and reasoning/thoughts. SUD+ADHD patients less frequently linked SU to physical health and more frequently perceived SU as helpful to self-regulate their behavior. Four treatment goals categories emerged: total abstinence, conditional abstinence, substance reduction, and unspecified. SUD+ADHD patents less frequently chose total abstinence, and when using more than one substance, they commonly chose variable goals. In contrast, SUD-ADHD patients chose more similar goals. SUD+ADHD patients showed a more complex relation to their SUD than SUD-ADHD patients.
PUBLIC INTEREST STATEMENT
Substances use disorder (SUD) is a serious persistent condition in which uncontrolled and frequent substance use (SU) intake continues even when affecting the persons’ health, relations and work. Attention deficit hyperactivity disorder (ADHD) starts in childhood, commonly continuing in adulthood. The core symptoms of ADHD are inattention, hyperactivity and impulsivity. We asked 12 adult SUD patients with (SUD+ADHD) and 10 without ADHD (SUD-ADHD) to describe the positive and negative sides of their SU and their SU-related treatment goals.
To most patients, SU changed negative thoughts, feelings, physical states and behavior into positive. Additionally, some enjoyed getting high/drunk. Paradoxically, SU also worsened negative thoughts, feelings, physical states and behavior.
SUD+ADHD patients most commonly mentioned that SU helped them control their behavior and less often linked SU to physical states at all. SUD+ADHD patients seldom considered quitting SU completely. SUD signifies a vicious circle, possibly more complex in persons with SUD+ADHD.
Substance use disorders (SUD) are described by symptoms of tolerance, craving, uncontrolled and persistent substance use (SU), in spite of detrimental biopsychosocial consequences (American Psychiatric Association [APA], Citation2013; Saunders, Peacock, & Degenhardt, Citation2018). Individuals with SUD are frequently afflicted with attention deficit hyperactivity disorder (ADHD) (van de Glind et al., Citation2014), mood, anxiety, and personality disorders (Chen et al., Citation2011). ADHD is a neurodevelopmental disorder characterized by inattention, hyperactivity, and impulsivity (APA, Citation2013), that shares cognitive, motivational and reward difficulties with SUD (Kalbag & Levin, Citation2005; Wilens & Biederman, Citation2006). Studies have shown that about 14% of SUD patients fulfill the criteria for ADHD diagnoses (Roncero et al., Citation2015; van de Glind et al., Citation2014). In SUD clinical settings, patients with SUD and ADHD (SUD+ADHD) present at a younger age (Roncero et al., Citation2015), have an earlier SU debut, greater SU severity (Torok, Darke, & Kaye, Citation2012; Young et al., Citation2015), higher rates of psychiatric comorbidity (Kim et al., Citation2006; van Emmerik-van Oortmerssen et al., Citation2014; Wilens et al., Citation2005), and cognitive and social impairments (Brooks, Vosburg, Evans, & Levin, Citation2006) than SUD patients without ADHD (SUD-ADHD). Accordingly, SUD+ADHD patients may be more difficult to treat for SUD.
The complexity of SUD+ADHD calls for more research (Matthys et al., Citation2014), including qualitative studies on how SUD+ADHD patients relate to their own SUD. The available research suggests that adults with ADHD report more positive than negative effects of SU (Harty, Pedersen, Gnagy, Pelham, & Molina, Citation2015; Jensen et al., Citation2017; Mitchell et al., Citation2017), such as SU to cope with negative states, feel accepted and normal (Nehlin, Nyberg, & Oster, Citation2015), improve negative mood and ADHD symptomatology, and to get high (Canela, Buadze, Dube, Eich, & Liebrenz, Citation2017; Mitchell et al., Citation2017; Weisner et al., Citation2017; Wilens et al., Citation2007; Young et al., Citation2017). However, SUD+ADHD individuals have reported negative effects from SU, (e.g. increased impulsivity, aggression and social problems) (Kronenberg, Slager-Visscher, Goossens, van den Brink & van Achterberg, Citation2014; Nehlin et al., Citation2015). It is still unclear whether SUD+ADHD patients’ SU perceptions differ from SUD-ADHD. This is crucial since intentional changes are only possible after a thorough evaluation in which the pros of changing a problematic behavior outweigh the cons (McEvoy & Nathan, Citation2007; Prochaska, DiClemente, & Norcross, Citation1992). This requires adequate cognitive functioning (Blume, Schmaling, & Marlatt, Citation2005; Le Berre et al., Citation2012), which may be reduced among SUD+ADHD patients (Brooks et al., Citation2006).
SUD patients reporting severe SU, tend to choose treatment goals of total abstinence (Lozano et al., Citation2015; Lozano, Stephens, & Roffman, Citation2006) whereas those reporting less SU severity are less likely to choose total abstinence goals (DeMartini et al., Citation2014).There are no clear indications concerning which treatment goals SUD+ADHD patients prefer. In SUD treatment settings, treatment goals of total abstinence are associated with favorable outcomes (Adamson, Sellman, & Frampton, Citation2009; Berger, Brondino, Fisher, Gwyther, & Garbutt, Citation2016; Bujarski, O’Malley, Lunny, & Ray, Citation2013; Meyer, Wapp, Strik, & Moggi, Citation2014). However, substance reduction may be a viable treatment goal in some cases (van Amsterdam & van den Brink, Citation2013). As ambivalence is common among SUD patients (Schlauch, Crane, Connors, Dearing, & Maisto, Citation2019), total abstinence may not be an option for some. Additionally, allowing total abstinence as the only outcome may keep some individuals from seeking SUD treatment (Wallhed Finn, Bakshi, & Andreasson, Citation2014). The acceptance of substance reduction is growing in SUD treatment centers (Klingemann & Rosenberg, Citation2009), whereas others may be still reluctant to accept treatment goals different from total abstinence (Davis & Rosenberg, Citation2013). As a positive therapeutic alliance is paramount in SUD treatment (Project Match Group, Citation1997), efforts should be made to understand SUD+ADHD patients’ rationale behind their treatment goals choices, which may prevent treatment dropout. Evidently, more qualitative research on SUD+ADHD patients’ perceptions of SU and their choice of treatment goal is needed.
The aims of this study were to qualitatively investigate whether (1) the positive and negative perceptions of SU and (2) SU-related treatment goals were different among SUD+ADHD patients and SUD-ADHD patients.
