Abstract
Many have suggested different ways of conceptualizing mental health conditions in mental health services. However, eliciting the unicity of the individual experience of mental health conditions in the diagnostic process remains challenging. In this position paper, we describe the diagnostic process in psychiatry and outline three challenges for which insights from the design research paradigm, in particular so-called generative sessions, may represent an opportunity for innovation. We suggest that by implementing generative sessions, conversations about individual experience can be initiated, the focus on diagnostic categories can be shifted towards personal variation, and the integration of empirical evidence of recovery can be facilitated. Therefore, we argue that exploring generative sessions in the diagnostic process can stimulate incremental and iterative advancements in diagnostic systems. To test its hypothesized impact on clinical practice, we recommend several directions for further research in co-creation with traditional mental health professionals, people with mental health conditions, and people with lived experience.
Background
It is estimated that at least one in four people will develop a mental health condition throughout their lifetime (World Health Organization Citation2001). Over the past years, different shifts are transforming mental health care services. For instance, promoting mental wellbeing and emphasis on preventative measures is something of growing interest. The emergence of positive psychology resulted in a focus on people’s positive attributes, psychological assets, and resilience (Seligman and Csikszentmihalyi Citation2000). The Foresight Report concluded after reviewing extensive evidence that there are five ways of promoting wellbeing: to connect, be active, take notice, keep learning, and give (The Government Office for Science Citation2008). In line with this, the recovery movement made important contributions to the recognition of the ability of people with mental health problems to participate in society (Davidson Citation2016), while in person-centred care the acknowledgment of experiential knowledge contributed to the focus on an individual’s goals and life circumstances (Dixon, Holoshitz, and Nossel Citation2016). Despite these developments, all focussing on concepts like resilience, autonomy, and agency of people, many individuals will still need clinical care, starting with a process of diagnosis and followed by application of a treatment plan. In the Netherlands – and in Western Medicine in general – the diagnosis is crucial for financing and operationalizing the treatment.
Instead of using the terms mental illness and mental disorders, we use the more neutral term ‘mental health conditions’, in line with The Lancet Commission report on Ending Stigma and Discrimination in Mental Health (Thornicroft et al. Citation2022). We only refer to mental illness and mental disorders to quote technical terms that remain the norm in clinical practice. In our view, mental health conditions are complex, part of the human condition, and subjective. The clinical relevance of mental health conditions refers to qualities of persistence, subjective suffering, and care needs.
Diagnosis and classification in psychiatry
The diagnostic process – arriving at a diagnosis – is a tailor-made process for each individual. It is an ongoing process of weighing data, aetiological consideration and hypothesis formation based on theory (Ruissen Citation2014). The diagnostic process is a professional activity based on three elements, grounded in research (Bruyn et al. Citation2003): theory development of the problems/complaints and problematic behaviour, operationalization and its subsequent measurement, and the application of appropriate diagnostic methods. At the heart of this process are hypotheses, selection of tools, and verifiable predictions. Tools and methods currently used in the diagnostic process can be categorized into interviews, observations, questionnaires, and tests (Barelds and Luteijn Citation2019). The diagnosis – the product of the diagnostic process – is considered important for treating people with mental health conditions. However, what should constitute a diagnosis remains a topic of discussion (Frances and Widiger Citation2012; Guloksuz and van Os Citation2018; Whitaker Citation2010). Currently, the diagnosis identifies the symptoms, causes, consequences, sustaining factors, disabling influences, and underlying mechanisms of the suffering – all as interpreted by the professional. Most importantly, diagnosis allows for the personal variation that exists between people. Thus, a professional wants to get a good understanding of the person’s situation to start therapy and treatment with a focus on reducing suffering and incapacity (Pies Citation2012) and to increase resilience.
Diagnosis refers to classification with treatment and prognostic utility (Pies Citation2012). Classification – the identification of a disorder – is, as opposed to diagnosis, universal, static, descriptive, often dichotomous or polytomous and, in the case of the DSM-5 (APA Citation2013), aetiology-free and atheoretical (Ruissen Citation2014). Classification is identifying and assigning a mental disorder to a described category – known in less friendly terms as ‘labelling’. Classification helps understanding information on mental disorders and enables researchers to quantitatively record the prevalence of mental disorders, as in the NEMESIS and NEMESIS-2 studies in the Netherlands (Vollebergh and Schoemaker Citation2003; de Graaf, Have, and van Dorsselaer Citation2010). However, classifications are sometimes perceived as nothing more than umbrella terms that indicate a collection of symptoms or patterns that frequently occur (Vanheule Citation2014) and have been criticized for as long as there is a classification system (van Os et al. Citation2013; Boevink Citation2006; Menninger et al. Citation1958). Therefore, it has been argued that mental health conditions should be considered more from the perspective of the individual experience of people who suffer from these conditions (Stoyanov et al. Citation2012). Given that exploring other paradigms is recommended (Leichsenring et al. Citation2022), that people with lived experience should have an important role (Thornicroft Citation2022), and that creative thinking is argued to be required (Borsboom, Haslbeck, and Robinaugh Citation2022), we see this as an opportunity to investigate how the introduction of insights of the design discipline might contribute to the diagnostic process.
In its current state, the diagnostic process faces multiple challenges with chances for innovation, with the challenge of eliciting and integrating the individual experience of mental health conditions as a common denominator. In this position paper, we describe the diagnostic process’s current challenges and argue why insights from the design research paradigm represent an opportunity for innovation. Based on literature, we have formulated the following challenges:
Balancing the asymmetrical interaction
There is a need to change the balance of power between patients and professionals in contemporary mental health care (Thornicroft Citation2022). For example, the diagnostic process mainly relies on information people with mental health conditions provide, conditioned by diagnostic methods, such as interviews, observations, questionnaires, and tests. While this seems appropriate from a professional’s point of view, these methods can result in asymmetry in interaction. Although asymmetry in interaction is common in health professional-patient relationships (Robinson Citation2003), the therapeutic alliance is pivotal in mental health care (Goldsmith et al. Citation2015). Interactions that rely too much on the professional can shape the individuals’ complaints and affect how they explain their illness and whether the professional adequately hears the individual experience of distress and suffering (Heritage and Maynard Citation2006). From the perspective of people with mental health conditions, the expectation may arise that they mainly need to present their complaints and therefore not speak about other aspects of their life (e.g. habits, interests, talents, wishes). At the same time, empirical evidence shows that focussing on strengths can promote recovery (Leamy et al. Citation2011).
