ABSTRACT
A 9 hour old twin neonate, who was treated with flecainide in utero for fetal supraventricular tachycardia, presented with hypotension and a wide complex tachycardia concerning for flecainide toxicity. The patient was given a bolus of sodium bicarbonate with transient narrowing of her QRS complex. She was then intubated and started on a sodium bicarbonate drip with full resolution of her wide complex tachycardia within 24 hours. Work up showed no evidence for structural cardiac pathology or infection and she did not experience any further arrhythmias after termination of her presenting wide complex tachycardia. The patient was discharged home at 10 days of age and has had no further sequelae. This case report describes a novel presentation of in utero flecainide toxicity and summarizes the therapies available to treat this rare, but potentially lethal, presentation.
Case presentation
A 9 hour old twin girl presented to our care with a wide complex tachycardia concerning for flecainide toxicity. Her prenatal course was complicated by in utero supraventricular tachycardia (SVT), for which her mother was treated with flecainide.
The patient was born at 35 weeks and 6 days gestation. Electrocardiogram (EKG) demonstrated a wide complex tachycardia with heart rate 190. She was breathing comfortably on room air and appeared well perfused. Her mother's flecainide level was found to be 1.6 (ref range 0.2–1.00) at the time of parturition.
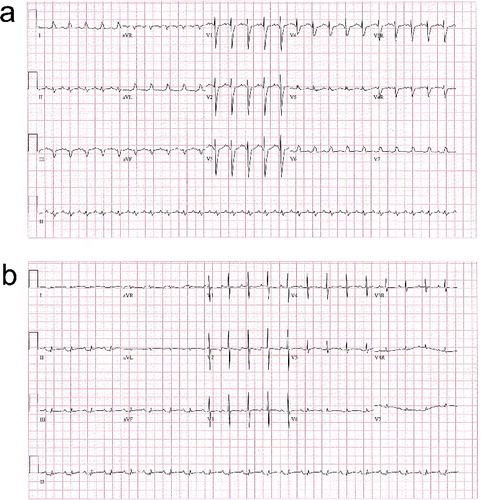
Upon transfer to our facility, the patient remained in a wide complex tachyarrhythmia (). She developed hypotension, with cool extremities and non-palpable lower extremity pulses bilaterally. Echocardiogram revealed mild to moderately depressed ventricular function with ventricular dyssynchrony. No structural abnormalities were identified.
Figure 1. Patient's initial EKG on admission. Patient was in a wide complex tachycardia (HR 195, QRS 164 ms).
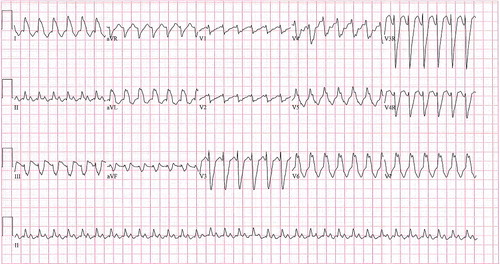
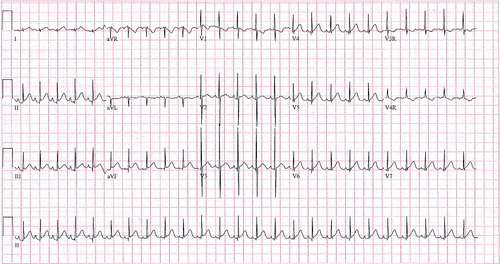
She was intubated and given a 2.5 mEq (1mEq/kg) IV bolus of sodium bicarbonate (NaHCO3), which led to a transient narrowing of the QRS complex. She was subsequently given four repeated doses (2.5 mEq × 2 followed by 5 mEq × 2) and started on a 0.5 mEq/kg/hr NaHCO3 drip that was then slowly up titrated based on clinical effect. She remained on the NaHCO3 drip for 8.5 hours. During this time, her cardiac output improved and her QRS complex narrowed (). Follow-up echocardiogram demonstrated improved ventricular function and synchrony. She was extubated on hospital day 2 and remained hemodynamically stable. Her EKG fully normalized and she did not experience recurrence of her wide complex rhythm nor did she re-develop SVT (). The patient was discharged home in good condition at 10 days of age.