1. Materials and methods
1.1. Participants
Between February 2010 and July 2012, previously detoxicated SUD inpatients were consecutively recruited from two SUD treatment units at the University hospital in Northern Norway the ReStart unit, and in the last two months of the recruitment period, the Færingen unit. Written and verbal information about the study was provided; 16 SUD+ADHD patients and 87 SUD-ADHD patients agreed to participate and signed an informed consent form.
The ADHD assessment (International Classification of Diseases 10th Revision, World Health Organization [WHO], Citation1992) was conducted by clinical experts, independently from this naturalistic study. We obtained information on the diagnosis of ADHD from medical records. The information on ADHD was well documented as per the national guidelines (Directorate of Health and Social Affairs, Citation2007). The mean age at ADHD assessment was 33.7 ± 10.5 years (range 18–50). Seven (58%) of the 16 SUD+ADHD patients were receiving psychostimulants (methylphenidate) during SUD treatment. More information about study participants and procedures is found in (Flores-Garcia et al., Citation2016).
This study comprises qualitative data from 12 of the 16 originally recruited SUD+ADHD patients, (four stopped treatment), and a subsample of 10 SUD-ADHD patients. Study participants were matched by age and SU severity, as young SUD patients seem to have high SU severity and a high dropout risk (Brorson, Ajo Arnevik, Rand-Hendriksen, & Duckert, Citation2013). The Regional Committee for Medical and Health Research Ethics granted approval for this study REK sør-øst B, 2009/1355b.
1.2. Measures and procedure
The ReStart unit and Færingen unit used the motivational interviewing (MI) (Rollnick & Miller, Citation1995) and Therapeutic community approaches (De Leon, Citation1999), respectively. Following treatment-as-usual (TAU) procedures, all study participants underwent M.I.N.I.PLUS (Sheehan et al., Citation1994) psychiatric interviews for the assessment of axis I disorders. Axis II disorders (Structured Clinical Interview for DSM-IV (SCID II) (First, Spitzer, Gibbon, Williams, & Benjamin, Citation1995) were only assessed when necessary. Substance use severity was assessed by the Alcohol Use Disorder Identification Test and the Drug Use Disorder Identification Test (Berman, Bergman, Palmstierna, & Schlyter, Citation2005; Saunders, Aasland, Babor, de la Fuente, & Grant, Citation1993). A semi-structured interview guide was developed by the leaders of the ReStart unit and the first author, which was adapted into a template form (see example in Appendix 1).
Participants were interviewed face-to-face and could attend as many interviews as they considered as necessary during their SUD treatment (range: 1–5 sessions). Most interviews took place at the beginning of treatment. They lasted about one hour each and were undertaken by a clinician with whom patients closely collaborated (both genders) or by the first author, who did not have a clinician role at the time of the study. Clinicians followed TAU procedures when administering the paper and pencil interview, which included (1) the perceived positive and negative aspects of SU and (2) the SU-related treatment goals. Study participants’ answers were documented in the template forms by the interviewers or, whenever preferred, by the participants themselves. Reading/writing assistance was provided. Since the treatment goals were meant to be evaluated at follow-up, patients were given a copy of the templates. Follow- up interviews were conducted three, six, and 12 months after discharge, including questions about non SU-related goals. This study exclusively reports the findings from interviews concerning SU-related goals during SUD treatment.
1.3. Data analysis
The reasoning of this study was deductive (i.e. top-down), contrary to inductive reasoning, which involves no previous conceptual bases (i.e. bottom-up reasoning) (Bengtsson, Citation2016; Elo & Kyngas, Citation2008). In content analysis there are two data analysis techniques: manifest and latent (Bengtsson, Citation2016). In manifest content analysis, the aim is to explicitly describe the data, whereas latent content analysis aims to be more in-depth (Bengtsson, Citation2016). Interview data were analyzed using manifest content analysis, following four steps: decontextualization, recontextualization, categorization, and compilation (Bengtsson, Citation2016). For the decontextualization step, LFG and MK separately initiated the open-coding process (i.e. finding meaning units in the original texts), looking for patterns. Each author entered preliminary simple codes into a logbook and LFG reviewed these codes in relation to the original text, recoding when considered appropriate. The logbook was updated every time the codes were reviewed. This step was conducted several times, until agreement upon the final codes was reached. For the recontextualization step, LFG and MK reviewed the final codes, excluding unrelated study topics and including relevant unclassified text. In the categorization step, provisional categories were created by organizing codes with similar patterns. The category descriptions were constructed from the data (Bengtsson, Citation2016; Elo & Kyngas, Citation2008) by LFG, MK and TNB. Inter-rater reliability was conducted (Hallgren, Citation2012) . In order to improve validity in the compilation step, codes and categories were first revisited by LFG and MK in relation to the original text, and then a second time by TNB. Frequency endorsements of codes and categories for SU aspects and treatment goals were summarized. The perceived positive and negative aspects of SU were categorized as intrapersonal and interpersonal. We mainly focused on the intrapersonal aspects, briefly mentioning the interpersonal since saturation was not reached in the latter. Treatment goals were classified by how concretely they were stated. Participants did not provide feedback on the findings. Examples of the coding process are shown in Table .
Table 1. Examples of the coding process. Interviews on the Positive and Negative Aspects of Substance Use and Treatment Goals
2. Results
Two of the patients in the study sample were from the Færingen unit. All patients but one (SUD+ADHD) were voluntarily receiving SUD treatment. Mann-Whitney U tests (Table ) confirmed that no significant differences were observed in age or degree of SU severity between the SUD+ADHD and SUD-ADHD patients. The majority had previously completed SUD treatment and consumption of more than one substance was common in both SUD groups. Kappa coefficients across all the categories were .65 > (from substantial to perfect), with an average of .85.
Table 2. Sociodemographic and clinical characteristics
2.1. Perceived positive aspects of substance use
Positive intrapersonal aspects of SU included: self- regulation of physical health, behavior, feelings, reasoning/thoughts, and the rewarding effects of SU (Table ). Positive interpersonal aspects comprised SU for social gathering, or drinking with meals. Compared to SUD-ADHD patients, SUD+ADHD patients rarely perceived SU as having positive effects on self-regulation of physical health, and more often perceived SU as having positive effects on self-regulation of behavior. Both SUD groups perceived SU as positive for the self-regulation of feelings, reasoning/thoughts, as well as for the rewarding effects, with a similar frequency.