Shifting the focus on diagnostic categories
The focus on diagnostic categories can obscure the individual experience of mental health conditions (Allsopp et al. Citation2019), and can result in stigma (Ben-Zeev, Young, and Corrigan Citation2010) and epistemic injustice (Crichton, Carel, and Kidd Citation2017). This is not desirable because it is known that groups identified by a common label have little in common. For example, it has been shown that patients with a diagnosis of depression or schizophrenia display extensive levels of heterogeneity in terms of psychopathology, need for care, treatment response, illness course, cognitive vulnerabilities, environmental exposures, and biological correlates – so extensive that it becomes implausible that these labels can provide much clinical utility (van Os Citation2010; van Os et al. Citation2021). In the DSM-5, two people could receive the same diagnosis without sharing any common symptoms, thus having different care needs (Olbert, Gala, and Tupler Citation2014).
The integration of empirical evidence of recovery
Empirical evidence of recovery shows that recovery is best judged by the person living with the experience (Slade and Longden Citation2015), and therefore there is a need to co-create novel concepts and language with people with lived experience (van Os and Guloksuz Citation2022). Individuals with mental health conditions often refer to recovery as a personal transformative journey (Deegan Citation1996; Piat and Lal Citation2012). From this perspective, an individual’s experience of a mental health condition is essential for a diagnosis. Eliciting individual experiences requires personalized diagnostics that allow for recognition of this experience and values as a more effective way of understanding mental health conditions (Allsopp et al. Citation2019).
Design for innovation in psychiatry
A design perspective may provide potential solutions for these challenges. A growing number of projects apply design and design research in different areas of mental health care. Design input ranges from improving mental health care for young people through design (Nakarada-Kordic et al. Citation2017; Johansson, Vink, and Wetter-Edman Citation2017; Scholten and Granic Citation2019) to the (co-)design of psychiatric facilities (Sumartojo et al. Citation2020; Majd, Golembiewski, and Tarkashvand Citation2020; Liddicoat Citation2019); the design of virtual reality therapies for people with autism (Adams et al. Citation2022; Terlouw et al. Citation2020; Terlouw et al. Citation2021) and psychosis (Knight et al. Citation2021); the design of a recovery program (Sanin, Spong, and McRae Citation2021); and even an attempt at redesigning psychiatry (Dorst Citation2019). These examples represent the need to explore different ways of conceptualizing mental health conditions (Dean Citation2017; Gardner and Kleinman Citation2019; van Os et al. Citation2019; Braslow, Brekke, and Levenson Citation2021; Scull Citation2021; Leichsenring et al. Citation2022). This need is strengthened by the demand for transformation in mental health care (WHO Citation2022). However, the exploration of how diagnosis can benefit from design remains underexposed, while design and design research, in our view, offers many possibilities for innovation in this specific area.
The potential of exploring design research in the diagnostic process
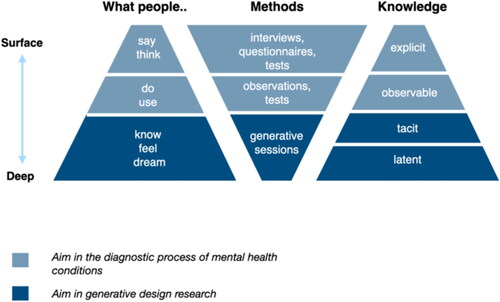
For innovation in psychiatry, design research is complementary to traditional medical health research because it follows an iterative cycle instead of a linear path (Roberts et al. Citation2016), and devises courses of action aimed at changing existing situations into preferred ones (Simon Citation1996). In this way, design research can address the unmet needs of people by describing solutions that would otherwise be difficult to imagine (Schön Citation2016). As opposed to the diagnostic process of mental health conditions, it is, from the perspective of design research, not sufficient to only examine and analyse what people say/think/do/use if the aim is to gain a deeper, more comprehensive understanding of their individual experience and needs. From this perspective, it seems a valid question whether an individual can be ‘known thoroughly’ if the diagnosis is merely based on methods such as interviews, observations, tests, and questionnaires. This does not imply that methods such as questionnaires have little use in the diagnostic process, as they can alert professionals to the presence of mental health conditions but ultimately it does not give an appraisal of the person’s individual experience (Vanheule Citation2017) and tacit knowledge. To map the individual experience and incorporate tacit knowledge in the design process, designers use generative sessions in addition to standard diagnostic methods (), as design research builds on the hypothesis that a large part of how people think, feel, and act is determined unconsciously (Sleeswijk Visser et al. Citation2005; Sanders Citation2010; Stappers and Sanders Citation2004).
Figure 1. Categorizing aims and methods from the diagnostic process of mental health conditions and generative design research, adapted from Sanders and Stappers (Citation2012).Footnote1.
Generative sessions and creative expression in psychiatry
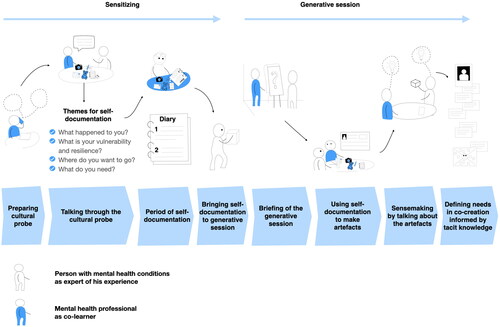
A generative session is a meeting in which individuals express their thoughts, feelings, and ideas through creative exercises. In design, participants are prepared for a generative session through a cultural probe – a technique designers deploy to collect inspirational (self-documentation) data about participants’ lives, values, and thoughts (Sanders and Stappers Citation2012). Generative sessions are not only focussed on the mind; the body is also active – participants are thinking to make and making to think. Creative expression is not new in psychiatry and mental health care. For example, Creative Arts Therapies are well-known therapies that use the creative and expressive process of art-making to improve and enhance individuals’ psychological and social wellbeing (Shafir et al. Citation2020). However, Creative Arts Therapies traditionally focus on the creative-expressive process as a form of therapy, while the generative sessions in this position paper are meant to make tacit knowledge tangible to inform the diagnostic process for the benefit of subsequent therapy. Both can potentially complement each other but are not interchangeable in practice.
