ABSTRACT
Background
A growing body of conceptual evidence over the last decade has increased our understanding of parents’ experiences of having an infant with complex congenital heart disease. These concepts include parents’ feelings of uncertainty, fear, excitement, and mastery. However, little is known about parents’ experiences, confidence, and knowledge acquisition during transition from hospital to home with their infant after the first stage of complex cardiac surgery. A theoretical framework to assess, plan and implement child and family centered care would assist children’s cardiac nurses responsible for parental education, discharge planning and coordination.
Aim
To explore parents’ experiences of the transition from hospital to home with their infant, following the first stage of cardiac surgery.
Design
A prospective mixed methods longitudinal design. Semi-structured interviews were undertaken, including administration of the Maternal Confidence Questionnaire at four timepoints: before discharge following stage one cardiac surgery (T0), 2 weeks’ post discharge (T1), 8 weeks’ post discharge (T2) and after stage two surgery (T3). Qualitative data were thematically analyzed. Descriptive statistics were used to characterize the sample and non-parametric repeated measures analysis of variance was used to analyze changes over time in maternal confidence scores.
Results
Sixteen parents of 12 infants participated. Four “patterns of transition experience” emerged, the fourth “Mastery”, is discussed in this paper. Mastery can be contextualized in terms of the parents’ journeys of knowledge construction, gaining confidence and reflection. Learning was dynamic and transformational, but successful learning and acquisition of knowledge was also dependent upon the parents’ ability to absorb, integrate and adjust at any given time. Confidence at T0 was significantly lower than at T1 (p = .011), T2 (p = .018) and T3 (p = .012). There were no significant differences between scores at T1, T2 and T3. Liminality, as a concept, described the between and betwixt time that parents experienced as they were preparing for discharge from hospital; excitement to be going home balanced with the fear of being alone and confidence in looking after their fragile infant.
Conclusion
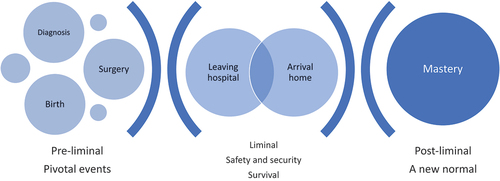
Parents of infants with complex congenital heart disease obtain knowledge, confidence, and mastery dependent upon their transition experience and their personal journey through pre-liminal, liminal, and post-liminal phases of discharge from hospital to home. A conceptual framework “Parenting through Transitions – hospital to home” emerged that could assist in structuring assessment of parents’ knowledge and support needs within a coordinated discharge process. Identifying individualized support would promote adaptation and adjustment during transition from the pre to post liminal phase, following their infant’s first stage of complex cardiac surgery.
What’s New
Parents learning was dynamic and transformational, learning opportunities overlapped transitional phases of their infant’s journey, but successful learning and acquisition of knowledge was also dependent upon the parents’ ability to absorb, integrate and adjust at any given time.
The transition from hospital to home and traversing the physical boundary of leaving the hospital for the first time with their infant (liminal phase), was loaded with emotionally traumatic experiences that could not be separated from the transition that was being explored within this study.
Adjusting to the new situation, developing confidence over time, and becoming comfortable as they mastered new skills, demonstrated that some of these parents could pass through that liminal space to mastery of a new normal (post-liminal phase), which encompassed competence, integration, and comfort.
