ABSTRACT
Internationally, the use of simulation-learning environments in nursing education has escalated over the last number of years. Simulations have been recognized as providing clinical opportunities for student nurses to gain experience in a safe and controlled learning environment. A module specifically preparing fourth year children’s and general nursing students for internship was developed. Preparation work for these simulation sessions included a video for the students to watch which demonstrated evidence-based care using sample simulations. This research aims to evaluate two simulation scenarios, using low-fidelity and high-fidelity mannequins for children’s nursing students as part of a nursing module preparing them for internship practice placement. This mixed-methods evaluation survey of students was conducted in one School of Nursing in a Higher Education Institute in Ireland in the academic year 2021–2022. A simulated learning package was created using a partnership approach with members from the Higher Education Institute and the clinical learning site and piloted with 39 students. This was evaluated using an anonymous, online questionnaire with 17 student responses. An ethical exemption was granted for this evaluation. All students reported the use of the simulations, including the pre-simulation video as beneficial to enhance their learning and to prepare them for internship. The use of low-fidelity and high-fidelity mannequins enhanced their learning process. Students recommended implementing further simulations throughout their programme to enhance their learning experiences. The findings of this evaluation can provide guidance to aid future development of interactive simulations in preparing students for practice placements. Both low fidelity and high fidelity have their places in simulation and education, depending on the scenario and associated learning outcomes. Collaboration between academia and clinical practice is crucial, to bridge the theory-practice gap and demonstrate a positive relationship between staff in both settings.
Introduction
Internationally, the use of simulation-learning environments in nursing education has escalated over the last number of years (D’Souza et al., Citation2017). Simulations have been recognized as improving patient safety, providing clinical opportunities for student nurses to gain experience in a safe and controlled learning environment (Aebersold, Citation2018; Lamé & Dixon-Woods, Citation2020) and improving learning outcomes (Haddeland et al., Citation2021). This paper will discuss the experiences of clinical educators and academic staff from a Higher Education Institute (HEI) and a partner hospital site, delivering both high-fidelity (HFS) and low-fidelity simulations (LFS) to students as part of a module preparing fourth year children’s and general nursing students for internship. Preparation work for these simulation sessions included a video for the students to watch which demonstrated evidence-based care using sample simulations, which have been reported as beneficial in the literature (Clerkin et al., Citation2022). A key emphasis was also placed on the importance of pre-brief and debrief sessions as part of the learning process which are recognized as key processes within simulation-based learning (Kolbe et al., Citation2015; Levett-Jones & Lapkin, Citation2011).
Clinical simulation in nursing education
Over the last few decades, nursing education has undergone major educational reforms across the globe. In Ireland, the apprenticeship model has been replaced by graduate and undergraduate nursing programmes taught in HEIs with practice placements being facilitated by clinical partners. These changes to nursing education allowed the nursing profession to become both an academic discipline and a practice profession. However, an important part of nursing education is that educational providers need to ensure nursing students are work ready upon graduation and that they practice nursing safely and competently throughout their career (Nursing and Midwifery Board of Ireland [NMBI], 2016). Liaw et al. (Citation2015) highlight the importance of a strong collaborative partnership between academic and service institutions as fundamental in the transition from nursing students to professional practitioners.
As part of their nursing training, clinical placements provide authentic and invaluable learning opportunities for nursing students to get hands-on experience in real-life situations. However, due to a variety of reasons, such as limited availability of clinical placements and higher students’ numbers enrolled in nursing programmes, a need to supplement increasingly limited practicum experiences, an increased workload, and staffing issues of ward nurses as well as patient safety issues, and ethical concerns (Roberts et al., Citation2019; Taylor et al., Citation2017; Ulenaers et al., Citation2021), clinical simulation has taken up an important role in creating optimal learning environments. Clinical simulation activities can incorporate scenarios of real-life events, the usage of high- and low-fidelity manikins or real-life actors as patients, role play, skills stations, and computer-based critical thinking games (Jeffries, Citation2005; Lateef, Citation2010). Clinical simulation allows the replacing and amplifying of real-life events to achieve educational goal through guided experiences and experimental learning in a safe way without placing patients or institutional resources at risk. Specific learning outcomes, learning needs and educational levels should determinate what simulation methods are best suited/adapted for clinical simulation.
