Abstract
Fibrolipomatous hamartoma is a rare benign slow growing fibrofatty tumor of peripheral nerves of unknown etiology. Clinical presentation may mimic carpal tunnel syndrome when involving the median nerve. We present a case of FLH of the median nerve in a 59-year-old female treated with decompression and collagen nerve wrapping.
Introduction
Lipomas are benign tumors consisting of adipose tissue that may grow anywhere in the body. Fibrolipomatous hamartoma (FLH) is a rare subtype in which adipose and fibrous tissue proliferates into the epineurium and perineurium of peripheral nerves resulting in a benign slow growing mass [Citation1]. FLH is an exceptionally rare tumor with one study citing 88 cases known worldwide [Citation2]. The median nerve is most commonly affected (80%), although occurrences in the radial and ulnar nerves as well as foot and brachial plexus have been reported. The exact etiology is not known. However, 33% of cases are associated with macrodactyly making a congenital cause the most widely accepted. Other theories include abnormal development of the transverse carpal ligament and microtrauma to the nerve with resulting fibrosis [Citation3].
FLH most commonly presents in early adulthood as a painless lump and in rare cases with paresthesia in the affected nerve distribution. When involving the median nerve this can mimic carpal tunnel syndrome (CTS) [Citation4]. The condition is readily diagnosed on magnetic resonance imaging as a pathognomonic ‘coaxial cable’ appearance of thickened nerve fascicles surrounded by fatty and fibrous tissue on axial imaging. Therefore, biopsy is confirmatory rather than diagnostic and given the nature of the tumor, risks injury to the nerve [Citation5]. Owing to the rarity of this tumor, treatment remains controversial ranging from observation of asymptomatic or minimally symptomatic cases to surgical decompression with debulking or excision with nerve grafting [Citation6]. Therefore, the management of FLH of the median nerve remains a challenge for hand surgeons warranting further education. Written informed consent was obtained from the patient in regard to publishing this report and associated figure images.
Case report
A 59-year-old right-handed female with severe grip weakness and paresthesia was referred to our clinic for bilateral CTS refractory to splinting and nonsteroidal anti-inflammatory agents. Her chief complaint was a 2-year history of numbness and tingling of the left wrist, hand and first through fourth fingers. Her symptoms had particularly worsened over the last year and the patient was scheduled for bilateral carpal tunnel releases with another provider but surgical treatment was delayed due to relocating. On our evaluation, she complained only of mild intermittent tingling in her right hand. She experienced constant left sided symptoms along with night awakenings. Examination demonstrated a palpable deep tissue mass just proximal to the carpal tunnel with moderate thenar atrophy, positive carpal compression test, Tinel’s and Phalen’s sign over the median nerve at the wrist on the left and weakly positive Tinel’s on the right. Radiographs demonstrated mild degenerative changes of the carpus and interphalangeal joints (). Due to concern for an underlying mass, the patient was subsequently referred for magnetic resonance imaging (MRI) and electromyography with nerve conduction study (EMG/NCS).
Figure 1. 1 A. Anteroposterior, 1B. oblique and 1 C. lateral radiographs of bilateral hands demonstrating mild degenerative carpal and interphalangeal joint changes with no other osseous or soft tissue abnormalities.

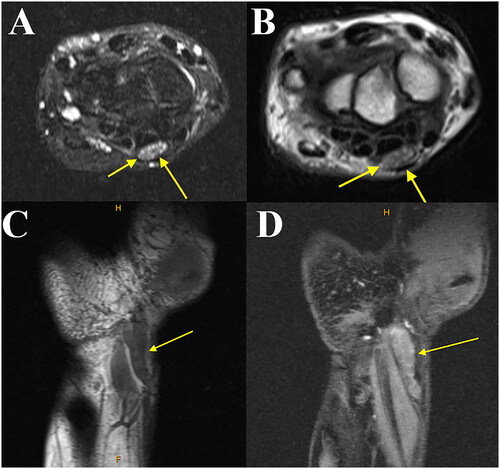
At follow up, the MRI showed an abnormal fusiform enlargement with mixed T1 and T2 signal involving the median nerve just proximal to the carpal tunnel. This mass measured 9.3 mm × 4.3 mm × 30 mm with a coaxial cable-like appearance suggestive of a fibrolipomatous hamartoma of the left median nerve (). There was also dorsal tilt of the lunate with mild dorsal subluxation of the capitate suggestive of dorsal intercalated instability as well as degeneration of the triangular fibrocartilage. EMG/NCS demonstrated moderate right and severe left CTS with motor and sensory components. The patient was offered surgery in the form of left open carpal tunnel release with tenosynovectomy, decompression of the median nerve in the forearm and collagen nerve wrapping.