Discussion
Flecainide is a class IC antiarrhythmic used to treat pediatric and fetal patients w/ recalcitrant SVT and ventricular dysrhythmias. For fetal populations in particular, flecainide appears to be more efficacious than digoxin [Citation1]. Flecainide works by blocking fast-acting sodium channels in the myocardium, thereby slowing the rate of depolarization in myocytes, resulting in slowed conduction in the atria and His-Purkinje system as well as reduced contractility [Citation2]. In large doses, flecainide can lead to conduction disturbances with widening of the QRS complex that then degrade into ventricular tachycardia, asystole, and cardiovascular collapse [Citation3]. Moreover, the drug has an active metabolite that results in a half life of nearly 30 hours, resulting in very slow clearance time. Overdose, while rare, has a mortality rate of up to 22% from associated cardiogenic collapse and shock [Citation4]. Cardiac toxicity typically predominates the symptoms noted with overdose, but neurotoxicity has also been described, including confusion/altered mental status, hallucinations, seizures, and myoclonus [Citation5]. Infants have experienced significant flecainide toxicity in the setting of accidental dosing errors [Citation6,Citation7]. However, toxic and lethal effects have also been noted in very young patients who have received appropriate dosing with levels within an acceptable therapeutic range, highlighting the narrow therapeutic index of this medication [Citation8].
Here we present a neonate with presumed flecainide toxicity after in utero treatment for fetal SVT. The patient lacked evidence for other possible causes such as electrolyte imbalances, signs of sepsis, or structural cardiac pathology. Though she presented with a wide complex tachycardia, her symptoms of reduced cardiac output and signs of hypoperfusion were out of proportion to the heart rate. Given these findings, the time course of clinical improvement and the rapid transient narrowing of her QRS complex in response to NaHCO3 treatment, and her mother's elevated serum flecainide levels, flecainide toxicity remains the most likely etiology for the patient's presentation.
Interestingly, the patient's twin brother did not show any evidence of concomitant toxicity despite being exposed to the same maternal serum levels. Flecainide is metabolized by CYP2D6, one of the cytochrome P450 enzymes [Citation9]. Due to genetic polymorphisms, about 7% of Caucasians and African Americans are deficient in this enzyme [Citation10]. Though we were unable to obtain confirmation in the form of a serum flecainide level, we speculated that the affected twin may have been a poor metabolizer of flecainide due to such a deficiency, and that she manifested a toxicity when she was separated from maternal/placental metabolic support.
Flecainide toxicity and treatment mirrors that of other sodium channel blockers such as tricyclic antidepressants and class IA antiarrhythmics. As in treatment of acute toxicity arising from these drugs, sodium bicarbonate is considered the cornerstone of treatment. Its efficacy in management of flecainide toxicity has been demonstrated in animal models as well as in clinical practice [Citation3,Citation6,Citation7,Citation11,Citation12]. Mechanistically, it is thought to increase extracellular sodium levels, thereby competitively overcoming the block on fast-acting sodium channels and stabilizing myocardium. Alkalization is also thought to play a role by converting flecainide, which is a weak acid, to the inactive non-ionized form that is incapable of receptor binding [Citation13,Citation14]. The therapeutic end point for treatment is narrowing of the QRS on ECG. If multiple doses fail to narrow the QRS complex and improve the hemodynamics, then alternative treatment options, lipid emulsion therapy, and extracorporeal membrane oxygenation (ECMO) can be considered [Citation6,Citation11,Citation12,Citation15–20].
In conclusion, we present a case of a newborn infant likely suffering from flecainide toxicity after in utero treatment for SVT. Flecainide toxicity has a very high associated morbidity and mortality that requires prompt recognition and treatment. Our patient responded well to standard treatment with IV sodium bicarbonate and supportive care. In patients with refractory flecainide toxicity, intralipid emulsion and ECMO may be considered.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Strizek B, Berg C, Gottschalk I, et al. High-dose flecainide is the most effective treatment of fetal supraventricular tachycardia. Heart Rhythm. 2016 Jun;13(6):1283–1288.