Introduction
A growing body of conceptual evidence over the last decade has increased our understanding of parents’ experiences of having an infant with complex congenital heart disease (CHD). These concepts include parents’ feelings of uncertainty, fear, excitement, and mastery (Pridham et al., Citation2010; Rempel & Harrison, Citation2007; Rempel et al., Citation2009, Citation2012, Citation2013). Rempel and Harrison (Citation2007) focused on experiences of parenting children with complex CHD, at a time when frameworks based on theory to underpin care were not available around parenting an infant with hypoplastic left heart syndrome (HLHS), due to the newness of the surgical procedures, medical and nursing care. In the early surgical era (Rempel & Harrison, Citation2007) parents safeguarded their child’s survival through performance of advanced nursing and assessment at home and identified strategies to safeguard themselves. Their worry related to their child’s immediate and ongoing survival and associated parenting stress (Rempel & Harrison, Citation2007). A later study (Rempel et al., Citation2012, Citation2013) included parents and grandparents of infants who underwent an altered surgical procedure for HLHS and were supported at home after discharge within a home monitoring program. The findings resulted in conceptualization of a four phased process of parenting children with HLHS called “parenting under pressure”. The four phases were described as overlapping and recurring throughout their journeys from diagnosis to first surgery, discharge home, awaiting and experiencing further surgery (Rempel et al., Citation2013). A theoretical framework of five facets of parenting was established to inform development of future parent interactions (Rempel et al., Citation2012) including “survival parenting, hands off parenting, expert parenting, uncertain parenting and supported parenting”. Pridham et al. (Citation2010) also presented concepts for a theoretical model for parental support for parents of infants with complex CHD. This theoretical model was underpinned by attachment-caregiving theory, drawing on the behavioral system of caregiving, the internal working model of parenting and motivation. Despite differences in the samples (Pridham et al., Citation2010; Rempel et al., Citation2012, Citation2013) and no information about the surgical era (Pridham et al., Citation2010) there are some similarities in the two models such as mastery of skills, vigilance, support, safeguarding survival of the infant, self, couple, and family.
The two models (Pridham et al., Citation2010; Rempel et al., Citation2012, Citation2013) have emerged from Canada and North America, where health care systems differ to the National Health Service in the United Kingdom (UK). In the UK, CHD Standards and Service Specifications were published in 2016 (NHS England, Citation2016) and include standards around planning discharge and provision of support for families. Having a theoretical framework upon which to assess, plan and implement care would assist the nurse in the UK responsible for planning discharge to meet the standard of “coordinating the process and linking with the child/young person and their family” (L13, L1) (NHS England, Citation2016). Furthermore, this could assist the Children’s Cardiac Nurse Specialist to meet the standard relating to assessing parents’ needs, enabling individualized psychosocial support to promote family (and child/young person’s) adaptation and adjustment (H14 L1, p. 208) (NHS England, Citation2016).
A mixed methods study exploring parents’ experiences of the transition from hospital to home with their infant following first stage cardiac surgery (Gaskin, Citation2018; Gaskin et al., Citation2021) identified four “patterns of transition experience”: safety and security (Gaskin, Citation2018) love and support (Gaskin, Citation2018) survival (Gaskin et al., Citation2021) and mastery. This paper presents the parents’ journey of mastery and construction of knowledge after their infant’s first stage of surgery and how liminality, defined as “moving through a betwixt and between time” (Hockey, Citation2002). The findings of this study informed the development of a conceptual framework called “Parenting through transitions – hospital to home”, supporting and progressing the findings of other research studies, highlighted above (Pridham et al., Citation2010; Rempel & Harrison, Citation2007; Rempel et al., Citation2009, Citation2012, Citation2013).
Methodology and methods
Design and participants
A prospective mixed methods longitudinal design was used to study a cohort of parents being discharged home with their infant from a tertiary children’s cardiac surgery center in the United Kingdom following the first stage of cardiac surgery for complex CHD (Gaskin, Citation2018; Gaskin et al., Citation2021). Parents were eligible to participate within the 15 month recruitment timeframe (pre-COVID19), if their infant had undergone the first stage of cardiac surgery for complex CHD [functionally univentricular heart and systemic shunt dependent lesions] during the neonatal period (0–4 weeks), if they could read and understand English and could give informed consent. Ethical approval was obtained from the University Research Ethics Committee, the National Research Ethics Committee and the Local NHS Research and Development approval at the study site (REC reference: 12/WM/0375, IRAS 92 184). The participant information sheet provided details of support available to parents, including the charity helpline for Little Hearts Matter.
