[Abstract:0068] [Addictions]
Optimization of therapeutic tactics in patients with opioid addiction
Abdullaeva Vasila
Department of psychiatry and addiction, Tashkent Pediatric Medical Institute, Tashkent, Uzbekistan
ABSTRACT
Introduction: Treatment and rehabilitation of patients with opioid addiction is a complex medical and social problem, covering not only the restoration of normal mental status, but also the physical health of patients. In this regard, the search for effective means that can neutralize the effects of chronic drug intoxication is one of the priorities in the treatment of these patients. In recent times, more and more attention is paid to the participation pathochemical reactions in the genesis of many diseases [2]. The study of the liver in heroin addiction is extremely important, because depends on it for abstinence for neutralization and clearance of the drug is carried by the liver [3]. In the literature, there is enough information, says the activation of free radical oxidation and the presence of endogenous intoxication with heroin addiction, shows aggravation of lipid peroxidation, increase the level of nitric oxide and peroxide hemolysis of red blood cells with increasing doses of heroin, as well as the correlation between low levels of NO and low concentrations of antioxidants at prolonged narcotization [1]. Nevertheless, the association of the level of reactive oxygen species and the characteristics of the course of withdrawal symptoms, the impact of somatic pathology, have been conducted. The object of the study was to examine the pathogenetic significance of systemic oxidative stress, depending on the duration of opioid narcotization and the effectiveness of antioxidant therapy.
Methods: The study included 52 male patients aged from 18 to 55 years with clinically-defined the drug addiction (ICD-10 — F11.2). All patients were male, average age 36.9 ± 6.7 years, experience of regular use of drugs from 1 year to 10 years. Patients were examined in the clinic of addiction in Tashkent. Two groups of patients were examined: the 1st group-26 patients who received complex treatment according to the conventional scheme; the 2nd group-26 patients who underwent conventional treatment in combination with antioxidants. To analyze the importance of clinical and dynamic factors in the development of opioid addiction we used clinical-psychopathological, biochemical and statistical methods. Also used clinical scale qualified assessments morbid attraction of Vinnikova (2001). To determine the intensity of lipid peroxidation to determine the level of malondialdehyde was conducted (MDA) in serum, the activity of catalase in the blood, the definition of medium molecular peptides (MMP). The control group consisted of 12 healthy men of the corresponding sex and age.
Results: The generation of reactive oxygen species is accompanied by damage to protein and lipid molecules. In the interaction of reactive oxygen species with these molecules are formed low molecular weight products with toxic effects. These products include medium-molecular peptides having a molecular weight of not more than 5000 Da. During the study we found that the total level of enzyme was higher in the study group than the control group, but is within the reference range (11–66 U/L), indicating the absence of acute or chronic liver disease. With this approach to the interpretation of the data could reveal that patients with a duration of narcotization up to 1 year has moderately severe endotoxemia — medium molecular peptides (0.063 ± 0.009*) increase 3 times and oxidative stress — malondialdehyde (1.31 ± 0.10*) increase 2.6 times due to lower activity of catalase in 1.5 times (26.9 ± 1.1*) compared with the control (malondialdehyde 0.51 ± 0.09 nmol/mg protein, medium molecular peptides 0.021 ± 0.001 AU/mg protein, catalase 40.1 ± 1.7 mmol of H2 O2 /mln. Erith*m), whereas patients with more than one year duration of narcotization the reduction of catalase activity was observed in 3.5 times — 11.6 ± 0.9** and the level of malondialdehyde — 2.61 ± 0.13** and medium molecular peptides — 0.109 ± 0.012** exceeded control in 5.0 and 5.5 times, respectively (Note: * — Significant in relation to the control, P < 0.05** — Significantly with respect to narcotization duration up to 1 year). Differences indicators, depending on the duration of narcotization in all cases were significant (Р < 0.05).
It should be noted that our results of research on the state of the antioxidant system in patients who use opioids, according to the oppression of the enzymatic link of antioxidant protection and the need to include substances with antioxidant properties, in the treatment of these patients. Relief of oxidative stress necessary to normalize membrane-destructive processes in the body, primarily in the brain and liver, will provide adequate metabolism microsomal oxidative preparations system used in treatment — antidepressants, antipsychotics, etc., optimizes post opioid detoxified, thus shortening during the withdrawal syndrome and reduce its severity.
Based on the identified pathochemical features of the course of acute and chronic drug intoxication opiates, as well as the availability of the system operating in the blood of opioid addicts, the traditional therapeutic tactics has been optimized as follows: included pathogenetic therapy with an effect on metabolic processes with the use of antioxidants, apply individual approaches appointment of psychotropic drugs in the framework of the existing treatment standards. Along with the traditional as membrane-pathogenetic therapy administered ethylmethylhydroxypyridine succinate (mexidol) at a dose of 500 mg/day for 2 admission. A comparative study of two groups of drug users receiving different treatments — traditional and optimized in combination with ethylmethylhydroxypyridine succinate (mexidol) shows a more pronounced therapeutic effect bioregularly antioxidant therapy.
As in people, long-term opiate abusers and drug addicts with experience within a 1-year-optimized therapy including antioxidants have beneficial effects more pronounced in patients subgroup with duration of narcotization over 1 year. They noted a significant decrease from baseline in MMP (0.045 ± 0.012***) and MDA (1.33 ± 0.10***), which proves that the contribution of the liver in the system OS development with opiate addiction, as well as the fact that the recovery of the antioxidant capacity of the body leads to the relief of the OS (Note: * — Significant in relation to the traditional method of treatment, P < 0.05; ** — Significantly relative to controls (P < 0.05); *** — significantly relative to the treatment (P < 0.05)).
The study period of abstinence in patients receiving optimized treatment including an antioxidant, found that significantly reduced the duration of withdrawal symptoms, reduced craving for the drug, and the low intensity of the generation of oxidative stress in the blood correlates with the effectiveness of therapy.
Discussion: Thus, the peculiarity of biochemical disorders of homeostasis in this category of patients is the development of enhanced generation of reactive oxygen species in the blood, resulting in the development of endotoxemia due to the accumulation of degradation products of macromolecules of protein and lipid nature. Probably, such an increase in the studied parameters was a consequence of the insufficiency of the protective system, including both enzymes with antiperoxide and antiradical mechanism of action, and antioxidants. Excessive formation of reactive oxygen species in abstinence initiates the process of lipid peroxidation in the blood of patients, which is confirmed by an increase in the level of MDA in plasma by 80–92% relative to the norm. Intensification of lipid peroxidation in drug addiction can lead to oxidative damage of biomolecules and cell structures. The results of the study show that in the first group of patients the dynamics of most of the studied biochemical parameters indicates the preservation of oxidative stress. The inclusion of antioxidants in the complex treatment of patients of the second group leads to the stimulation of the antioxidant system of the blood.
It should be noted that our results of research on the state of the antioxidant system in patients who use opioids, according to the oppression of the enzymatic link of antioxidant protection and the need to include substances with antioxidant properties, in the treatment of these patients. Relief of oxidative stress necessary to normalize membrane-destructive processes in the body, primarily in the brain and liver, will provide adequate metabolism microsomal oxidative preparations system used in treatment — antidepressants, antipsychotics, etc., optimizes post opioid detoxified, thus shortening during the withdrawal syndrome and reduce its severity.
Conclusions: Using optimized therapy helped achieve a significant reduction from baseline indicators of lipid peroxidation, which proves that the liver contribute to the development of the system operating in opium addiction, as well as the fact that the recovery of the antioxidant capacity of the body leads to the relief of the oxidative stress. The study period of abstinence in patients receiving optimized treatment including an antioxidant, found that significantly reduced the duration of withdrawal symptoms, reduced craving for the drug, and the low intensity of the generation of active forms of oxygen in the blood correlates with the effectiveness of therapy. Inclusion of ethylmethylhydroxypyridine succinate (mexidol) in the complex treatment of opioid addiction contributes to sustainable and prolonged suppression of free radical oxidation in the blood, observed immediately after treatment.
[Abstract:0084] [Mood disorders]
The relationship between leptin receptor polymorphism and suicide in depressed adolescents
Açıkel Sadettin Buraka, Eroğlu Cananb, Dikmen Asiye Uğraşc and Kurar Ercanb
aDepartment of Child and Adolescent Psychiatry, Dr. Sami Ulus Maternity and Child Health Hospital, Ankara, Turkey
bDepartment of Medical Biology, Necmettin Erbakan University Meram School of Medicine, Konya, Turkey
cDepartment of Public Health, Gazi University School of Medicine, Ankara, Turkey
ABSTRACT
Introduction: Suicide, which is the second leading cause of death among the ages from 10 to 24, is a public health problem, especially for adolescents, young people and middle-aged adults. Genetic studies (i.e. adoption and twin studies) suggest that the presence of a genetic component which causes the predisposition to suicide is independent from the presence of a genetic component which is associated with a psychiatric disorder [1]. Although genetics is an important factor that might be associated with suicide, limited progress is achieved to identify the candidate genes in adolescents.
Leptin is produced by white adipose tissue and plays a role in energy metabolism. The general effect of leptin is inhibiting appetite by leptin receptors located in hypothalamus. Also, leptin has an impact on mood. Although there are inconsistent results, low leptin levels are associated with depression in clinical studies [2]. In addition to this, leptin resistance (peripheral hyperleptinemia due to the resistance in central signaling) might comprise a risk for depression. It has been suggested that the increased risk of depression that is associated with obesity may be related to leptin resistance [3,4].
Major depressive disorder is a remarkable risk factor in adolescent suicide. Current studies have suggested that leptin resistance is an important factor in depression [3]. Leptin receptor gene polymorphisms are one of the most important factors that cause leptin resistance. In this study, it is aimed to investigate relationships between major depressive disorder, suicide and leptin receptor gene single nucleotide polymorphism.
Methods
Study sample
This study has been carried out at the outpatient unit of Child and Adolescent Psychiatry Department, Meram School of Medicine, Necmettin Erbakan University, in Konya, Turkey. The diagnostic evaluation has been made according to the DSM-5 diagnostic criteria with K-SADS-PL version. Having psychiatric treatment in the last 3 months, an additional medical condition, being diagnosed with neurodevelopmental disorders such as autism, schizophrenia, bipolar disorder and intellectual disability have been considered as the exclusion criteria. The control group is consisted of adolescents and families who has the same age and sex, without any psychiatric disorder. This study has also been approved by Necmettin Erbakan University Ethical Committee.
Psychometric Scales
Childhood Depression Inventory (CDI)
CDI is a self-assessment scale applicable to the children between the ages of 6 and 17. The cut point is recommended as 19. The validity and reliability of the inventory in Turkish have also been formed.
State-Trait Anxiety Inventory for Children
This anxiety scale that is developed by Spielberger for children consists of two parts with 20 questions. The validity and reliability of the inventory in Turkish have also been formed.
Negative Life Events List
Negative Life Events List is used which has been developed to be used in a thesis study before. If any negative life events occur, the adolescent who fills in the list is asked to respond as “yes” or “no”.
The Suicide Probability Scale (SPS)
The SPS, which has been developed by Cull and Gill, consists of 36 statements rated on a four-point scale. The reliability and validity of Turkish version have been conducted.
Genetic Analysis: The DNA isolation from blood samples is performed by using standard phenol / chloroform method [5]. Primers used in the amplification of leptin receptor gene (LEPR) single nucleotide polymorphism (SNP) regions are identified by using the literature [6–8] or the LEPR DNA sequence (GenBank accession code NG_015831). DNA products that are amplified by PCR have been examined for polymorphisms by reacting with the corresponding restriction endonuclease (RE).
Statistical Analysis: The analysis of the data has been performed by using a Statistical Package programmer for Social Sciences (SPSS) 20.0 statistical software (Chicago, IL, USA). Logistic and linear regression were conducted to assess the determinants of SPS scores. In linear regression model, having a normal genotype was coded as “0” and having a mutant allele (heterozygote and homozygote genotype) was coded as “1” as an independent variable. By this way, the data was converted to ordinal. A two-tailed p-value of 0.05 was considered to be statistically significant.
Results: The study sample consisted 203 adolescents. 97 (21 male, 76 female) of them had been diagnosed with major depressive disorders and 106 (28 male, 78 female) of them are healthy. There was no significant difference between the patient and the control groups in terms of demographics. Only maternal educational level was found to be significantly different between the groups. The independent sample t-test had shown that CDI, STAI and SPS total scores were significantly higher in the patient group.
In this study, five leptin receptor single nucleotide polymorphisms associated with leptin resistance in central nervous system have been examined. rs1805134, rs1805096, rs1171276, rs9436746 and rs1137101 were said polymorphisms. Regarding the number of people having homozygote or heterozygote genotype, the study has shown that there was no statistically significant difference between the patient and the control groups in chi-square analysis. Afterwards, the same analysis was performed in five SNP regions in which the patient and the control groups are separated in terms of having a mutant allele or not. It is concluded that there was no statistically significant difference between the groups.
The linear regression analysis was used to determine the predictors of suicide probability scores. The depending variables that were encoded as SPS total scores and CDI scores, state and trait anxiety scores, parental depressive scores, the number of negative life events, having a mutant allele for all SNP regions and previous suicide attempts are involved in the analysis to determine the predictor(s). As a result, R2: 0.786 of this model, a previous suicide attempt (B:5.553, t:2.613 p:0.035) and having a mutant allele in rs1171276 SNP region (B:4.346 t:2.220 p:0.048) have been found as the strongest predictors of SPS total scores. The regression results are shown in Table 1 in details.
Discussion: This is the first study that has ever been carried out to investigate the relationship between LEPR polymorphism and suicidal behavior in an adolescent sample. It has been found that carrying “G” mutant allele in rs1171276 SNP region and previous suicide attempt are statistically significant in the prediction of suicidal behavior in the whole sample.
There are several studies suggesting the potential relationship between serum leptin levels and suicide in adult samples. Atmaca et al. have found that plasma leptin levels were significantly lower in suicide attempters compared to healthy controls [9]. Although some opposite results are present, it has been mentioned that low serum leptin levels and reduced leptin mRNA in central nervous system might contribute to suicidal behaviors. As mentioned above in the introduction, leptin hypofunction might occur via low levels or resistance on the receptor. rs1171276 SNP is an intronic mutation and the results of A>G transformation in the leptin receptor DNA might break the leptin signaling in the central nervous system. By this way, this SNP might be leading to leptin hypofunction and suicidal behavior.
In literature, there are several studies indicating the relationship between leptin and impulsivity which is an important trait for suicidal behavior. In a recent study, it has been found that serum leptin levels are significantly lower in antisocial personality disorder patients compared to healthy controls. Moreover, leptin levels are inversely correlated with the severity of antisocial personality disorder symptoms [10]. In consideration of these findings, leptin hypofunction via low serum level or leptin resistance might be related to impulsive behavior which is an important trait for adolescent suicide.
Limitation of the study is the relatively small sample size to determine whether a single nucleotide polymorphism is a risk factor for a psychiatric disorder or a behavior. The data being collected from a single clinic is a limitation in generalizing the results. Similar studies should be carried out on a community basis.
This is first study to investigate the relationship between suicidal behavior and leptin receptor polymorphism in an adolescent sample. Further ones are needed for more clear results.
Table 1. Linear Regression Analysis Results.
Acknowledgments
This study has been supported by Necmettin Erbakan University Scientific Research Projects Commission with project number 161518007.
[Abstract:0116] [Addictions]
Comparison of executive functions in adolescents with synthetic cannabinoid and Semi-Synthetic opiate use disorder
Alaca Rümeysaa, Yüksel Tuğbaa, Karaçetin Gülb and Çiftçi Arzuc
aDepartment of Child and Adolescent Psychiatry, Dicle University, Diyarbakır, Turkey
bDepartment of Child and Adolescent Psychiatry, Istanbul Bakırköy Mental Health and Nerve Diseases Training at the Research Hospital, Istanbul, Turkey
cChild and Adolescent Substance Abuse Treatment Center (ÇEMATEM) of Bakirkoy Training and Research Hospital for Psychiatry, Neurology and Neurosurgery, Istanbul, Turkey
ABSTRACT
Introduction: Synthetic cannabinoids (SC) and THC act on cannabinoid receptor type 1 (CB1) and cannabinoid receptor type 2 (CB2) in brain and peripheral organs [1]. Endocannabinoid system plays a key role in the regulation of neurodevelopmental processes. When the literature was reviewed, two studies evaluating the effects of synthetic cannabinoids on executive functions using neuropsychological tests were found. In a study by Cohen et al (2017); synthetic cannabinoid, cannabis users and control group were compared using by Stroop test, n-back test and long-term memory test. They found that attention, response inhibition, working memory and long-term memory functions were found to be more impaired in the SC group than in the cannabis and control groups [2]. SC, cannabis users and control group compared with a large neuropsychological battery by Yilmaz at all (2018); Synthetic cannabinoid users were found to have more impaired executive functions compared to other groups. Also; It has been reported that they perform worse memory functions such as learning, recall, recognition [3].
In the literature, there are fewer studies on the effects of chronic opiate use on executive functions compared to studies on THC or stimulants. Studies on these issues have inconsistent findings. Some studies have reported impairments in strategic planning, decision making, response control and cognitive flexibility however in some other studies no clear impairment was found in comparison with healthy controls. Especially; the magnitude of impairment in memory, attention, executive functions and other cognitive abilities remains unclear. In a study by Ornstein et al., some changes have been shown on attention, set change, and sequence creation tasks in heroin users [4]. Pau et al. (2002) found that heroin use had a negative effect on impulse control; it has no effect on abilities such as attention, mental flexibility and abstract reasoning [5].
Synthetic cannabinoids and semi-synthetic opiate (SSO) (heroin) using have high rates among drug users who applied to treatment for substance abuse in adolescent age group in Turkey. Therefore; it is important to expand our clinical knowledge regarding these two user groups and get to know patient profiles more closely. Our aim is to expand our clinical knowledge about these two groups and to compare the executive functions of these two groups with neuropsychological test battery.
Methods
Study Participants
Participants comprised 62 patients between the ages of 15 and 18. The patients who were being treated between January - June 2018, in the department of Child and Adolescent Substance Abuse Treatment Center (ÇEMATEM) of Bakirkoy Training and Research Hospital for Psychiatry, Neurology and Neurosurgery of Istanbul. Two groups were present in our study: synthetic cannabinoid use disorder group and semi-synthetic opiate use disorder group.
The first group was the SC use disorder group and consisted of 30 adolescents with 24 male and 6 female patients. The patients who were using SC at least 6 months and at least once a week. The patients who used drugs other than SC more than once a week in the last 6 months and SSO use at any time in their lives were not included in this group.
The second group was the semi-synthetic opiate use disorder group consisted of 32 adolescents with 24 male and 8 female patients. The patients who were using SSO at least 6 months and at least once a week. The patients who used drugs other than opiates more than once a week in the last 6 months and SC use at any time in their lives were not included in this group.
Patients with psychoactive substance use in the last 24 hours, have a clinical findings of intoxication or withdrawal, in active psychotic and manic episodes, autism, hearing-visual impairment, illiterate were excluded from the study.
The Ethics Committee approval was obtained before the study. All of the participants were informed about the interview and tests to be applied and written consent was taken from each participant. After the sociodemographic data form was completed, psychiatric comorbidities of the patients were evaluated by using the Kiddie Schedule for Affective Disorders and Schizophrenia-Present and Lifetime Version (KSADS-PL). Then, Stroop Color Vocabulary Test and Wisconsin Card Sorting Test (WCST) were used to evaluate the executive functions of the cases..
Assessments
Sociodemographic data form. This form is an interview form with detailed questions about age, gender, educational status, family information and substance use in order to determine the sociodemographic characteristics of the participants by the researchers.