People as experts of their own experience: explicit, observable, and tacit knowledge
In generative sessions, people are positioned as the experts of their own experience, as designers believe perceptions of experience are essential to understand people (Sanders and Stappers Citation2016). These experiences are seen as tacit knowledge: knowledge that is not explicit and therefore difficult to articulate (Polanyi Citation1966). In his book The Tacit Dimension, Polanyi (Citation1966) wrote: ‘I shall reconsider human knowledge by starting from the fact that we can know more than we can tell.’ We argue that the same goes for people and their mental health: individuals have a deeper understanding of their mental health than they can tell. In the case of mental health conditions, tacit knowledge could refer to latent attitudes, behaviours, habits, wishes, rituals, and beliefs that affect the individual experience of mental health and are difficult to make explicit. For example, if an individual with mental health conditions knows he has trouble sleeping due to persistent anxiety, it can be seen as explicit knowledge; it can be written down, transmitted, and understood by a professional. The individual can also communicate his symptoms and information on the duration, frequency, and intensity of these symptoms. Moreover, having trouble sleeping can easily be measured and monitored, which makes it observable knowledge. It can also be observed if the individual appears anxious or may have difficulty with daily tasks or social interactions.
In contrast, the individual’s ability to cope with personal anxiety experiences in daily life – which is highly contextual, intuitive, and subjective – requires all kinds of knowledge that is internalized. The ability to cope – the tacit knowledge – consists of underlying mechanisms such as disabling and sustaining factors, triggers, and even strengths that enable the individual to get through the day and manage the symptoms, which could provide potential starting points for recovery. However, this knowledge is developed through personal experience and is difficult to tell or observe. Sharing individual experience, even on an explicit level, can be impeded by various vulnerabilities, such as low literacy and intellectual disability, which are prevalent in the mental health care population. Therefore, generative sessions provide opportunities for innovation: in these sessions, individuals can express themselves differently. From a design perspective, individuals can co-create and talk about artefacts (i.e. objects made by human beings). This activity can provide profound insights into an individual’s narrative, contextual strengths, needs, and goals, which can inform the diagnosis ().
Figure 2. Visualization of the potential process of sensitizing and generative sessions in the diagnostic process of mental health conditionsFootnote2.
Underestimating the capacity for productive collaboration
Although patients with severe mental health conditions have temporary reductions in the mental capacity required for partaking in generative sessions – over the life course, this is only a limited part of their experience and for many patients their capacity for productive collaboration is underestimated in medical environments. Nakarada-Kordic et al. (Citation2017) aptly describe in their paper on co-design and psychosis that frequent stigma, misrepresentation and bias relating to psychosis could have easily led them to believe that the most challenging aspect of engaging with this group would be their state of mental health, while in the workshops it became clear that their unique interests and needs presented a far more significant challenge. Also, in recovery colleges – run by people with lived experience – many individuals show growth in their capacity for co-creation as required for generative sessions. That people have the capacity for co-creation, even when suffering from lasting unpleasant experiences that impact mental health, has been shown in a design research study on loneliness. In a generative session, participants who experienced loneliness and had difficulty expressing their needs made artefacts to elicit their individual experiences of loneliness. Making and talking through the artefacts showed that the unicity of each participant’s individual experience could only be met by co-designing tailored interventions beyond the definition (or label) of loneliness (Veldmeijer et al. Citation2020).
Towards the use of generative sessions in the diagnostic process in psychiatry
In this section, we will argue why generative sessions are an answer to the three challenges described earlier in this paper.
Balancing the asymmetrical interaction
We have argued that the asymmetrical interaction between the professional and patient in the diagnostic process needs to be balanced. It has been proposed that in the moral era of medicine, there is a need for a different relationship between professional and patient, in which the patient is seen as equal (Berwick Citation2016; Groenewoud, Westert, and Kremer Citation2019; Brouwers, van Gestel-Timmermans, and van Nieuwenhuizen Citation2013). In generative sessions, people with mental health conditions can be guided in small steps towards discovering, constructing, and expressing implicit levels of knowledge (Sleeswijk Visser et al. Citation2005), co-developed with the professional. Explaining the artefact embodies valuable information (Sleeswijk Visser et al. Citation2005; Stappers and Sanders Citation2004), which can be achieved through storytelling (Terken, Buskermolen, and Eggen Citation2015). Storytelling techniques collectively build empathy and understanding for the expression of tacit knowledge (van Rijn et al. Citation2011). Talking about artefacts in the diagnostic process could be beneficial, as it has been suggested that important clues for recovery support can be found in people’s narrated struggles (van Sambeek et al. Citation2021). From a socio-technical perspective, artefacts as boundary objects can promote dialogue and mutual understanding between stakeholders (Kuipers Citation2019), such as patients and professionals. They can help manifest different perspectives through perspective-making and -taking, providing insights into someone’s life, social context, and personal goals (Terlouw et al. Citation2022). Conversations around artefacts may provide a shift in the power balance towards a more reciprocal dynamic in interaction, letting individuals with mental health conditions steer the dialogue into the area of their individual experience.