Data collection
Demographic data (Gaskin, Citation2018; Gaskin et al., Citation2021) were collected at baseline (T0) by the Research Nurse before semi-structured interviews were conducted at four time points: before discharge following stage one cardiac surgery (T0); two weeks after discharge (T1); eight weeks after discharge (T2) and after stage two surgery (T3). The interview guide was developed in collaboration with the research team, PhD supervisory team and external advisory group. The Middle Range Transition Theory (Meleis et al., Citation2000) informed design of the interview topic guide () to explore the type, patterns, and properties of the parents’ transitions, identifying processes that moved them toward health or vulnerability and risk. The interviews were audio-recorded and transcribed verbatim using QRS NVivo10.
Table 1. Interview topic guide.
All interviews were conducted by the Principal Investigator (PI), except for two interviews (at T0) conducted by the Research Nurse (RN) because of earlier than expected discharge of the infants. The PI (KG) was based at the university more than 30 miles away and unable to get to the hospital in time. Interview training had been provided for the RN with particular emphasis on open questions and staying in the interviewer role rather than deviating to a counselor role, directing parents to the participant information leaflet for available support services. A date and time for the subsequent telephone interviews was arranged at the end of each interview; after two attempts to call with no response the parent was deemed not available. The final interview was arranged by the Research Nurse, and undertaken by the PI, after the second stage of surgery had been conducted and they were ready to go home; they were given the choice of a face to face or telephone interview.
Instruments
Confidence in the parenting role was measured at each of the timepoints using the Maternal Confidence Questionnaire [MCQ] (Badr, Citation2005). Few tools have been developed and psychometrically tested to assess maternal confidence (Parker et al., Citation1992). The scale consists of 14 items: each item is answered on a 5-point scale from 1 = never to 5 = a great deal. The scale measures maternal confidence in parenting skills and the mother’s ability to recognize her infant’s needs. After reversing the two negatively worded items (items 10 and 12), a total score is derived from the mean of the totaled 14 item scores. Total scores vary from 14 (lower maternal confidence) to 70 (higher maternal confidence) and means vary between 1 and 5 for each question. The MCQ is uni-dimensional with a higher score indicating a higher perceived competence (Badr, Citation2005). Face and content validity have been evidenced (Zahr, Citation1991). The scale has been used in more than 40 research studies, establishing reliability and validity; it has also been translated into 9 languages (Meleis et al., Citation2000). The MCQ has been used in one other study (Fonseca et al., Citation2013) including both mothers and fathers of infants with a congenital anomaly (17.8%, n = 16 with CHD). In this latter study, the dimension “Evaluation of the Parenting Experience” was excluded because its Cronbach’s alpha was only .56 for the comparison group. For the remaining dimensions, values for Cronbach’s alpha ranged from .75 (Caretaking Tasks, clinical group) to .84 (Knowledge of the Infant, comparison group).
Data analysis
Qualitative analysis
Criteria for trustworthiness of a qualitative study provided the framework for design and reporting (Guba, Citation1981) and corresponded to constructs utilized within positivist research (Shenton, Citation2004). A six-phased approach was used to become familiar with the data: generate initial codes; search for themes; review themes; define and name themes; and produce the report (Braun & Clarke, Citation2006).
Quantitative analysis
The Statistical Package for the Social Sciences (IBM SPSS Inc.) version 26 for Windows was used for the quantitative data analysis. Descriptive statistics were used to characterize the sample and non-parametric repeated measures analysis of variance was used to look at changes over time in maternal confidence scores.
Mixed methods analysis
Comparison occurred within and across the time points to identify relationships between the qualitative and quantitative data. As the dominant approach was qualitative, the quantitative data were amalgamated as relevant into the patterns arising from the qualitative analysis.
The analysis by the PI (KG) was independently verified by the Chief Clinical Investigator (DB), external advisor (JW) two members of the PhD supervisory team (GF and TK).