The Kiddie Schedule for Affective Disorders and Schizophrenia-Present and Lifetime Version (KSADS-PL). This form is used to detect psychopathologies in children and adolescents according to DSM-IV diagnostic criteria, it was prepared as a semi-structured interview form by Kaufman et al. (Kaufman et al., 1997). The validity and reliability study of the Turkish version was performed by Gökler et al.
Stroop Color-Vocabulary Test. The Stroop test is considered the gold standard of attention testing in the literature. The Turkish validity and reliability study of the Stroop Color Vocabulary Test was performed in 1999 by Karakaş et al. [6].
Wisconsin Card Sorting Test. The Wisconsin Card Sorting Test, a test by Berg and Grant in 1948, is a test that evaluates executive functions in the literature. The Turkish adaptation study of the Wisconsin Card Sorting Test was performed in 1998 by Karakaş et al. [7]
Statistical analysis: SPSS version 18.0 was used for statistical analysis of the study data. Student-t test was used to compare two quantitative variables with normal distribution. Mann Whitney U test were used for pairwise comparisons of quantitative variables that do not show normal distribution and for descriptive statistical methods (mean, standard deviation, frequency, median, minimum, maximum, ratio). Pearson's Chi-Square test and Fisher's Exact test were used to compare qualitative data. Pearson Correlation Test and Spearman Correlation Test were used to evaluate the relationships between the parameters. Statistical significance was accepted as p < 0.05 and Statistical significance tendency was accepted 0.05 < p < 0.10.
Results: In our study, the mean age of the SC group was 17.0 ± 0.9 and the mean age of the SSO group was 17.3 ± 0.8. No statistically significant difference was found between the study groups in terms of age, gender, duration of education, school success, open secondary education and study status (p > 0.05).
The mean age of onset the SC group was 14 ± 1.4, and the SSO group was 14 ± 1.6. 83% of the SC group and 94% of the SSO group were using the substance every day. The mean total use dose was 2190 gr / g in the SC group and 1998 gr / g in the SSO group. The duration of the abstinence period was determined as minimum 2 days, maximum 913 days, the average 60 days in the SC group and the minimum 2 days maximum 548 days, the average 14 days in the SSO group. In our study, no statistically significant difference was found between the sociodemographic characteristics, age of starting, duration, frequency of substance use, abstinence time of the patients (p > 0.05). All of the patients (100%) were using tobacco, and all of the SSO group were receiving buprenorphine-naloxone treatment. No significant difference was found between the two groups in terms of other psychotropic drug use (p > 0.05). There was no statistically significant difference between the groups for lifetime use of cigarette, volatile substance, cocaine, methamphetamine, alcohol and cannabis, but lifetime ecstasy use (U = 256.00, p < 0.001) was higher in the synthetic cannabinoid group. No statistically significant difference was found between the study groups in terms of comorbid psychopathologies (p > 0.05).
In the Stroop Test, selective attention functions of the semi-synthetic opiate group were found to be worse than the synthetic cannabinoid group (p < 0.05). In the WCST test, the synthetic cannabinoid group was shown to exhibit more perseverative behavior, but was not statistically significant (0.05 < p < 0.10). The other Stroop and WCST performances were not significantly difference between the two groups (p > 0.05). We found that selective attention function is impaired with increased using amount of synthetic cannabinoids; selective attention, cognitive flexibility and response inhibition is impaired with increased using amount of semi-synthetic opiate. Moreover, it was determined that as the abstinence period decreased, the selective attention function worsened, and the reading speed slowed down in semi-synthetic opiate users.
Conclusions: No studies have been found in the literature comparing the executive functions of adolescents using synthetic cannabinoids and opiates. In this respect, our study should be an important study. The sociodemographic characteristics, comorbid psychopathologies, substance use characteristics and executive functions other than selective attention of adolescents with synthetic cannabinoids and semi-synthetic opiates using are similar in our study.
According to the results of the neuropsychological test; It is possible to say that heroin has impaired executive functions as much as cannabinoids, since selective attention functions of SSO users are much worse compared to SC users and they perform similar in terms of other executive functions.
In both groups, a positive relationship was found between the throughout life amount of substance used and impaired executive functions. İt was determined that as the abstinence period decreased, the selective attention function worsened and the reading speed slowed down in SSO users. There is a need for further studies on the effects of SC and SSO on executive functions with limited number of studies in the literature.
[Abstract:0132] [Neuroscience: Neuroimaging-Genetics-Biomarkers]
The possible role of the kynurenine pathway and the Cytokine levels in the adolescents with major depression
Öztürk Masuma, Sapmaz Şermin Yalınb, Kandemir Hasanb, Taneli Fatmac and Aydemir Ömerd
aDepartment of Child and Adolescent Psychiatry, Kızıltepe State Hospital, Mardin, Turkey
bDepartment of Child and Adolescent Psychiatry, Manisa Celal Bayar University Faculty of Medicine, Manisa, Turkey
cDepartment of Biochemistry, Manisa Celal Bayar University Faculty of Medicine, Manisa, Turkey
dDepartment of Psychiatry, Manisa Celal Bayar University Faculty of Medicine, Manisa, Turkey
ABSTRACT
Introduction: The biological mechanisms underlying major depressive disorder (MDD) are not yet sufficiently understood. Due to current antidepressant treatments focussed on normalisation of monoamines, such as serotonin and norepinephrine, dysfunction in monoamine neurotransmission has been studied the most. However, more complex mechanisms are thought to be associated with depression. In addition to neuroinflammation caused by stress and associated changes in the brain, changes in the immune system are also included in the aetiology of MDD [1]. The kynurenine pathway has been proposed to play a key role between peripheral inflammation and alterations in the central nervous system. This is due to reduced usability of tryptophan and production of oxygen radicals and highly potent neurotoxic agents in this pathway [2]. Tryptophan entering the kynurenine pathway is transformed into N-formyl kynurenine by enzymes tryptophan 2,3-dioxygenase (TDO) and indolamine 2,3-dioxygenase (IDO), which differ in terms of their cell localisations and substrate specificities. This step of the kynurenine pathway is the first step of the pathway and is also the rate-limiting step. After this step, other metabolites, such as 3-hydroxyantralinic acid, kynurenic acid and quinolinic acid, which have physiological and pathophysiological effects on cellular functions via other enzymes in the catabolic pathway, are formed [3]. In this study, we aimed to compare the metabolites of the serum kynurenine pathway (tryptophan, kynurenine, quinolinic acid and kynurenic acid) and interferon (IFN)-γ, interleukin (IL)-6, IL-1β and high-sensitivity C-reactive protein (hsCRP) levels in patients with MDD and in healthy controls and to evaluate the relationship between cytokine levels and the functioning of the kynurenine pathway.
Methods: This study was conducted between November 2016 and April 2018 at the Manisa Celal Bayar University Faculty of Medicine (MCBUFM) Department of Child and Adolescent Psychiatry Outpatient Clinic. In the semi-structured psychiatric interview conducted by the researcher, the patients who were diagnosed with MDD were included in the study by reviewing the inclusion and exclusion criteria. For the healthy control group, young patients aged 13–18 years who were admitted to the MCBUFM Pediatrics Outpatient Clinic for any reason, did not have a chronic disease and were not diagnosed with a psychiatric disorder before, were referred to the researcher.
Inclusion and Exclusion Criteria of the Study: Exclusion criteria for all participants were determined as follows: having used drugs affecting the immune system in the last 6 months, having any immunological disease, haematological disease, infectious disease in the last month, having a significant medical or neurological disease or substance abuse in the last 3 months.
Inclusion criteria for the patient group were determined as follows: being in the age range of 13–18 years, having a diagnosis of active MDD according to DSM-5, persistence of MDD episode for at least 6 weeks and having a score of ≥37 in the Children's Depression Rating Scale-Revised (CDRS). Patients who had psychotropic medication use in the last 6 weeks and patients who were diagnosed with bipolar disorder, schizophrenia, pervasive developmental disorder, post-traumatic stress disorder, Tourette syndrome, eating disorder, obsessive compulsive disorder and substance abuse during their life time were excluded from the study.
Exclusion criteria for the healthy control group were determined as follows: having a history of major psychiatric illness and psychotropic drug use.
Clinical Evaluation: Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL), CDRS-Revised were applied, and a sociodemographic data form was completed. All patients were asked to fill out the DSM-5 Level 2 Irritability Scale-Child Form and the DSM-5 Level 2 Depression Scale-Child Form.
Biochemical Analyses: For the measurement of neurobiological markers, blood samples were collected into 10 mL anticoagulant tubes, preferably between 9.00 and 10.00 a.m. on an empty stomach in the morning. The venous blood samples were centrifuged at 3000 rpm for 15 minutes to be separated from their serum and stored at −80°C until analysed.
Serum samples were analysed for IL-6, IL-1β, TNF-α, interferon (IFN)-γ, tryptophan, quinolinic acid, kynurenic acid and kynurenine levels by the enzyme-linked immunosorbent assay. High-sensitivity (hs) CRP test was analysed with the original reagents on the Beckman Coulter AU5821 analyser, which was able to measure within a range of 0.08–80 mg/L by the immunoturbidimetric method.
Statistical Evaluation: The data obtained from the study were evaluated by using the Statistical Package for Social Sciences 21.0 programme. Continuous variables obtained by measurement were expressed as mean ± standard deviation, and categorical variables were expressed as percentage and number. In the mean comparison between the two groups with normal distribution, Student's t-test was used for independent groups and Mann–Whitney U test, which is a non-parametric test, was used for those that did not show normal distribution. One-way analysis of variance was used for the comparison of three or more groups with normal distribution, and the non-parametric Kruskal–Wallis analysis was used for those that did not show normal distribution. Chi-square analysis and Fisher's exact test were used to compare categorical data. In order to determine the direction and level of the relationship between numerical variables, Pearson's test was used for those with normal distribution and Spearman correlation test was used for those that did not show normal distribution. In all analyses, p < 0.05 was considered statistically significant.
Results
Demographic and clinical features: The study included 48 patients with MDD and 31 healthy controls. No statistically significant difference was found between the groups in terms of age and gender. In the MDD group, 30 (62.5%) patients had at least one comorbid psychiatric diagnosis.
Kynurenine Metabolite Levels: Significant differences were found between the groups when the levels of tryptophan (p = 0.046), quinolinic acid (p = 0.003), kynurenine/tryptophan (KIN/TRP) ratio (p = 0.032) and kynurenic acid/quinolinic acid (KYNA/QA) ratio (p = 0.040) were compared. With significant difference, quinolinic acid and KIN/TRP ratio increased in the patient group, whereas tryptophan and KYNA/QA ratio decreased in the patient group. No significant difference was found between the groups in terms of kynurenine (p = 0.564) and kynurenic acid (p = 0.182) levels (Table 1).
When the relationship of the kynurenine pathway metabolites with the clinical data was examined in all patients included in the study, a statistically significant positive correlation was found between quinolinic acid and CDRS scores (r = 0.368, p = 0.009), DSM-5 level-2 depression scale scores (r = 0.341, p = 0.015) and DSM-5 level-2 irritability scale scores (r = 0.370, p = 0.008). A statistically significant (r = −0.288, p = 0.043) weak negative correlation was found between KYNA/QA ratio and irritability scale total scores.
Cytokine Levels: No significant difference was found between the groups when the levels of IFN-γ (p = 0.897), IL-6 (p = 0.086), IL-1beta (p = 0.134) and hsCRP (p = 0.473) were compared. When the relationship of the IFN-γ, IL-6, IL-1β and hsCRP variables with clinical data was examined in all patients included in the study, there was a statistically significant negative correlation between IL-6 and DSM -5 level-2 depression scale total scores (r = −0.369, p = 0.009) and IL-6 and DSM -5 level-2 irritability scale total score (r = −0.345, p = 0.015).
The Relationship of IFN-γ, IL-6, IL-1β and hsCRP Cytokines with KIN/TRP and KYNA/QA Ratios in the whole sample: As a result of the analysis, there was a weak negative correlation between IFN-γ and KIN/TRP ratio (r = −0.279, p = 0.016).
Discussion: In our study, the KIN/TRP and the quinolinic acid level were found to be significantly higher in the adolescents with depression compared to the healthy controls, whereas the tryptophan level and the KYNA/QA ratio were found to be significantly lower. As a result of our study, it was determined that the activity of the IDO enzyme (kynurenine/tryptophan ratio) increased in patients with MDD, and there was an imbalance between neurotoxic and neuroprotective products in the kynurenine pathway. These findings suggest that tryptophan is catabolised via the kynurenine pathway instead of the serotonin pathway in MDD cases, and neurotoxic molecules in this pathway increase and contribute to the aetiology of MDD. The elevation of the KIN/TRP ratio in patients with MDD was consistently accompanied by a high level of quinolinic acid and a decrease in the KYNA/QA ratio. In addition, the correlation of these values with the severity of depression and irritability suggests that this pathway can be included in the aetiology of depression. The high levels of neurotoxic metabolites in patients with MDD support the hypothesis that this pathway contributes to the aetiology of depression through decrease in the availability of tryptophan as well as neurotoxic molecules in the pathway.
[Abstract:0146] [Autism]
MACROD2 Gene expression profile in Autism Spectrum disorder: a case-control study
Alnak Alpera, Özücer İpek Kuşcua, Çağlayan Ahmet Okayb and Coşkun Murata
aDepartment of Child and Adolescent Psychiatry, Istanbul School of Medicine, Istanbul University, Istanbul, Turkey
bDepartment of Medical Genetics, School of Medicine, Istanbul Bilim University, Istanbul, Turkey
ABSTRACT
Introduction: Autism spectrum disorder (ASD) is a neurodevelopmental disorder characterized by deficits in communicative and social skills, and repetitive behaviors and/or restricted interests, with early onset. Pathogenetic mechanisms involved in ASD etiology have not been fully understood. Heritability of ASD is high, ranging from 0.38 to 0.90 (1). Genetic mechanisms underlying ASD are as complex and heterogenous as its clinical heterogeneity, including single gene disorders, polygenic mechanisms and epigenetic alterations (2). In the literature, thousands of genetic variations involving more than 100 genes have been identified as either associated with or carrying risk for ASD. Though, many of these variants show incomplete penetrance and may be localized in non-coding regions (3,4). Thus, it may be useful to evaluate transcriptional activity of a gene in which genetic variations were previously identified.
Macro Domain Containing Gene 2 (MACROD2) is located on chromosome 20 and genetic alterations in this gene were recently shown to be associated with ASD (5). Macro domains act as deacetylases binding ADP-ribose and although their functions are largely unknown, it is thought that they have an important role in regulating gene expression and DNA repair (6,7).
Preliminary studies linking MACROD2 gene to ASD were from a transgenerational genome-wide screening study by Tsang et al. in which they found this region as a candidate region for ASD (8). In a genome-wide scan for common alleles in ASD, Anney et al. analyzed 1385 ASD probands from 1369 families for 1 million SNPs. In this study, strongest associations were detected in a small intronic region of MACROD2. Association for a single nucleotide polymorphism located in this region (rs4141463) reached the significance level, p = 2.1×10−8 (5).
Several recent studies were conducted to replicate this finding. Curran et al. conducted a case-control study of 1170 cases with autism and 35307 control participants and they noted that they did not replicate the findings of the study by Anney et al (9). After this failure to replicate, few more studies from different ethnic groups were also published controversial results (10–16).
In this case-control study, we aimed to examine gene expression profile of MACROD2 gene in a group of children with ASD compared to healthy controls in Turkey.
Method
Participants
Subjects for study group were recruited among those who have been followed up with diagnosis of ASD according to DSM-5 criteria in our department. 100 young subjects aged 2 to18 years old-with DSM-5 diagnosis of ASD were included. Diagnosis of ASD was confirmed by the authors through detailed clinical examination. Childhood Autism Rating Scale (CARS) and Aberrant Behavior Checklist (ABC) were applied to evaluate symptom severity and/or accompanying behavioral and emotional difficulties. Participants were required not to have severe/ profound intellectual disability, previously known genetic, metabolic or progressive neurologic diseases. Subjects for control group were recruited among referral to our department. Age and gender matched subjects were approached for the participation to study. They were required to be free of diagnosis of ASD, intellectual disability, previously known genetic, metabolic or progressive neurologic diseases. They were also undergone detailed clinical examination by the authors to make sure they meet inclusion criteria. 100 children were included as control group. This study was supported by a grant from Scientific Research Project Coordination Unit of Istanbul University (project ID no: TTU-2017-26608).
Instruments
Interview Form. Interview form was developed by authors and included questions on patient's date of birth, gender, contact information and other basic sociodemographic information.
Childhood Autism Rating Scale (CARS). Childhood Autism Rating Scale is a frequently used, valid and reliable scale developed by Schopler et al. (1980) to assess disease severity and differentiate individuals with ASD and those with other developmental delays (17,18). It consists of 15 items, each assessing different aspects of ASD symptoms and development. The scale form that had been adapted into Turkish was shown to be valid and reliable (19).
Aberrant Behavior Checklist (ABC). Aberrant Behavior Checklist is a useful tool for evaluating inappropriate and maladaptive behaviors which has been translated into more than 25 languages and is used commonly worldwide in subjects with ASD and developmental delay. Turkish form of ABC consists of 46 questions assessing five domains of behavior: hyperactivity/noncompliance, lethargy/social withdrawal, stereotypic behavior, self-injurious behavior and other behaviors (20).
Gene Expression Analysis
Total RNA was extracted from whole blood using Hybrid-RTM (GeneAll, Seoul, South Korea, catalog no: 315-150) and transcribed into complementary DNA with Ipsogen® cDNA Synthesis Kit according to the manufacturer's instructions (Qiagen GmbH, Hilden, Germany, catalog no: 679923). The quantity, quality and integrity of RNA were assessed on Qubit 2 fluorometer (Thermo Fisher Scientific Inc, Wilmington, DE, USA). Real-Time Quantitative PCR analysis was performed using Thermo Scientific RevertAid First Strand cDNA Synthesis Kit (Thermo Fisher Scientific Inc, Wilmington, DE, USA, catalog no: K1622). Four different MACROD2 and three reference genes ABL-1, CUL1 and ZNF207 primers were used. Relative changes in gene expression were analyzed with the ΔCT method (21).
Statistical Analysis
R 3.4.0 and Statistical Program for Social Sciences (SPSS for Windows, 21.0) were used for statistical analyses. Kolmogorov-Smirnov test used for assessing normal distribution of data. Descriptive data were presented as mean and standard deviation. Two different statistical analyses (t test and Wilcoxon Rank Sum test) was performed and P value < 0.05 was considered to be statistically significant.
Results: A total of 200 children were included in the study. The mean age of study and control groups were 9.22 ± 3.62 (2 to 17 years) and 9.21 ± 3.57 (3 to 17 years) respectively. 87 percent of study group and 85 percent of control group were male. There was no significant difference in terms of gender (p = 0.684) and age (p = 0.900) between the two groups. There was no statistically significant difference between the two groups in terms of mother's (t = 0.918; p = 0.349) and father's age (t = 1.754, p = 0.081) at birth.
Gene Expression Analysis
MACROD2 gene expression was observed in 26% of study group and 18% of the control group. Three reference genes (ABL-1, CUL1 and ZNF207) defined as housekeeping genes were expressed in all samples. Although MACROD2 gene expression was found to be decreased in study group, this finding did not reach statistical significance. Results were outlined at Table 1 and shown as box-plot graphic in Figure 1 and 2.
We also conducted several analyses to examine association between MACROD2 gene expression status in study group and CARS scores, ABC total scores, mother's and father’ age at birth. There were no statistically significant differences between MACROD2 expression status and CARS scores (t = -0.678, p = 0.499), ABC total scores (t = -0.011, p = 0.992), mother's age (t = -0.711, p = 0.479) and father's age (t = -0.128, p = -0.908) at birth.