In addition to being part of the educational changes, clinical simulation was introduced as an innovative and effective teaching strategy since nursing is a performance-based profession. Nowadays, more and more HEIs utilize clinical simulation to replace required clinical practice hours (Roberts et al., Citation2019). Clinical simulation, a central pedagogical educational approach, provides nursing students with cognitive learning and an opportunity to integrate theoretical knowledge into practical knowledge and to practice their clinical and decision-making skills. Additionally, students are able to practice psychomotor skills and are able to develop confidence, self-efficacy, and critical thinking skills (Cant & Cooper, Citation2017).
High fidelity mannequins, capable of realistic physiological responses to nursing students’ actions, are useful for complex patient care and emergency team scenarios (Morton et al., Citation2019). While low-fidelity mannequins and partial task simulators (e.g., hands or arms) are mainly used to acquire relevant psychomotor skills, such as CPR skills or intravenous catheterization (Koukourikos et al., Citation2021; Watson et al., Citation2021). Standardized patients, actors, or volunteers playing the role of patients or family members behaving in a particular way, are often used for role-play scenarios when realist clinical interaction is required such as in communication or scribed case scenarios (Koukourikos et al., Citation2021).
High fidelity simulation
The use of HFS has become embedded in clinical teaching over the past few years (Nash & Harvey, Citation2017). It offers staff and students the opportunity to improve clinical competencies both technical and non-technical in a safe realistic environment (Morton et al., Citation2019). These skills which are deemed essential during emergency management of critically ill children require high levels of competency. HFS provides an environment with a high level of accuracy and clinical reality (Watson et al., Citation2021). It allows participants the opportunity to put skills attained in classrooms into practice using a team approach, thus aiding the translation of knowledge from theory to practice (Weiler et al., Citation2018).
By using HFS, students can enhance non-technical skills required as part of multi-disciplinary team management of medical emergencies (Brohard et al., Citation2021). These include critical thinking, problem solving, and high-level communication skills (Hallin et al., Citation2016). By allowing students to initiate interventions, the facilitator can trigger realistic clinical responses to these interventions, allowing students to receive immediate feedback on their actions. HFS with good reflective feedback assists the transition from students to qualified nurses by encouraging independency and to assume the roles of responsibility (Watson et al., Citation2021). Morton et al. (Citation2019) states that repeated HFS increases confidence levels and improve resuscitation skills.
Low fidelity simulation
Nursing requires cognitive and psychomotor skills to become proficient in their profession (Morgaonkar et al., Citation2017). LFS can assist in delivering this practical education where nurses have an opportunity to master teamwork and communication skills (Pollard & Wild, Citation2014). Simulation bridges the gap between theory and practice gap giving the nurse the opportunity to practice and master skills prior to real clinical situations (Ummu, 2019). In this scenario where pre- and post-operative care was the lesson, LFS facilitated the nurse to practice nursing care, bringing the journey of the surgical patient to life. LFS has a very valuable place in education as it allows the student to learn at their own pace facilitating practice in a safe environment with no risk to the patient (Garner et al., Citation2018). Massoth et al. (Citation2019) found that confidence, skills, and knowledge increased equally in LFS, which differed in that the students that used HFS were overconfident with no increase in knowledge and skill. Regarding retention of knowledge, Angelina et al. (Citation2021) established that skills were highly retained after 6 months post a LFS on an obstetrics scenario.
From a cost-effective perspective LFS is preferable (Meska et al., Citation2016). Mannikins are less expensive than those for high fidelity simulation. LFS requires less facilitators also as there is less technology to contend with (Tjoflåt et al., Citation2017). The facilitator sets the scene and can be accessible if support is required throughout the simulation. However, debriefing requires the same number of facilitators as HFS. In addition to the cost-effectiveness element manikins are easily transportable to satellite centers for training, making it more accessible for students to practice in hospital or university campus (Hart et al., Citation2017). LFS is suited as a teaching strategy for specific non-technical nursing skills whilst delivering knowledge at a controlled pace in real time, and thus was selected for one of the simulation scenarios.
Aim
This research aimed to evaluate two simulation scenarios, using low-fidelity and high-fidelity mannequins for children’s undergraduate nursing students as part of a children’s nursing module preparing them for internship practice placement.
The objectives were to understand student engagement and perceived learning with the simulations.