Shifting the focus on diagnostic categories
We have suggested that the focus on diagnostic categories needs to be shifted. The profound needs that are collected through generative sessions can shift the focus from diagnostic categories to individual experience and personal variation. This can provide an alternative explanation for people who do not feel their mental health experience is validated by diagnostic categories. For instance, generative sessions can help explore multiple perspectives on the personal experiences of a psychotic episode. It has been shown that delusional experiences may sometimes refer to higher-order personal dynamics and enduring meaning, which may not be fully captured by a strictly medical perspective (Feyaerts et al. Citation2021). In addition, studies show an association between creativity on the one hand and both bipolar disorder and schizotypy on the other (Thys, Sabbe, and De Hert Citation2014). It raises the question of why creativity is commonly neglected in the diagnostic process. For some people, it could be an authentic way of expressing themselves and help to find meaning and significance (Kapoor and Kaufman Citation2020). For example, studies show that design activity could be therapeutic for some people with psychosis (Illarregi et al. Citation2022) and can help draw out their unique experiences and perspectives (Nakarada-Kordic et al. Citation2017). This shows that design activity, as co-developed in generative sessions, holds the potential to holistically stimulate perceptions of people with mental health conditions, as recommended for mental health practice and research (Gardner and Kleinman Citation2019; Borsboom, Cramer, and Kalis Citation2018). A holistic perspective can address the dynamic interaction of different elements (Federoff and Gostin Citation2009) and fits the concept of positive health (Huber et al. Citation2011), positive psychology (Seligman and Csikszentmihalyi Citation2000), positive psychiatry (Jeste et al. Citation2015), and evidence-based practice (Rycroft-Malone et al. Citation2004). The professional can play an active role by preparing these sessions and giving meaning to the findings in co-creation with the person with mental health conditions to form a diagnosis that comprises individual experience and personal variation.
The integration of empirical evidence of recovery
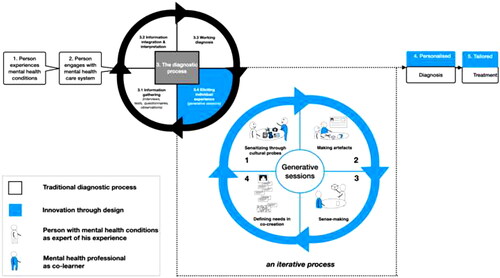
We reasoned that innovation starts with the integration of empirical evidence of recovery. In line with empirical evidence of recovery (Leamy et al. Citation2011; Slade and Longden Citation2015; van Os and Guloksuz Citation2022), the Lancet Commission report on Stigma and Discrimination (Thornicroft et al. Citation2022) emphasized once again that the view of ‘nothing about us without us’ is only possible through engaging people with lived experience. The integration of generative sessions in the diagnostic process corresponds to those needs. As the aim in the moral era of medicine should be to add value to the lives of patients (Berwick Citation2016), it seems worthwhile to explore if generative sessions in the diagnostic process make people with mental health conditions feel empowered in the diagnostic process. Sanin, Spong, and McRae (Citation2021) already showed that participation in creative activities can generate feelings of empowerment and can contribute to recovery in the broader context of mental health. Empowerment in personal recovery is linked to the ability of individuals to discover, develop, build, and learn to use their strengths effectively (Boevink Citation2009). In generative sessions, insights can be gained into the contexts in which a person has strengths and the contexts in which the problems manifest themselves more. With these insights, multiple perspectives can be explored, ultimately leading to the necessary actions for recovery, which is deeply personal (Anthony Citation1993). From a design perspective, the diagnostic process should be iterative, moving along with the dynamics of the individual experience of mental health conditions. In this process, the professional can position himself as a co-learner by entering a shared transformative journey in which the right actions to achieve recovery are learned together (Boumans Citation2015) ().
Figure 3. How design research can potentially strengthen the diagnostic process of mental health conditions.Footnote3.
Future research
In this position paper, we illustrated how insights from the design research paradigm, in particular generative sessions, can stimulate the suggested incremental and iterative advancements in diagnostic systems (Stein et al. Citation2022). For future research, several directions can be explored, including traditional mental health professionals, people with mental health conditions, and people with lived experience. First, the application of design research methods in mental health care needs to be reviewed. A second direction for future research is reviewing the evidence from the diagnostic process and personal recovery. Together, these directions can provide working factors that could be integrated into the design rationale of the generative session’s concept. This concept needs to be co-designed, tested and studied to explore for which target group generative sessions are most suitable. When the concept has been tested, the effect of the concept on the relationship between the patient and the professional should be examined, and the user experience should be mapped. Most importantly, it should be investigated whether people with mental health conditions feel their care needs have been answered instead of measuring the quality of care by the remission of symptoms.
Conclusion
In this position paper, we have discussed and visualized the potential added value of generative sessions to the diagnostic process of mental health conditions. We have outlined three challenges in the diagnostic process where generative sessions can be an opportunity for innovation. We have suggested that generative sessions can help initiate reciprocal conversations about individual experience, can assist in shifting the focus from diagnostic categories to personal variation, and can support the integration of empirical evidence of recovery. Therefore, we have argued that exploring generative sessions in the diagnostic process can stimulate incremental and iterative advancements in diagnostic systems. We have recommended several directions for further research in co-creation with traditional mental health professionals, people with mental health conditions, and people with lived experience.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Notes on contributors
Lars Veldmeijer
Lars Veldmeijer is PhD-candidate at Utrecht University Medical Centre and researcher and lecturer at the NHL Stenden University of Applied Sciences. For his PhD, he combines his lived experience in mental health care with his expertise of design for health. His main research topic is exploring the potential of design research and co-creation for the diagnostic process of mental health conditions. Mail: [email protected] and [email protected]
Gijs Terlouw
Gijs Terlouw is senior researcher and lecturer at the NHL Stenden University of Applied Sciences at the academy of healthcare. His dissertation researched the role of boundary objects in design and health innovation.
Job van ‘t Veer
Job van ‘t Veer is Professor of Digital Innovation in Healthcare. In his research projects, the emphasis is always on a design-based approach: improving care and support in an innovative way, in co-creation with clients, patients, residents and professionals. Both the design of digital tools and the implementation of these innovations has his attention.
Jim van Os
Jim van Os is Professor of Psychiatry and Chair of the Division Neuroscience at Utrecht University Medical Centre and Visiting Professor at the Institute of Psychiatry at King’s College London. He works at the interface of critical neuroscience, public health and mental health service reform in co-creation with people with 'lived experience’ in mental health care.