Discussion: There is a growing body of research in the genetics of ASD. Despite significant progress has been made in recent years with the developing molecular genetic analysis technology, exact etiology of ASD remains unclear. MACROD2 is a gene located on 12.1 region in the long arm of chromosome 20 and it encodes for a protein which has an ADP binding deacetylase component (7). It is highly expressed in both fetal and adult brain particularly in periventricular area (12,22). Genetic alterations in this gene were recently shown to be associated with ASD (9–13,15,16). However, while majority of these studies evaluated genomic changes in MACROD2, expression level of MACROD2 was not examined. Several studies have stated that significance of genomic variations of MACROD2 in ASD may show ethnic differences (5,9,10). As far as we know, the current study is the first case control study to evaluate MACROD2 gene expression profile in subjects with ASD in Turkish population.
In our study, we analyzed 100 subjects with ASD and 100 gender and age matched children with normal development. Given the fact that there is no normative range of expression level of MACROD2 gene in different tissues according to gender and age, it may be important to exclude gender and age effects between the study and control groups. Expression of MACROD2 in the study group was lower than the control group. However, this difference was not statistically significant (p = 0.124). This may be accounted by several methodological limitations such as small sample size and several inherent conditions such as low rate of gene expression both in study and control groups. Also, peripheral expression of MACROD2 may not be predictive of genuinely neural expression (23). Given that changes in brain tissue in ASD occur in the fetal period and in the early years of life, the gene expression levels in the age range of 2-18 years of our study may not reflect these periods. However, this situation constitutes a general limitation for expression studies, rather than specific to our study. Furthermore, genetic variations within the MACROD2 gene which were previously shown to be associated with ASD may be affecting the expression of other genes in its neighborhood rather than itself (12).
Conclusion: Genetic variations in MACROD2 were shown to be associated with ASD from several previous studies. As the first case-control study of MACROD2 gene expression in ASD in Turkish population, we found decreased yet not statistically significant level of MACROD2 expression in subjects with ASD compared to normally developing children. Given the lack of information on the expression profile of the MACROD2 gene in different tissues through developmental periods, this case-control study may provide a basis for future studies in this area.
Acknowledgements
This study was supported by a grant from Scientific Research Project Coordination Unit of Istanbul University (project ID no: TTU-2017-26608).
[Abstract:0196] [Psychotherapies]
Investigation of the relationship between clinical characteristics, automatic thought and dysfunctional schemas in major depressive disorders
Yığman Fatiha, Özdel Kadira and Efe Cananb
aHealth Sciences University Dışkapı Yıldırım Beyazıt Research and Training Hospital, Ankara, Turkey
bGölbaşı Şehit Ahmet Özsoy State Hospital, Ankara, Turkey
ABSTRACT
Introduction: Major depressive disorder (MDD) is quite common in the general population and is an important public health problem worldwide. The prevalence of life-long MDD in the United States is about 15% [1] and it is associated with significant functional impairments, reduced quality of life, and suicidal behavior [2].
Cognitive theory examines the cognitive structures of people in two main sections: automatic thoughts and schemas. Schemas can be examined in two parts as intermediate beliefs (conditional rules) and core beliefs. In this sense, a three levels of cognition structure will emerge: core beliefs are the most entrenched and at the inner level of beliefs, automatic thoughts are at the most superficial level of cognition, and intermediate beliefs are between core beliefs and automatic thoughts [3].
There were three hypotheses in this study: first, there was a difference in negative cognitions between healthy control group and depression patients. Secondly, negative cognitions of patients with severe depression were more intense than those of patients with moderate depression. Thirdly, the negative cognitions of recurrent depressive events were more severe than the first episode depressive patients.
Methods
Study Participants
A total of 101 patients with an age range of 18-65 who were consecutively presented to psychiatry outpatient clinics of Diskapi Yıldırım Beyazit Training and Research Hospital and who were diagnosed as depression between January 2017 and April 2017 were included in the study. The patients were screened and diagnosed with the Structured Clinical Interview for DSM IV Axis I Disorders (SCID-I). 101 depression cases and 82 healthy control groups were included in the study. Psychotic patients, patients with bipolar disorder, patients with dementia, patients with organic mental disorder (OMD), patients with mental retardation were not included in the study.
Beck Depression Inventory (BDI), Beck Anxiety Inventory (BAI), Automatic Thoughts Scale (ATS), Short Form of Dysfunctional Attitudes Scale (DAS-A), the and Social Comparison Scale (SCS) were used as reliable and valid assessment instruments.
The data were evaluated with SPSS 15.0 for Windows. Chi-square test was used to determine whether there was any difference between the groups in terms of categorical variables. In the parametric comparisons, two independent samples were used. Since the parametric assumptions were met for the relationship between the numerical variables, Pearson correlation was used.
Results: A total of 101 patients who met the required criteria participated in the study and 82 healthy subjects were included in the study. The sociodemographic data of the study groups is in Table 1.
When depression and control group were compared; significant differences were found in all scales.
When the first-episode MD and the recurrent MD group were evaluated, the mean scores of the BDI were higher in the first episode MD group, however, there was no difference between the BDI scores and whether depression was recurrent or not (p: .099 > 0.050).
There was a significant difference between whether depression was recurrent or not and the subscale of ATQ, “Personal Maladjustment and Desire For Change” (.010 < 0.05), and this difference was due to higher scores on the first-episode depression group.
When the patients were separated as mild, moderate and severe depression according to the Beck Depression Inventory, it was determined that there was 1 person who met mild depression criteria.
When cognitive subscales were evaluated according to severity of depression; there was a significant difference between the groups in all subscales.
When the intra-scale correlation within the patient group were evaluated, there was a significant correlation between the Beck Depression Inventory and the Beck Anxiety Inventory (0.601 > 0.05).
There was a significant correlation between the Beck Depression Inventory, and the negative self-concept subscale (0.730) and the Automatic Thoughts Scale (0.745).
Discussion: When the BDI scores were evaluated in terms of recurrent depression, no relation was found with previous depressive episode, and we could not find a relationship between symptom severity and depression recurrence.
According to the results of our study, no relation was found between automatic thoughts and recurrence of depression. Nevertheless, when we looked at the severity of depression, we observed that the negative automatic thoughts was more intense in the group with severe depression and a strong positive correlation between the severity of depression symptoms and the negative automatic thoughts.
There was no relationship between dysfunctional attitudes and recurrence of depression according to the results of our study. Again, when we analyzed the severity of depression, we observed that severity of depression was associated with dysfunctional attitudes.
In our study, when the average scores of patients and control group were compared according to the Social Comparison Scale items, it was observed that the control group gave higher scores in all subscales. In the recurrent depression group, there was no significant difference between the groups with the first-episode of depression. When assessed on the basis of severity of depression, the scores of the severe depression group were lower in all sub-items and the scale total score.
According to our results, there was a strong relationship between depression symptomatology and automatic thoughts. Cognition at the level of intermediate belief and core belief is one step behind that of automatic thoughts as well as being associated with the severity of depression.
Our findings suggested that the activation of cognitive traits was largely related to severity, regardless of depression recurrent or not, on the contrary, the factor that determined the severity of the symptoms suggested that the cognitive traits were related to the degree of activity.
In this study, which we planned to evaluate cognitive processes related to depression, we had limitations such as not showing the necessary attention when patients were filling some self-reported scales, fewer number of patients in some subgroups, and different sex ratios between groups. In addition, the evaluation of cognition at the level of core belief is rather difficult and indirectly, the existence and severity of core beliefs can be predicted through the existence of personality disorder. Moreover, this study is a cross-sectional planned study and makes it difficult to interpret some findings because it is not prospective. Because of these limitations, long-term studies and studies including more cases will be useful.
Table 1. Sociodemographic data of the study groups.
Table 2. Evaluation of Recurrences of Depression and Cognitive Scales.
Table 3. Evaluation of Severity of Depression and Cognitive Scales
Table 4. Analysis of Intercorrelations of Scales in the Patient Group
[Abstract:0257] [Sleep Disorders]
Effects of second generation antipsychotics risperidone, olanzapine and aripiprazole on sleep structure in the treatment of first-episode psychosis patients
Subaşı Elifa, Akçay Bülent Devrimb and Yetkin Sinanb
aDepartment of Psychiatry, Gülhane Education and Research Hospital, Ankara, Turkey
bDepartment of Psychiatry, Gülhane Education and Research Hospital, Sleep Research Center, Ankara, Turkey
ABSTRACT
Introduction: Sleep disorders are a common problem in non-organic psychosis patients and are an important part of the clinical picture. In this patient group, disturbances in sleep structure are seen more frequently than healthy individuals. A limited of polysomnography studies have been conducted in patients with first-episode psychosis and there is no consensus on sleep structure. Concurrently, the effects of atypical antipsychotics on sleep structure could not be elucidated clearly. In this study, 13 first-episode psychosis patients who underwent polysomnographic study were evaluated retrospectively and were aimed to compare effects on the sleep structures of the second-generation oral antipsychotics risperidone, olanzapine, aripiprazole were used in the treatment of these patients.
Methods: This study was carried out retrospectively from the inpatient files in the psychiatry clinic of Gülhane Education and Research Hospital. The records and polysomnographic records of the first episodes of psychosis patients with polysomnographic studies were examined and compared in Gülhane Sleep Research Center. It was learned from retrospective analysis that risperidone was started to 5 patients, olanzapine to 4 and aripiprazole to 4 patients, as monotherapy and in the first month and sixth month, polysomnography recordings of the patients were examined and compared. Polysomnography recordings were made according to the American Academy of Sleep Medicine (AASM) criteria by using the Grass Comet Plus AS40 polysomnography device. The records obtained by the sleep technicians were scored by the experienced physicians in the field of sleep medicine. Statistical analyzes were performed with IBM SPSS Statistics 25 package program. Since the data did not fit the normal distribution and the sample size was not sufficient, a non-parametric test, Wilcoxon test, was applied. According to this test, p < 0.05 was accepted as significant.
Results: All patients included in the study were male and the mean age was 23.96 ± 3.74. Comparison of polysomnographic evaluations at 1th month and 6th months; the mean dose of the drug was 6 mg / day in the patient group who used risperidone (n = 5). From the parameters related to the continuity of sleep; increased sleep efficiency, increased total sleep time, decreased number of total wakefulness were found to and from sleep structure related parameters; increased Stage 3 sleep time and increased percentage were found to. These differences were statistically significant (p < 0.05). (See Table 1) The mean dose of the drug was 10 mg / day in the patients with olanzapine (n = 4). From the parameters related to the continuity of sleep; decreased sleep latency, decreased the number of wakefulness were found to. from REM sleep related parameters; REM latency was found to be shorter. These differences were statistically significant (p < 0.05). (See Table 2) The mean drug dose was found to be 15 mg / day in the patient group who used aripiprazole (n = 4). In this group, no statistically significant difference was found between the data obtained from the polysomnographic records of the patients at the first and sixth months of therapy, and the parameters related to the sleep consistency, structure and REM sleep (p > 0.05). (See Table 2)
Discussion: Sleep structure in schizophrenia is impaired according to healthy individuals. In particular, it was noted that slow wave sleep (delta sleep) and REM sleep are markedly reduced, sleep is superficial and frequent awakening. There are two main difficulties in sleep studies in schizophrenia. The first is that patients are not compatible for sleep studies. The second is the difficulty in finding a patient who has not used any drugs, has no mood disorder and is in the first psychotic episode. The fact that our study was performed on first-episode psychosis patients who had no previous antipsychotic drug without mood disorder provided the effects of antipsychotic drugs on sleep more clearly. In psychotic disorder, regulation of sleep and alertness includes many neuronal regions and neurotransmitters. Many antipsychotics have the potential to affect the regulation of the sleep-wake system with their activities on the central nervous system, especially with the gamma-neurobutyric acid, glutamate, acetylcholine, noradrenaline, serotonin, dopamine and histamine in the neurotransmitter system. Antipsychotic drugs may cause sedation by increasing the activity of systems that provide sleep or by reducing the activity of systems that provide alertness. By contrast, they can increase alertness by using opposing mechanisms. Therefore, knowing the receptor mechanisms of these drugs helps us to predict their effects on sleep and wakefulness functions. Sleep disorders are common in patients with psychotic episodes, including insomnia, excessive sleep, and sleep patterns.
Generally, medications for psychosis can aggravate patients and make the over-sleep condition worse. For patients with excessive sleep, choosing a less sedative antipsychotic and careful management of sleep disturbances are also important in terms of compliance with treatment in patients receiving antipsychotic treatment. Many antipsychotic drugs cause sedation, but the sedative effect of all drugs is not the same. Sedation is involved with dosage and the amount of drug that reaches the central nervous system determined by its affinity for the histamine H1 receptors. Atypical antipsychotics usually lead to less sedation than traditional antipsychotics, while providing similar or greater reduction in symptoms. Studies have shown that atypical antipsychotics, such as risperidone, olanzapine, quetiapine and ziprasidone, generally cause less sedation compared to traditional antipsychotics, but are effective in controlling psychosis and agitation. Tandon et al. examined sleep disturbances in 40 schizophrenic patients and found that sleep latencies, increased arousal during sleep, and sleep duration during sleep and sleep activities increased compared to those in the non-psychiatric control group. Benson and Zarcone compared 18 patients with schizophrenia and 13 non-psychiatric control groups. The study found that there was an increase in stage 1 sleep time in schizophrenia patients compared to the control group and a decrease in stage 3 (slow wave) sleep duration. The total sleep efficiency in patients with schizophrenia was 83% and non-psychiatric control group was 95%, respectively. Because of these changes in sleep patterns, they concluded that patients with schizophrenia often have insufficient sleep. The choice of antipsychotic drug in patients with psychosis is very important since it is in close relation with the sleep disorders of the patient and the clinical course. In one study, sleep measurements in only schizophrenic patients with atypical antipsychotic risperidone (N = 5) or only conventional antipsychotic haloperidol (N = 5) revealed a significant difference in the slow-wave sleep of the 2 groups. Slow wave sleep was detected in 27% of patients receiving risperidone and 20% in haloperidol group. This was the only significant difference between the two groups (p < 0.05). In our study, the rate of slow wave sleep in patients who used risperidone was 14.14% at 1 month and this rate increased to 20.74% at 6 months.
Risperidone can prolong the amount of slow wave sleep in patients because it has a higher affinity for serotonin 5-HT2 receptors than haloperidol. 5-HT2 receptors have been reported to play a role in controlling sleep quality. Another atypical antipsychotic olanzapine also has a high affinity for 5-HT2 receptors. Therefore, while the antipyretic effect of some antipsychotic drugs has a negative effect on patients, atypical antipsychotics such as risperidone and olanzapine may have the potential to improve sleep quality in individuals. Aripiprazole is an antipsychotic agent used in the treatment of schizophrenia with partial agonistic activity at 5HT1A receptors and antagonistic activity at 5HT2A receptors and dopamine-2 (D2) receptors. In patients with aripiprazole use at the first month of the treatment and at the 6th month of the treatment, the total sleep time and sleep efficiency, sleep latency and waking time were decreased, while there was an increase in sleep time and sleep rate, while this difference was not statistically significant. To date, no polysomnographic studies have been published on the effects of aripiprazole on sleep patterns of healthy subjects and schizophrenic patients. In this respect, the data we obtained about aripiprazole in our study which examined the sleep structures of non-affective first-episode psychosis patients will contribute to the literature.
In our study, the effects of risperidone, olanzapine and aripiprazole on the sleep structures of the first episode psychosis patients, which are frequently used in clinical practice, have been examined. Results in; risperidone and olanzapine had a statistically significant positive effect on sleep continuity and structure, and aripiprazole did not show a statistically significant change on sleep.
KEYWORDS: psychosis; atypical antipsychotic; sleep; sleep structure; polysomnography
Table 1. Patient group using risperidone.
Table 2. Patient group using olanzapine.
Table 3. Patient group using aripiprazole.
[Abstract:0307] [Schizophrenia and other psychotic disorders]
The effect of psychosocial interventions on the clinical course of individuals with schizophrenia
Ercan Doğu Selmaa, Kayıhan Hülyab, Erdi Fundaa, Örsel Sibela and Karadağ Hasana
aDepartment of Psychiatry, University of Health Sciences, Ankara, Turkey
bDepartment of Occupational Therapy, Hacettepe University Faculty of Health Sciences, Ankara, Turkey
ABSTRACT
Introduction: Schizophrenia is a chronic disease that causes difficulties in the functional, social, family and work life of individuals. The positive, negative and cognitive symptoms of the disease make it difficult for the individuals to perform their daily life activities and the individuals have problems in social participation independently. Developing skills to cope with these problems and gaining new skills is important for the functionality of these individuals. Studies show that psychosocial interventions contribute to increase the compliance to treatment and the reduction of psychopathological symptoms of individuals with schizophrenia. Occupational therapy aim to improve well-being and health in individuals with schizophrenia through activity. Occupational therapy enables the use of activities to develop, improve and maintain daily life activities, working and leisure skills of individuals with a physical, mental or developmental problem. It is a client-centered process in which the desires and needs of individuals are prioritized. Occupational therapy intervention programs that applied individually or as a group and life skills trainings have been found to be associated with improvement in negative symptoms and progress in social functioning in individuals with schizophrenia. From this point of view, the aim of this study is to compare the effects of psychosocial intervention programs on the clinical symptoms in individuals with schizophrenia.
Methods: The study included 60 individuals followed in Ankara Dışkapı Training and Research Hospital between the ages of 18-59. Individuals who were diagnosed with schizophrenia according to DSM-5, who did not have mental retardation or organic brain disease, had no alcohol / substance abuse or dependence and were not hospitalized in the last six months were included in the study. As psychosocial interventions, social skills training (SST) was applied to one group and social skills training with occupational therapy intervention (SST+OT) was applied to the other group. Individuals were divided into groups equally and homogeneously. The SST+OT program included communication and problem-solving skills, planning skills of daily living activities and recreational skills. In addition to routine treatment follow-up, it consisted of 16 sessions lasting 50 minutes per week. In addition to the routine treatment, the SST program, which consisted of 10 sessions of communication and problem solving skills lasting 50 minutes per week, was applied to the social skills training group. The effect of both interventions on psychopathology was compared. Before, after the interventions and at 6 months follow up, Sociodemographic Data Form, Brief Psychiatric Rating Scale (BPRS), Negative Symptoms Assessment Scale (SANS), Calgary Depression Scale for Schizophrenia (CDSS) were administered.
Results: The mean age of the patients was found to be 38.90 ± 8.89. 23 (38.3%) of the patients were female and 37 (61.7%) of the patients were male. 12 (20%) of the patients were married, 43 (71.7%) were single, 5 (8.3%) were divorced. Of the patients 9 (15%) were from primary school, 12 (20%) were from secondary school, 28 (46.7%) were from high school, 11 (18.3%) were from university graduates. There was no significant difference between the groups in terms of sociodemographic data and clinical scales at baseline. In order to compare the measurements of both of the groups before, after the intervention and 6 months follow-up, 2-way analysis of variance was used for repeated measurements. Table 1 shows the mean scores, standard deviations, F and p values of the participants in both groups, SST group and SST+OT group, obtained before, after the intervention program and follow-up. According to the results of 2-way analysis of variance for the repeated measures, the effect of time (Wilks λ = .203, F (2,116) = 153.388; p = 0.000) and Time x group interaction was found to be statistically significant on the BPRS scale score (Wilks λ = .898, F (2,116) = 3.643; p = .035). According to the results of the variance analysis for the repeated measurements, the change in time (Wilks λ = .828, F (2,116) = 153.388; p = 0.005) was significant in terms of depression score, whereas the effect of interaction between time and group was not statistically significant (Wilks λ = .897, F (2.116) = 2.935; p = 0.072). According to the results of 2-way analysis of variance for the repeated measures, the effect of time (Wilks λ = .064, F(2,116) = 438.844; p = 0.000) and Time x group interaction was found to be statistically significant on the total score of SANS scale (Wilks λ = .810, F(2,116) = 10.247; p = 0.000).