Results
Parents of 13 infants were recruited (from forty-seven families meeting the inclusion criteria); one parent was removed from analysis as they did not participate, resulting in 16 parents (12 mothers, 4 fathers) participating. Completion of interviews () and report tools varied due to readmissions of the infant to hospital or non-availability of the parents. The qualitative data set included 38 interviews. Mean duration of interviews was: T0: 21 mins (SD 9); T1: 19 mins (SD 12), T2: 22 mins (SD 10), T3: 31 mins (SD 12). The increase in duration may have been due to parents’ improved confidence and as T3 interviews were conducted after second stage surgery, parents were feeling more relaxed. Parents’ and infants’ demographics are presented in .
Table 2. The number of completed self-report tools and interviews at T0, T1, T2, T3.
Table 3. Parents’ and infants’ demographics data.
The fourth theme “Mastery” is reported here. Mastery can be contextualized in terms of the parents’ journeys of knowledge construction, gaining confidence and reflection. Parents’ quotes are illustrated in .
Table 4. Illustrative quotes.
Knowledge construction
Knowledge construction commenced from the time of their infant’s diagnosis. Parents’ experiences of learning, knowing, and understanding their infant’s diagnosis were dependent upon when they received the diagnosis; the social situation; who was involved in providing the information; and how the information was given and where.
Knowledge construction was not only an explicit transfer of information but tacitly embodied through their emotions and feelings of shock and devastation. Experiential learning (both explicit and tacit) continued in the ward environment as parents asked questions and eagerly watched and learned from the nursing and medical staff to ensure safety and security once they were discharged home. Parents also learned from the experiences of other parents, the excitement of another infant being discharged or the distress of another infant’s death, as well as through sharing their collective parenting experiences. They learned the social and cultural norms of being in hospital; being a “cardiac parent” and being part of a socially constructed community of medical parents.
For parents transitioning home with their infant, (“pre-liminal phase”) there were physical boundaries, such as crossing the threshold of the ward into the outside world, possibly for the very first time with their fragile baby. These parents and their infants had already transitioned across several physical and situational boundaries since their infant’s birth, such as retrieval and transfer from the maternity unit, and transition to the ward from intensive care. Parents had faced a roller coaster of emotionally traumatic events. So, the transition from hospital to home and traversing the physical boundary of leaving the hospital for the first time with their infant was loaded with emotionally traumatic experiences that could not be separated from the transition that was being explored within this study.
However, for some families, transition from hospital to home was a constraint but it was also enabling. Liminality occurred for parents at the point of being told that they could go home with their baby; this was not accounted for in the middle range transition theory but refers to the “liminal phase.” For a while, some parents were in an uncertain place where they could not visualize what was ahead and how it would feel, and this created anxiety and fear at the same time as excitement. For these parents the transition from hospital to home was a crossing point from a place of safety and security into the unknown, uncertain place. Parents were also bounded by the physical, emotional, and social constraints in terms of their preparedness to go home, the fragility of their infant, the distance between the hospital and home, their home environment, and the availability of support. Those parents that did not want to go home were not ready or comfortable enough to cross the physical boundary into the liminal space. Parents were also bounded by a common ground, the social community that they had developed whilst in the ward environment of being a parent, but more importantly the boundary of being a parent of an infant with CHD. Exiting into a world where those boundaries were different, where other parents did not have the same experiences as theirs, was frightening, irritating, and isolating.
Once home, further experiential learning occurred: establishing their own routines, learning to cope without the safety net of the monitors, alarms, and readily available specialist knowledge in hospital. But knowing that specialist advice was available at the end of the phone. They learned to cope on their own, to source love and support from other places and to develop personal knowledge of their infant’s individualized needs. This knowledge became cognitively more explicit, as they learned to understand the signs and symptoms they were observing and hearing.
Parents already bound by the cardiac parent community had to decide whether to integrate the explicit and tacit knowledge and information presented to them by different social constructs, such as individuals with only “normal baby experience” and other cultural and social environments (knowing the diversity of environments and organizing days out around giving medications and feeds). An important element of this learning was the shift in their sources of support and the integration of knowledge, as parents began sharing their experiences and listening to others in the wider “cardiac parent community” via social networking sites.