Table 3. Description and frequency endorsement of the self-reported Positive and Negative Aspects of Substance Use in SUD patients with (N = 12) and without ADHD (N = 10)
2.1.1. Self-regulation of physical health
Self-regulation of physical health was predominantly mentioned by SUD-ADHD patients. SU was considered to alleviate physical pain, improve sleep quality and appetite. For instance:
“I sleep very well” (SUD-ADHD P10, alcohol).
Substances were additionally perceived to counteract withdrawals caused by other substances:
“It (cannabis) lessens the suboxone withdrawal” (SUD-ADHD P6).
2.1.2. Self-regulation of behavior
Patients used substances to help them redirect unwanted behavior, and to complete or cope with activities perceived as demanding. These SU perceptions were described to a greater degree by SUD+ADHD patients across different substances. SUD+ADHD P1 said:
” I start using without thinking about it. Amphetamine allows me to control my impulsivity. I function normally, getting things done”.
In this example SU was initiated by impulsive behavior and paradoxically, SU was perceived to manage the impulsivity. SUD+ADHD P6 said:
“It (amphetamine) keeps me from doing harmful/impulsive things”.
Similar to the previous example, P6 perceived that SU helped stop unwanted behavior. SUD+ADHD P4 expressed that SU assisted in everyday life functioning and in relating to others:
“I am able to socialize” (alcohol)
”It helps me in my everyday life” (benzodiazepines).
SUD+ADHD P10 asserted that alcohol helped to pause an activity at hand allowing him to switch to a more enjoyable task.
“To postpone important tasks. I have a tendency to do a lot of one specific thing. I want to allow myself to do meaningless things” SUD+ADHD P10.
Some of the SUD-ADHD patients linked SU to improved productivity:
“I become hard-working” (P5, amphetamine).
2.1.3. Self-regulation of feelings
The positive effects of SU to self-regulate feelings was expressed as the substances helping to improve negative feelings or cope with overwhelming feelings. For instance:
“It helps relieve the anxiety so I can tolerate being on my own company. It is better to use medication that is addictive than to have no quality of life at all” (SUD+ADHD P8, benzodiazepines).
P8 accepted having a benzodiazepine addiction, experiencing that its use reduced negative feelings in order to tolerate his own company. Other examples of perceived positive mood changes due to SU were “to calm down”, “to stop boredom” and “feeling good about oneself.” For instance:
“I feel happy” (SUD-ADHD P7, alcohol).
2.1.4. Self-regulation of reasoning/thoughts
The perceived positive effects of SU in reasoning/thoughts involved improve positive thinking, cognitive endurance, concentration, and limiting negative thoughts (e.g. “flashbacks disappear” and “increased self-knowledge/self-confidence”). Other examples include:
“At first, you become collected” (alcohol), and “I become creative, sharp” (amphetamine) (SUD+ADHD P12).
“I become more focused” (SUD-ADHD P2, amphetamine).
P12 experienced being collected and creative when using alcohol and amphetamines; P2 reported similar effects by amphetamines.
2.1.5. The rewarding effects
The rewarding effects of SU were meant to enhance pleasant effects, and did not have self-regulating purposes. Some examples provided were “becoming comfortably numb when talking too much,” the enjoyment of “getting high,” “euphoria,” “laughter,” and “stronger sensory impressions”. The rewarding effects of SU were expressed across different substances:
“I have experienced many good trips” (SUD+ADHD P5, amphetamine).
Some patients noted that combining substances intensified the rewarding effects:
“I feel pleasure when used in combination with heroin” (SUD-ADHD P8, benzodiazepines).
2.2. Negative aspects of substance use
The perceived negative aspects of SU followed themes similar to the positive aspects including the consequences of SU on physical health, behavior, feelings, and reasoning/thoughts (Table ). The negative interpersonal consequences comprised ruptures in close relationships, economic problems, loss of drivers’ licenses, and legal problems.
2.2.1. Consequences on physical health
As with the perceived positive aspects, SUD+ADHD patients uncommonly related SU to physical health consequences compared to SUD-ADHD patients. This category included problems with blood pressure, oral health, sleep issues, decreased appetite and digestive problems, hepatitis, weight gain, breathing difficulties and increased physical pain:
”I become weak, in pain, have a bad appetite. I become tired and hungry” (SUD-ADHD P5, amphetamine).
P5 mentioned the diverse physical consequences of amphetamine use. SUD+ADHD P8 expressed:
“It (heroin) destroys the veins”.
2.2.2. Consequences on behavior
SU negatively impacted behavior, resulting in passivity, aggression, and a reduced control over such as “becoming inactive, passive and postponing tasks,” “saying or doing things I did not intend to,” “losing spontaneity,” and “having to use a lot of it”. The negative actions were unintended:
“I become aggressive if I drink spirits or too much” (SUD+ADHD P11, alcohol).
“The addictive behavior. I am out of control, with aggressive behavior” (SUD-ADHD P4, alcohol).
2.2.3. Consequences on feelings
The negative consequences of SU on feelings varied in intensity, from expressing
depressed mood to emotional numbness. For instance:
“I might experience depression. It might be strengthened by alcohol” (SUD+ADHD P9, alcohol).
“I become emotionally blunted” (SUD-ADHD P1, benzodiazepines).
Other commonly mentioned consequences of feelings were expressed as “the worsening of anxiety,” “feeling unease,” “being unmotivated,” and “becoming irritable or angry.”
2.2.4. Consequences on reasoning/thoughts
For some patients, SU resulted in weakened reasoning/thoughts (e.g. “losing sense of time and place,” and having “deteriorated memory and concentration.” Further, participants described mental exhaustion and decision-making that was contrary to their own moral standards:
“I become mentally tired” (SUD+ADHD P7, amphetamine).
“My ability to make the right decisions decreases. I have low scruples” (SUD-ADHD P4, amphetamine).
Other consequences on reasoning/thoughts included “having psychotic thoughts,” and “remorse.”
In sum, SUD+ADHD patients less frequently linked SU to physical health (either positively or negatively) compared to SUD-ADHD patients. Furthermore, SUD+ADHD patients more frequently linked SU to positive changes in behavior than SUD-ADHD patients. Otherwise, the SUD groups had similar perceptions across the different substances.
2.3. Substance use-related treatment goals
Four treatment goals categories were identified. Total abstinence, which referred to clear statements of wanting to completely abstain from SU. When multiple substances were involved total abstinence was sometimes limited to one specific substance. Conditional abstinence consisted of quitting SU or refraining from illegal use, on the condition of initiating, changing, or increasing the dosage in the prescription medication. Substance reduction consisted of reduced SU in frequency and amount compared to the consumption before entering SUD treatment. Unspecified consisted of vague statements of avoiding SU or indirectly related to SU.