Discussion: According to the results of our study, there was a decrease in general psychiatric symptoms, depressive symptoms and negative symptoms at the end of each intervention. In the follow-up, general psychiatric symptoms and negative symptoms continued to decline. In literature, researches on this topic support the notion that psychosocial skills training results in a decrease in the negative symptoms of schizophrenia. Psychosocial skills training decreases symptom severity in schizophrenia patients and reduces the rate of comorbidity, such as substance use. Xiang and colleagues (2006) conducted a study with 96 schizophrenia patients that received routine psychiatric outpatient care and in addition 50% of the patients also received psychosocial skills training and the other 50% received supportive counseling, each for the duration of 6 months. They stated that the psychosocial skills training group improved significantly more in terms of psychiatric symptoms and social functioning [1].
We compared the groups in terms of psychosocial intervention, it was seen that there was a change in terms of psychiatric symptoms and negative symptoms in both groups; this change was more in the social skills training with occupational therapy group. When the literature on the effect of occupational therapy interventions on disease symptoms is examined; individual-centered occupational therapy studies and life skills training were found to lead to improved clinical and negative symptoms. Foruzandeh and Parvin (2013) compared the effect of the occupational therapy program (30 subjects) on the clinical symptoms of the disease in individuals with schizophrenia with the routine treatment group (30 subjects). The occupational therapy program consisted of expressive, artistic activities and recreational activities. An activity program was planned, which was structured according to the individual and where individuals applied their chosen activities. The program was conducted as 3 hours per week for 6 months. As a result of the study, a significant improvement was found in the positive and negative symptoms of the individuals compared to the control group [2]. The lack of an interest of individuals with schizophrenia and the inability to perform daily living activities (ADL) effectively and in a routine may lead them to focus more on the symptoms and to bring complaints about the symptoms in the interviews. Regulating the ADL with occupational therapy interventions, teaching to finding something they can do and learning what they can do may lead to decreasing to focus on symptoms. Occupational therapy interventions in schizophrenia do not focus directly on the treatment of clinical symptoms, but rather aim to increase individuals’ social participation, quality of life and well-being. Our study findings are consistent with the literature. As a result of a review by Perilli and colleagues (2018) comparing the impact of occupational therapy interventions and social skills training in social participation in people with schizophrenia, the authors concluded that both interventions were largely beneficial [3]. When the literature is reviewed, there is limited number of studies comparing occupational therapy program with social skills training. Therefore, this study is the first study in our country in terms of addressing occupational therapy interventions with social skills training.
We assume that findings of our study support that occupational therapy is essential in psychosocial therapy interventions of schizophrenia.
Table 1. BPRS, CDSS, SANS Scores Mean, Standard Deviations, F and p values by group and time
[Abstract:0336] [Addictions]
Needs of addicted patients who applied to addiction treatment centers
Karakaya İbrahima, Sacakli Gamzeb, Bilici Rabiac and Ogel Kultegind
aDepartment of Psychiatry, Cappadocia University, Nevsehir, Turkey
bGeneral Directorate of Health Services, Ministry of Health, Ankara, Turkey
cDepartment of Psychiatry, Erenkoy Research and Training Hospital for Psychiatry, Istanbul, Turkey
dDepartment of Psychiatry, Moodist Hospital, Istanbul, Turkey
ABSTRACT
Introduction: Substance addiction has become a common public health problem which negatively affects the mental and physical health of the individuals, family relations, quality of life, economic and social situation and leads to significant problems in almost every societies [1–2].
According to European Monitoring Center for Drugs and Drug Addiction [3] there has been a rapid increase in the number of dependent patients admitted to the clinic for treatment in Turkey reports.
A rapid increase of drug addiction in Turkey brings various imperatives that need solutions. Many treatment centers (AMATEM) have been opened in different provinces to examine, prevent and treat alcohol and substance addiction. In our country where the number of patients and addiction treatment centers have increased rapidly, many new studies related to addiction have been published. In these studies, psychosocial causes of addiction and other psychological variables related to dependence [2–4], sociodemographic characteristics, frequency and type of substances used have been revealed [5–9]. However, there are not enough studies in the literature which focus on the psychological, social and economic needs of the patients who applied for treatment in treatment centers.
The aim of this study was to determine the psychological, economic and social needs of the patients who applied to Alcohol and Drug Addiction Treatment and Research Centers (AMATEM).
Methods: This study was carried out with patients who applied to AMATEMs (Adana Dr. Ekrem Tok Mental Health and Diseases Hospital, Manisa Mental Health and Diseases Hospital, Elazığ Mental Health and Diseases Hospital, Samsun Mental Health and Diseases Hospital, Gaziantep 25 Aralık State Hospital, Konya Training and Research Hospital) between 2017 and 2018. The ethics committee approval was obtained from Erenköy Mental and Neurological Diseases Training and Research Hospital Clinical Research Ethics Committee. Male and female patients among 18 - 70 ages who are being treated for alcohol and substance addiction will be included in the study. Patients who have inadequate education level, mental retardation, dementia or physical and psychiatric disorders that lead to create difficulties to response questions in the survey, who are under 18 years old, who receive addiction treatment in their first week or have concentration or distraction problems and who are still in the delirium are excluded in the study. A sociodemographic form and a structured self-report questionnaire consisting of 30 items assessing psychological, social, informational and financial needs of patients was given to all participants. Informed consent forms were obtained from all participants. Data were analyzed with descriptive statistics in SPSS ™ database.
Results: A total of 328 patients (314 male, 9 female and 5 unresponsive) were included in the study. The mean age of the participants was 30.4 ± 10.1 years, and the age range was between 18- 69. 48.8% of the participants had secondary school degree while 23.3% high school, 12.9% primary school, 5.8% illiterate, 8% associate degree / bachelor's degree and 1.2% had no education. 56.2% of the participants were single, 32.4% were married, 7.4% were divorced, 2.2% were living separately and 0.3% were widowed.
While 48.6% of the participants had an occupation, 32.6% did not define themselves in any occupations. 48.3% of the participants had an income, while 51.6% did not have sufficient income. 82.4% of the participants were living with their families and 78.3% of them stated that there was no housing problem after treatment.
83.5% of the participants had an inpatient treatment while16.5% of them had an outpatient treatment. 42.1% of the participants reported using of more than one substance, while 30.1% used only opiate and 15.5% used alcohol. 39.8% of the participants had problems due to alcohol and substance for 0-5 years, 31.2% for 6-10 years, 19.4% for 11-20 years, and 6.9% for more than 20 years.
66.7% of the participants stated that they had sufficient knowledge about the physical and mental damage of alcohol and substance, 57.1% of them had legal consequences and 49.1% of them had sufficient knowledge about how to get rid of addiction. 64.9% of the respondents thought that their families had partial or adequate knowledge about alcohol/drug addiction, while 35.1% stated that their families had no sufficient knowledge. 67.1% of the participants stated that they received moral supports from their families and 60.3% of them received financial supports.
44% of the participants have problems with their spouses or partners and 48% have problems with their relatives. 45.7% of the participants stated that they did not know how to prepare CV and 76.1% had problems in managing budget. 55% of the participants did not have a hobby and 84.8% did not have a regular sports habit. 68.9% of participants stated that they need support for changing the social environment.
Discussion: In this study, the majority of the participants consisted of inpatients, middle school graduates, unemployed and male adults. More than one substance (42.1%), opiate (30.1%) and alcohol (15.5%) were frequently used by the participants. According to TUBIM (2018) the majority of patients in treatment centers in Turkey was more than one substance and opiate users [10].
The aim of this study was to determine the economic, psychological and social needs of patients had drug/alcohol addiction. In this respect, the participants’ knowledge about alcohol and substance, their attitudes towards addiction, their interpersonal relations, their economic conditions, their social and cultural activities, their daily functioning, their psychiatric and physical illnesses were assessed.
Occupation, working status, income and education level are important factors determining socioeconomic status (SES) and evaluating the economic needs and quality of life of the participants [11]. Substance addiction is a disorder affects human health directly or indirectly is also considered as an important risk factor in substance addiction [11]. According to the results, 68.3% (n = 159) of the participants had a secondary education level or below. 32.6% (n = 100) of participants did not have an occupation, 65.8% (n = 212) did not have regular income. 58.1% (n = 186) of participants also stated they did not have a work after treatment. These results, which are consistent with the findings of other studies in the literature, indicate that substance addicts’ participation in social, vocational and educational life has important role on the treatment of addiction [12]. It has been shown that employment is an effective predictor of treatment in achieving positive results, low rate of relapse and crime [13–14]. For this reason, it is thought that social studies and policies such as creating occupation, new jobs and education opportunities will decrease the relapse rates while increasing the patients’ SES, quality of life, participation in social life [15].
Psychological, economic and social support from family or relatives is effective at every stage of substance dependence [16]. In this study, patients stated that they received social and economic support from their families during the treatment process. On the other hand, it was seen that a great majority of them had various problems with their families, spouses or relatives. Therefore, informing the families of the patients about substance dependence, giving trainings on how to approach patients and providing psychotherapy services are seen as important needs [16–17].
Daily routines such as budget allocation, preparing a CV, communication skills, physical exercise, social activity, daily chores and cooking are important needs in terms of self-efficacy and social functionality [2]. According to the findings of this study, the majority of patients experience deficiencies in CV preparation, physical exercise, and participation in social activities, budget allocation and culinary works. Considering the prognosis of drug addiction, patients are gradually moving away from social life due to individual and social reasons such as social isolation, exclusion, stigmatization, unemployment and lack of self-confidence in the substance use and treatment process [18]. Therefore, psychosocial rehabilitation to increase the social functioning and psychological well-being of the patients, increasing the number of social facilities and centers in which patients can explore their own areas of interest and spend their free time are important needs in the treatment of substance dependence [17–19].
The easy access of the dependent patients to the treatment centers, health workers and the social groups supporting addiction treatment are important for the continuity of the treatment and relapse prevention. According to the results, 38.1% (n = 120) of the participants could not reach to treatment centers easily when they needed, 54.8% (n = 135) of them were not able to find a place in AMATEMs for inpatient treatment and 59.6% (n = 87) of them had difficulties in accessing support groups easily. Social and medical services that help to patients to access treatment centers and support groups easily was seen as important need. Public or private health care institutions are required to carry out studies that will meet these needs of patients and it is thought to be beneficial in the continuation and success of treatment.
Any psychiatric or physical illness accompanied by addiction are important in the case of the formulation of treatment for patients. In this study, 18.9% (n = 61) of the participants had physical diseases and 18.6% (n = 60) had psychiatric diseases. Considering these findings, it is necessary to develop and implement medical treatment and psychotherapy techniques for physical and psychiatric diseases of addicted patients.
[Abstract:0355] [Mood disorders]
Dynamic thiol/disulphide homeostasis as a novel oxidative stress marker to differentiate bipolar and unipolar depression: a machine learning case study
Erzin Gamzea, Özkaya Güvenb, Topçuoğlu Cananc, Yüksel Rabia Nazikd, Erel Özcane and Göka Erold
aPsychiatry Department, Ankara Dışkapı Training and Research Hospital, Ankara, Turkey
bSchool of Medicine, Biostatistics Department, Uludağ University, Bursa, Turkey
cBiochemistry Department, Ankara Numune Training and Research Hospital, Ankara, Turkey
dPsychiatry Department, Ankara Numune Training and Research Hospital, Ankara, Turkey
eBiochemistry Department, Yıldırım Beyazıt University, Ankara, Turkey
ABSTRACT
Introduction: Bipolar depression (BPD) and unipolar depression (UPD) are complex and multifactorial mental disorders characterized by mood swings, disability, and impaired quality of life [1]. Although, there are significant differences in bipolar depression compared to unipolar depression, such as the addition of mood stabilizers to treatment, and the fact that many antidepressants are not preferred as the first option, there are not a biomarker to differentiate the two disorders. Previously, we examined thiol disulphide homeostasis in order to find out whether thiol disulphide would be a trait or a state marker for mania period and remission period in patients with bipolar disorder [2]. In this study, we aimed to compare thiol disulphide balance of bipolar disorder - depressive episode (BPD) and unipolar depression (UPD) with healthy controls to determine whether there are differences in oxidative indicators involved in UPD and BPD. In the literature, machine learning has become an new instrument for providing with predictive analysis for studies in the psychiatry field [3]. Therefore, another objective of our study is applying two different decision tree machine learning algorithms to find out if it is possible to classify these disorders with using data concerning thiol disulphide balance.
Methods: All the participants were interviewed by an experienced clinician according to the Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders, fifth version (DSM–5). Healthy control group members, who were between between 18 and 65 years old, showed no evidence of any present or previous psychiatric disease. The Hamilton Depression Rating Scale (HAM-D) and Young Mania Rating Scale (YMRS) were also used to support the diagnoses of depression (i.e., HAM-D ≥8 or YMRS score <7). Our study was approved by the ethics committee of the Ankara Numune Training and Research Hospital. Each patient and one of their first-degree relatives as well as controls signed a written consent. A 5 cc of venous blood was collected from each participant. Blood cells were separated from serum and the samples were stored at -80°C. Biochemical analyses were performed on these samples. Body Mass Index (BMI) was measured for each patient. Weight and height of the patients were measured. BMI was calculated with kg/m2 formula. The exclusion criteria were antioxidant treatment or vitamin supplementation history for 6 months prior to inclusion, pregnancy, mental retardation, obesity, previous electroconvulsive therapy (ECT) history, history of alcohol or drug dependence or traumatic head injury, any past or present major medical or neurological illness, having any systemic or metabolic disease and any additional psychiatric disorder or mental retardation.
Biochemical tests
Fasting blood samples were collected from each participant in plain tubes. Serum samples were separated after centrifugation at 1300 g for 10 minutes and stored at –80°C until thiol disulphide homeostasis tests were performed. After the native and total thiols were determined, disulphide amounts, disulphide/total thiol percent ratios (SS/SH+SS), native thiol/total thiol percent ratios (SH/SH+SS), and disulphide/native thiol percent ratios (SS/SH) were calculated (used modified Elman reagents for thiol measurement).
Statistical analysis
The data was examined by the Shapiro Wilk test whether or not it presents normal distribution. Normally distributed data are presented as means with standard deviation and were compared with a two-sample t test and One-way ANOVA. Non-normally distributed data are presented as medians with minimum and maximum, and were compared using the Mann-Whitney U and Kruskal Wallis tests. Categorical variables were compared using Pearson's chi-squared test and Fisher-Freeman-Halton test. Correlations between variables were tested using Pearson and Spearman correlation coefficients. p < 0.05 was considered as significance levels. Statistical analyses were performed with IBM SPSS ver.23.0 (IBM Corp. Released 2015. IBM SPSS Statistics for Windows, Version 23.0. Armonk, NY: IBM Corp.).
Predictive analysis
The data was analyzed using two decision tree machine learning algorithms implemented in the H2O artificial intelligence platform. Gradient boosting machine (GBM) and distributed random forest (DRF) supervised learning algorithms were used to classify bipolar depression, unipolar depression and control groups considering their data about thiol disulphide homeostasis. Before the analysis the data set was splitted to two as 70% for training set and 30 for validation set. While running the algorithms k-fold cross validation, where k was 5, was also applied in order to randomly validate results across the data set.
Results: 37 BPD (23 female, 14 male), 24 UPD (15 female, 9 male) and 50 control patients (30 female 20 male) were included in the study; no significant differences in terms of age and sex were found in the three groups. Average age (mean ± standart deviation) is 38.4 ± 10.7 years for BPD group, 40.6 ± 14.1 years for UPD group and 37.2 ± 9.8 years for the control group. Median HAM-D score is 11/8-40 (median/min-max) for BPD group and 13/8-32 (median/min-max) for UPD group. There is also no significant difference between these groups in terms of HAM-D scores (p = .795). No significant difference was also obtained between BPD and UPD groups regarding smoking (packet-year) (p = .315).
There were not any difference between BPD and UPD groups in terms of serum native thiol level (p = .518), serum total thiol level (p = .081), disulphide level (p = .132), disulphide/native thiol ratio (p = .494), disulphide/total thiol ratio (p = .491), native thiol/total thiol ratio (p = .489). In terms of serum disulphide levels, disulphide/native thiol, disulphide/total thiol and native thiol/total thiol ratios, there were statistically significant difference between BPD and control group (respectively p = .015, p = .001, p = .001 and p = <.001). In terms of serum disulphide levels, disulphide/native thiol, disulphide/total thiol and native thiol/total thiol ratios, there were statistically significant difference between UPD and control group. (respectively p = <.001, p = <.001, p = <.001 and p = .001). Native thiol level was statistically significantly lower in BPD group than control group (p = .009).
In the predictive analysis part both machine learning algorithms presented at least 70% accuracy in classifying three groups existing in the data set. Both algorithms classified bipolar depression patients with 0.27 error rate. GBM classified unipolar depression patients with 0.12 error rate while DRF classified the same group with 0.25 error rate. Control group was classified by the GBM and DRF algorithms with 0.14 and 0.12 error rates respectively (Figure 1).
Discussion: The level of thiol as an antioxidant parameter has been previously examined in a variety of disorders in psychiatry. Most of these studies, however, are aimed at showing the oxidative degradation in these disorders. According to our knowledge, This is the first study to evaluate whether there is a significant difference between BPD and UPD in terms of oxidative stress by evaluating the thiol disulphide homeostasis. In both unipolar depression and bipolar depression groups, disulphide levels were found to be higher and native thiol levels were found to be lower respectively compare to healthy control groups. In our previous study, thiol and native thiol levels were found to be lower in bipolar disorder patients during mania and remission period, while there was no difference between these two groups in terms of disulphide levels compared to healthy controls. This led to the conclusion that the cause of thiol loss may be related to nutrition rather than oxidative damage [2]. In this study, it was found that the native thiol value was low and the disulphide value was high which might be an indication that there is an increase in oxidative stress in patients with bipolar and unipolar depression patients compared to healthy controls. Whereas, there was no significant difference in thiol/disulphide balance between BPD and UPD which may imply that there is a common oxidative damage in both disorders.
Machine learning is a fundamental computer science technique that recently applied many areas of science including psychiatry. One of the few studies in the literature was concentrated on prediction of short-term outcome of autism spectrum disorders [3]. In our study, we used supervised machine learning algorithms to classify patients with BPD and UPD according to their thiol/disulphide balance parameters. Use of this method in similar studies may lead formation of a literature which could inspire designing more studies using machine learning. of Further studies with larger data sets might help enhancing the accuracy of machine learning in the field of psychiatry.
Limitations of our study are failure to eradicate other oxidative stress related variables such as smoking for control group. We have a small group of participants for this study. Since we could not include the untreated patients in our study, we could not evaluate the effects of the drugs on the patients. This can be stated as another limitation of our study. Detection of oxidative molecules for BPD and UPD can be helpful in reducing morbidity especially in treatment and follow-up periods. Although there is not enough evidence yet, results of our study may imply that thiol and disulphide levels could be oxidative markers for BPD and UPD and also therapeutic targets in terms of future pharmacological trials. However, to better understand the relationship between oxidative stress and BPD and UPD, there is a need for further studies.