Methodology
Methods
This mixed-methods evaluation survey of students was conducted in one School of Nursing in a HEI in Ireland in the academic year 2021–2022. A simulated learning package was created using a partnership approach with members from the Higher Education Institute and the clinical learning site. Pre-learning work for these simulations included learning resources and a video created by the staff in the HEI and the clinical site. All 4th year undergraduate nursing students on a BSc Children’s & General Nursing programme were potential participants in this study (n = 39). An ethical exemption was granted for this evaluation, as within the HEI specific educational practices, such as this evaluation, are situated in the category of ethical exemptions. This was evaluated using an anonymous, online questionnaire with 17 student responses. Questionnaires were utilized as the evaluation tool and were distributed using an online platform after the simulation sessions. The anonymous questionnaire was designed to elicit information on the participants’ views of the learning support package they received prior to the simulation sessions and were anonymously coded. The participants’ overall experience of the teaching session in relation to decision-making skills, knowledge gained, confidence building, and whether it was a valuable experience in comparison to other methods including lectures and role-plays were evaluated.
These students had not had simulations incorporated earlier into their training program due to resource constraints and restrictions within the curriculum planning. Going forward, simulations will now be incorporated earlier into this nursing program. For the purposes of these simulations, both HFS and LFS were utilized as teaching methods for differing scenarios on different days. HFS was used for a scenario on a deteriorating 6-month-old baby admitted to the ward with bronchiolitis and having apneic episodes. Vital signs were provided for the baby on handover from the emergency department, and half an hour later the baby deteriorated quickly with additional vital signs provided. LFS was utilized for a pre- and post-operative simulation scenario of a 4-week-old infant undergoing a pyloromyotomy. The two infants were representative of different ethnic origins to represent EDI within the clinical setting. The students were provided with a scenario of receiving handover of the infant after a night shift, with an anxious mother in attendance. The students had to prepare the infant for theater and complete the post-operative journey afterward. There was a maximum of 10 students in each simulation lab, with the group split in two. One group of students went first, carrying out the simulation, and the second group observed the simulation. The second group then repeated the same simulation after a debriefing session, reflecting on what occurred in the first simulation. As this was the students first time participating in simulations, the facilitators opted to debrief after the first simulation, before the next simulation occurred to maximize learning for the students.
The facilitators were registered nurses, with two facilitators having specific further education completed in simulation-based training and education. The facilitators comprised of staff in the HEI alongside those from the clinical partner sites. The students were asked for confidentiality within the sessions, to protect the integrity of the scenarios for the next group. There was limited time between group transitions, which also minimized the risk of specific details being shared. A limitation to this simulations setting was repeating the same simulation. This was due to time and resource constraints from the facilitator’s perspectives. When planning future simulations, the facilitators aim to create a variety of simulations and use different simulations for each group.
Participants were informed via the questionnaire that participation was voluntary, and the participants had to consent to participate before proceeding with the questionnaire. The questionnaire included five statements, with an additional six in an open-ended comments section. Participants were asked to indicate their level of agreement on a 5-point Likert scale ranging from Strongly Agree to Strongly Disagree. In total, 17 questionnaires were returned, representing a 43.5% of the total number distributed. Although the authors recognize this as a limitation that over half of the students did not participate in this evaluation. Findings from the closed Likert-style questions are reported first, followed by a discussion with the responses to the questions posed in the open responses section of the questionnaire.
Findings
Participants were asked to indicate their views in relation to the pre-learning materials provided for the medical simulation and the overall usefulness of the medical simulation. The medical simulation referred to the care of a child with a medical condition, e.g., bronchiolitis, as opposed to those requiring a surgical intervention. The question asked and the responses given in relation to this question are seen in .
Table 1. Overall views relating to the medical simulation.
Participants were asked to indicate their views in relation to the pre-learning materials provided for the surgical simulation and the overall usefulness of the surgical simulation ().
Table 2. Overall views relating to the surgical simulation.
Participants were asked to indicate their views in relation to the sample simulation video that was created with members from the Higher Education Institute and the clinical learning site (). The students reported on the beneficial use of the pre-learning materials in preparation for the simulations. One student reported feeling an additional surgical scenario learning video would be useful as they did not have experience of working on a surgical ward.
Table 3. Overall views relating to the simulation sample video.
Open-ended questions
Participants were invited to add comments about six areas, including what they found useful, recommendations to improve future simulations and any additional comments.
Participants reported benefits to the simulations as a chance to practice in a clinical setting, being helpful for clinical placement, encouraging critical thinking, whilst improving communication among peers and being an opportunity to learn:
To see how much I actually knew/didn’t know and what I would do in that situation. It really makes you think and it’s a great way to learn and remember the information.
Many positives were associated with both the HFS and LFS including the applicability to practice, provide opportunities for critical thinking and role-playing different roles within the scenario:
Being in the lab doing the simulation in person, role playing the different roles in the scenario, getting used to using all the documentation in person that we will use on placement.