2.3.1. Treatment goals of total abstinence
This category comprised clear statements of wanting to abstain completely from SU, such as “I won’t use the substance anymore,” “stay clean for good,” or “quit using”. For instance, SUD-ADHD P10 said:
“I want alcohol to be completely absent. I am sober today. I want to keep being sober”.
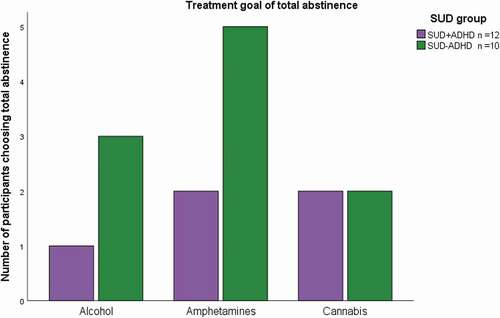
P10 clearly preferred to continue abstaining from alcohol use. Treatment goals of total abstinence were less common among SUD+ADHD patients compared to SUD-ADHD patients. Figure depicts the frequency in which total abstinence goals were chosen. SU was limited to alcohol, amphetamines, and cannabis as these were the most frequently used substances by both SUD groups.
Figure indicates that compared to SUD-ADHD patients, SUD+ADHD patients less frequently preferred total abstinence concerning alcohol and amphetamines.
2.3.2. Treatment goals of conditional total abstinence
Conditional total abstinence (i.e. abstaining totally from SU or stop illegal use if changes in pharmacological treatment status were made). This category was represented by SUD+ADHD patients, P6 expressed the following:
“Stay away from illegal use of amphetamines for medicinal use. Don’t take amphetamine unless I start with dextroamphetamine.”
P6, was receiving methylphenidate and would compromise to stop illegally buying amphetamines if the current prescription was changed to dextroamphetamine (a more potent stimulant) (Kolar et al., Citation2008). Although the example above refers to amphetamines, other substances were described similarly:
“To eliminate illegal use of benzodiazepines. In the past, when I received the right benzodiazepine dose, I stopped using illegally” (SUD+ADHD P8).
P8 was able to stay away from illegal benzodiazepine use in the past when receiving an adequate dose. P8 would eliminate illegal use if the medication dosage was increased.
2.3.3. Treatment goals of substance reduction
Substance reduction goals were somewhat common among SUD+ADHD patients. Examples of treatment goals of reduced SU are provided below:
“Try to reduce. Drink for example once a month without getting drunk” (SUD+ADHD P1).
“Abstain from alcohol while I am under SUD treatment. Drink a couple of beers once a month. So that alcohol does not affect my everyday life” (SUD+ADHD P12).
Substance reduction was also mentioned by a few SUD-ADHD patients:
“Take a break from cannabis. Get in control, don’t feel powerless. I want to use 1–2 grams about 1–2 times a week” (SUD-ADHD P2).
P2 wanted to limit the amount and episodes of cannabis use.
2.3.4. Unspecified treatment goals
Unspecified treatment goals were frequent in both SUD groups. Statements such as “wishing not to use,” “trying to avoid using,” or those not directly related to SU were categorized as unspecified:
”Dare to open up about my alcohol problem” (SUD+ADHD P3).
P3 did not express a concrete goal concerning alcohol use.
Whenever more than one substance was involved, SUD+ADHD patients commonly chose different goals across the different substances, while the SUD-ADHD patients frequently had the same goals. For instance, when asked about the treatment goals for each substance, SUD+ADHD P4 decided on total abstinence from amphetamine and reduction in alcohol use:
“No more amphetamine.”
“Abstaining completely from drinking (alcohol) until the next follow-up, but eventually drink normally.”
Similarly, SUD+ADHD P11 wanted to completely abstain from benzodiazepine use, was unclear about cannabis, and expressed ambivalence toward alcohol:
“I won’t use benzodiazepines anymore.”
“avoid using cannabis.”
“I want to find out which goal I want to have in relation to alcohol. It is not a problem in itself, but I am starting to wonder whether I should stop drinking. Can it lead to other substance use? Can I become addicted to alcohol instead of other substances?”
In contrast, the SUD-ADHD patients tended to report the same goals across the different substances of use. For example, concerning total abstinence, P9 reported:
“To continue abstaining totally” (SUD-ADHD P9, amphetamine and cannabis).
In the following case, SUD-ADHD P1 expressed similar goal patterns concerning alcohol and benzodiazepines. Both cases were categorized as unspecified:
“I want to take one day at a time” (alcohol).
“Accept that the doctor refuses to prescribe me benzodiazepines.”
In sum, SUD+ADHD patients chose treatment goals of total abstinence less frequently than the SUD-ADHD patients. Additionally, those SUD+ADHD patients using more than one substance commonly set different treatment goals across the different substances, while SUD-ADHD patients usually had similar goals across the different substances. Unspecified treatment goals were observed in both SUD groups.
3. Discussion
We explored whether SUD+ADHD and SUD-ADHD patients had different positive and negative perceptions of SU and preferred different treatment goals. We found that SUD+ADHD patients rarely perceived neither positive nor negative aspects of SU related to physical health, and more frequently perceived positive effects of SU on self-regulation of behavior. Otherwise, the SUD groups expressed similar perceptions. With regard to the SU-related treatment goals, SUD+ADHD patients set total abstinence less frequently. Additionally, the treatment goals among SUD+ADHD patients using more than one substance were variable across the different substances, whereas among SUD-ADHD patients consuming more than one substance, treatment goals were similar across the different substances. It was unclear why SUD+ADHD patients seldom linked SU to physical health. Since both SUD groups showed similar SU profiles and high SU severity, it was plausible to expect that both groups also perceived similar effects of SU on physical health. This finding contradicts previous studies showing that individuals with SUD+ADHD consider that SU negatively impacts their physical health (Jensen et al., Citation2017; Kronenberg et al., Citation2014). One possible explanation is that SUD-ADHD patients were in worse somatic health than SUD-ADHD patients. Alternatively, the cognitive issues associated with ADHD (Brooks et al., Citation2006; Marx, Krause, Berger, & Hassler, Citation2014), possibly interfered with SUD+ADHD patients’ evaluations of the pros and cons of SU on their physical health.