Figure 2. 2 A. T2 axial, 1B. T1 axial, 1 C. T1 coronal, and 1D. T2 coronal magnetic resonance imaging of the left wrist demonstrating abnormal enlargement with mixed signal involving the median nerve just proximal to the carpal tunnel (yellow arrow). Note the coaxial cable-like appearance on the coronal imaging and honeycombing on the axial consistent with fibrolipomatous hamartoma.
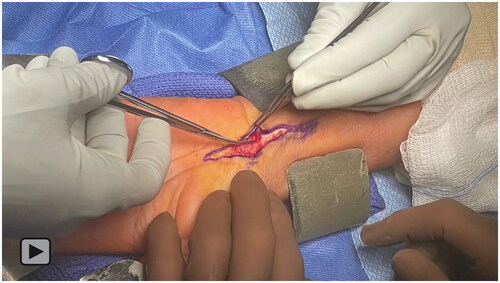
The surgery was completed using an extensile approach to the carpal tunnel (). The carpal tunnel was released and there were no masses within the carpal tunnel. There was extensive tenosynovitis of all flexor tendons within the tunnel (). Tenosynovectomy was performed and later demonstrated benign fibroconnective tissue with focal myxoid changes on pathology. Following release of the carpal tunnel, the incision was extended proximally to identify the mass. Meticulous dissection of the borders of the median nerve with careful hemostasis was used. A gray fusiform mass was identified 5 cm proximal to the level of the carpal tunnel (). After exposure and epineurolysis, this measured 25 mm × 8 mm × 5 mm (). The mass did not extend to the pronator teres and therefore a complete decompression at this level was not deemed necessary. The mass was found to be intimately associated with the fascicles and therefore excision was deemed inappropriate due to potential denervation of the hand (). Biopsy of the mass was also not performed for this reason. The intraoperative findings and pathology were consistent with the preoperative diagnosis of FLH (). Following decompression and neurolysis to prevent postoperative scarring and adhesions, the median nerve was encased with a 7 mm collagen nerve wrap. After copious irrigation, the skin was closed with nylon suture. The patient was placed into a well padded volar splint to protect the incision during postoperative healing.
Figure 3. Intraoperative image of left wrist demonstrating a planned extensile approach (bold line) to the carpal tunnel.
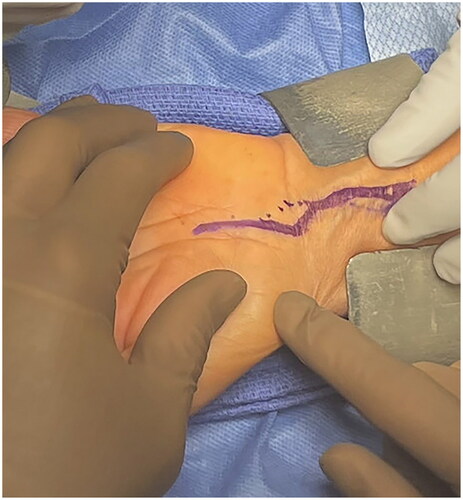
Figure 4. Intraoperative image of the left wrist. Tenosynovectomy is performed demonstrating extensive tenosynovitis (yellow arrow). The flexor tendons underlying the tenosynovium are seen in the bed of the wound (blue arrow). The retractor at the bottom of the image is protecting the median nerve from inadvertent injury.
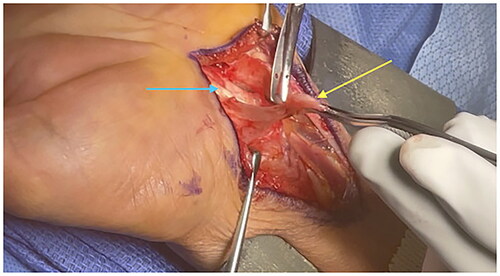
Figure 5. Intraoperative image of the left wrist. The median nerve is seen with an abnormal fusiform mass (yellow arrow). Micro-instrumentation is used to reveal the underlying mass to further assess for possible removal.