It makes you consider what actually needs to be done in that situation and it makes you realize how much you didn’t know. Very practical and a great way to learn.
Students enjoyed having two groups within the one simulation session, as it provided them with additional learning opportunities and a chance to learn from their mistakes, with one student reporting within the HFS feeling at ease that they:
weren’t expected to perform the simulation perfectly - The structure of having one group carry out the role play first, and then a second group to do it after talking through the scenario - I felt we were wanted to contribute to the session, and I enjoyed talking through everything and giving our opinions.
With other students reporting gaining support and help from their peers, whilst practicing in a hands-on environment:
It was great to actually have to take part and not watch/listen to someone else carrying out an example etc, I liked when we were stopped during the simulation and advice/feedback was given, it was great that the environment was made feel realistic etc. I found the simulation to be a brilliant learning experience, much more beneficial than listening to a power point presentation on how to do something.
Similar findings were expressed with the LFS:
I learned a lot about being responsible for a surgical patient. I found it very applicable to practice. I learned from my own and other’s mistakes.
Conversations were open so we could ask questions if we needed to … We could draw on what the other group did to enhance our learning.
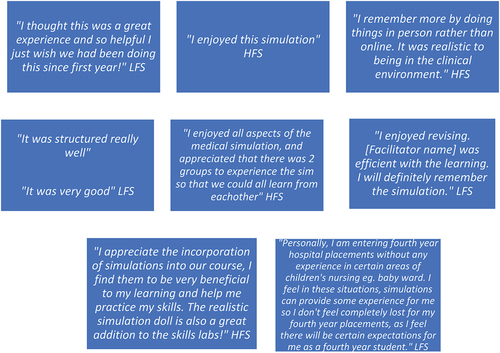
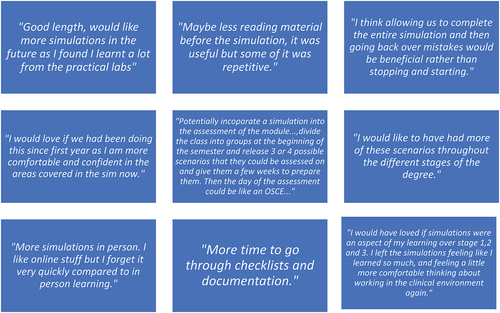
No students reported any negative feedback on the simulations. There was an overwhelming consensus that all students wanted more simulations, both HFS and LFS, throughout their course with one student stating “more sims would be more beneficial like multi organ failure, sepsis, respiratory arrest, these sims really helped with my confidence dealing with some aspects of nursing care but more labs would enhance my confidence and learning” and another student reported wanting “more simulations in the future as I found I learnt a lot from the practical labs”. Students reported not wanting to change anything, other than wanting to explore additional scenarios in addition to the two that were carried out. Other words used by the participants to describe the simulations are highlighted in .
Students were asked for suggestions to improve future simulations and some of these are highlighted in . The overall feedback was that students wanted more simulations across all stages of their nursing programme.
Discussion
All students reported the use of the simulations, including the pre-simulation video as beneficial to enhance their learning and to prepare them for internship. During internship placement, the students are expected to work within their hospital as a member of the nursing team and take responsibility for a patient caseload (Ahanchian et al., Citation2017). The transition process from student nurse to qualified nurse can be a complex experience (Bartley & Huntley-Moore, Citation2021) and stressful for many students (Edwards et al., Citation2015; Van Rooyen et al., Citation2019).
These two simulation sessions gave students the opportunity to become aware of various team roles and their responsibilities within clinical scenarios. Several students commented positively on this in the evaluation quoting they found “role playing the different roles in the scenario” as useful. The overall feedback from the students was positive, with students requesting “more simulations like this.” Over half of the students reported wanting to incorporate simulations into their assessments, with students indicating it was a positive way to demonstrate their clinical skills and critical thinking, in comparison to written assignments or exams.
The students underwent a pre-briefing and debriefing session before and after each simulation session, with students reporting these sessions were helpful in integrating the theory and practice aspects of the simulation, whilst also providing an opportunity to reflect on their experiences. Debriefing is reported as an essential component of simulation which was evident in this study (INACSL Standards Committee et al. Citation2021; Şahin & Başak, Citation2021; Schober et al., Citation2019). In addition, reflection is a critical component to the simulation debriefing sessions (Krogh et al., Citation2016). Students were encouraged to reflect on the positive experiences of their individual and team performance post simulation and on aspects that could be improved on for future practices. Teaching and clinical staff who conducted the debriefing sessions with the students found it a positive exercise. However, the introduction of a reflective modelfor example, Gibbs (Citation1988) could be implemented for future debriefing sessions, which would provide more structured, deeper reflection, and discussion.