The findings that SUD+ADHD patients perceived that SU was positive for self-regulating unwanted behavior (e.g. impulsivity) supports previous studies (Kronenberg et al., Citation2014; Nehlin et al., Citation2015). Potentially, the behavioral impulsivity inherent in ADHD (Crunelle, Veltman, van Emmerik-van Oortmerssen, Booij, & van den Brink, Citation2013) may explain the positive link between SU and self-regulation of behavior made by these participants. However, this is a hypothesis that needs to be further investigated.
The findings that the SUD groups perceived SU as positive for the self-regulation of feelings, reasoning/thoughts and the rewarding effects are in line with previous studies on individuals with problematic SU with and without ADHD (Mitchell et al., Citation2017; Wilens et al., Citation2007). Interestingly, both SUD groups expressed seeking SU for their rewarding effects (enjoying the high/being drunk). Novelty seeking (e.g. impulsive seeking of highly rewarding events) (Cloninger, Przybeck, Svrakic, & Wetzel, Citation1994) has been associated with SUD (Palmer et al., Citation2013) and ADHD (Perroud et al., Citation2016). The most recognized hypotheses on the link between SUD and ADHD are self-medication (SU to relieve negative states) (Khantzian, Citation1985) and a biological predisposition to seek immediate rewards (Ortal et al., Citation2015; Sousa et al., Citation2011; S. Young & Sedgwick, Citation2015). The present results are in line with both hypotheses.
A trend in which SUD+ADHD patients rarely preferred treatment goals of total abstinence was observed. To our knowledge, there is no research on this topic among SUD+ADHD patients. However, some SUD field studies have suggested that individuals consider changing their problematic SU when they experience greater cons than pros from SU in their lives (DeMartini et al., Citation2014; Prochaska et al., Citation1992). The findings on the SU-perceptions suggest that SUD+ADHD patients experienced more pros than cons from SU. This may explain why they less commonly preferred total abstinence goals. The finding that SUD+ADHD patients had variable treatment goals whenever multiple substances were involved may be related to problem-solving difficulties associated with ADHD (Young, Citation2005).
Notably, unspecified SU-related goals were frequent in both groups. These may be expressions of ambivalence, common among individuals with SUD (Magill, Stout, & Apodaca, Citation2013; Schlauch et al., Citation2019). However, we cannot rule out that treatment goals categorized as unspecified were merely a result of methodological issues (e.g. how the questions were asked and interpreted by the interviewers and participants, coding process, etc). Additionally, as motivation toward total abstinence may be strongest early in treatment, eventually decreasing (Wallhed Finn et al., Citation2014), the timing in which the interviews were conducted might have been crucial in participants’ treatment goals preferences.
Overall, our findings of how substances positively and negatively affected patients’ feelings, reasoning/thoughts, physical health, behavior, and social relations support the current biopsychosocial understanding of SUD (APA, Citation2013; Saunders et al., Citation2018). Furthermore, this apparent contradiction in which SU may represent a sustained way to cope with negative states and, paradoxically exacerbate them, may reflect the negative cycle inherent in SUD, as previously reported (Kronenberg et al., Citation2014; Pettersen, Ruud, Ravndal, & Landheim, Citation2013). The present results indicate that SUD+ADHD patients’ relation to their SU is highly complex.
3.1. Clinical implications
SUD+ADHD patients may require more guidance than SUD-ADHD patients in assessing the positive and negative effects of SU and in setting treatment goals compatible with their degree of SU and life goals. We recommend the following interventions: A) SUD+ADHD patients should be systematically asked about their SU perceptions, including physical health previous to setting treatment goals. B) SU severity should be systematically assessed. This may enable a better understanding of SUD+ADHD patients’ rationale behind their SU, and compensate for potential problem-solving difficulties. The updated definition of SUD (APA, Citation2013; Saunders et al., Citation2018), may be a useful guideline to appropriately assess SU severity. C) To avoid attrition, alternative goals to total abstinence should be considered. D) A meaningful therapeutic alliance may facilitate a common understanding of patients’ SU perceptions and goals.
3.2. Limitations
The number of participants in this study was relatively small. Additionally, to reduce patient burden, in-depth interviews were not conducted. Consequently, crucial themes concerning everyday functioning, emotional liability, and psychostimulant treatment remained unexplored. Furthermore, although the vast majority of study participants were recruited from the ReStart unit, participants from the Færingen unit might have provided answers according this units’ TAU practice. Moreover, our findings may be attributed to methodological procedures, not ADHD status. No information was obtained from four SUD+ADHD patients (treatment drop-outs) who may have had greater SU severity. The present finings should be considered as preliminary, as further research on this topic is needed.
Acknowledgements
The authors thank Hanne Nergård and Henrik Broberg of the Færingen unit who assisted in the recruitment process, the clinicians of the ReStart unit who assisted in the recruitment process and conducted the interviews, Assoc. Prof Elinor Ytterstad who conducted the subsampling presented in this study and all participants, for your time and dedication to this study.
Additional information
Funding
Notes on contributors
Lizbett Flores-García
Lizbett Flores-García MSc. Research fellow at the University Hospital of Northern Norway and UiT the Arctic University of Norway. Her research interest is in substance use disorders and ADHD.
Michael B. Lensing
Michael B. Lensing PhD. Senior advisor at the Norwegian Centre of Expertise for Neurodevelopmental Disorders and Hypersomnias at Oslo University Hospital. His main research interest is in ADHD, autism spectrum disorders, Tourette syndrome, and rare diseases.
Trond N. Bjerke
Trond N. Bjerke PhD. Head of research on addictions at the University Hospital of Northern Norway. His main research interest is in addictions, particularly physical activity in treatment of substance use disorders.
Martin Kvalnes
Martin Kvalnes Cand. Philol. Senior counselor at the University Hospital of Northern Norway. His main research interest is in substance use disorders from a social and historical perspective.
Martin Eisemann
Martin Eisemann Professor at Psychology Department, UiT the Arctic University of Norway. His main research interest is in personality psychology and vulnerability models of psychopathology.
References
- Adamson, S. J., Sellman, J. D., & Frampton, C. M. (2009). Patient predictors of alcohol treatment outcome: A systematic review. Journal of Substance Abuse Treatment, 36(1), 75–20. doi:10.1016/j.jsat.2008.05.007.
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author.