Table 1. Decision tree machine learning algorithms’ classification performance
[Abstract:0412] [Psychopharmacology]
Society and physician response to developing psychiatry: changes in preschool children within 15 years
Dag Pelin, Güler Aksu Gülen and Akdere Dogdu Pinar
Department of Child and Adolescent Psychiatry, Mersin University, Mersin, Turkey
ABSTRACT
Introduction: The major milestone of modern psychopharmacology was the discovery of chlorpromazine that named as 4560 RP in 1951, followed showing favorable effects of chlorpromazine in various psychiatric disorders by Jean Delay and Pierre Denikel. Since then, rapidly developing psychiatry science has gained important clues about the pathophysiology of psychiatric disorders through the support of modern technology. These developments provide an inspiration for developing of both psychopharmacology and psychotherapy methods for the treatment of these disorders. The possible side effects of the first agents were perceived as frightening by society and therefore the society's perspective on psychiatry had been adversely affected. It is expected that the negative point of view of the society to psychiatry can be broken by developing agents have higher effect while causing less side effects and increasing availability of the psychotherapy methods, especially in the last 25 years.
Still, the idea of interfering with a developing organism, differing pharmacokinetic and pharmacodynamic effects of all pharmacological agents in childhood from adults, possible and frightening side effects of these agents, the difficulties of applying drugs to children enforce clinicians. These challenges get more compeller for preschool children.
We aimed to examine the changes on applying to clinic in the community and approaches of child and adolescent mental health professionals, in the last 15 years.
Methods: The data of all, 0–6 years old children who applied to Mersin University School of Medicine Hospital Child and Adolescent Psychiatry outpatient clinic between the years of 2002 and 2004 and between 2016 and 2018 collected retrospectively from the medical reports of the patients. The data from the patients applied between the years of 2002–2004 was accepted as the earlier group and the data from the patients applied between the years of 2016–2018 was accepted as the late group. Thusly, two groups created. Only the data from the first visit were evaluated. The sociodemographic data such as age, gender, schooling, families’ educational status, families’ health status, the major complaints of the patients, the diagnoses they received by the first visit and the prescribed agents during the first visit were compared between the groups. There was no exclusion criteria for 0–6 age patients.
The normality control of continuous data was made by Shapiro Wilk test. Student's t-test was used to determine the difference of the mean age between the groups. Chi-square test was used to analyze the categorical data. Paired comparison test used to analyze two categories that have significant correlations. The statistical significance value was accepted as 0.05 in all analyzes.
Results: 540 patients who applied to the clinic between 2002 and 2004 and 1353 patients who applied between 2016 and 2018 and thusly a total of 2082 patients who were 0–6 years old were included in this study. As a result of the analysis, the rate of applying to the clinic in the 0–6 age group increased by 2.3 times in 15 years. In both groups, the majority of the patients were male. While the age at admission to the clinic was significantly decreased, the application of family with a low level of education had increased significantly. The rate of schooling was higher in late group. The rate of parents without any psychiatric disorders was higher in late group.
The referral to the clinic for consultation was significantly increased. The most common complaints were determined as speech problems (31%), general behavioral problems (13.7%), mobility (10.6%) and irritability (10.5%) in the earlier group; on the other hand the most common complaints were speech problems (28.9%), mobility (12.1%), general behavior problems (11.9%) and irritability (11.6%) in the late group. There was no significant difference between the rates of most common complaints. Although the rate of diagnosing as normal psychiatric evaluation, attention deficit and hyperactivity disorder (ADHD) or oppositional defiant disorder (ODD) were significantly increased in late group; the rate of any speech disorder was significantly decreased. Autism and developmental delay rates were similar among the groups.
When the rates of prescribing pharmacological agent treatment were examined, it was increased from 14.1% to 22.9%. While most frequently prescribed pharmacological agents were risperidone (36.3%), thioridazine (26.4%), fluoxetine (13.2%) in the earlier group, they were risperidone (76.9), fluoxetine (14.1%), methylphenidate (4.8%) in the late group. While the prescribing of risperidone was found to be significantly increased among the groups, there was a significant decrease in the prescribing of typical antipsychotics and antihistaminergic agents. There was no significant difference between the rates of fluoxetine or methylphenidate prescription.
Discussion: In the last 20 years, child-centered family structure has been increasingly assumed by societies with changing psychiatric paradigms. Now, the fact of many psychiatric disorders, which were formerly attributed only to adulthood, can be seen or begin in childhood has a solid scientific basis, so this may lead to families to be more sensitive for behavioral problems in childhood and thusly make them seek much more and earlier professional support. The increasing of the rate of admission to clinic for consultation without any psychiatric complaints can be explained by decreasing prejudices against psychiatry science. Furthermore, the increasing of the rate of applications from families have lower levels of education, can support increment of the acceptance of possible psychiatric disorders by a wider population of society.
In this study, the number of visits to the psychiatry clinic found increased dramatically, while the referral age decreasing. However, the general complaints of the patients are similar. Nevertheless, the patients were more likely to have attention deficit and hyperactivity disorder or oppositional defiant disorder diagnoses. This may be explained by sensitization of families and teachers to behavioral signs due to increasing the expectation of adaptation to the rules of collective life in this age group depending on increased school enrollment rate before age 6. While the rate of complaint for speech problem remained unchanged between the groups, decreasing of diagnosing with any speech disorder (speech sound disorder, speech fluency disorder in childhood) or delayed language development, indicates families to be more sensitive to deviations which are variants of normal.
On the other hand, according to the results of this study, the rate of detection of developmental delay or autism extension disorders was not changed over the years. This shows severe psychiatric disorders, which significantly effect functionality, force the parents to seek help at all times.
The increasing psychopharmacological knowledge creates significant changes in treatment choice of mental health care professionals. Despite similar efficacy, more acceptable side effect profiles raise preferabilities of atypical antipsychotics to typical antipsychotics, particularly in childhood. Having relatively well known data about on, the possibility of benefiting from some side effects (sedation, appetizing), high therapeutic effect, availability of oral solution form providing ease of use in childhood cause risperidone to be more preferred [2]. Also positive reports for risperidone on treatment of ADHD or ODD in preschool period increase prescribing of risperidone for preschool children.
It is a striking and thought-provoking finding of this study is that one of the most commonly prescribing agents for the treatment of psychiatric disorders in preschool children 15 years ago is not used today. The new generation of antipsychotic agents, named as atypical antipsychotics, was discovered in 1959 by the discovery of clozapine, but they were started to be developing in the 1990s. One of these agents, risperidone, has found extensive usage in child and adolescent psychiatry clinics with its wide range of efficacy. In recent years, usage of risperidone is raising due to increasing in the number of studies showing the effectiveness of risperidone for many different psychiatric disorders or symptoms. Many studies have reported this founding to be valid in 0-6 years old preschool children in accordance with our study [3]. But then, considering the average of human life and time of atypical antipsychotics in use, we may say these agents are quite new. Therefore, cognizing the possible effects of commonly prescribing antipsychotics in different developmental periods of brain may be the most important step to preventing serious side effects that can have an impact on children's health into adulthood.
On the other hand it is known that preschool children can be more sensitive to side effects of antipsychotics’ than adolescents or adults. Currently, there is limited knowledge about the long-term effect of exposure to antipsychotics on developing brain [4]. Moreover, there is not satisfactory data about long term outcomes of known side effects such as hyperprolactinemia of these agents [5]. When all of these issues are considered, it is needed to following-up of patients treating by these agents, which are commonly used during a sensitive brain developing period such as preschool age, meticulously, running long-term and large-sample studies, and increasing cumulation of literature on these agents for this period.
At last, it is a highly predictable truth that developing psychiatry science will continue to affect both mental health professionals and society about psychiatric disorders. The advance of public awareness, as well as the development and implementation of more acceptable treatment strategies, is an important step for increasing the sensitivity to the symptoms of childhood psychiatric disorders, raising the conscious and unconscious acceptability of the situation and thereby early recognition of psychiatric disorders. In addition, the psychopharmacological treatment strategies that applied on the preschool period, that brain develops rapidly, are also affected by these developments. It should be accepted that the scientific literature for the agents preferred for this age group needs to be expanded. Therefore, the science of psychopharmacology that effects on rapidly developing brain must keep pace with the speed of the developing brain.
KEYWORDS: childhood; psychopharmacology; risperidone
[Abstract:0488] [ADHD]
Effects of stimulants on body mass index and sleep in children with ADHD
Turan Serkana, Aydın Zeynepb and Pekcanlar Aynur Akayb
aÖdemiş State Hospital, İzmir
bDokuz Eylul University Child and Adolescent Pyschiatry Unit, İzmir, Turkey
ABSTRACT
Introduction: Sleep problems in children with ADHD are frequently reported. Delay of falling asleep, night waking, morning awakening problems, daytime sleepiness, snoring, parasomnias and night terror are common sleep problems in ADHD [1]. It has been suggested that the interaction between ADHD and sleep is related to hypo-arousal condition (similar to narcolepsy), delayed sleep onset latency, respiratory-related sleep problems, restless leg syndrome and epilepsy / EEG interictal discharges [2]. However, in sleep studies with both subjective and objective sleep tools, a consistent result has not yet been found.
Decreased appetite is the most frequent adverse event of stimulants, but it is not necessarily related to a decrease in height (Harstad et al. 2014). The association between stimulants and a delay in growth is still unclear and a focus of controversy.
Our study aims to evaluate the effects of methylphenidate (MPH) on sleep parameters and the effects of the chronic impact of methylphenidate (MPH) on BMI in these patient group and compared with healthy children.
Methods: The clinical sample consisted of children with a history of 51 ADHD cases who applied to Dokuz Eylul University Child and Adolescent Psychiatry Outpatient Clinic after the ethics committee approval was obtained. Six participants for whom missing or erroneous entries in the data collection instruments were excluded from the study. The Sixty-five children who were appealed to our pediatrics outpatient clinic by parents for causes such as headache, acute infections but did not meet any diagnostic criteria effectuates healthy sample group. Finally, the data was collected on the total 110 cases that were subjected to statistical analysis.
After the participants who were included in the study were informed about the aim and method of the research, written consent was obtained from both groups. Height, weight and body mass index measurements of ADHD cases were obtained from hospital records. The participants who were appreciated with K-SADS-PL by blinded professionals completed a data form containing questions regarding sociodemographic and clinical features, Wechsler Intelligence Scale for Children-Revised (WISC-R) and Conners Parent Rating Scale-Revised Short Form (for only ADHD cases to support the diagnosis), The Pittsburgh Sleep Quality Index (PSQI) and Children's Sleep Habits Questionnaire (CSHQ)-Abbreviated Form (all participants).
Sociodemographic Data Form: It is an information form filled by the researchers to obtain information about age, gender, education, family type, socioeconomic level, home conditions, status of parents, background and family history.
Conners Parent Rating Scale-Revised Short Form (CPRS-RSF): This form is widely used for the assessment of the prevalence of ADHD and its effect on diagnosis and treatment. Studies on the new version are described in U.S., and Canada. Apart from this, CPRS-RSF has been used in different cultures such as Germany, Australia, China, England, Switzerland, Spain, Cuba and Malaysia. The validity and reliability study of the scale was conducted by Kaner (2013).
The Pittsburgh Sleep Quality Index (PSQI): PSQI; It was developed in 1989 by Buysse et al. and Cronbach's alpha = 0.80 to adequate internal consistency has been shown to have test-retest reliability and validity (Buysse, Reynolds, Monk, Berman and Kupfer,1989). The validity and reliability study of the PSQI in our country was conducted by Ağargün et al. (1999). In this study, Cronbach's alpha value was found to be 0.79 (Cronbach alpha = 0.79). The PSQI is a self-report scale that assesses sleep quality and disorder over a period of one month.
Children's Sleep Habits Questionnaire (CSHQ)-Abbreviated Form: The Child Sleep Habits Questionnaire (CSHQ) Abbreviated Form, developed by Owens et al in 2000 to examine the sleep habits and sleep related problems of children, consists of 33 items. Eight subscales have been defined in the scale such as bedtime resistance, delay of falling asleep, sleep duration, sleep anxiety, night waking, parasomnia, disturbance in sleep, sleepiness during the day. The scale was completed retrospectively by the parents. Parents are asked to evaluate their sleep habits over the previous week. As a cut-off point of the GHQ, the total score of 41 is accepted and the values above this are considered to be clinically significant. The questionnaire also includes three open-ended questions about the child's sleep habits (the time of bedtime, the length of sleep during the whole day, the time when he wakes up at night).
Statistical Analysis: Differences in all study variables were analyzed by using the Statistical Package for the Social Sciences (IBM, NY), version 22 for Windows. Before the statistical analysis was performed, it was checked whether the data met the assumptions of the parametric tests and the normal distribution and homogeneity of variance by using the Shapiro–Wilk test. Variables that don’t show normal distribution were evaluated by Mann-Whitney U test. In the interpretation of the variables, descriptive statistical techniques and quantitative data analysis were used. Chi-square analysis was used to compare categorical variables between groups. The Pearson Correlation Test was used to determine the direction and level of correlation between the variables and the results were indicated by r (correlation coefficient) and p value (significance level). P < 0.05 was considered statistically significant.
Results: Forty-five patients with ADHD and 65 age and sex matched control groups were included in the study. 35 (77%) of the patients with ADHD and 47 (72%) of the control group were male.
Table 1 summarizes first and last visit follow-up body mass index points, WISC-R intelligence test scores, mean methylphenidate duration of use months and mean methylphenidate doses of ADHD cases. Table 2 summarizes the total and subscale scores of ADHD and control subjects from The Child Sleep Habits Questionnaire (CSHQ) Abbreviated Form. A significant difference was found between the two groups in terms of sleep delay, sleep duration, daytime sleepiness scores and total sleep scores (p < .05). There were no differences in other sub-tests between bedtime resistance, sleep breathing problems, sleep anxiety, night waking and parasomnia scores (p > 0.05).
Total and subscale scores of participants from The Pittsburgh Sleep Quality Index (PSQI) are reported in Table 3. All of the subscales, except use of sleep medication were higher in ADHD group. Total score and subscales about sleep latency, sleep disturbance and subjective sleep quality were significantly different (p < 0.05). There was no significant difference in scores of sleep duration, sleep efficiency and daytime dysfunction.
Discussion: In this study, we found that sleep problems are more common in ADHD group. With the idea that sleep changes may be due to ADHD drugs (especially stimulants) in children with ADHD, studies have shown that these drugs are only one of the causes of sleep disorders in ADHD and children have more sleep problems than controls, independent of ADHD treatment [3]. Nevertheless, the stimulants used in the first step caused sympathomimetic effects by increasing the amount of extracellular dopamine and noradrenaline, and thought to reduce the sleep awareness and fatigue awareness. The results of our study are one of the most common side effects associated with insomnia or sleep-stimulating drugs, delayed for more than 30 minutes, consistent with the literature.
In contrast to the previous studies, stimulant drugs contributed positively to the body mass of the case sample. This is because; limited number of samples, short follow-up period and not calculated z values. In some studies about stimulant drugs used in the treatment of Attention Deficit Hyperactivity Disorder, although it has been reported that it may cause a delay in growth in children, it has been shown that although the most common side effect of stimulants, there is not any effect on height. For this reason, stimulant and growth retardation is still a controversial issue. Some studies report a negative impact on height (Lisska and Rivkees 2003; MTA Cooperative Group 2004; Charach et al. 2006; Swanson et al. 2007; Faraone et al. 2008; Powell et al. 2015); some studies emphasize that they did not make significant changes (Biederman et al. 2003, Harstad et al. 2014).
There are several limitations in our study. Relatively small number of the cases, using self-evaluation of the scales in the study, the fact that objective measurement tools such as polysomnography, actigraphy and MLST could not be included in the study are among the limitations of the study. Further studies need to evaluate whether this higher incidence of sleep problems is due do methylphenidate use or the common etiology with ADHD.
KEYWORDS: Methylphenidate; attention-deficit/hyperactivity disorder; sleep; body mass index; child
Table 1. Characteristics of participants.
Table 2. Means and standart deviations of the Child Sleep Habits Questionnaire (CSHQ) Abbreviated Form total and sub-scores of ADHD and the control group.
Table 3. Means and standard deviations of the Pittsburgh Sleep Quality Index (PSQI) total and sub-scores of ADHD and the control group.
[Abstract:0489] [DEHB]
Arterial spin labeling evaluation of children with ADHD
Baytunca Muharrem Buraka, Frederick Blaiseb, Suren Serkana, Bacanli Alia, Yazici Kemal Utkua, Ongur Dostc, Ozyurt Onurd and Ercan Eyup Sabria
aDepartment of Child and Adolescent Psychiatry, School of Medicine, Ege University, Izmir, Turkey
bMcLean Imaging Center, Department of Psychiatry, Harvard University, Belmont, MA, USA
cDivision of Psychotic Disorders, McLean Hospital, Harvard Medical School, Belmont, MA, USA
dBogazici University Teknopark, Istanbul, Turkey
ABSTRACT
Introduction: Attention deficit hyperactivity disorder is a neurodevelopmental disorder with a prevalence of 3% to 5% among children. Thus far, researchers have reported abnormalities in medial and orbitofrontal, parietal, cingulate cortices during the cognitive tasks in functional magnetic resonance imaging (fMRI) studies. Arterial Spin Labeling (ASL) is utilized to quantify brain tissue perfusion by using labeled arterial blood as an endogenous tracer. Increased rCBF during the resting state ASL scan was found in the left caudate, inferior/medial frontal gyrus and bilateral cingulate gyrus and precuneus in adult subjects with ADHD relative to controls (O’Gorman et al., 2008). Further, increased rCBF in the right-sided frontoparietal areas including medial (BA8, 9) and inferior frontal gyrus, occipital gyri (BA18), bilateral anterior cingulate (BA32) was reported in several ASL studies utilizing with sustained attention and vigilance tasks (Kim et al., 2005; Lim et al., 2009). However, these prior studies were conducted on adults and most did not include ADHD subjects. To the best of our knowledge, this is the first event-related ASL study comparing children with ADHD and control subjects in the literature. In our study, we hypothesized areas implicated in the dorsal and ventral attention networks (right hemisphere dominant frontal, parietal areas) might show abnormal activation in children with ADHD relative to the control counterparts.
Methods: Subjects were required to be between the ages of 8 and 18 years old, right-handed, free of any psychiatric and medical comorbidity, possess an intelligence quotient (IQ) score above than 80, and be drug-naive. The control subjects were required to be free of any psychiatric disorder in addition to the aforementioned criteria. Subjects were required to respond to go cues as fast as they can while also withholding from responding when the no-go cue is presented. The image analyses were performed by FEAT (fMRI Expert Analysis Tool) Version 6.
Results: In the present study, the male-to-female ratio was 12/5 in the control group and 19/1 in the ADHD group (p = 0.075). The mean age of control and ADHD groups were 10.88 ± 1.45 and 11 ± 1.91, respectively (p = 0.112). The mean WISCR results of control and ADHD groups were not also found statistically different (115 ± 11.11 vs. 110 ± 16.70, p = 0.882).
Behavioral results: The subdomains of the ADHD scale rated by parents statistically differed between the groups. The mean inattention score was 13.80 ± 4.49 in the ADHD group and 1.35 ± 2.76 in the control group (p < 0.000). The hyperactivity-impulsivity score was 11.50 ± 8.75 in the ADHD group and 0.82 ± 1.59 in the control group (p < 0.000). The mean oppositional defiant disorder score was 3.30 ± 4.30 in the control and 0.70 ± 1.21 in the ADHD group (p = 0.024). The mean inattention subscale score by teachers was 14.0 ± 6.24 in the ADHD group and 0.94 ± 1.88 in the control group (p < 0.000). The mean hyperactivity-impulsivity score was 10.70 ± 7.94 in the ADHD group and. 0.70 ± 1.21 in the control group (p < 0.000). The mean oppositional defiant disorder score was 2.70 ± 4.76 in the ADHD group and 0.11 ± 0.48 in the control group (p = 0.187).