Johnson (Citation2019) suggests that in HFS, the observers can achieve better learning outcomes than participants, which was observed during the study conducted. In an era of staff shortages and increased clinical acuity, the transition from student to staff nurse can be highly stressful (Watson et al., Citation2021). The use of HFS allowed the team to recreate highly stressful clinical situations, thus allowing students to assume pivotal team roles to manage these complex situations thus improving critical thinking and situational awareness (Weiler et al., Citation2018). The team consisted of 4–5 nursing students, who each had a different role to play including a newly qualified nurse, an internship student nurse, and a parent. Each student was briefed by a facilitator regarding their role before the simulation commenced. HFS offers a higher level of reality by incorporating a team approach into sims so that all members of the team must be cognizant of the need for good communication and teamwork. Weiler et al. (Citation2018) also state that the use of HFS can elicit “real life” psychological responses from students, thereby adding to the sense of reality.
Prior to both simulations, the students had pre-learning material to complete. This pre-learning material included watching the simulation video created by the clinical and HEI staff, reading relevant articles, and resource materials. The students were strongly encouraged to complete this pre-learning material. However, some students admitted they did not complete this due to personal circumstances including lack of time and family commitments. These students continued to participate in the simulations. Immediately prior to the LFS the students had a briefing of the capabilities of the low fidelity mannikin including the limitations, which was important to prepare the student for the simulation (Tjoflåt et al., Citation2017). LFS encourages critical thinking as the student is required to ask questions without being prompted by an alarming monitor in high-fidelity simulation (Tjoflåt et al., Citation2017). The HFS had an added level of complexity and included additional features including crying, coughing, changing in respiratory rate and rhythm.
Students in this study had never experienced simulation-based teaching before. Although the students expressed, they were nervous and anxious at the beginning of the simulation sessions, the overall feedback was these simulations were very beneficial for students and they wish to have simulations as a form of teaching methods across the years “I would like to have had a more of these scenarios throughout the different stages of the degree”.
These findings are consistent with the literature on LFS, with Scott and Gartner (Citation2019) reporting that LFS provides proven effective learning, Pollard and Wild (Citation2014) highlighting that LFS has a place in education when teaching non-technical skills, for example communication and team dynamics and Findik et al. (Citation2019) finding LFS is a very beneficial learning method for nursing students. The students reported similar findings with the LFS.
Benefits to using LFS include being very accessible and inexpensive (Meska et al., Citation2016). It is easy to take the low fidelity mannikin to different skills sites reducing the risk of damaging the mannikin (Sarmah et al., Citation2017). A facilitator equipped with the knowledge of scenarios that can occur in real life can make the learning experience interesting which in turn creates learning for the student. A little action or drama can add to the teaching and learning experience too and may even add some humor (Arveklev et al., Citation2015). Setting the scene is also very important with LFS (Nestel et al., Citation2019). Within this LFS the facilitator conveyed gentleness and care toward the mannikin to help promote a real-life experience. This LFS proved to be a beneficial exercise for the pre-operative and post-operative scenario as there was less distraction from the high-tech element of high fidelity and focused on the care of preparing an infant for surgery using the pre-operative checklist finding the identification band was incorrect or the blood results were not all present as per guidelines for a child undergoing a pyloromyotomy. This facilitated the thought process and action in how to rectify those real situations. LFS also involves creativity as Hart et al. (Citation2017) demonstrates and acting skills from the facilitator and students makes the learning experience more real, leading to deeper learning. Introducing the unexpected by stepping in and demonstrating the infant in pain and the student being the “insistent” recovery nurse that wants to move the patient to the ward presented a learning opportunity and a time to explore solutions while again advocating for the infant.
In the LFS, the infant had an NG, and it was interesting that some students did not remark on this. This presented another learning opportunity, and it was evident that some students were not familiar with the care of the child with pyloric stenosis. The students were taught now of the importance of following this up when accepting care from the registered nurse working in recovery. Reminding the learner about the importance of asking questions and knowing what your responsibilities are when accepting patient care at any stage of your professional career. This taught the students the importance of working within their Scope of Practice NMBI (Citation2015) and following The Code of Professional Conduct and Ethics Professional Guidance NMBI (Citation2021) and most importantly advocating for their patient which is always paramount in their practice.