- Bengtsson, M. (2016). How to plan and perform a qualitative study using content analysis. NursingPlus Open, 2, 8–14. doi:10.1016/j.npls.2016.01.001
- Berger, L., Brondino, M., Fisher, M., Gwyther, R., & Garbutt, J. C. (2016). Alcohol use disorder treatment: The association of pretreatment use and the role of drinking goal. Journal of the American Board of Family Medicine, 29(1), 37–49. doi:10.3122/jabfm.2016.01.150143
- Berman, A. H., Bergman, H., Palmstierna, T., & Schlyter, F. (2005). Evaluation of the drug use disorders identification test (DUDIT) in criminal justice and detoxification settings and in a Swedish population sample. European Addiction Research, 11(1), 22–31. doi:10.1159/000081413
- Blume, A. W., Schmaling, K. B., & Marlatt, G. A. (2005). Memory, executive cognitive function, and readiness to change drinking behavior. Addictive Behaviors, 30(2), 301–314. doi:10.1016/j.addbeh.2004.05.019
- Brooks, D. J., Vosburg, S. K., Evans, S. M., & Levin, F. R. (2006). Assessment of cognitive functioning of methadone-maintenance patients: Impact of adult ADHD and current cocaine dependence. Journal of Addictive Diseases, 25(4), 15–25. doi:10.1300/J069v25n04_02
- Brorson, H. H., Ajo Arnevik, E., Rand-Hendriksen, K., & Duckert, F. (2013). Drop-out from addiction treatment: A systematic review of risk factors. Clinical Psychology Review, 33(8), 1010–1024. doi:10.1016/j.cpr.2013.07.007
- Bujarski, S., O’Malley, S. S., Lunny, K., & Ray, L. A. (2013). The effects of drinking goal on treatment outcome for alcoholism. Journal of Consulting and Clinical Psychology, 81(1), 13–22. doi:10.1037/a0030886
- Canela, C., Buadze, A., Dube, A., Eich, D., & Liebrenz, M. (2017). Skills and compensation strategies in adult ADHD - A qualitative study. Plos One, 12(9), e0184964.
- Chen, K. W., Banducci, A. N., Guller, L., Macatee, R. J., Lavelle, A., Daughters, S. B., & Lejuez, C. W. (2011). An examination of psychiatric comorbidities as a function of gender and substance type within an inpatient substance use treatment program. Drug and Alcohol Dependence, 118(2–3), 92–99. doi:10.1016/j.drugalcdep.2011.03.003
- Cloninger, R. C., Przybeck, T., Svrakic, D., & Wetzel, R. D. (1994). The temperament and character inventory (TCI): A guide to its development and use. St Louis, MO: Center for Psychobiology of Personality, Washington University.
- Crunelle, C. L., Veltman, D. J., van Emmerik-van Oortmerssen, K., Booij, J., & van den Brink, W. (2013). Impulsivity in adult ADHD patients with and without cocaine dependence. Drug and Alcohol Dependence, 129(1–2), 18–24. doi:10.1016/j.drugalcdep.2012.09.006
- Davis, A. K., & Rosenberg, H. (2013). Acceptance of non-abstinence goals by addiction professionals in the United States. Psychology of Addictive Behaviors, 27(4), 1102–1109. doi:10.1037/a0030563
- De Leon, G. (1999). Therapeutic communities. In H. K. M. Galanter (Ed.), Textbook of substance abuse treatment (2nd ed., pp. 447–462). Washington, DC: American Psychiatric Press.
- DeMartini, K. S., Devine, E. G., DiClemente, C. C., Martin, D. J., Ray, L. A., & O’Malley, S. S. (2014). Predictors of pretreatment commitment to abstinence: Results from the COMBINE study. Journal of Studies on Alcohol and Drugs, 75(3), 438–446. doi:10.15288/jsad.2014.75.438
- Directorate of Health and Social Affairs. (2007). Veileder i diagnostikk og behandling av AD/HD: Diagnostikk og behandling av hyperkinetisk forstyrrelse/attention deficit hyperactivity disorder (AD/HD) hos barn, ungdom og voksne IS-1244. [National guidelines for diagnosis and treatment of AD/HD. in children, adolescentes and adults (IS-1244)]. (IS 1244). Oslo, Norway: Sosial-og Helsedirektoratet.
- Elo, S., & Kyngas, H. (2008). The qualitative content analysis process. Journal of Advanced Nursing, 62(1), 107–115. doi:10.1111/j.1365-2648.2007.04569.x
- First, M. B., Spitzer, R. L., Gibbon, M., Williams, J. B. W., & Benjamin, L. (1995). Structured clinical interview for DSM-IV (SCID II). New York: State Psychiatric Institute.
- Flores-Garcia, L., Ytterstad, E., Lensing, M. B., & Eisemann, M. (2016). Exploring personality and readiness to change in patients with substance use disorders with and without ADHD. Journal of Attention Disorders. doi:10.1177/1087054716677819.
- Hallgren, K. A. (2012). Computing inter-rater reliability for observational data: An overview and tutorial. Tutorials in Quantative Methods for Psychology, 8(1), 23–34. doi:10.20982/tqmp.08.1.p023
- Harty, S. C., Pedersen, S. L., Gnagy, E. M., Pelham, W. E., Jr., & Molina, B. S. (2015). ADHD and Marijuana-Use expectancies in young adulthood. Substance Use & Misuse, 50(11), 1470–1478. doi:10.3109/10826084.2015.1018545
- Jensen, P. S., Yuki, K., Murray, D., Mitchell, J. T., Weisner, T., Hinshaw, S., … Wells, K. (2017). Turning Points in the lives of youth of with/without ADHD: Are they linked to changes in substance use?. Journal of Attention Disorders, 22(9_suppl), 38s–48s. doi:10.1177/1087054717700977
- Kalbag, A. S., & Levin, F. R. (2005). Adult ADHD and substance abuse: Diagnostic and treatment issues. Substance Use & Misuse, 40(13–14), 1955–1981, 2043–1958. doi:10.1080/10826080500294858
- Khantzian, E. J. (1985). The self-medication hypothesis of addictive disorders: Focus on heroin and cocaine dependence. American Journal of Psychiatry, 142(11), 1259–1264.