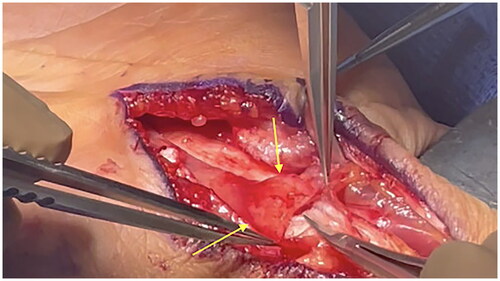
Figure 6. Intraoperative image of the left wrist. The median nerve is positioned on a background with fibrolipomatous hamartoma demonstrated next to the measuring utensil. Neurolysis of the epineurium has been performed and the mass is seen to be intimately associated with the underlying fascicles preventing excision.
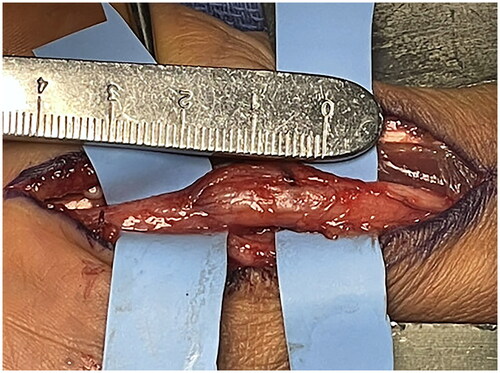
Figure 7. Intraoperative image of the left wrist. The median nerve is wrapped with a collagen nerve wrap to prevent adhesions and scarring of the nerve postoperatively.

Video 1. Intraoperative video of the left wrist demonstrating an extensile approach to the carpal tunnel for decompression and collagen nerve wrapping of a fibrolipomatous hamartoma of the median nerve.
On postoperative day 3, the patient was placed into a custom molded removable wrist orthosis and offered occupational therapy which she attended initially but was then noncompliant. The patient reported continued although improved postoperative numbness in the median nerve distribution. She continued home exercises and returned to work 2 weeks after surgery with 10 lb lifting restrictions. Sutures were removed at this time. The patient experienced pillar pain which improved 4 weeks after surgery when she began attending occupational therapy. Grip strength improved to 4+/5 with full range of motion. The patient returned to full duty as a cashier at 8 weeks. At final follow up at 6 months, the patient had minimal residual numbness in the distal thumb, index, middle and radial half of the ring finger. She had a mildly hypertrophic scar that improved with silicone gel sheets and daily scar massages.
Discussion
FLH is an exceptionally rare benign overgrowth of fibrous and adipose tissue into epineural and perineural tissue of peripheral nerves that can present a unique and challenging situation for both the patient and surgeon [Citation2]. While the etiology is unclear, FLH has been theorized to be congenital in origin with macrodactyly, abnormal flexor retinaculum or transverse carpal ligament development. Other described etiologies include microtrauma and chronic inflammation of the nerve [Citation3, Citation6]. The median nerve near the carpal tunnel is the most common site for FLH along with brachial plexus, radial, ulnar, posterior tibial and fibular nerves as less often reported sites [Citation3]. The presentation of FLH of the median nerve typically overlaps with that of CTS including decreased sensation, paresthesia and motor deficits in the median nerve distribution. Many patients may neglect seeking medical attention prior to having symptoms of compressive median neuropathy due to the slow-growing nature of FLH [Citation6]. Physical examination often demonstrates a nontender fusiform mass in the volar aspect of the wrist and differential diagnoses should include traumatic neuromas, ganglion cysts, lipomas and vascular malformations prior to further workup [Citation2]. MRI remains the gold standard for definitive diagnosis of FLH [Citation5]. The pathognomonic ‘coaxial cable’ appearance of the enlarged median nerve on axial MRI views yield a positive predictive value of 94% in diagnosing lipomatous median nerve lesions, therefore rendering biopsy obsolete [Citation1]. Specifically in our case, the palpable mass proximal to the carpal tunnel detected on examination and negative pathology on plain radiographs prompted ordering of MRI to discern the diagnosis of FLH. It should be noted that in this patient, the mass was proximal to the carpal tunnel and with most modern techniques would go undetected with a standard carpal tunnel release.