Recommendations/Implications for practice
Following these simulations, the authors discovered HFS and LFS both have a place in simulation, depending on the clinical scenarios to be explored.
The findings from this study present a platform to provide a basis for more simulations across an undergraduate nursing programme.
Students reported learning by observing their peers participating in simulations. They reflected on the importance of learning as observers, rather than actively participating in the simulation. This is crucial to the development of further simulations and the unique learning obtained from the observers. The use of a simulation video created in collaboration between the HEI and clinical site was an additional benefit for the students in their pre-simulation phase. The use of this video showed best practice and allowed the students to learn within a safe, controlled environment.
Conclusion
These simulation experiences were very rewarding for the students and beneficial for their learning. The simulation experiences allowed students to develop their critical thinking skills, integrate theory and practice, and critically reflect on their performance both individually and as part of a team, whilst in a safe, supportive environment. The use of low-fidelity and high-fidelity mannequins enhanced their learning process, depending on the scenario. Students recommended implementing further simulations throughout their programme to enhance their learning experiences. The findings of this evaluation can provide some guidance to aid future development of interactive simulations in preparing students for practice placements.
Author contributions
Katie Hill created the idea for this manuscript and completed data collection. All authors contributed to the data analysis and write-up phase of this manuscript. All authors reviewed the final draft before submission and contributed to the revisions.
Ethics
An ethical exemption was granted for this evaluation.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Aebersold, M. (2018). Simulation-based learning: No longer a novelty in undergraduate education. OJIN: The Online Journal of Issues in Nursing, 23(2). https://doi.org/10.3912/OJIN.Vol23No02PPT39
- Ahanchian, M., Sharafi, S., Vafaee, M., & Hajiabadi, F. (2017). Evaluate the effectiveness of internship program in nursing student using Kirkpatrick’s model. Research in Medical Education, 9(1), 17–19. https://doi.org/10.18869/acadpub.rme.9.1.17
- Angelina, J. A., Stephen, K. M., & Ipyana, M. (2021). The impact of low fidelity simulation on nurse competence in active management of third stage of labor: An intervention study in primary health care settings in Tanzania. Clinical Simulation in Nursing, 56, 10–21. https://doi.org/10.1016/j.ecns.2021.03.009
- Arveklev, S. H., Wigert, H., Berg, L., Burton, B., & Lepp, M. (2015). The use and application of drama in nursing education—An integrative review of the literature. Nurse Education Today, 35(7), e12–e17. https://doi.org/10.1016/j.nedt.2015.02.025
- Bartley, N., & Huntley-Moore, S. (2021). Supporting the transition from nursing student to newly qualified children’s nurse. Nursing Children and Young People, 34(3), 18–25. https://doi.org/10.7748/ncyp.2021.e1372
- Brohard, C., Moreland, E., Shammas, S., & Tonsul, R. (2021). From development to implementation: The effectiveness of a high-fidelity simulation for advance care planning for undergraduate nursing students. Journal of Hospice and Palliative Nursing, 23(6), 504–511. https://doi.org/10.1097/NJH.0000000000000798
- Cant, R. P., & Cooper, S. J. (2017). Use of simulation-based learning in undergraduate nurse education: An umbrella systematic review. Nurse Education Today, 49, 63–71. https://doi.org/10.1016/j.nedt.2016.11.015
- Clerkin, R., Patton, S., Moore, Z., Nugent, L., Avsar, P., & O’Connor, T. (2022). What is the impact of video as a teaching method on achieving psychomotor skills in nursing? A systematic review and meta-analysis. Nurse Education Today, 111, 105280. https://doi.org/10.1016/j.nedt.2022.105280
- D’Souza, M. S., Venkatesaperumal, R., Chavez, F. S., Parahoo, K., & Jacob, D. (2017). Effectiveness of simulation among undergraduate students in the critical care nursing. International Archives of Nursing and Health Care, 3(4). https://doi.org/10.23937/2469-5823/1510084
- Edwards, D., Hawker, C., Carrier, J., & Rees, C. (2015). A systematic review of the effectiveness of strategies and interventions to improve the transition from student to newly qualified nurse. International Journal of Nursing Studies, 52(7), 1254–1268. https://doi.org/10.1016/j.ijnurstu.2015.03.007
- Findik, U. Y., Yesilyurt, D. S., & Makal, E. (2019). Determining student nurses' opinions on the low-fidelity simulation method. Nursing Practice Today, 6(2), 71–76.