Nynke Boonstra
Nynke Boonstra is Professor of Nursing in Mental Health at Utrecht University Medical Centre and Professor of Care and Innovation in Psychiatry at NHL Stenden University of Applied Sciences. She also works at KieN Early Intervention Service in Leeuwarden, the Netherlands. Her main research interests surround themes such as personal recovery, the professional-patient relationship, resilience, and diagnosis from a holistic perspective.
Notes
1 The original figure (Sanders and Stappers Citation2012) linked methods to different levels of knowledge in design research. We have adapted this model by adding the methods used in the diagnostic process of mental health conditions and thereby providing insight into why the use of generative sessions can be beneficial in gaining a complete picture of a person's experience and knowledge of mental health conditions, as the figure shows tacit and latent knowledge is not addressed by the traditional methods.
2 This framework comprised the central components of context mapping (Sleeswijk Visser et al. Citation2005) and redesigned these components to fit the needs of mental health care based on the academic literature.
3 This framework visualises the novel concept of generative sessions in the diagnostic process of mental health conditions. Future research with people with lived experience and traditional mental health professionals should inform the exact operationalisation and effects of generative sessions in clinical practice and determine if they should have a place in the diagnostic process.
References
- Adams, L., E. Simonoff, K. Tierney, M. J. Hollocks, A. Brewster, J. Watson, and L. Valmaggia. 2022. “Developing a User-Informed Intervention Study of a Virtual Reality Therapy for Social Anxiety in Autistic Adolescents.” Design for Health 6: 114–133. doi:10.1080/24735132.2022.2062151.
- Allsopp, K., J. Read, R. Corcoran, and P. Kinderman. 2019. “Heterogeneity in Psychiatric Diagnostic Classification.” Psychiatry research 279 (September 1): 15–22. doi:10.1016/j.psychres.2019.07.005.
- American Psychiatric Association 2013. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington: American Psychiatric Association.
- Anthony, W. A. 1993. “Recovery from Mental Illness: The Guiding Vision of the Mental Health Service System in the 1990s.” Psychosocial Rehabilitation Journal 16 (4): 11–23. doi:10.1037/h0095655.
- Barelds, D. P. H, and F. Luteijn. 2019. Psychological Diagnostics in Health Care. Amsterdam: Boom.
- Ben-Zeev, D., A. M. Young, and P. W. Corrigan. 2010. “DSM-V and the Stigma of Mental Illness.” Journal of Mental Health 19 (4): 318–327. doi:10.3109/09638237.2010.492484.
- Berwick, D. M. 2016. “Era 3 for Medicine and Health Care.” JAMA 315 (13), 1329–1330. doi:10.1001/jama.2016.1509.
- Boevink, W. A. 2006. “From Being a Disorder to Dealing with Life: An Experiential Exploration of the Association between Trauma and Psychosis.” Schizophrenia bulletin 32 (1): 17–19. doi:10.1093/schbul/sbi068.
- Boevink, W. A. 2009. “Lijfsbehoud, Levenskunst en Lessen om Van te Leren [Body Preservation, Art of Living and Lessons to Be Learnt].” In HEE-Gesch(r)Ift), 1–86. Utrecht: Trimbos-instituut. ISBN/EAN: 978-90-5253-639-2
- Borsboom, D., A. O. J. Cramer, and A. Kalis. 2018. “Brain Disorders? Not Really: Why Network Structures Block Reductionism in Psychopathology Research.” The Behavioral and Brain Sciences 42 (January 24): e2. doi:10.1017/S0140525X17002266.
- Borsboom, D., Jonas M. B. Haslbeck, and Donald J. Robinaugh. 2022. “Systems-Based Approaches to Mental Disorders Are the Only Game in Town.” World psychiatry : official Journal of the World Psychiatric Association 21 (3): 420–422. doi:10.1002/wps.21004.
- Boumans, J. 2015. “Naar het Hart Van Empowerement: Een Onderzoek Naar de Grondslagen Van Empowerement Van Kwetsbare Groepen. Deel II: Over de Vraag Wat Werkt [to the Heart of Empowerment: An Examination of the Foundations of Empowerment of Vulnerable Groups.” In Part II: On the Question of What Works], 64–71. Utrecht: Movisie. ISBN: 978-90-8869-118-8
- Braslow, J. T., J. S. Brekke, and J. Levenson. 2021. “Psychiatry’s Myopia—Reclaiming the Social, Cultural, and Psychological in the Psychiatric Gaze.” JAMA Psychiatry 78 (4): 349–350.
- Brouwers, E. P. M., J. A. W. M. van Gestel-Timmermans, and C. van Nieuwenhuizen. 2013. “Herstelgerichte zorg in Nederland: modegril of Daadwerkelijke Verandering? [Recovery-Oriented Care in The Netherlands: fad or Real Change?”] Psychopraktijk 4: 14–17.
- Bruyn, E. E. J., A. J. J. Ruijssenaars, N. Pameijer, and E. J. M. Aarle. 2003. De diagnostische Cyclus: een Praktijkleer [The diagnostic cycle: a practical theory]. Leuven: Acco uitgeverij.
- Crichton, P., H. Carel, and I. J. Kidd. 2017. “Epistemic Injustice in Psychiatry.” BJPsych bulletin 41 (2): 65–70. doi:10.1192/pb.bp.115.050682.
- Davidson, L. 2016. “The Recovery Movement: Implications for Mental Health Care and Enabling People to Participate Fully in Life.” Health affairs (Project Hope) 35 (6): 1091–1097. doi:10.1377/hlthaff.2016.0153.
- de Graaf, R., M. L. Have, and S. van Dorsselaer. 2010. “De psychische Gezondheid Van de Nederlandse Bevolking: NEMESIS-2: opzet en Eerste Resultaten.” “[The Mental Health of the Dutch Population: NEMESIS-2: design and First Results].” Utrecht: Trimbos-instituut.