Confidence
Parents’ confidence levels (MCQ) at the four interview time points are presented alongside their illustrative quotes (). Confidence (MCQ) scores could range between 14–70, higher scores equated to higher levels of confidence. There was an increase in mean MCQ from T0 (50, SD 7.86) to T1 (mean 57, SD 6.24) and a decrease in MCQ for some parents at T2 (mean 57, SD 3.81). There was an increase in mean MCQ scores at T3 (mean 60, SD 4.69). A one-way ANOVA indicated a significant difference between scores across the time points (p = .005) for mothers. Post-hoc Wilcoxon tests to determine where the differences were indicated that confidence at baseline, T0, was significantly lower than at T1 (p = .011), T2 (p = .018) and T3 (p = .012). There were no significant differences between scores at T1, T2 and T3. Although not significant, there was a trend of increasing confidence scores over time. A one-way ANOVA was not performed for fathers’ confidence scores as complete data were only available for two fathers across the four time points.
Reflection and looking to the future
In the accounts at T3 it became evident that emotional learning was taking place, parents could reflect on their feelings and emotions at T0 and recognize how they had moved on; knowing what they did now, they wondered why they had been so fearful about going home for the first time. Parents’ accounts at T3 demonstrated positivity more than negativity and a shift in focus toward looking to the future, recognizing that there was still some learning and uncertainties ahead. A process of integration was identified at T3, where parents could assimilate the emotional, experiential, and cognitive learning that had taken place, resulting in the development of knowing and creation of knowledge.
The time frame in achieving this “post liminal,” new-normal was different and dynamic for each family, but so was the length of time that they were at home with their fragile infant between the first and second stages of surgery. Whilst there were some similarities identified through the inductive qualitative analysis, the key message was the diversity of each family’s experience. They had different ways of coping, different demographics, different family resilience strategies, different support mechanisms and different values and beliefs.
Discussion
The first main finding was that the concept of knowledge construction, resulting in increasing confidence and mastery for these parents, was one building block in the theory of transition from hospital to home. Confidence levels were significantly lower before parents were discharged home with their infant (T0), compared to confidence levels at each of the other three time points. So other building blocks of each parent’s multi-faceted transitions needed to be considered due to the various nuances of the parents’ experiences (Gaskin, Citation2018; Gaskin et al., Citation2021). Thus, whilst the transition related to the physical transition from hospital to home, here transition was also identified as a journey through the construction of knowledge from the point of diagnosis and varied depending upon individual parental characteristics, therefore learning was not simply information transfer.
Transmission of the professional’s knowledge cannot be assumed as sufficient for parents to fully understand the implications of having an infant with complex CHD (Giordan et al., Citation1999). Ayra et al. (Citation2013) explored the expectations of parents and cardiologists regarding education and counseling and found that parents would have preferred more than cardiologists perceived them to want. Twaddell (Citation2013) explored parents’ information needs in comparison to information given by HCPs during their infant’s hospitalization and after their infant’s discharge; parents looked for information relating to their infant’s changing needs and condition and wanted consistent information about the condition of their infant in terms they understood. Likewise, Tregay et al. (Citation2016) qualitatively assessed the discharge processes and post-discharge care in the community for infants discharged after CHD surgery in the first year of life. Written documentation from tertiary centers frequently lacked crucial information and contained too many specialist terms, further demonstrating that these parents want consistent and individualized information.
In our study, parents came to the situation with their own ideas and experiences that influenced their knowledge construction (Arya et al., Citation2013) perhaps reflecting constructivist models of learning. It was not only the scientific concepts impacting on their infant’s survival that parents needed to learn, but they also needed to learn to be parents of an infant with complex CHD and the minutiae that accompanied the responsibility, throughout the multi-faceted transitions that they experienced. The maternal confidence questionnaire (Badr, Citation2005) focuses on “knowledge, skills, and feelings”, suggesting that the significantly lower confidence levels prior to discharge home (T0) may have related to parents’ lack of knowledge, lack of skills and mixed emotions (feelings) before going home.