- Garner, S. L., Prater, L. S., Raj, L., Leena, G. V., & Anitha, A. J. (2018). Effectiveness of peripheral intravenous skill continuing education using low-fidelity simulation among nurses in India. The Journal of Continuing Education in Nursing, 49(6), 255–261. https://doi.org/10.3928/00220124-20180517-05
- Gibbs, G. (1988). Learning by doing a guide to teaching and learning methods. EMIJ Oxford Brookes University.
- Haddeland, K., Slettebø, Å., & Fossum, M. (2021). Enablers of the successful implementation of simulation exercises: A qualitative study among nurse teachers in undergraduate nursing education. BMC Nursing, 20(234). https://doi.org/10.1186/s12912-021-00756-3
- Hallin, K., Bäckström, B., Häggström, M., & Kristiansen, L. (2016). High-fidelity simulation: Assessment of student nurses’ team achievements of clinical judgment. Nurse Education in Practice, 19, 12–18. https://doi.org/10.1016/j.nepr.2016.03.010
- Hart, D., Nelson, J., Moore, J., Gross, E., Oni, A., & Miner, J. (2017). Shoulder dystocia delivery by emergency medicine residents: A high‐fidelity versus a novel low‐fidelity simulation model—A pilot study. AEM Education and Training, 1(4), 357–362. https://doi.org/10.1002/aet2.10054
- INACSL Standards Committee, Decker, S., Alinier, G., Crawford, S. B., Gordon, R. M., & Wilson, C. (2021). Healthcare simulation standards of best practice the debriefing process. Clinical Simulation in Nursing, 58, 27–32. https://doi.org/10.1016/j.ecns.2021.08.011
- Jeffries, P. (2005). A framework for designing, implementing, and evaluate simulations used as teaching strategies in nursing. Nursing Education Perspectives, 26(2), 96–103.
- Johnson, B. K. (2019). Simulation observers learn the same as participants: The evidence. Clinical Simulation in Nursing, 33, 26–34. https://doi.org/10.1016/j.ecns.2019.04.006
- Kolbe, M., Grande, B., & Spahn, D. R. (2015). Briefing and debriefing during simulation-based training and beyond: Content, structure, attitude and setting. Best Practice & Research Clinical Anaesthesiology, 29(1), 87–96. https://doi.org/10.1016/j.bpa.2015.01.002
- Koukourikos, K., Tsaloglidou, A., Kourkouta, L., Papathanasiou, I. V., Iliadis, C., Fratzana, A., & Panagiotou A. (2021). Simulation in clinical nursing education. Acta Informatica Medica, 29(1), 15–20. https://doi.org/10.5455/aim.2021.29.15-20
- Krogh, K., Bearman, M., & Nestel, D. (2016). “Thinking on your feet” – A qualitative study of debriefing practice. Advances in Simulation, 1(12). https://doi.org/10.1186/s41077-016-0011-4
- Lamé, G., & Dixon-Woods, M. (2020). Using clinical simulation to study how to improve quality and safety in healthcare. BMJ Simulation and Technology Enhanced Learning, 6(2), 87–94. https://doi.org/10.1136/bmjstel-2018-000370
- Lateef, F. (2010). Simulation-based learning: Just like the real thing. Journal of Emergencies, Trauma, and Shock, 3(4), 348–352. https://doi.org/10.4103/0974-2700.70743
- Levett-Jones, T., & Lapkin, S. (2011). The effectiveness of debriefing in simulation-based learning for health professionals: A systematic review. JBI Library of Systematic Reviews, 9(64), 1–16. https://doi.org/10.11124/jbisrir-2011-317
- Liaw, S. Y., Palham, S., Chan, S. W. C., Wong, L. F., & Lim, F. P. (2015). Using simulation learning through academic-practice partnership to promote transition to clinical practice: A qualitative evaluation. Journal of Advanced Nursing, 71(5), 1044–1054. https://doi.org/10.1111/jan.12585
- Massoth, C., Röder, H., Ohlenburg, H., Hessler, M., Zarbock, A., Pöpping, D. M., & Wenk, M. (2019). High-fidelity is not superior to low-fidelity simulation but leads to overconfidence in medical students. BMC Medical Education, 19(1), 1–8. https://doi.org/10.1186/s12909-019-1464-7
- Meska, M. H. G., Mazzo, A., Jorge, B. M., Souza-Junior, V. D. D., Negri, E. C., & Chayamiti, E. M. P. C. (2016). Urinary retention: Implications of low-fidelity simulation training on the self-confidence of nurses. Revista da Escola de Enfermagem da USP, 50(5), 831–837. https://doi.org/10.1590/s0080-623420160000600017
- Morgaonkar, V. A., Shah, B. V., Nimbalkar, S. M., Phatak, A. G., Patel, D. V., & Nimbalkar, A. S. (2017). Educational intervention to improve intravenous cannulation skills in paediatric nurses using low-fidelity simulation: Indian experience. BMJ Paediatrics Open, 1(1), e000148. https://doi.org/10.1136/bmjpo-2017-000148
- Morton, S. B., Powers, K., Jordan, K., & Hatley, A. (2019). The effect of high-fidelity simulation on medical-surgical nurses’ mock code performance and self-confidence. Medsurg Nursing, 28(3), 177–182.