- Dean, C. E. 2017. “Social Inequality, Scientific Inequality, and the Future of Mental Illness.” Philosophy, Ethics, and Humanities in Medicine: PEHM 12 (1 (December 19): 1–12. 10.1186/s13010-017-0052-x
- Deegan, P. 1996. “Recovery as a Journey of the Heart.” Psychiatric Rehabilitation Journal 19 (3): 91–97. doi:10.1037/h0101301.
- Dixon, L. B., Y. Holoshitz, and I. Nossel. 2016. “Treatment engagement of Individuals Experiencing Mental Illness: Review and Update.” World psychiatry : official Journal of the World Psychiatric Association 15 (1): 13–20. doi:10.1002/wps.20306.
- Dorst, K. 2019. “Design beyond Design.” She Ji: The Journal of Design, Economics, and Innovation 5 (2 (June 1): 117–127. doi:10.1016/j.sheji.2019.05.001.
- DSM-5 Zinvol Ingezet Kan Worden Voor Het Vak [Separating Diagnosis and Classification in Psychiatry. How the DSM-5 Can Be Meaningfully Applied to the Profession].” Tijdschrift voor Psychiatrie 56 (8): 523–530.
- Federoff, H. J., and L. O. Gostin. 2009. “Evolving from Reductionism to Holism: Is There a Future for Systems Medicine?” JAMA 302 (9): 994–996. doi:10.1001/jama.2009.1264.
- Feyaerts, J., W. Kusters, Z. Van Duppen, S. Vanheule, I. Myin-Germeys, and L. Sass. 2021. “Uncovering the Realities of Delusional Experience in Schizophrenia: A Qualitative Phenomenological Study in Belgium.” The lancet. Psychiatry 8 (9): 784–796. doi:10.1016/S2215-0366(21)00196-6.
- Frances, A. J., and T. Widiger. 2012. “Psychiatric Diagnosis: Lessons from the DSM-IV past and Cautions for the DSM-5 Future.” Annual review of Clinical Psychology 8: 109–130. doi:10.1146/annurev-clinpsy-032511-143102.
- Gardner, C., and A. Kleinman. 2019. “Medicine and the Mind — the Consequences of Psychiatry’s Identity Crisis.” The New England Journal of Medicine 381 (18): 1697–1699. doi:10.1056/NEJMp1910603.
- Goldsmith, L. P., S. W. Lewis, G. Dunn, and R. P. Bentall. 2015. “Psychological Treatments for Early Psychosis Can Be Beneficial or Harmful, Depending on the Therapeutic Alliance: An Instrumental Variable Analysis.” Psychological medicine 45 (11): 2365–2373. doi:10.1017/S003329171500032X.
- Groenewoud, A. S., G. P. Westert, and J. A. M. Kremer. 2019. “Value Based Competition in Health Care’s Ethical Drawbacks and the Need for a Values-Driven Approach.” BMC Health Services Research 19, 256. doi:10.1186/s12913-019-4081-6.
- Guloksuz, S., and J. van Os. 2018. “The Slow Death of the Concept of Schizophrenia and the Painful Birth of the Psychosis Spectrum.” Psychological medicine 48 (2): 229–244. doi:10.1017/S0033291717001775.
- Heritage, J., and D. W. Maynard. 2006. Communication in Medical Care: Interaction between Primary Care Physicians and Patients. Cambridge: Cambridge University Press.
- Huber, Machteld, J. André Knottnerus, Lawrence Green, Henriëtte van der Horst, Alejandro R. Jadad, Daan Kromhout, Brian Leonard, et al. 2011. “How should we Define Health?” BMJ (Clinical Research ed.) 343: d4163. doi:10.1136/bmj.d4163.
- Illarregi, E. R., K. Alexiou, G. DiMalta, and T. Zamenopoulos. 2022. “Is designing Therapeutic? A Case Study Exploring the Experience of co-Design and Psychosis.” Psychosis. doi:10.1080/17522439.2022.2052450.
- Jeste, D. V., B. W. Palmer, D. C. Rettew, and S. Boardman. 2015. “Positive Psychiatry.” The Journal of Clinical Psychiatry 76 (6): 675–683. doi:10.4088/jcp.14nr09599.
- Johansson, L. S., J. Vink, and K. Wetter-Edman. 2017. “A Trojan Horse Approach to Changing Mental Health Care for Young People through Service Design.” Design for Health 1, 245–255. doi:10.1080/24735132.2017.1387408.
- Kapoor, H., and J. C. Kaufman. 2020. “Meaning-Making through Creativity during COVID-19.” Frontiers in Psychology 11, 595990. doi:10.3389/fpsyg.2020.595990.
- Knight, I., J. West, E. Matthews, T. Kabir, S. Lambe, F. Waite, and D. Freeman. 2021. “Participatory Design to Create a VR Therapy for Psychosis.” Design for Health 5, 119 http://dx.doi.org/10.1080/24735132.2021.1885889.
- Kuipers, D. 2019. Design for Transfer: Figural Transfer through Metaphorical Recontextualization in Games for Health. Rijksuniversiteit Groningen, Groningen.
- Leamy, M., V. Bird, C. Le Boutillier, J. Williams, and M. Slade. 2011. “Conceptual Framework for Personal Recovery in Mental Health: Systematic Review and Narrative Synthesis.” The British Journal of Psychiatry : The Journal of Mental Science 199 (6): 445–452. doi:10.1192/bjp.bp.110.083733.
- Leichsenring, F., C. Steinert, S. Rabung, and J. P. A. Ioannidis. 2022. “The Efficacy of Psychotherapies and Pharmacotherapies for Mental Disorders in Adults: An Umbrella Review and Meta-Analytic Evaluation of Recent Meta-Analyses.” World psychiatry : official Journal of the World Psychiatric Association (WPA) 21 (1): 133–145. doi:10.1002/wps.20941.
- Liddicoat, S. 2019. “Mental Health Facility Codesign: A New Research Method for Integrating the Service User Voice in Design Processes Using Virtual Reality.” General psychiatry 32 (3): e100061. doi:10.1136/gpsych-2019-100061.
- Majd, N. F., J. Golembiewski, and A. Tarkashvand. 2020. “The Psychiatric Facility: How Patients with Schizophrenia Respond to Place.” Design for Health 4 (3): 384–406. doi:10.1080/24735132.2020.1846849.