Imaging results: When combining the go and no-go conditions, the between-group analyses contrasting the ADHD and control groups revealed statistically significant activation in the right anterior cingulate cortex (BA32) extending to the right medial frontal gyrus BA 10 and BA 11 from the voxel-based analysis. Notably, no brain areas were found to be more greatly activated in control subjects over their ADHD patient counterparts.
Go task results: The voxel-based analysis revealed no significant activation difference between the groups. However, when a lenient cluster threshold (2.3) was employed, three activation clusters were identified in those with ADHD. The first cluster included right superior parietal lobule (BA7) and right precuneus. The second cluster was comprised of right middle frontal (BA10) and inferior frontal gyrus. The last cluster included the right-sided temporal lobe (BA42), inferior parietal lobe (BA40) and supramarginal gyrus. The control group showed no greater activation than the ADHD group in any brain region at the threshold of 3.1 or 2.3.
No-go task results: Again, we failed to find any brain activation differences between groups at the voxel-based analysis level. When the cluster threshold was decreased to 2.3, left precuneus (BA7) and right cuneus and precuneus (BA19 and BA7) areas showed statistically significant activation in the ADHD group when compared to the control group.
Discussion: This is the first event-related ASL study comparing children with ADHD to healthy counterparts in the literature. The most striking finding of the present study was the increased rCBF in the right anterior cingulate cortex (ACC) (BA32) and right middle frontal cortex (BA 10, 11) in the ADHD group during the go/no-go task. It has been reported that ACC engages with attention allocation, conflict resolution, novelty detection and response inhibition. Prior research revealed that the right MFG is the area modulating the linkage of dorsal and ventral attention systems. Consistent with this, we found the right middle frontal gyrus to be significantly activated in children with ADHD relative to control subjects during go/no-go task in the present study. In a meta-analysis of fMRI studies that also implemented the go/no-go paradigm, rMFG was shown to display greater activation in children with ADHD relative to healthy controls. Researchers in several SPECT studies have also reported decreased rCBF in the right MFG (BA10 and 11), middle temporal gyrus, and the bilateral cerebellum as well as increased rCBF in the posterior brain areas during resting state in children with ADHD (Kim et al, 2002; Lee et al, 2005). The present study suggests that those with ADHD might exhibit greater rCBF increase in the right-sided ACC and MFG in order to maintain the attention demanded by the go/no-go task.
The dorsal attention network engages with goal-driven stimuli during a given task. Its core regions are the dorsal parietal cortex (particularly superior parietal cortex and intraparietal sulcus) and dorsal frontal cortex near precentral gyrus in each hemisphere (Corbetta et al). In our study, subjects were required to produce and maintain their endogenous attention signal in order to hit the button across go trials, a task that which mainly involves the dorsal attention network. Although we were not able to see any statistically significant difference between the diagnostic groups when applying a cluster significance threshold of 3.1, a more lenient threshold of 2.3 enabled us to observe consistent findings with this hypothesis. It is worth noting that the use of 3.1 as a significance threshold is a recent development due to Eklund's work in BOLD fMRI (Eklund et al, 2016). It has yet to be established whether the higher threshold is necessary for ASL analyses. In order to explore this, we repeated our analysis using permutation testing and this would seem to indicate that non-Gaussian shaped spatial autocorrelation is not the problem in ASL data that it is in BOLD fMRI, so 2.3 would seem to be the appropriate significance level for ASL analyses using FLAME. This deserves further study.
We identified three right-sided core clusters in the superior parietal lobe (BA7), middle/inferior frontal gyrus, and temporoparietal areas – including the posterior transverse temporal lobule (BA42), inferior parietal lobule (BA40) and supramarginal gyrus – in children with ADHD during the go session. It should be cautiously noted that the two latter clusters are within the ventral attention network. The ventral network consists of the temporoparietal junction, supramarginal gyrus and middle/inferior frontal gyrus, as well as the frontal operculum and anterior insula. The ventral attention network is activated along with the dorsal attention network when a behaviorally relevant, rather than distinctive but unimportant stimuli stimulus, is presented (Corbetta et al, 2008). In a visual sustained attention task-integrated ASL study, researchers have reported greater activation in the right middle frontal gyrus (BA8,9) bilateral occipital gyrus (BA18), right cuneus (BA18) and the left cingulate gyrus (BA32) when compared to the resting state in adults (Kim et al., 2005). Additionally, a significant rCBF increase was reported in the right middle/inferior frontal gyrus, right inferior parietal lobe, during a sustained attention task in an ASL study. In the same study, the authors reported that increased pre-task resting state rCBF in the rMFG was associated with worse performance during the cognitive task. Demeter reported increased activation in the right middle frontal gyrus and parietal during sustained attention task via ASL scan. Therefore, the activated brain regions involved in both dorsal and ventral network systems during the go/no-go paradigm in our study were consistent with and expanded upon these preexisting findings.
Importantly, we identified significant activation in the left precuneus extending to the right precuneus and bilateral cuneus during the no-go condition with a lenient threshold (2.3). The left precuneus was reported to be a cross-network connector between the default and dorsal attention networks. Several neuroimaging studies have indicated that the precuneus co-activates in concert with lateral parietal areas for visually guided behavior, attention shifting and spatial attention. Notably, it was also stated that the left precuneus co-activates within the default mode network during resting state but enhances its activity during a given task. With a similar but not identical neuropsychological task (go, no-go and lure condition), Wang reported increased activation in precuneus during the no-go task in children with ADHD when compared to the control subjects. Therefore, the increased rCBF in the bilateral precuneus in children with ADHD during the no-go trials might be related to the response inhibition and shifting attention.
One of the major limitations of this study was the lack of resting state CBF quantification, which prevented us from comparing the baseline rCBF patterns in children with and without ADHD. Our study did not enable us to observe the any potentially dynamic response of the deactivated areas during the go/no-go task.
In sum, we found that children with ADHD displayed increased rCBF in the right anterior cingulate cortex (BA32) and MFG (BA10 and 11) relative to control subjects during a cognitive attention task. Additionally, we observed increased rCBF in the dorsal and ventral network-associated parietal areas in these child ADHD patients relative to their counterparts. These results indicate that children with ADHD needed to over-activate their dorsal and ventral attention network-related regions to compensate for the attention demand by a given task.
Figure 1. Anterior Cingulate Cortex (right) and medial frontal cortex (right) are the identified areas showing greater activation in children with ADHD relative to control counterparts.
Table 1. Socio-demographic and behavioral results of the diagnostic groups.
Table 2. The ASL comparison of the diagnostic groups during entire scan.
Table 3. The ASL contrast of the diagnostic groups during go pairs.
Table 4. The ASL contrast of the diagnostic groups during no-go pairs.
[Abstract:0501] [Schizophrenia and other psychotic disorders]
Reduced blood agmatine level in early-onset schizophrenia
Baytunca Muharrem Buraka, Kalyoncu Tugbaa, Ozbaran Burcua, Kose Sezena and Ongur Dostb and Uzbay Tayfunc
aDepartrment of Child and Adolescent Psychiatry, School of Medicine, Ege Universitesi, Izmir, Turkey
bMcLean Hospital, Harvard Medical School, Belmont, MA, USA
cNeuropsychopharmacology Research and Application Center (NPARC), Uskudar University, Istanbul, Turkey
ABSTRACT
Introduction: Agmatine is a polyamine which is synthesized from L-arginine by the arginine decarboxylase enzyme. Given the neurophysiological effects of agmatine in the central nervous system (CNS), this molecule may play a role in certain CNS disorders. Agmatine possesses several physiological features which suggest it may be a novel neurotransmitter.1,2 Like many other neurotransmitters, agmatine is produced in neurons, storage in synaptic vesicles and released by the Ca+2 dependent depolarization in the axon terminal. Moreover, the physiological effects of agmatine are terminated by neuronal uptake.3,4 Agmatine blocks ligand-gated cation channels, particularly of the NMDA subclass, and has an affinity to imidazoline and α2 adrenoceptors.3,5 Agmatine also inhibits/regulates nitric oxide (NO) synthase (NOS), which results in decrement of NO production and subsequent neurotoxicity.6–10 These notable neurophysiological functions and interactions of agmatine have raised concern regarding its involvement in the pathogenesis of several CNS disorders.2
The underlying neurobiological mechanisms of schizophrenia are poorly understood. The hypofunction of NMDA glutamate receptors is proposed to be one responsible mechanism; neurodegenerative processes may also be involved.11–13 Agmatine's interaction with NMDA receptors and neuroprotective effects have led researchers to examine the involvement of agmatine in schizophrenia pathogenesis. Neuronal NO is a molecule which may induce neurotoxicity and increased NO radicals are found in postmortem brain tissues in patients with schizophrenia.14,15 NO is an enhancer of NMDA receptor function.16 The activation of NMDA receptors is accompanied by increased formation of NO and increased NO release.17 The NO that is produced diffuses back to the presynaptic neuron where it enhances the activity of glutamate cyclase and cGMP.18 Administration of an NO donor in schizophrenia patients was also shown to acutely reduce symptom severity.19 From this perspective, the regulation of NOS by agmatine may be directly and indirectly related to schizophrenia pathophysiology. Lower levels of agmatine may give rise to increased NOS radicals which result in neurotoxicity or in the reverse direction higher level of agmatine may contribute to the hypofunction of NMDA by inhibiting production of NO and its downstream actions.
Agmatine itself blocks ligand-gated NMDA receptors and deteriorate NMDA receptor functioning.3,5 However, in a recent postmortem study, Liu reported no change in the total NOS activity in brain tissue of schizophrenia subjects whereas agmatine level was increased.20 There are conflicting reports on the role of agmatine in animal models21–23 and patient studies.20,24
In the present study, we aimed to examine blood agmatine level in adolescents experiencing a first psychotic episode. We hypothesized that blood agmatine level might be significantly differ from their healthy control comparisons.
Methods
Subjects: This study was approved by the Ethical Committee of Ege University School of Medicine. Participants and their legal guardians provided written consent forms. Inclusion criteria for adolescents with the first psychotic episode were: being under 20 years of age and drug-naive, absence of substance use history or major medical disorders (including neurological disorders), possessing clinically normal IQ and lack of any psychotropic drug use. These criteria were the same for healthy subjects, except for lack of having any psychiatric disorder. Psychiatric evaluation of all subjects was depended on Diagnostic and Statistical Manual for Mental disorders (DSM)-V.25 The severity of psychotic attack was assessed by the Scale for the Assessment of Positive Symptoms (SAPS). Blood sampling was obtained during the psychotic episode. Subjects were followed up at least six months to confirm the diagnosis of early-onset schizophrenia. Blood sample from the subjects were first stored in lithium heparinized tubes after phlebotomy, and then centrifuged at 10.000 rpm for 15 minutes. Supernatant plasma was then transferred to cryotubes. These samples were stored at −80 refrigerator until to be analyzed.
Laboratory measurement of blood agmatine level
Standards and Reagents: The reference standards of agmatine sulfate salt and 1,6-diaminohexane (as an internal standard-IS) were all obtained from Sigma Aldrich. Heptafluorobutyric acid (HFBA) was obtained from Sigma Aldrich. Methanol [HPLC grade] and acetic acid were provided from Merck [Germany].
LC-MS/MS Condition: Liquid chromatography separation was performed on Agilent 6410 B LC-MS/MS system. A SHIM –PACK XR-ODS column (75 mm*3.0 mm, 2.2 um) were held at 30 C. Chromatographic separations was achieved with gradient elution using a mobile phase composed of 0.05% heptafluorobutyric acid (HFBA) in water (A) and 0.05% heptafluorobutyric acid (HFBA) in methanol (B). The HPLC gradient program was as follows: 20% B →20% B at 0.01–2.00 min; 20% B →50% B at 2.01–4.00 min; 50% B at 4.01–6.00 min; 20% B at 6.01–9.00 min. The flow rate was set at 0.4 mL min−1 with a sample injection volume of 30 ul. Mass spectrometry was performed using an Agilent 6410 triple quadrupole mass spectrometer [Agilent Tech., Switzerland] equipped with an ESI source. The multiple reaction monitoring [MRM] mode was employed for the determination of Agmatine and 1,6 –diaminohexane (as an internal standard) due to its high selectivity. The specific precursor-to-ion transitions monitored were m/z 131.1 → 72.21, m/z 117.1→100.1 for agmatine, and IS respectively. The dwell times used were 0.05 s. Collision-induced dissociation [ CID] was carried out using nitrogen. The collision energy was 10 and 15 eV for agmatine and IS. The fragmentor voltage was set at 80 and 90 EV respectively in the positive-ion mode. Nitrogen was used as desolvation [10 L/min] and nebulizer pressure 50 psi [40 L/h]. The source and desolvation temperatures were optimized and kept at 350°C. The system was controlled by Agilent MassHunter Workstation B.01.04 software, Agilent [Switzerland].
Preparation of stock solutions and calibration standards: Stock solution of agmatine was prepared in methanol (0.20 mg mL−1). The stock solution of agmatine was diluted with methanol: water [30: 70, v/v] to achieve a working standard solution at the concentration of 0.41 ug mL−1. This working standard solution was used in the preparation of standard and quality control samples. The stock solution of internal standard was prepared in methanol (1 ug mL−1). The internal standard working solution was prepared by diluting this solution to 100 ng mL−1 in methanol: water [30:70, v/v]. All solutions were stored at 4°C until required. Appropriate volumes of these stock solution were spiked to blank plasma to prepare eight effective calibration standard and quality control samples. The calibration standard samples included concentrations of 3.06, 5.10, 10.20, 20.40, 40.80, 61.20, 81.60 and 102.00 ng/mL for agmatine. The quality control samples included concentrations of 15.30, 51.00 and 81.60 ng/mL for agmatine.
Preparation of plasma samples: To 0.5 ml plasma sample was added 100 µl of IS working solution, 50 ul methanol: water (20:80 v/v), 600 ml 0.1% acetic acid in methanol for liquid-liquid extraction. Each sample vortex-mixed for 3 min at 15.000 rpm. The supernatant was transferred to another tube and followed by evaporating to dryness at 30°C under the stream of nitrogen. The residue was dissolved in 100 ul methanol, and 30 microliters were injected automatically onto LC-MS/MS system.
Data analysis: IBM SPSS version 20 was utilized to perform statistical comparisons. Assumptions of normality were tested and validated. Sociodemographic variables were contrasted with χ2 (chi-square) test and independent sample t test was employed to compare blood agmatine levels between-groups. The correlation of agmatine level and SAPS score was performed using Pearson correlation.
Results: In the present study, 18 adolescents with schizophrenia (8 males/10 females) and 12 healthy controls (3 males/9 females) were included. No significant difference was found concerning gender distribution (p = 0.442). The mean age was 17.00 ± 3.08 in schizophrenia group and 15.75 ± 0.62 in healthy counterparts (p = 0.180). The blood agmatine level (mean ± SD) was detected as 4.04 ± 2.34 ng/ml in schizophrenia group but 9.11 ± 1.18 ng/ml in healthy controls (F = 8.01, t = −6.88, p = 0.008, one-tailed). Total SAPS score was 24.06 ± 1.86 in schizophrenia group and no correlation was found between the mean SAPS score and blood agmatine level (r = 0.425, p > 0.05).
Discussion: In the present study, in contrast to our previous study24, we found that blood agmatine levels to be statistically lower in patients with schizophrenia than their healthy counterparts. As detailed in Introduction, agmatine is a molecule that has notable interactions with NMDA receptors. It was found that agmatine blocks cation channels of NMDA receptors and reverse glutamatergic transmission in a physiological antagonistic manner.26 It is known that hypofunction of NMDA receptors is responsible for some symptoms of schizophrenia27–29, therefore, it is plausible that the agmatine reduction might be a compensatory mechanism against the NMDA receptor hypofunction.
In some studies, agmatine levels was measured in the acute phase of the experiments, but no data were presented with regard to the alteration of prolonged agmatine administration. Knox and colleagues reported that acute administration of PCP (a molecule that mimics schizophrenia-like symptoms) in rats resulted in a significant decrease of endogenous agmatine levels in the hippocampus but not prefrontal cortex, which partially consistent with our study.30 In the present study, we noted a decrease in blood agmatine levels in human participants, whereas Knox's found this finding in PCP induced psychotic condition in rats. Surprisingly, in the same study, the authors observed that metabolic pathway of L-arginine and NOS activity shown to be altered from its natural machinery following PCP treatment. Thus, L-arginine and its metabolites (i.e., agmatine), as well as NOS activity, seem to dynamically respond to PCP treatment.30 One should consider that agmatine is a subcomponent of a complex and multidirectional pathway related to glutamatergic transmission. Thus, it is still not clear whether agmatine (directly or indirectly) mediates NMDA receptor functioning or decrement in agmatine levels is a compensatory mechanism.
On the other hand, since agmatine is an inhibitor and regulator of NO by blocking NOS enzyme, therefore, low level of agmatine might cause an increment in NO levels. Consistent with this hypothesis, blood NO level was found to be higher in schizophrenia subjects, and this association was found to be correlated with episode frequency and disease heritability.31,32 Researchers also reported increased neuronal NOS expression in prefrontal cortex of those with schizophrenia.14,15,33,34 In addition to the lack of a clear conclusion of whether abnormalities in NO and its pathway is a result or cause of schizophrenia, we still do not have sufficient data to suggest if agmatine may be a regulator on this mechanism of action. However, in the present study, NO level was not measured in subjects, and this was a limitation of the study to draw a conclusion.
The age effect on agmatine levels is an important issue to be discussed. In the present study, we identified statistically lower agmatine levels in adolescents with schizophrenia. This finding is notably different from Uzbay's study who reported increased agmatine levels in adults with schizophrenia. Unfortunately, the effect of age on blood agmatine levels for humans is still not well understood. Researchers have reported increased and decreased agmatine levels with age in various brain regions in animal studies.35–38 In another human study, agmatine levels were reported to be significantly lower in autistic children relative to control counterparts.39 Recently, researchers reported significantly lower levels of agmatine in post-mortem-brain tissue of adults who committed suicide.40 However, there is still no study assessing the long term fluctuations/course of agmatine in humans. Therefore, the contrary result of our study to the previous agmatine level in adult schizophrenia study might be related to age dependent alterations in agmatine. Future studies evaluating the long term course of agmatine may fill this gap in the literature.
In conclusion, blood agmatine level found to be decreased in adolescents experiencing the first psychotic attack in comparison to healthy controls. This decrement may be a compensatory mechanism in reaction to NMDA receptor hypofunction given the blockade effect of agmatine on this receptor. Since NO seems to be an enhancer of NMDA receptor and agmatine inhibits the production of NO this may be another mechanism to restore weakened glutamatergic transmission in the result of NMDA hypofunction. It should be noted that administration of NO donors reduces psychosis severity in rats41 and schizophrenia patients.42 Further, reduction in agmatine level, in the long run, may result in loss of control in NO production, which subsequently can cause neurotoxicity and the establishment of psychosis. Further studies assessing long-term fluctuations of agmatine across the psychotic course and its dynamic association with the other elements of this pathway (i.e., NO, L-arginine) are warranted.
Figure 1. Blood agmatine levels in diagnostic groups (mean agmatine level was 4.04 ± 2.34 ng/ml in schizophrenia subjects and 9.11 ± 1.18 ng/ml in healthy controls, p = 0.008).