- Krishnan SC, Antzelevitch C. Flecainide-induced arrhythmia in canine ventricular epicardium. Phase 2 reentry? Circulation. 1993;87:562–572.
- Courand, P, Sibellas F, Ranc S, et al. Arrythmogenic effect of flecainide toxicity. Cardiol J. 2013;20:203–205.
- Koppel C, Oberdisse U, Heinemeyer G. Clinical course and outcome in class IC antiarrhythmic overdose. Clin Toxicol. 1990; 28:433–444.
- Ghika J, Goy J, Naegeli C, et al. Acute reversible ataxo-myoclonic encephalopathy with flecainide therapy. Schweiz Arch Neurol Psychiatr. 1994;145 (1):4–6.
- Kwan D, Vohra R, Dyer J, et al. An infant with a heartbreaking medication error. Pediatr Emerg Care. 2014;30(12):e1–5.
- Jang D, Hoffman R, Nelson L. A case of near-fatal flecainide overdose in a neonate successfully treated with sodiumbicarbonate. J Emerg Med. 2013;44(4):781–783.
- Romain N, Giroud C, Michaud K, et al. Fatal flecainide intoxication. Forensic Sci Int. 1999;106(2):115–123.
- Doki K, Homma M, Kuga K, Kusano K, Watanabe S, Yamaguchi I, Kohda Y. Effect of CYP2D6 genotype on flecainide pharmacokinetics in Japanese patients with supraventricular tachyarrhythmia. Eur J Clin Pharmacol. 2006;62(11):919–926.
- Koski, A, Ojanpera, I, Sistonen, J, et al. A fatal doxepin poisoning associated with a defective CYP2D6 genotype. Am J Forensic Med Pathol. 2007;28(3):259–261.
- Ellsworth H, Stellpflug S, Cole J, et al. A life-threatening flecainide overdose treated with intravenous fat emulsion. Pacing Clin Electrophysiol. 2013;36:87–89.
- Moussot PE, Marhar F, Minville V, et al. Use of intravenous lipid 20% emulsion for the treatment of a voluntary intoxication of flecainide with refractory shock. Clin Toxicol (Phila). 2011;49:514.
- Bajaj AK, Woosley RL, Roden DM. Acute electrophysiologic effects of sodium bicarbonate administration in dogs treated with O-desmethyl encainide. Circulation. 1989;80:994–1002.
- Salerno DM, Murakami MM, Johnston RB, et al. Reversal of flecainide-induced ventricular arrhythmia by hypertonic sodium bicarbonate in dogs. Am J Emerg Med. 1995;13(3):285–293.
- Mukhtar O, Archer J, Dargan P, et al. Lesson of the month 1: acute flecainide overdose and the potential utility of lipid emulsion therapy. Clin Med. 2015;15(3):301.
- Brumfield E, Bernard KR, Kabrhel C. Life-threatening flecainide overdose treated with intralipid and extracorporeal membrane oxygenation. Am J Emerg Med. 2015;33:1840.e3–1840.e5
- Weinberg GL, VadeBoncouer T, Ramaraju GA, et al. Pretreatment or resuscitation with a lipid infusion shifts the dose–response to bupivacaine-induced asystole in rats. Anesthesiology 1998;88(4):1071–1075.
- Fettiplace MR, Ripper R, Lis K, et al. Rapid cardio-tonic effects of lipid emulsion infusion. Crit Care Med. 2013;41(8):e156–e162.
- Cave G, Harvey M, Quinn P, et al. Hypertonic sodium bicarbonate versus intravenous lipid emulsion in a rabbit model of intravenous flecainide toxicity: no difference, no sink. Clin Toxicol. 2013;51:394–397.
- Auzinger GM, Scheinkestel CD. Successful extracorporeal life support in a case of severe flecainide intoxication. Crit Care Med. 2001;29(4):887–890.