- Menninger, K., H. Ellenberger, P. Pruyser, and M. Mayman. 1958. “The Unitary Concept of Mental Illness.” Bulletin of the Menninger Clinic 22 (1): 4–12. doi:10.1007/BF01741038.
- Nakarada-Kordic, I., N. Hayes, S. D. Reay, C. Corbet, and A. Chan. 2017. “Co-Designing for Mental Health: Creative Methods to Engage Young People Experiencing Psychosis.” Design for Health 1, 229–244. doi:10.1080/24735132.2017.1386954.
- Olbert, C. M., G. J. Gala, and L. A. Tupler. 2014. “Quantifying Heterogeneity Attributable to Polythetic Diagnostic Criteria: Theoretical Framework and Empirical Application.” Journal of Abnormal Psychology 123 (2): 452–462. doi:10.1037/a0036068.
- Piat, M., and S. Lal. 2012. “Service providers’ Experiences and Perspectives on Recovery-Oriented Mental Health System Reform.” Psychiatric rehabilitation Journal 35 (4): 289–296. doi:10.2975/35.4.2012.289.296.
- Pies, R. 2012. “Bereavement, Complicated Grief, and the Rationale for Diagnosis in Psychiatry.” Dialogues in Clinical Neuroscience 14 (2): 111–113. doi:10.31887/DCNS.2012.14.2/rpies.
- Polanyi, M. 1966. The Tacit Dimension. London: Routledge & Kegan Paul.
- Roberts, Jess P., Thomas R. Fisher, Matthew J. Trowbridge, and Christine Bent. 2016. “A Design Thinking Framework for Healthcare Management and Innovation.” Healthcare 4 (1): 11–14. doi:10.1016/j.hjdsi.2015.12.002.
- Robinson, J. D. 2003. “An Interactional Structure of Medical Activities during Acute Visits and Its Implications for Patients’ Participation.” Health communication 15 (1): 27–57. doi:10.1207/S15327027HC1501_2.
- Ruissen, A. M. 2014. “Diagnostiek en Classificatie Scheiden in de Psychiatrie. Hoe de Rycroft-Malone.”
- Rycroft-Malone, J., K. Seers, A. Titchen, G. Harvey, A. Kitson and B. McCormack 2004. “What Counts as Evidence in Evidence-Based Practice?” Journal of Advanced Nursing 47 (1): 81–90.
- Sanders, E. B.-N, and P. J. Stappers. 2012. Convivial design Toolbox: Generative Research for the Front End of Design. Amsterdam; Enfield: BIS; Publishers Group UK [distributor].
- Sanders, E. B.-N, and P. J. Stappers. 2016. “Co-Creation and the New Landscapes of Design.” Design: Critical and Primary Sources. 4, 5–18. doi:10.5040/9781474282932.0011.
- Sanders, E. B.-N. 2010. “Converging Perspectives: Product Development Research for the 1990s.” Design Management Journal (Former Series) 3 (4): 49–54 doi:10.1111/j.1948-7169.1992.tb00604.x.
- Sanin, J., L. Spong, and C. McRae. 2021. “Creative Wellbeing. Prototyping an Arts-Health Practice Program for Mental Health Recovery.” Design for Health 5, 61–81. doi:10.1080/24735132.2021.1927504.
- Scholten, H., and I. Granic. 2019. “Use of the Principles of Design Thinking to Address Limitations of Digital Mental Health Interventions for Youth: Viewpoint.” Journal of Medical Internet Research 21 (1): e11528. doi:10.2196/11528.
- Schön, D. A. 2016. “Designing: Rules, Types and Worlds.” Design: Critical and Primary Sources 9, 181–190. doi:10.5040/9781474282932.0016.
- Scull, A. 2021. “American Psychiatry in the New Millennium: A Critical Appraisal.” Psychological medicine 51 (16): 2762–2770. doi:10.1017/S0033291721001975.
- Seligman, M. E., and P. M. Csikszentmihalyi. 2000. “Positive psychology: An Introduction.” The American Psychologist 55 (1): 5–14. doi:10.1037/0003-066x.55.1.5.
- Shafir, T., H. Orkibi, F. A. Baker, D. Gussak, and G. Kaimal. 2020. “Editorial: The State of the Art in Creative Arts Therapies.” Frontiers in Psychology 11: 68. doi:10.3389/fpsyg.2020.00068.
- Simon, H. A. 1996. The Sciences of the Artificial. Cambridge: Mit Press.
- Slade, M., and E. Longden. 2015. “Empirical Evidence about Recovery and Mental Health.” BMC Psychiatry 15 (1): 1–14. doi:10.1186/s12888-015-0678-4.
- Sleeswijk Visser, F. S., P. J. Stappers, R. van der Lugt, and E. B.-N. Sanders. 2005. “Contextmapping: Experiences from Practice.” CoDesign 1: 119–149 http://dx.doi.org/10.1080/15710880500135987.
- Stappers, P., and E. Sanders. 2004. “Generative Tools for Context Mapping: Tuning the Tools.” In Design and emotion, : the experience of everyday things: Proceedings of the 3rd International Conference on Design and Emotion. edited by Deana McDonagh, Paul Hekkert, Jeroen van Erp, Diane Gyi, 77–81. Taylor and Francis.
- Stein, D. J., S. J. Shoptaw, D. V. Vigo, C. Lund, P. Cuijpers, J. Bantjes, N. Sartorius, and M. Maj. 2022. “Psychiatric Diagnosis and Treatment in the 21st Century: Paradigm Shifts versus Incremental Integration.” World Psychiatry: Official Journal of the World Psychiatric Association 21 (3): 393–414.
- Stoyanov, D., P. K. Machamer, K. F. Schaffner, and R. Rivera-Hernández. 2012. “The Challenge of Psychiatric Nosology and Diagnosis.” Journal of Evaluation in Clinical Practice 18 (3): 704–709. doi:10.1111/j.1365-2753.2012.01844.x.