For parents in our study, learning was dynamic and transformational; learning opportunities overlapped transitional phases of their infant’s journey, but successful learning and acquisition of knowledge were also dependent upon the parents’ ability to absorb, integrate and adjust at any given time. Feelings about going home referred to their fears (Gaskin et al., Citation2021) lack of preparation for discharge and concerns about looking after their fragile infant at home on their own, balanced with their excitement about the situational change from the institutionalized hospital environment to the physical and psychological comforts of their own home. We identified a time of “liminality” when parents were moving through a liminal space (Turner, Citation1967, Citation1969; Van Gennep, Citation1960); in contrast, to the “false optimism” discussed by Lee and Rempel (Citation2011). This betwixt and between time enabled the parents to develop, maintain and restore a sense of self and control such that they were ready to face the hurdle of the transition from hospital to home.
Whilst processes of parents moving “from one place to another” had been identified in the models “Parenting Under Pressure” and “Facets of Parenting” (Rempel et al., Citation2012, Citation2013) and perhaps as motivational categories (Pridham et al., Citation2010) none of the extant evidence identified liminality as a concept or as a means of contextualizing the transitional parenting experience. A conceptual framework emerged () called “Parenting through Transitions – hospital to home”, representing a dynamic model of transition, incorporating the concept of liminality and parental experiences of transition through a pre-liminal phase, liminal phase, and post-liminal phase.
Mastery (post liminal phase) also related to “reflection and looking to the future”. Parents’ accounts at T3 demonstrated that the space or distance from their infant’s hospitalization had afforded them the opportunity to undergo a process of rational analysis of their earlier experiences (Jordi, Citation2011). It was evident that this reflective process was cognitive and included the richness and complexity of their feelings (Gaskin et al., Citation2021) induced before and during the traumatic events they experienced. Jordi (Citation2011) argues that the individuality of our experiences provides us with tacit knowledge that enables us to have awareness of who we are and that this implicit knowledge also materializes explicitly, resulting in cognitive construction of its meaning becoming evident in language, which reflects the findings here.
Whilst parents learnt cognitively and emotionally from other cardiac parents in hospital, there was a shift in the sources of advice and support that parents utilized over time. External engagement with other cardiac parents and parent support groups increased as the parents became more confident. In addition, the mechanism of obtaining advice and support became more virtual, with parents choosing to communicate with other cardiac parents via online social networking sites. Some parents actively sought electronic resources and Applications that they could utilize to support the constant monitoring of their infant. Online systems are currently being explored as a method of providing support post-discharge alongside an early warning tool for parents to use at home to assess and monitor their infants, called the Congenital Heart Assessment Tool (Gaskin et al., Citation2022, Citation2018; Smith et al., Citation2022).
Limitations
Telephone interviews were more difficult with some parents in relation to keeping the conversation going. Including only English-speaking parents limited the number of parents that could be approached as well as limiting the nature of experiences identified. Not all parents participated in all four interviews, for a variety of reasons. One parent was very nervous about being “interviewed” before discharge and her interpretation of the word “interview” may have impacted on her lack of participation with the other three interviews. The one-way ANOVA for maternal confidence scores only included those mothers with complete data sets (n = 6); as there were only two complete data sets for fathers this precluded further analysis of these scores.
Conclusion
Parents of infants with complex CHD obtain knowledge, confidence, and mastery dependent upon their transition experience and their personal journey through pre-liminal, liminal, and post-liminal phases of discharge from hospital to home. Parents need to be effectively and individually prepared for the intricacies of being a cardiac parent and to identify signs of clinical deterioration before their infant is discharged. However, for discharge preparation to be successful and consistent, nurses need to have knowledge of learning theories, coaching and guidance skills to effectively teach parents about their infant’s condition and what to look out for.
Acknowledgments
Suzie Hutchinson, CEO, and Isabelle Baumber, Parent Representative, Little Hearts Matter; Amanda Daniels, Advanced Nurse Practitioner, Birmingham Children’s Hospital, and David Barron, Chief Clinical Investigator, Consultant Cardiac Surgeon, Birmingham Children’s Hospital; Dr Jo Wray, Institute of Child Health, London contributed as members of the External Advisory Group and Research Team.