Management of FLH, which mostly depends on the clinical severity of compressive median neuropathy, remains controversial and ranges from carpal tunnel decompression to radical excision with or without nerve grafting [Citation1, Citation5]. Conservative surgical treatments including carpal tunnel decompression have yielded successful outcomes with complete resolution of symptoms [Citation1, Citation2]. Decompression and release of FLH fascial elements may also lead to reduction in mass size and improve opponens pollicis strength [Citation6]. Although radical surgical excision with nerve graft has historically demonstrated poor outcomes, Prabhu et al. reports successful outcomes and minimal complications in all 6 of their patients treated with excision, microdissection and sural nerve graft reconstruction [Citation3]. Due to the increased risk of median nerve damage and donor site morbidity, radical excision with or without nerve autograft should be reserved for symptomatic patients with large masses who have failed previous decompression [Citation7]. In our case, a decision was made to take a conservative approach and perform an open carpal tunnel release, tenosynovectomy and median nerve decompression with application of a collagen nerve wrap. This biodegradable type 1 collagen material acts as an interface between nerve and surrounding tissues to prevent postoperative adhesions and scarring to the median nerve [Citation8]. To our knowledge, there is one previous case of nerve wrapping to supplement median nerve FLH decompression. Elbayer et al. describes a case of median nerve decompression for FLH in which the patient subsequently underwent an additional surgery 5 months after for median nerve coverage with an acellular dermal substitute and pronator quadratus flap due to persistent hyperesthesia. In contrast to our case, flexor tendon tenosynovectomy was not reported in this case. Similar to our case, this patient reported 95% resolution of paresthesia and complete resolution of symptoms at the 6 month and 2 year follow-up visits, respectively [Citation9]. The application of nerve wraps should be considered to prevent postoperative fibrous healing following decompression or radical excision of FLH.
Disclosure statement
The authors report there are no competing interests to declare.
References
- Ranjan R, Kumar R, Jeyaraman M, et al. Fibrolipomatous hamartoma (FLH) of median nerve: a rare case report and review. Indian J Orthop. 2020;55(Suppl 1):267–272. Published 2020 Jun 1. doi:10.1007/s43465-020-00149-9.
- Al-Jabri T, Garg S, Mani GV. Lipofibromatous hamartoma of the median nerve. J Orthop Surg Res. 2010;5(1):71. Published 2010 Sep 28. doi:10.1186/1749-799X-5-71.
- Prabhu A, Anil R, Kumar N. Fibrolipomatous hamartoma of the median nerve: an outcome of surgical management in six consecutive cases. Niger J Surg. 2020;26(2):153–158. doi:10.4103/njs.NJS_16_20.
- Pallewatte AS, Samarasinghe EC. Fibrolipomatous hamartoma arising from the median nerve-a case report. Indian J Radiol Imaging. 2021;31(2):472–475. doi:10.1055/s-0041-1734332.
- Rai V, Sabhikhi GS, Sircar P, et al. Fibrolipomatous hamartoma of median Nerve - A diagnostic challenge. J Orthop Case Rep. 2021;11(11):69–73. doi:10.13107/jocr.2021.v11.i11.2520.
- Senger JL, Classen D, Bruce G, et al. Fibrolipomatous hamartoma of the median nerve: a cause of acute bilateral carpal tunnel syndrome in a three-year-old child: a case report and comprehensive literature review. Plast Surg (Oakv). 2014;22(3):201–206. doi:10.1177/229255031402200307.
- Paletta FX, Senay LC.Jr. Lipofibromatous hamartoma of median nerve and ulnar nerve: surgical treatment. Plast Reconstr Surg. 1981;68(6):915–921. doi:10.1097/00006534-198112000-00012.
- Kokkalis ZT, Mavrogenis AF, Ballas EG, et al. Collagen nerve wrap for median nerve scarring. Orthopedics. 2015;38(2):117–121. doi:10.3928/01477447-20150204-04.
- Elbayer AM, Alharami S, Elhessy AH. Lipofibromatous hamartoma of the median nerve: a case report. Cureus. 2023;15(1):e33516. Published 2023 Jan 8. doi:10.7759/cureus.33516.