- Sumartojo, S., S. Pink, M. Duque, and L. Vaughan. 2020. “Atmospheres of Care in a Psychiatric Inpatient Unit.” Design for Health 4, 24–42. doi:10.1080/24735132.2020.1730068.
- Terken, J., D. O. Buskermolen, and B. Eggen. 2015. “The Co-Constructing Stories Method: Feedback of Designers on Use of the Method in Real Design Cases.” The International Journal of Design Management and Professional Practice 8 (2): 17–28. doi:10.18848/2325-162X/CGP/v08i02/38623.
- Terlouw, G., D. Kuipers, L. Veldmeijer, J. van ’t Veer, J. Prins, and J.-P. Pierie. 2022. “Boundary Objects as Dialogical Learning Accelerators for Social Change in Design for Health: Systematic Review.” JMIR Human Factors 9 (1): e31167. doi:10.2196/31167.
- Terlouw, Gijs, Derek Kuipers, Job van 't Veer, Jelle T. Prins, and Jean Pierre E. N. Pierie. 2021. “The Development of an Escape Room-Based Serious Game to Trigger Social Interaction and Communication between High-Functioning Children with Autism and Their Peers: Iterative Design Approach.” JMIR serious Games 9 (1): e19765. doi:10.2196/19765.
- Terlouw, Gijs, Job Tb van 't Veer, Jelle T. Prins, Derek A. Kuipers, and Jean-Pierre E. N. Pierie. 2020. “Design of a Digital Comic Creator (It’s Me) to Facilitate Social Skills Training for Children with Autism Spectrum Disorder: Design Research Approach.” JMIR mental Health 7 (7): e17260. doi:10.2196/17260.
- The Government Office for Science. 2008. Foresight Mental Capital and Wellbeing Project. Final Project Report. London: The Government Office for Science. Accessed October 24 2022. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/292453/mental-capital-wellbeing-summary.pdf
- Thornicroft, G. 2022. “Psychiatric Diagnosis and Treatment in the 21st Century: Paradigm Shifts or Power Shifts?” World Psychiatry.” Official Journal of the World Psychiatric Association 21 (3): 334–335.
- Thornicroft, G., C. Sunkel, A. Alikhon Aliev, S. Baker, E. Brohan, R. el Chammay, K. Davies, et al. 2022. “The Lancet Commission on Ending Stigma and Discrimination in Mental Health.” Lancet 400 (10361): 1438–1480. doi:10.1016/S0140-6736(22)01470-2.
- Thys, E., B. Sabbe, and M. De Hert. 2014. “Creativity and Psychopathology: A Systematic Review.” Psychopathology 47 (3): 141–147.
- van Os, J. 2010. “Are Psychiatric Diagnoses of Psychosis Scientific and Useful? The Case of Schizophrenia.” Journal of Mental Health 19 (4): 305–317. doi:10.3109/09638237.2010.492417.
- van Os, J., and S. Guloksuz. 2022. “Schizophrenia as a Symptom of Psychiatry’s Reluctance to Enter the Moral Era of Medicine.” Schizophrenia Research 242: 138–140. doi:10.1016/j.schres.2021.12.017.
- van Os, J., L.-K. Pries, M. ten Have, R. de Graaf, S. van Dorsselaer, M. Bak, G. Kenis, et al. 2021. “Context v. Algorithm: Evidence That a Transdiagnostic Framework of Contextual Clinical Characterization is of More Clinical Value than Categorical Diagnosis.” Psychological Medicine, Firstview, 1–9. doi:10.1017/S0033291721003445.
- van Os, J., P. Delespaul, J. Wigman, I. Myin-Germeys, and M. Wichers. 2013. “Psychiatry beyond Labels: Introducing Contextual Precision Diagnosis across Stages of Psychopathology.” Psychological medicine 43 (7): 1563–1567. doi:10.1017/S0033291713000937.
- van Os, J., S. Guloksuz, T. W. Vijn, A. Hafkenscheid, and P. Delespaul. 2019. “The Evidence-Based Group-Level Symptom-Reduction Model as the Organizing Principle for Mental Health Care: Time for Change?” World psychiatry : official Journal of the World Psychiatric Association 18 (1): 88–96. doi:10.1002/wps.20609.
- van Rijn, H., F. S. Visser, P. J. Stappers, and A. D. Özakar. 2011. “Achieving Empathy with Users: The Effects of Different Sources of Information.” CoDesign 7, 65–77. doi:10.1080/15710882.2011.609889.
- van Sambeek, N., A. Baart, G. Franssen, S. van Geelen, and F. Scheepers. 2021. “Recovering Context in Psychiatry: What Contextual Analysis of Service Users’ Narratives Can Teach about Recovery Support.” Frontiers in Psychiatry 12: 773856. doi:10.3389/fpsyt.2021.773856.
- Vanheule, S. 2014. Diagnosis and the DSM: A Critical Review. Hampshire: Palgrave Macmillan. doi:10.1057/9781137404688.
- Vanheule, S. 2017. Psychiatric Diagnosis Revisited: From DSM to Clinical Case Formulation. Cham: Springer. doi:10.1007/978-3-319-44669-1_2.
- Veldmeijer, L., B. Wartena, G. Terlouw, and J. V. Veer. 2020. “Reframing Loneliness through the Design of a Virtual Reality Reminiscence Artefact for Older Adults.” Design for Health 4, 407–426. doi:10.1080/24735132.2020.1848976.
- Vollebergh, W. A. M, and C. G. Schoemaker. 2003. “Psychische stoornissen in Nederland: overzicht Van de Resultaten Van NEMESIS.” “[Mental disorders in the Netherlands overview of the results of NEMESIS].” Huisarts en Wetenschap 47, 781.
- Whitaker, R. 2010. Anatomy of an Epidemic: Magic Bullets, Psychiatric Drugs, and the Astonishing Rise of Mental Illness in America. New York City: Crown Publisher Group.
- World Health Organization 2001. World mental Health Report: Mental Disorders Affect One in Four People. Geneva: World Health Organization.
- World Health Organization 2022. World mental Health Report: Transforming Mental Health for All. Geneva: World Health Organization.