Mel Rooney, Needa Mohammed and Lucy Cooper, Research Nurses, Wellcome Trust Clinical Research Facility, Birmingham Children’s Hospital, recruited families into the study and gathered baseline data.
Coventry University was the sponsor for the study (2012-2016). Professor Gill Furze and Dr Tim Kilner, Coventry University PhD Supervisory Team 2011 until 2013, contributed to the design of the feasibility study and preparation for ethics approval. Dr Charlotte Hilton became Director of Studies in 2013-2016, Dr Martin Bollard and Dr Penny Upton joined the supervisory team in 2015-2016.
The team acknowledge the support of Heart Research UK [grant number RG2620/12/14] and the NIHR through the Comprehensive Clinical Research Network as the Feasibility Study has been adopted to the NIHR Portfolio.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Arya, B., Glickstein, J. S., Levasseur, S. M., & Williams, I. A. (2013). Parents of children with congenital heart disease prefer more information than cardiologists provide. Congenital Heart Disease, 8(1), 78–85. https://doi.org/10.1111/j.1747-0803.2012.00706.x
- Badr, L. K. (2005). Further psychometric testing and use of the maternal confidence questionnaire. Issues in Comprehensive Pediatric Nursing, 28(3), 163–174. https://doi.org/10.1080/01460860500227572
- Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. https://doi.org/10.1191/1478088706qp063oa
- Fonseca, A., Nazaré, B., & Canavarro, M. C. (2013). Parental psychological distress and confidence after an infant’s birth: The role of attachment representations in parents of infants with congenital anomalies and parents of healthy infants. Journal of Clinical Psychology in Medical Settings, 20(2), 143–155. https://doi.org/10.1007/s10880-012-9329-9
- Gaskin, K., Barron, D., & Wray, J. (2021). Parents’ experiences of transition from hospital to home after their infant’s first stage cardiac surgery: Psychological, physical, physiological and financial survival. Journal of Cardiovascular Nursing, 36(3), 283–292. Epub ahead of print. PMID: 32842034. https://doi.org/10.1097/JCN.0000000000000727
- Gaskin, K., Smith, L., & Wray, J. (2022). An improved congenital heart assessment tool: A quality improvement outcome. Cardiology in the Young, 33(4), 1–6. https://doi.org/10.1017/S1047951122001275
- Gaskin, K. L. (2018, July-August). Patterns of transition experience for parents going home from hospital with their infant after first stage surgery for complex congenital heart disease. Journal of Pediatric Nursing, 41, e23–e32. Advance online publication. https://doi.org/10.1016/j.pedn.2017.11.013
- Gaskin, K. L., Wray, J., & Barron, D. J. (2018, March 22). Acceptability of a parental early warning tool for parents of infants with complex congenital heart disease: A qualitative feasibility study. Archives of Disease in Childhood. 103(9),880–886. Online: 1468-2044 Published online. https://doi.org/10.1136/archdischild-2017-313227
- Giordan, A., Jacquemet, S., & Golay, A. (1999). A new approach for patient education: Beyond constructivism. Patient Education & Counseling, 38(1), 61–67. https://doi.org/10.1016/S0738-3991(98)00108-6
- Guba, E. G. (1981). Criteria for assessing the trustworthiness of naturalistic inquiries. Education Communication Technology, 29(2), 75–91. https://doi.org/10.1007/BF02766777
- Hockey, J. (2002). The importance of being intuitive: Arnold Van Gennep’s the rites of passage. Mortality, 7(2), 210–217. https://doi.org/10.1080/135762702317447768
- Jordi, R. (2011). Reframing the concept of reflection: Consciousness, experiential learning, and reflective learning practices. Adult Education Quarterly, 61(2), 181–197. https://doi.org/10.1177/0741713610380439