- Kim, J. W., Park, C. S., Hwang, J. W., Shin, M. S., Hong, K. E., Cho, S. C., & Kim, B. N. (2006). Clinical and genetic characteristics of Korean male alcoholics with and without attention deficit hyperactivity disorder. Alcohol and Alcoholism, 41(4), 407–411. doi:10.1093/alcalc/agl034
- Klingemann, H., & Rosenberg, H. (2009). Acceptance and therapeutic practice of controlled drinking as an outcome goal by Swiss alcohol treatment programmes. European Addiction Research, 15(3), 121–127. doi:10.1159/000210041
- Kolar, D., Keller, A., Golfinopoulos, M., Cumyn, L., Syer, C., & Hechtman, L. (2008). Treatment of adults with attention-deficit/hyperactivity disorder. Neuropsychiatric Diseases and Treatment, 4(2), 389–403.
- Kronenberg, L. M., Slager-Visscher, K., Goossens, P. J., van den Brink, W., & van Achterberg, T. (2014). Everyday life consequences of substance use in adult patients with a substance use disorder (SUD) and co-occurring attention deficit/hyperactivity disorder (ADHD) or autism spectrum disorder (ASD): a patient's perspective. Bmc Psychiatry, 14, 264. doi:10.1186/s12888-014-0264-1
- Le Berre, A. P., Vabret, F., Cauvin, C., Pinon, K., Allain, P., Pitel, A. L., … Beaunieux, H. (2012). Cognitive barriers to readiness to change in alcohol-dependent patients. Alcoholism Clinical and Experimental Research, 36(9), 1542–1549. doi:10.1111/j.1530-0277.2012.01760.x
- Lozano, B. E., Gros, D. F., Killeen, T., Jaconis, M., Beylotte, F. M., 3rd, Boyd, S., & Back, S. E. (2015). To reduce or abstain? Substance use goals in the treatment of veterans with substance use disorders and comorbid PTSD. The American Journal on Addictions, 24(7), 578–581. doi:10.1111/ajad.12263
- Lozano, B. E., Stephens, R. S., & Roffman, R. A. (2006). Abstinence and moderate use goals in the treatment of marijuana dependence. Addiction, 101(11), 1589–1597. doi:10.1111/add.2006.101.issue-11
- Magill, M., Stout, R. L., & Apodaca, T. R. (2013). Therapist focus on ambivalence and commitment: A longitudinal analysis of motivational interviewing treatment ingredients. Psychology of Addictive Behaviors, 27(3), 754–762. doi:10.1037/a0029639
- Marx, I., Krause, J., Berger, C., & Hassler, F. (2014). Dissociable patterns in the control of emotional interference in adults with attention-deficit/hyperactivity disorder (ADHD) and in adults with alcohol dependence. Plos One, 9(9), e107750. doi:10.1371/journal.pone.0107750
- Matthys, F., Soyez, V., van den Brink, W., Joostens, P., Tremmery, S., & Sabbe, B. (2014). Barriers to implementation of treatment guidelines for ADHD in adults with substance use disorder. Journal of Dual Diagnosis, 10(3), 130–138. doi:10.1080/15504263.2014.926691
- McEvoy, P. M., & Nathan, P. (2007). Perceived costs and benefits of behavioral change: Reconsidering the value of ambivalence for psychotherapy outcomes. Journal of Clinical Psychology, 63(12), 1217–1229. doi:10.1002/(ISSN)1097-4679
- Meyer, A., Wapp, M., Strik, W., & Moggi, F. (2014). Association between drinking goal and alcohol use one year after residential treatment: A multicenter study. Journal of Addictive Diseases, 33(3), 234–242. doi:10.1080/10550887.2014.950025
- Mitchell, J. T., Weisner, T. S., Jensen, P. S., Murray, D. W., Molina, B. S., Arnold, E. L., … Nguyen, J. L. (2017). How Substance users with ADHD perceive the relationship between substance use and emotional functioning. Journal of Attention Disorders, (9_suppl), 49s–60s. doi:10.1177/1087054716685842
- Nehlin, C., Nyberg, F., & Oster, C. (2015). The patient’s perspective on the link between ADHD and substance use: A qualitative interview study. Journal of Attention Disorders, 19(4), 343–350. doi:10.1177/1087054714554618
- Ortal, S., van de Glind, G., Johan, F., Itai, B., Nir, Y., Iliyan, I., & van den Brink, W. (2015). The role of different aspects of impulsivity as independent risk factors for substance use disorders in patients with ADHD: A review. Current Drug Abuse Reviews, 8(2), 119–133. doi:10.2174/1874473708666150916112913
- Palmer, R. H., Knopik, V. S., Rhee, S. H., Hopfer, C. J., Corley, R. C., Young, S. E., … Hewitt, J. K. (2013). Prospective effects of adolescent indicators of behavioral disinhibition on DSM-IV alcohol, tobacco, and illicit drug dependence in young adulthood. Addictive Behaviors, 38(9), 2415–2421. doi:10.1016/j.addbeh.2013.03.021
- Perroud, N., Hasler, R., Golay, N., Zimmermann, J., Prada, P., Nicastro, R., … Baud, P. (2016). Personality profiles in adults with attention deficit hyperactivity disorder (ADHD). Bmc Psychiatry, 16, 199. doi:10.1186/s12888-016-0906-6
- Pettersen, H., Ruud, T., Ravndal, E., & Landheim, A. (2013). Walking the fine line: Self-reported reasons for substance use in persons with severe mental illness. International Journal of Qualitative Studies on Health and Well-being, 8, 21968. doi:10.3402/qhw.v8i0.21968
- Prochaska, J. O., DiClemente, C. C., & Norcross, J. C. (1992). In search of how people change. Applications to addictive behaviors. American Psychologist, 47(9), 1102–1114. doi:10.1037/0003-066X.47.9.1102
- Project Match Group. (1997). Matching alcoholism treatment to client heterogenety: Project MATCH post treatment drinking outcomes. Journal of Studies on Alcohol, 58(1), 7–29. doi:10.15288/jsa.1997.58.7
- Rollnick, S., & Miller, W. R. (1995). What is Motivational Interviewing? Behavioural and Cognitive Psychotherapy, 23(4), 325–334. doi:10.1017/S135246580001643X
- Roncero, C., Ortega, L., Perez-Pazos, J., Lligona, A., Abad, A. C., Gual, A., … Daigre, C. (2015). Psychiatric comorbidity in treatment-seeking alcohol dependence patients with and without ADHD. Journal of Attention Disorders, 23(12), 1497–1504. doi:10.1177/1087054715598841
- Saunders, J. B., Aasland, O. G., Babor, T. F., de la Fuente, J. R., & Grant, M. (1993). Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption–II. Addiction, 88(6), 791–804. doi:10.1111/add.1993.88.issue-6
- Saunders, J. B., Peacock, A., & Degenhardt, L. (2018). Alcohol use disorders in the draft ICD-11, and how they compare with DSM-5. Current Addiction Reports, 5(2), 257–264. doi:10.1007/s40429-018-0197-8
- Schlauch, R. C., Crane, C. A., Connors, G. J., Dearing, R. L., & Maisto, S. A. (2019). The role of craving in the treatment of alcohol use disorders: The importance of competing desires and pretreatment changes in drinking. Drug and Alcohol Dependence, 199, 144–150. doi:10.1016/j.drugalcdep.2019.02.027
- Sheehan, D., Janavs, J., Baker, R., Harnett-Shehaan, K., Knapp, E., & Sheehan, M. (1994). Mini international neuropsychiatric interview. Tampa: University of South Florida.