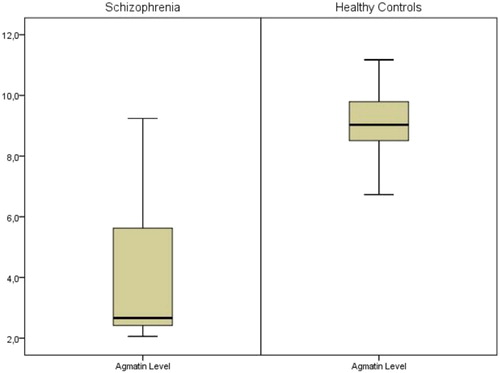
Acknowledgements
Authors would like to thank to Pharm. Selma Özilhan for her kind contributions for measuring agmatine levels in blood samples. This study was funded by Ege University, Scientific Research Projects (fund number: 15-TIP-066). The authors of the study declare no conflict of interest.
[Abstract:0537] [Mood disorders]
The expression of emotion and coping with stress in major depressive disorder patiens with somatic symptoms
Gök Fulyaa and Eroğlu Meliha Zenginb
aDepartment of Psychiatry, Kocaeli Derince Research and Training Hospital, Kocaeli, Turkey
bDepartment of Psychiatry, Haydarpasa Numune Research and Training Hospital, Istanbul, Turkey
ABSTRACT
Introduction: Depression is one of the most important problems affecting public health due to its prevalence, sustainability, disability and economic consequences. It is common for depression to be manifested by somatic complaints rather than other mood symptoms. Studies on the association of depression and somatization suggest that more somatic symptoms may be associated with more severe mood disorder, and that this association may complicate the diagnosis and treatment of both conditions. However, expressing feelings and thoughts after the troubled events positively affects both mental and physical health; suppressing feelings and thoughts creates a negative effect. Non-functional strategies used to cope with life problems can also be triggers for somatic or psychological symptoms. The aim of this study was to evaluate the somatic symptoms of the patients with Major Depressive Disorder (MDD) who applied to our outpatient clinic and to examine the relationship between these symptoms with emotion expression styles, coping attitudes, depression and anxiety levels and to compare them with the healthy control group.
Methods: 74 patients who consulted Haydarpasa Numune Research and Training Hospital between August 2017 and October 2017 and were diagnosed with MDD according to DSM-5 and 73 healthy control group patients were included in the study. All the participants were evaluated with Psychosomatic Symptoms Subscale of Rosenberg's Self-Esteem Scale (R-SES), Emotional Expression Styles Inventory (EESI), COPE Inventory, Beck Depression Inventory (BDI) and Beck Anxiety Inventory (BAI).
SPSS 22.0 statistical package program was used for statistical analysis. Pearson's chi-square test and Fisher Exact test to compare categorical data; t-test to compare scales between groups; in the case of two groups Independent samples t test, in case of more than two groups One way ANOVA test to examine the relationships between the scales with sociodemographic characteristics in the group and LSD test to determine the group that cause the difference; Pearson Correlation analysis to determine relationships between the scales; Linear Regression analysis was used to examine the effect of independent variables on dependent variable. The results were evaluated at 95% confidence interval and p < 0.05 significance level.
Results: In our study, 55% (%74.3) of the patient group was female and 19% (%25.7) of them was male while 47% (%64.4) of the control group was female and 26% (%35.6) of them was male.
When the correlation between the scales in the patient group has been analysed, the results have shown that as the R-SES score increases, so does the BDI and BAI scores. As the score of the self-focused expression of happiness and reflecting sadness and anger on one's face increases, the BDI scores too; the score of self-focused and other-focused manifestation of happiness and verbal expression of rage increases in reverse proportion to the BAI score; as the score of the use of beneficial social support, active coping, planning, positive reinterpretation and development increases, the score of BDI decreases; the score of ignoring in behavioural terms and substance abuse increases in direct proportion to the BDI score. As the score of problem-focused and emotion-focused coping increases, the BDI score decreases and as the non-functional coping score increases, so does the BDI score. As the score of refraining increases, the BAI score too. Moreover, the score of non-functional coping increases in direct proportion to the BAI score.
As the self-focused manifestation of happiness increases, the R-SES score decreases and as the aggressive expression of sadness and anger increases, so does the R-SES score. The result of the regression analysis that has been carried out in our study to assess the correlation between emotional expression and psychosomatic symptoms is that the level of the patients’ self-focused expression of happiness decreases the level of psychosomatic symptoms (ß = −0.767; t = −2.325; p = 0.023). When emotional expression variables along with depression and anxiety levels have been added to the analysis, the BAI level of patients has been found to increase the level of psychosomatic symptoms (ß = 0.290; t = 5.436; p = 0.000) while the levels of depression and emotional expression has been found not to affect the level of psychosomatic symptoms significantly (p > 0.05).
After the correlation between COPE subscales and R-SES subscale scores in the patient group has been evaluated, it has been found that as the score of the use of beneficial support, positive reinterpretation and development, the use of emotional and social support increases, the score of R-SES decreases and as denial and substance abuse increase, the R-SES score too. Therefore, when considered in general terms, as the non-functional coping score increases, so does the R-SES score. As a result of the regression analysis that has been carried out in our study in order to determine the correlation of COPE subscales to psychosomatic symptoms, the levels of patients’; focusing on the problem, revealing emotions, accepting and substance abuse have been discovered to increase the psychosomatic symptoms (ß = 0.637, t = 2.225, p = 0.030; ß = 0.741, t = 2.445, p = 0.018; ß = 0.554, t = 2.446, p = 0.018), and it has been indicated that other coping strategies does not affect the level of psychosomatic symptoms significantly (p > 0.05). When COPE variables together with the levels of depression and anxiety have been added to the analysis, it is seen that the substance abuse and acceptance attitudes of the patients increase the levels of psychosomatic symptoms (ß = 0.480, t = 2.601, p = 0.012; ß = 0.550, t = 2.438, p = 0.018), and the attitude of suppressing other engagements decrease the levels of psychosomatic symptoms (ß = −0.457, t = −2.185, p = 0.033). Whereas the level of BDI in the patients does not affect the level of subscales significantly (p > 0.05), the level of BAI increases the level of psychosomatic symptoms (ß = 0.320, t = 6.336, p = 0.000). So, in this case it is seen that other COPE subscales do not influence the levels of psychosomatic symptoms significantly either (p > 0.05).
Discussion: It is known that most of the depressive disorder patients present with somatic symptoms rather than mood symptoms, somatic symptoms and emotional distress are generally associated and highly correlated with each other. In this study, we aimed to evaluate the relationship between somatic symptoms, emotion expression and stress coping styles and the relationship between these parameters in the depressive patient group and compare them with healthy controls.
One of the most important results in our study is the relationship between emotion expression and somatization. Psychosomatic symptoms decreased with increasing expression of happiness; psychosomatic symptoms increased with the aggressive expression of sadness and anger. It has been shown that the level of depression decreases with the expression of happiness and expressing sadness and anger to the other side verbally, level of depression increases with reflecting on the face and hiding sadness. In our study, regression analysis conducted to determine the relationship between emotion expression and psychosomatic symptoms showed that patients’; level of self-focused happiness expression was predictive of psychosomatic symptom level and decreased psychosomatic symptom level. These results show that the emotions expressed in the positive way will enable the mental distress to be experienced without somatization and to be easily recognized by physicians. In our study, it is seen that as the use of social support which is one of the problem-focused coping strategies, positive reinterpretation and development and emotional support which are two of the emotion-focused coping strategies increase, psychosomatic symptoms decrease while as non-functional denial and substance abuse in coping increase, the psychosomatic symptoms increase too. In addition, it has been shown that depressive patients used attitudes that were dysfunctional and more exhibited as avoidance behaviours than healthy controls when dealing with stress, these patients exhibit functionally accepted problem-focused and emotion-focused coping strategies. While depression levels are lower in those who exhibited problem-focused and emotion-focused coping behaviours, depression levels of those who preferred non-functional attitudes are significantly higher. Because of regression analysis to determine the relationship between coping strategies and psychosomatic symptoms, it has been discovered that focusing on the problem and predicting emotion, acceptance and substance use are predictors of psychosomatic symptoms and these attitudes increased the level of psychosomatic symptoms. From these results, it is understood while actively coping with the problems led us to solve the problem; avoidance behaviours are not functional and current stress manifests itself through bodily complaints.
In our study, it has also been shown that the levels of depression and anxiety increase as psychosomatic symptoms increase too, in short, if the individual expresses the negative emotions and thoughts in somaticized state, the severity of the disease is higher. Consistent with the literature, somatic symptoms are more closely related to the level of anxiety than depressive symptoms.
When depression and anxiety levels were added to the regression analysis to evaluate the relationship between emotion expression and coping variables with psychosomatization showed that anxiety level of patients increased the level of psychosomatic symptoms; depression level did not significantly affect the level of psychosomatic symptoms. As mentioned in the past literature, one of the most important predictors of somatization is anxiety.
In conclusion, these findings support the association of somatic symptoms with emotion expression and coping with stress in MDD patients. Somatic symptoms are considered the most common symptoms in the depressive patient group, and it is even suggested that depression with somatic symptoms is the most common type of affective disorder in the community. The suppression of emotions makes the patients with depressive disorder see the doctor in a more somaticized condition. The widespread occurrence of somatization of mental distress in collectivist cultures, including Turkey, increases the importance of this issue. However, dysfunctional avoidance attitudes that have been chosen to cope with the stress caused an increase in somatic symptoms. We believe, it will be beneficial that treatments related to the expression of emotions and functional attitudes, especially problem focused approaches, in dealing with stress in the management of depression patients, where physical complaints are predominant.
[Abstract:0579] [DEHB]
Counselors’ knowledge about attention-deficit/hyperactivity disorder and learning disability
Doğru Hicran and Esin İbrahim Selçuk
Department of Child and Adolescent Psychiatry, Ataturk University, Erzurum, Turkey
ABSTRACT
Introduction: Attention deficit hyperactivity disorder (ADHD) affects approximately % 5-10 children and manifests in childhood with symptoms of hyperactivity, impulsivity, and/or inattention. The symptoms affect cognitive, academic, behavioral, emotional, and social functioning [1]. Learning disability is a neurodevelopmental disorder which can interfere with learning basic skills such as reading, writing and/or math. Attention-Deficit/hyperactivity disorder (ADHD) and Learning disorders (LD) are complicated disorders with accompanied by a lot of symptoms. In order to cope with the symptoms, children need continuous support from parents, teachers, and school counselors. The aim of this study was to evaluate the knowledge of counselors about the features of ADHD and LD and to determine the nature of a sample of these counselors knowledge and misperceptions with regard to ADHD and LD.
Methods: Sampling of this study is chosen from the teachers who work in all types of schools which work dependent upon National Education Directorship of Administrative Province, in Erzurum. 113 school counselors were included in the study. A short questionnaire was prepared about ADHD and LD, which has the option of filling the spaces and marking multiple choice question. A short socio-demographic data form were filled out. The socio-demographic part consisted of open-ended questions having children, concerning degrees, years of teaching experience, etc. Teachers also rated their self-confidence to interfere a child with ADHD and LD effectively, by means of a 6-point scale. And a 28-question survey was written and tested. This part concerned personal opinions about the interventions for problems and marking in multiple choice questions. These questions survey that teachers’ knowledge and misperceptions of ADHD and LD in three specific areas: symptoms/diagnosis of ADHD and LD, general knowledge about the nature, causes and outcome of ADHD and LD and possible interventions with regard to ADHD and LD, which was also examined in the present study. The detailed parameters were evaluated during the study. For comparison of normally distributed variates Student t-test was used.
Results: 113 cases were included in the study. The current educational level of the all participants was a four-year teaching diploma. The mean age of the patients was 28.5 ± 9.4. A total of 69 patients were female (61.1%) and 44 patients were male (38.9). There was a significant differences between female and male ages (p = 0.021). While the rate of teachers working area in the city center was 54% (n: 61), the percentage of teachers working area in the periphery was 46% (n: 52). Mean number of students assisted by teachers were 382.7 ± 48.8. Mean duration of teaching year was 5.7 ± 2.4 years. Mean number of having child was 1.47 ± 1.1. A total of 56 (49.6%) patients were married and 55 patients were single (48.7%). While the majority of participants 89 (%n: 100) responded suitably about the pathophysiology of ADHD, 11% (n: 13) responded that there was no ADHD disease.
The results were interpreted as follows: Correct responses represent knowledge about ADHD and LD, whereas don't know responses reflect a lack of knowledge. Incorrect responses indicate misperceptions. The results of this questionnaire suggest that there is a substantial lack of knowledge about ADHD and LD among counselors.
The correct response percentages of teachers about ADHD and LD treatment was respectively 91.2% and 45%. Therefore, it can be said that counselors have more knowledge about ADHD treatment than LD treatment. Also, 72% of the teachers (n: 81) responded that the group which is the most benefited from individual training is DEHB while 28% (n: 32) of the teachers responded that the group which is the most benefited from individual training is LD.
In the present study, 28% of the respondents incorrectly believed that increasing dietary intake of sugar or food additives will effectively increase the symptoms of ADHD.
In the literature, when adolescents with ADHD are compared with non ADHD children, those with ADHD are at higher risk for school suspension, academic failure, dropping out of school and substance abuse [2]. However, in this study, 16% of the counselors reported that they believed that ADHD treatment was associated with increased risk for addiction.
Teachers indicated that they had very little or no training in ADHD or LD. Teachers responded that the most of their knowledge was acquired through what is portrayed about ADHD or LD in media reports and internet, which is often incorrect and not based on scientific research.
When the participants were asked about the frequency of the diagnosis of ADHD; 22% was associated with doctors extreme diagnosing, 56% was associated increase in awareness, 11% was associated with the use of chemical agents, 12% was associated with inappropriate parental attitudes.
The results of this study suggest that there is a substantial lack of knowledge among counselors in certain key areas of ADHD or LD. For example, 12% of the counselors indicated that they believed that there was no ADHD disease. This lack of knowledge is a matter of concern since counselors play an important role in the recognition, intervention, referral and treatment of ADHD. The results of this study show that, teachers need adequate support training on ADHD or LD. Because these disorders manifest itself in many different symptoms and it is not easy to address them appropriately. When we asked for the strategies to the counselors, they have reported some useful and following answers; Seating the student near the teacher's desk, Splitting longer assignments into smaller segments, providing more breaks during class time, creating opportunities for movement throughout the day, using some statements like “first/then” vs … (the results will be shared in detail during the oral presentation.)
Discussion: ADHD and LD is a neurodevelopmental disorder that can persist throughout life. These diseases are a risk factor for other psychiatric comorbidities if it continues in adulthood. Symptoms of ADHD and LD vary across tasks and settings. Especially children diagnosed with ADHD work best on tasks that they have chosen themselves and that they find interesting. In addition, the most benefited from individual training is LD. In this study, it was seen that the counselor teachers did not have sufficient equipment about recognition, intervention, referral and treatment of ADHD and LD. This situation can have an important impact on the academic and social life of a child and also it can be reflected in child's whole life.
The results of this questionnaire suggest that there is a substantial lack of knowledge about ADHD and LD among counselors. But they are especially stabilized to serve as a key intermediary between parents and teachers. Also, counselors can be essential in helping students with ADHD and LD thrive. It is very important that ADHD or LD manifests itself in many different ways, so counselors should be equipped with adequate in these common diseases. Adequate training efforts are required for teachers to enhance their equipment. Further research is required for the structure of adequate training efforts.
[Abstract:0074] [Addictions]
The relationship of NLR and PLR with early prognosis in alcohol use disorder
Erdoğan Kaya Ayşea, Bülent Yazıcı Ahmeta, Kaya Muhammedb and Yazıcı Esraa
aDepartment of Psychiatry, Sakarya University School of Medicine, Sakarya, Turkey
bDepatment of Internal Medicine, Health Sciences University Derince Research and Training Hospital, Kocaeli, Turkey
ABSTRACT
Introduction: Alcohol and substance use disorder, which is one of the public health problems in Turkey as well as all over the world, includes the presence of many physiological, cognitive and behavioural symptoms that point to the chronic use of alcohol or substance by the individual despite the significant problems that occur with the substance (1).
Alcohol is known to be the most commonly abused substance in the world after caffeine and tobacco. The first sources associated with the discovery and use of alcohol effects by humans are from 3000 to 4000 B.C. When looking at the chemical structure, it is seen that alcohol consists of compounds containing aliphatic hydroxyl groups. Aliphatic groups that are medically important are methanol and ethylene glycol. In addition to their pleasant effects, acute toxic effects are also important in terms of medical. Ethyl alcohol taken orally is absorbed rapidly by passive diffusion from the gastrointestinal tract. Alcohol taken into the body is mainly metabolized from the liver and alcohol is biotransformated through the dehydrogenase and microsomal enzyme system (2).
The most important pharmacological effects of alcohol are leading depression and disinhibition of the central nervous system. Side effects from mild sedation to severe consciousness, motor coordination and balance problems can significantly affect patients ‘ lives. In addition, it has an inhibitory effect on the respiratory system, irritant effects on the gastrointestinal tract, negative effects on the metabolic and endocrine system, and teratogenic effects. In addition to these effects, alcohol withdrawal clinic is known to have great importance in terms of medicine such as alcohol addiction. Symptoms of alcohol withdrawal include a mild agitation, or a new spectrum, ranging from anxiety to life-threatening delirium tremens (3).
Besides the mentioned effects of alcohol, it has important effects on haematological and immune system. Alcohol also disrupts the function of humoral and cellular immunity and provides the basis for infection and inflammation in many tissues (4). Recently, the view that many chronic diseases are secondary to chronic inflammation is gaining more and more supporter. Alcohol and substance abuse can also be among these chronic diseases. However, a biomarker, which may be a clear indicator of alcohol-related inflammation, has not yet been identified. The complete blood count parameters used as nonspecific inflammatory markers are useful because they are inexpensive and easily accessible. Neutrophil lymphocyte ratio (NLR) and Platelet lymphocyte ratio (PLR) are an easily calculated index of systemic inflammation (5).
Relaps is one of the most important factors in the follow-up and treatment of alcohol use disorders. In several studies, cumulative relapse rates among people treated for alcohol dependence were found to be 58% 3 months after treatment. In a study conducted with alcohol use disorders in Turkey, the relapse rate was found to be 62% at the end of 12 months (6).
The aim of this study was to compare the NLR and PLR values of the patients diagnosed with alcohol use disorder with the healthy control group and to examine the suitability of withdrawal severity, NLR and PLR as early prognostic markers of chronic alcoholism treatment.
Our hypothesis is that alcohol dependence is associated with an inflammatory process, that NLR increases in alcohol dependence compared to healthy control group, as well as that NLR and withdrawal severity can be used to help predict early prognosis.
Method: The study was conducted with alcohol use disorder patients who were treated in Alcohol-Substance Use Disorders Treatment and Education Center (AMATEM) of Sakarya University School of Medicine Training and Research Hospital between the years of 2018–2019. The participants of the study were 18-65 years old, hospitalised patients (Patient group, n = 39), and healthy individuals (Control group, n = 39). Patients with chronic physical illness were not included in the study. Routine blood tests were conducted in both groups. In order to assess the severity of withdrawal in the patient group, the routinely conducted Clinical Institute Withdrawal Assessment for Alcohol Scale, revised (CIWA-Ar) scores were recorded. This scale was developed by Sullivan in 1989. It is a 10-item scale used to measure the severity of alcohol withdrawal syndrome. When possible, the patients’ use of substances during the 3 months after treatment was also examined. The patients were classified into two groups according to their use of alcohol during the 3 months after treatment as: Relapse (turning back to the previous drinking pattern) or Remission (not to consume any alcohol or not to continue to consume alcohol even if lapses are experienced). The effect of severity of withdrawal, NLR and PLR measured before treatment on relapse ratios in the 3-month follow-ups were examined. The data were analyzed by the Statistical Package for the Social Sciences (SPSS Inc; Chicago, IL, USA) 22.0 statistical program. Student T test was used to compare the mean ages of patients and control groups. Student T test was also used to compare the mean values of NLR and validity of withdrawal severity in relapse and remission groups. The Mann-Whitney U-test was used to compare the mean values of the other linear variables, since other linear variables did not show a standard distribution according to the Kolmogorov–Smirnov and Shapiro–Wilk normality tests.