- Lee, A., & Rempel, G. R. (2011). Parenting children with hypoplastic left heart syndrome: Finding a balance. Pediatric Nursing, 16(3), 179–189. https://doi.org/10.1111/j.1744-6155.2011.00289.x
- Meleis, A. I., Sawyer, L. M., Im, E. O., Hilfinger Messias, A. K., & Schumacher, K. (2000). Experiencing transitions: An emerging middle-range theory. Advances in Nursing Science, 23(1), 12–28. https://doi.org/10.1097/00012272-200009000-00006
- NHS England. (2016) CHD standards and service specification. Retrieved November 5, 2023, from https://www.england.nhs.uk/wp-content/uploads/2018/08/Congenital-heart-disease-standards-and-specifications.pdf
- Parker, S. J., Zahr, L. K., Cole, J. G., & Brecht, M. L. (1992). Outcome after developmental intervention in the neonatal intensive care unit for mothers of preterm infants with low socioeconomic status. The Journal of Pediatrics, 120(5), 780–785. https://doi.org/10.1016/S0022-3476(05)80248-3
- Pridham, K., Harrison, T., Krolikowski, M., Bathum, M. E., Ayres, L., & Winters, J. (2010). Internal working models of parenting. Motivations of parents of infants with a congenital heart defect. Advances in Nursing Science, 33(4), E1–E16. https://doi.org/10.1097/ANS.0b013e3181fc016e
- Rempel, G. R., & Harrison, M. J. (2007). Safeguarding precarious survival: Parenting children who have life –threatening heart disease. Qualitative Health Research, 17(6), 824–837. https://doi.org/10.1177/1049732307303164
- Rempel, G. R., Harrison, M. J., & Williamson, D. L. (2009). Is “treat your child normally” helpful advice for parents of survivors of treatment of hypoplastic left heart syndrome? Cardiology in the Young, 19(2), 135–144. https://doi.org/10.1017/S1047951109003485
- Rempel, G. R., Ravindran, V., Rogers, L. G., & Magill-Evans, J. (2013). Parenting under pressure: A grounded theory of parenting young children with life-threatening congenital heart disease. Journal of Advanced Nursing, 69(3), 619–630. https://doi.org/10.1111/j.1365-2648.2012.06044.x
- Rempel, G. R., Rogers, L. G., Ravindran, V., & Magill-Evans, J. (2012). Facets of parenting a child with hypoplastic left heart syndrome. Nursing Research and Practice, 2012, 1–9. [online] Retrieved November 5, 2023, from. https://doi.org/10.1155/2012/714178
- Shenton, A. K. (2004). Strategies for ensuring trustworthiness in qualitative research projects. Education for Information, 22(2), 63–75. https://doi.org/10.3233/EFI-2004-22201
- Smith, L., Wray, J., & Gaskin, K. (2022). Evaluating the congenital heart assessment tool: A quality improvement project. Cardiology in the Young, 1–8. https://doi.org/10.1017/S1047951122001792
- Tregay, J., Wray, J., Crowe, S., Knowles, R., Daubeney, P., Franklin, R., Barron, D., Hull, S., Barnes, N., Bull, C., & Brown, K. L. (2016). Going home after infant cardiac surgery: A UK qualitative study. Archives of Disease in Childhood, 101(4), 320–325. https://doi.org/10.1136/archdischild-2015-308827
- Turner, V. (1967). The forest of symbols: Aspects of Ndembu Ritual. Cornell University Press.
- Turner, V. (1969). The ritual process: Structure and anti-structure. Routledge.
- Twaddell, J. W. (2013) Parent education needs of infants with complex life-threatening illnesses [ Unpublished PhD Thesis]. The University of North Carolina at Greensboro. Retrieved November 5, 2023, from https://libres.uncg.edu/ir/uncg/f/Twaddell_uncg_0154D_11155.pdf
- Van Gennep, A. (1960). The rites of passage. Routledge and Kegan Paul.
- Zahr, L. K. (1991). The relationship between maternal confidence and mother-infant behaviours in premature infants. Research in Nursing & Health, 14(4), 279–286. https://doi.org/10.1002/nur.4770140406