- Sousa, N. O., Grevet, E. H., Salgado, C. A. I., Silva, K. L., Victor, M. M., Karam, R. G., … Bau, C. H. D. (2011). Smoking and ADHD: An evaluation of self medication and behavioral disinhibition models based on comorbidity and personality patterns. Journal of Psychiatric Research, 45(6), 829–834. doi:10.1016/j.jpsychires.2010.10.012
- Torok, M., Darke, S., & Kaye, S. (2012). Attention deficit hyperactivity disorder and severity of substance use: The role of comorbid psychopathology. Psychology of Addictive Behaviors, 26(4), 974–979. doi:10.1037/a0027846
- van Amsterdam, J., & van den Brink, W. (2013). Reduced-risk drinking as a viable treatment goal in problematic alcohol use and alcohol dependence. Journal of Psychopharmacology, 27(11), 987–997. doi:10.1177/0269881113495320
- van de Glind, G., Konstenius, M., Koeter, M. W. J., van Emmerik-van Oortmerssen, K., Carpentier, P.-J., Kaye, S., … Young, J. (2014). Variability in the prevalence of adult ADHD in treatment seeking substance use disorder patients: Results from an international multi-center study exploring DSM-IV and DSM-5 criteria. Drug and Alcohol Dependence, 134, 158–166. doi:10.1016/j.drugalcdep.2013.09.026
- van Emmerik-van Oortmerssen, K., van de Glind, G., Koeter, M. W. J., Allsop, S., Auriacombe, M., Barta, C., … Young, J. T. (2014). Psychiatric comorbidity in treatment-seeking substance use disorder patients with and without attention deficit hyperactivity disorder: Results of the IASP study. Addiction, 109(2), 262–272. doi:10.1111/add.12370
- Wallhed Finn, S., Bakshi, A. S., & Andreasson, S. (2014). Alcohol consumption, dependence, and treatment barriers: Perceptions among nontreatment seekers with alcohol dependence. Substance Use & Misuse, 49(6), 762–769. doi:10.3109/10826084.2014.891616
- Weisner, T. S., Murray, D. W., Jensen, P. S., Mitchell, J. T., Swanson, J. M., Hinshaw, S. P., … Stehli, A. (2017). Follow-up of young adults with ADHD in the MTA: Design and methods for qualitative interviews. Journal of Attention Disorders, 22(9_suppl), 10s–20s. doi:10.1177/1087054717713639.
- Wilens, T. E., Adamson, J., Sgambati, S., Whitley, J., Santry, A., Monuteaux, M. C., & Biederman, J. (2007). Do individuals with ADHD self-medicate with cigarettes and substances of abuse? Results from a controlled family study of ADHD. The American Journal on Addictions, 16(Suppl 1), 14–21; quiz 22–13. doi:10.1080/10550490601082742
- Wilens, T. E., & Biederman, J. (2006). Alcohol, drugs, and attention-deficit/hyperactivity disorder: A model for the study of addictions in youth. Journal of Psychopharmacology, 20(4), 580–588. doi:10.1177/0269881105058776
- Wilens, T. E., Kwon, A., Tanguay, S., Chase, R., Moore, H., Faraone, S. V., & Biederman, J. (2005). Characteristics of adults with attention deficit hyperactivity disorder plus substance use disorder: The role of psychiatric comorbidity. American Journal on Addictions, 14(4), 319–327. doi:10.1080/10550490591003639
- World Health Organization. (1992). The ICD-10 classification of mental and behavioural disorders: Clinical descriptions and diagnostic guidelines. Geneva, Switzerland: Author.
- Young, J. T., Carruthers, S., Kaye, S., Allsop, S., Gilsenan, J., Degenhardt, L., … Preen, D. (2015). Comorbid attention deficit hyperactivity disorder and substance use disorder complexity and chronicity in treatment-seeking adults. Drug and Alcohol Review, 34(6), 683–693. doi:10.1111/dar.2015.34.issue-6
- Young, S. (2005). Coping strategies used by adults with ADHD. Personality and Individual Differences, 38(4), 809–816. doi:10.1016/j.paid.2004.06.005
- Young, S., Gonzalez, R. A., Wolff, K., Mutch, L., Malet-Lambert, I., & Gudjonsson, G. H. (2017). Transitions and motivations for substance misuse in prison inmates with ADHD and conduct disorder: Validation of a new instrument. Journal of Dual Diagnosis, 13(2), 91–100. doi:10.1080/15504263.2017.1290859
- Young, S., & Sedgwick, O. (2015). Attention deficit hyperactivity disorder and substance misuse: An evaluation of causal hypotheses and treatment considerations. Expert Review Neurotherapeutics, 15(9), 1005–1014. doi:10.1586/14737175.2015.1059756
Appendix 1.
Example of interview guide
1. SUBSTANCE USE INFORMATION
2. TREATMENT GOALS RELATED TO SUBSTANCE USE
3. TREATMENT GOALS RELATED TO OTHER LIFE DOMAINS. SELECTION OF IMPORTANT DOMAINS
Keyword list:
Select domains that you want to prioritize, and rate them on the next page. Remember! Choosing the number of domains should be realistic to work with, considering the next evaluation date and your own opportunities.
__ Self-growth: well-being, self-worth (specify)
__ Health: Physical health, mental health (specify)
__ Economy
__ Network: Public support system/social/friends/family (specify)
__ Carrer/Job
__Substance abuse, coping strategies
__ Inattention
__ Impulsivity
__ Hyperactivity
__ Other? What?
4. TREATMENT GOALS RELATED TO OTHER LIFE DOMAINS.