- Nash, R., & Harvey, T. (2017). Student nurse perceptions regarding learning transfer following high-fidelity simulation. Clinical Simulation in Nursing, 13(10), 471–477. https://doi.org/10.1016/j.ecns.2017.05.010
- Nestel, D., Moloney, K., & Hyde, S. (2019). Setting the scene for simulation-based education. Cambridge University Press.
- NMBI. (2016). Nurse registration programmes standards and requirements (4th ed.). Nursing and Midwifery Board of Ireland.
- Pollard, C. L., & Wild, C. (2014). Nursing leadership competencies: Low-fidelity simulation as a teaching strategy. Nurse Education in Practice, 14(6), 620–626. https://doi.org/10.1016/j.nepr.2014.06.006
- Roberts, E., Kaak, V., & Rolley, J. (2019). Simulation to replace clinical hours in nursing: A meta-narrative review. Clinical Simulation in Nursing, 37, 5–13. https://doi.org/10.1016/j.ecns.2019.07.003
- Şahin, G., & Başak, T. (2021). Debriefing methods in simulation-based education. Journal of Education and Research in Nursing, 18(3), 341–346. https://doi.org/10.5152/jern.2021.57431
- Sarmah, P., Voss, J., Ho, A., Veneziano, D., & Somani, B. (2017). Low vs. high fidelity: The importance of ‘realism’ in the simulation of a stone treatment procedure. Current Opinion in Urology, 27(4), 316–322. https://doi.org/10.1097/MOU.0000000000000401
- Schober, P., Kistemaker, K. R. J., Sijani, F., Schwarte, L., van Groeningen, D., & Krage, R. (2019). Effects of post-scenario debriefing versus stop-and-go debriefing in medical simulation training on skill acquisition and learning experience: A randomized controlled trial. BMC Medical Education, 19(334). https://doi.org/10.1186/s12909-019-1772-y
- Scott, A., & Gartner, A. (2019). 9 low fidelity simulation in a high fidelity world. Postgraduate Medical Journal, 95(1130), 687–688. https://doi.org/10.1136/postgradmedj-2019-FPM.9
- Taylor, C., Angel, L., Nyanga, L., & Dickson, C. (2017). The process and challenges of obtaining and sustaining clinical placements for nursing and allied health students. Journal of Clinical Nursing, 26(19–20), 3099–3110. https://doi.org/10.1111/jocn.13658
- Tjoflåt, I., Bodil, B. V., & Eldar, S. (2017). Implementing simulation in a nursing education programme: A case report from Tanzania. Advances in Simulation, 2(1). https://doi.org/10.1186/s41077-017-0048-z
- Ulenaers, D., Grosemans, J., Schrooten, W., & Bergs, J. (2021). Clinical placement experience of nursing students during the COVID-19 pandemic: A cross-sectional study. Nurse Education Today, 99, 104746. https://doi.org/10.1016/j.nedt.2021.104746
- Van Rooyen, D., Jordan, P., Caka, E. M., & ten Ham-Baloyi, W. (2019). Transitioning of final year nursing students to professional nurses: A best practice guideline. South African Journal of Higher Education, 33(6), 300–314. https://doi.org/10.20853/33-6-2442
- Watson, C., Gómez-Ibánez, R., Granel, N., & Bernabeu-Tamayo, M. D. (2021). Nursing students first experience on high fidelity simulation: A phenomenological research study. Nurse Education in Practice, 55, 103162. https://doi.org/10.1016/k.nepr.2021.103162
- Weiler, D. T., Gibson, A. L., & Saleem, J. J. (2018). The effect of role assignment in high fidelity patient simulation on nursing students: An experimental research study. Nurse Education Today, 63, 29–34. https://doi.org/10.1016/j.nedt.2018.01.012