Results: All 78 participants (composed of 39 patients and 39 healthy subjects) were males. The remission-relapse data of the 6 patients who did not attend for follow-up could not be obtained.
There was no significant difference between the age of healthy controls and the patients. (p > 0.05). Patients with alcohol use disorder had significantly higher NLR mean scores than the healthy controls. (p: 0.000) (Table 1). The mean age, NLR and PLR values in the patient group and control group are shown in Table 1.
The mean NLR values and severity of withdrawal in the relapse group were significantly higher compared to the remission group (p ≤ 0.05 for both), and the PLR values did not reveal any significant differences (p > 0.05) (Table 2). The mean NLR, PLR and 1st day withdrawal severity values in the remission and relapse group are shown in Table 2.
Discussion: In our study, patients with alcohol use disorder had significantly higher NLR mean scores than the healthy controls. This led the researchers to think that inflammatory mechanisms may be involved in the aetiopathogenesis of alcohol addiction. When the literature on this subject is examined, it is seen that there is a significantly higher NLR rate in the synthetic cannabinoid and opioid addicts compared to the healthy control group (7,8). However, we did not find a study on alcohol addicts on this subject in the literature survey, so we did not compare it with our study. Additionally, the NLR and severity of withdrawal in the relapse group were significantly higher compared to the remission group, and the PLR values did not reveal any significant differences. These results indicate that alcohol addiction is related to an inflammatory process. Furthermore, NLR and severity of withdrawal can be used to help in the prediction of early prognosis. Since severity of withdrawal mainly related to duration and amount of alcohol use (9), this results about NLR and withdrawal severity can give a point of view to alcohol addiction. Although many studies have shown that it is important to know the biological, psychological and social characteristics of patients in predicting the prognosis of alcohol use disorder patients, no predictive biomarker has been found yet (6). As far as we know, our study is the first clinical research on this subject. The fact that our study included a small number of patients and our study was a short-term follow-up study are main limitations of our study. There are many factors affecting relapse rate duration of alcohol abstinence period as a confounding factor (10). Our study couldn't include these factors. This is another limitation of study. Since our study included only male patients, it was not possible to compare between genders. In addition, we could not compare other markers of inflammation because they were not routinely examined. As a result, more research is needed to associate alcohol use disorder and withdrawal with inflammatory markers.
Table 1. Data of patients with alcohol use disorder and the healthy controls.
Table 2. Remission and relapse groups’ values of severity of withdrawal and NLR-PLR.
[Abstract:0298] [Autism]
Serum S100B, NT-3 and BDNF levels in children with autism spectrum disorder according to the initial type
Tunca Hüseyina and İşeri Elvanb
aDiyarbakir Children’s Hospital, Diyarbakir, Turkey
bDepartment of Child and Adolescent Psychiatry, Gazi University School of Medicine, Ankara, Turkey
ABSTRACT
Introduction: Autism spectrum disorder (ASD) is a complex neurodevelopmental disorders characterized with impairments in communication, reciprocal social interaction, presence of restricted and repetitive patterns of behavior. Although numerous studies showed that genetic, environmental, neurological and immunological factors are implicated, the etiopathogenesis of ASD remains poorly understood. Recent studies have focused on the contribution of neuroinflammation.
Neuroinflammation and neurotrophic factors including brain derived neurotrophic factor (BDNF) and neurotrophin 3 (NT3) are implicated in the pathophysiology of autism spectrum disorder (ASD). Elevated S100B protein levels accurately reflect the presence of glial cell pathology and continuing neurological damage in neuropathological conditions, including traumatic head injuries, psychiatric disorders, cerebrovascular insult and neurodegenerative diseases [1]. Although numerous studies indicate the contribution of neuroinflammatory changes to ASD, elevated S100B level in serum has been reported in only one study [2].
The aim of this study was to examine the interventions on the serum levels of S100B in relation to NT3 and BDNF in patients with congenital ASD in comparison with the patients with regressive ASD.
Methods: In this study, has been enrolled 52 children (45 boys and 7 girls) in the range of 29-72 months (mean ± SD = 43.25 ± 8.62 months) with diagnosed as ASD by the Diagnostic and Statistical Manual of Mental Disorders Fifth Edition (DSM-5) diagnostic criteria based on clinical examination. ASD patients were divided as two groups; symptoms of autism from birth to ASD group called as 'Congenital ASD (n = 37)' group, symptoms of autism beginners after 18 months to ASD group called as 'Regressive ASD 'group. Also, it has been enrolled 29 healthy children (22 boys and 7 girls) in the range of 25-65 months (mean ± SD = 46.17 ± 12.68) as control group. From all included participants collected blood samples. The blood samples were centrifuged, and then the separated serum was stored at −80 °C until analyzed for S100B, BDNF and NT3 levels.
All families who agreed to participate in the study provided written consent was obtained. Ethical approval for the study was taken from Gazi University Faculty of Medicine Research Ethics Committee.
Statistical Analysis: Research data is installed and evaluated via "SPSS (Statistical Package for Social Sciences) for Windows 22.0 (SPSS Inc, Chicago, IL)". Statistical significance level was adopted as p < 0.05.
Results: It has been no significantly statistical difference in terms of age and gender at congenital ASD, regressive ASD and control groups (p > 0.05).
It has been determined statistically significant difference in terms of blood S100B values of the study groups (p < 0.05). Post-hoc pairwise comparisons revealed significant difference between the congenital ASD group and the control group. Serum S100B level of congenital OSB group was significantly higher than control group. On the other hand study groups have no statistically significant difference in terms of serum BDNF and NT3 levels (p > 0.05).
Discussion: In the present study, S100B level was found to be higher in patients with congenital ASD than regressive ASD and control groups.
Association of serum levels of S100B with autoimmunity were examined in children with ASD in a previous study. Although there was no association, elevated level of S100B has been reported first time in ASD [2]. In the present study shows that serum S100B level is increased in patients with ASD at the age between 29-72 months.
Neurotrophic factors including NT3, NT4 and BDNF play a critical role in many processes in CNS including neurogenesis, synaptic plasticity, long-term potentiation and all cognitive functions. It is known that NT3 plays a key role in the maturation of glutamatergic synapse development. In previous studies, NT3 has been shown to be involved in the development and survival of the climbing fiber system of the inferior olive and the cerebellar Purkinje cell. Therefore, a deficiency in NT3 level would be expected to cause a deficit in activity dependent synapse and neuron elimination in ASD, leading to impairment in development of brain. In consistent with this view, several studies show that serum NT3 levels are reduced in children with ASD [3]. Several studies show that serum NT3 levels are reduced in children with ASD.
There are studies showing that BDNF levels are high in autism as well as studies showing that it is low. Although BDNF level increases with age in serum, BDNF in young children with ASD has been reported to be higher in than adult controls. Conversely, decreased level of BDNF also has been shown in another studies. In the present study, BDNF level in serum was not found to be higher in comparison with ASD and controls.
Table 1. Distribution of S100B, BDNF and NT-3 Values Between the Congenital and Regressive ASD Group and Control Group
[Abstract:0422] [Autism]
Effects of riluzole and gabapentin on spatial learning, locomotor activity of anxiety and social behaviors in autism-like rat model
Demirkaya Sevcan Karakoça, Orak Cenkb, Şirinyıldız Ferhatb, Yeşilçayır Gül Taşlıb, Cesur Gökhanb and Ek Onurb
aDepartment of Child and Adolescent Psychiatry, School of Medicine, Adnan Menderes University, Aydin, Turkey
bDepartment of Physiology, Adnan Menderes University School of Medicine, Aydin, Turkey
ABSTRACT
Introduction: Autism spectrum disorder (ASD), is a neurodevelopmental disorder, characterized by difficulties in social interaction and communication and as well as repetitive and ritualistic behaviors.
Despite the burden of the ASD on individual, family and community is high, ASD is still a disorder with a poorly understood pathophysiology and a lack of symptom specific drug discovery. Various neurotransmitter mechanisms have been studied in ASD. Recent studies have proposed that disruptions in the glutamate and GABA functions are important in the neurobiological etiology of ASD.
Due to ethical problems on developing human brain, the study on neurobiology of the childhood neuropsychiatric disorders is firstly conducted by animal experiments. The goals of animal models are validating hypotheses about the mechanisms underlying the disease and evaluating the translational benefit of the therapeutics for the ASD.
Clinically, valproic acid (VPA) is a medication used for epilepsy and mood swings. However, the use of VPA during childbearing years, and particularly during early pregnancy, is of concern. For years, it has been associated with various teratogenic effects and, more recently, increased risk of autism. Reported clinical trials have caused a ripple of pre-clinical studies using VPA to induce autism-like behavior in rats and mice [1].
In this study, we aimed to examine effects of the riluzole, an antiglutamate agent, and gabapentin which increases GABAergic transmission, on learning, anxiety and social behaviors in prenatal VPA induced autism-like rat model.
Methods: Ethical approval was taken from the Adnan Menderes University Faculty of Medicine Ethical Board of Experiments on Animals.
With the light of given literature, we used VPA for autism model [1]. On the 12.5th gestational day, valproic acid was applied parenterally to the female Wistar Albino rats, except for the autism-negative control group, to create autism-like model (ALM).
Newborn male rat pups (n = 40) divided into 5 equal groups; negative control (no valproate exposure), autism; ALM-nontreated (sham control), ALM plus riluzole treated, ALM plus gabapentin treated, and ALM plus combination of gabapentin and riluzole treated (n = 8).
Riluzole (10 mg/kg/day per oral (p.o.)) and gabapentin (300 mg/kg/day p.o.) were administered via orogastric gavage in the 3rd postnatal week (juvenile rats) for 2 weeks. Behavioral apparatus designed for mouse behavioral assays were applied in the 6th postnatal week [2]. These assays were open field maze (OFM), three-chambered sociability test (TCST) and Morris-water Maze Test (MWM).
Open Field Maze; consists of a wall-enclosed area that is of sufficient height to prevent the subject from escaping. The time spent outside the central area was measured as a sign of anxiety. Locomotor activity is also observed as an indicator of anxiety.
Three-Chambered Sociability Test: The three chamber test is a commonly used method to measure social approach behaviour in mice. After adaptation to the three-chamber arena, a mouse is released into the middle chamber and allowed to explore the other compartments.
The sociability index is the ratio of the time spent with the foreign animal to the time spent in the empty room whereas the social preference index is the ratio of the time spent with the novel rat to the time spent with the familiar rat. Morris-Water Maze Test: a classic test for examining spatial learning and memory. It is a round white pool 94 cm in diameter and 31 cm deep which was filled to a depth of 30 cm with water with non-toxic dye. There is an escape platform in the center of the one quadrant of the pool. The platform was hidden after the rats had learned the location of the escape platform for 4 days. On the 5th day, the time that the rats spend in the quadrant had platform was calculated.
Results: Both sociability and social preference indices with strangers in TCST were lower in the ALM rats than the negative groups (p < 0.01) indicating that the model was well fitted. Sociability index was the highest in negative control group which was an indicator that the experimental model fitted. Grooming as a sign of compulsive and ritualistic behaviors, was the highest in the autism group without any treatment. Learning was the worst in the autism group with gabapentin. Among the drug groups, combined treated rats showed the highest sociability index and social preference index (p < 0.01). In the OFT, riluzole treated group had spent more rearing behaviors and spent less time in the outer squares (periphery) (p < 0.05). Gabapentin treated rats showed the least rearing and grooming behaviors in the OFT. In the MWM test, the percent of the time spent in the previously learned platform was the highest in the riluzole only group (p < 0.05) and this learning was the worst in the gabapentin treated rats (p > 0.05) (Table 1).
Discussion: Here we used VPA to create an autism model. Depending on outcome data of behavioral tests, we could suggest that prenatal VPA exposure on a specific day can be used for experimental models of autism.
Our results suggest that riluzole, an antiglutamatergic agent, seems to have some possible positive effects on social interaction, locomotor behaviors for anxiety and spatial learning in an autism-like rat model. However, riluzole was shown as ineffective in irritability in clinical cases [3], some more research on social effects of riluzole would promise better outcomes depending on animal results.
In our experiment, if gabapentin is used alone, helped to play a mild positive role on social behavior whereas a negative role in spatial learning. However gabapentin may attenuate the social behaviors in combined treatment.
Gabapentin may also decrease exploratory motions as well as anxiety levels. If we consider grooming as stereotypes, gabapentin decreases stereotypical movements.
Further molecular and biochemical studies are needed to reveal the underlying etiological and therapeutic mechanisms of these neurotransmitter modulators mainly for glutamate. Also instead of VPA induced models, transgenic or knockout models for autism would supply more accurate data on therapeutic challenges for autism. Due to lack of investigations on medical interventions for ASD, our results have provided new data on possible pharmacological treatments of core symptoms of autism.
Table1. Behavioral results of experimental groups.
References
- Бохан HA. Нейробиологические проблемы изучения аддиктивных расстройств. Сибирский вестник психиатрии и наркологии 2008; 1:59-63.
- Abdullaeva VK. Clinical-psychological and pathochemical mechanisms of the opioid addiction of persons with comorbid pathology. ISJ Theoretical & Applied Science 2016; 01(33): 58-63.
- Khalsa JH. Medical Consequences of Drug Abuse and Cooccurring Infections: Research at the National Institute on Drug Abuse. Subst. Abus 2008; 29 (3):5-16.
- Brent D, Mann JJ. Family genetic studies, suicide, and suicidal behavior. Am J Med Genet Part C Semin Med Genet. 2005 Feb 15;133C(1):13–24.
- Stieg MR, Sievers C, Farr O, Stalla GK, Mantzoros CS. Leptin: A hormone linking activation of neuroendocrine axes with neuropathology. Psychoneuroendocrinology. 2015;51:47–57.
- Milaneschi Y, Simmons WK, van Rossum EFC, Penninx BW. Depression and obesity: evidence of shared biological mechanisms. Mol Psychiatry. 2018 Feb 16
- Hryhorczuk C, Sharma S, Fulton SE. Metabolic disturbances connecting obesity and depression. Front Neurosci. 2013;7(7 OCT):1–14.
- Sambrook J, Fritsch E, Maniatis T. Molecular Cloning: A Laboratory Manual (Fourth Edition). 2nd ed. New York, USA: Cold-Spring Harbor; 1989. 9.16-9.19.
- Gotoda T, Manning BS, Goldstone AP, Imrie H, Evans AL, Strosberg AD, et al. Leptin receptor gene variation and obesity: lack of association in a white British male population. Hum Mol Genet. 1997 Jun;6(6):869–76.
- Jakopec M. Association between LEPR gene 1019 polymorphism and the morphological characteristics in Roma population of Croatia. Master Thesis. 2015.
- Suriyaprom K, Tungtrongchitr R, Thawnasom K. Measurement of the levels of leptin, BDNF associated with polymorphisms LEP G2548A, LEPR Gln223Arg and BDNF Val66Met in Thai with metabolic syndrome. Diabetol Metab Syndr. 2014;6(1):6.
- Atmaca M, Kuloglu M, Tezcan E, Ustundag B, Gecici O, Firidin B. Serum leptin and cholesterol values in suicide attempters. Neuropsychobiology. 2002;45(3):124–7.
- Tutuncu R, Gunay H, Balibey H, Abaslı D. Decreased Leptin Levels in Antisocial Personality Disorder Patients. Klin Psikofarmakol Bülteni-Bulletin Clin Psychopharmacol. 2013 Mar 8;23(1):72–6.
- Fattore L, Fratta W. Beyond THC: The New Generation of Cannabinoid Designer Drugs. Front Behav Neuroscience. 2011;5(September):1–12.
- Cohen K, Kapitány-Fövény M, Mama Y, Arieli M, Rosca P, Demetrovics ZWA. The effects of synthetic cannabinoids on executive function. 2017; 1121-1134.
- Yilmaz H, Bozkurt M, Evren C, Umut G, Keskinkilic C. Evaluation of cognitive functions in individuals with synthetic cannabinoid use disorder and comparison to individuals with cannabis use disorder. Psychiatry Res. 2018;262(June 2017):46–54.
- Ornstein TJ, Iddon JL, Baldacchino AM, Sahakian BJ, London M, Everitt BJ, et al. Profiles of cognitive dysfunction in chronic amphetamine and heroin abusers. Neuropsychopharmacology. 2000;23(2):113–126.
- Pau CWH, Lee TMC, Chan SFF. The impact of heroin on frontal executive functions. Arch Clin Neuropsychol. 2002;17(7):663–670.
- Karakaş S, Erdoğan E, Sak L, Soysal AŞ. Stroop Testi TBAG Formu: Türk Kültürüne Standardizasyon Çalışmaları. Klin Psikiyatr. 1999;75–88.
- Karakaş S. (WCST) ve Stroop Testi TBAG formu puanlarının test içi ve testler-arası ilişkileri. X Ulus Psikol Kongresi özet kitabı. 1998;44.
- Won E, Kim Y-K. Stress the autonomic nervous system, and the immune-kynurenine pathway in the etiology of depression. Current neuropharmacology. 2016;14(7):665-73.
- Hochstrasser T, Ullrich T, Sperner-Unterweger B, Humpel C. Inflammatory stimuli reduce survival of serotonergic neurons and induce neuronal expression of indoleamine 2,3-dioxygenase in rat dorsal raphe nucleus organotypic brain slices. Neuroscience. 2011;184: 128-38.
- Chen Y, Guillemin GJ. Kynurenine pathway metabolites in humans: disease and healthy states. International Journal of Tryptophan Research. 2009; 2: IJTR. S2097.
- Hallmayer J, Cleveland S, Torres A, Phillips J, Cohen B, Torigoe T, et al. Genetic heritability and shared environmental factors among twin pairs with autism. Archives of general psychiatry. 2011;68(11):1095-102.
- Caglayan AO. Genetic causes of syndromic and non-syndromic autism. Developmental Medicine & Child Neurology. 2010;52(2):130-8.
- Geschwind DH. Genetics of autism spectrum disorders. Trends in cognitive sciences. 2011;15(9):409-16.
- Huguet G, Benabou M, Bourgeron T. The Genetics of Autism Spectrum Disorders. In: Sassone-Corsi P, Christen Y, editors. A Time for Metabolism and Hormones. Cham: Springer International Publishing; 2016. p. 101-29.
- Anney R, Klei L, Pinto D, Regan R, Conroy J, Magalhaes TR, et al. A genome-wide scan for common alleles affecting risk for autism. Human molecular genetics. 2010;19(20):4072-82.
- Chen D, Vollmar M, Rossi MN, Phillips C, Kraehenbuehl R, Slade D, et al. Identification of macrodomain proteins as novel O-acetyl-ADP-ribose deacetylases. The Journal of biological chemistry. 2011;286(15):13261-71.
- Han W, Li X, Fu X. The macro domain protein family: structure, functions, and their potential therapeutic implications. Mutation research. 2011;727(3):86-103.
- Tsang KM, Croen LA, Torres AR, Kharrazi M, Delorenze GN, Windham GC, et al. A genome-wide survey of transgenerational genetic effects in autism. PloS one. 2013;8(10):e76978.
- Curran S, Bolton P, Rozsnyai K, Chiocchetti A, Klauck SM, Duketis E, et al. No association between a common single nucleotide polymorphism, rs4141463, in the MACROD2 gene and autism spectrum disorder. American journal of medical genetics Part B, Neuropsychiatric genetics: the official publication of the International Society of Psychiatric Genetics. 2011;156b(6):633-9.
- Anney R, Klei L, Pinto D, Almeida J, Bacchelli E, Baird G, et al. Individual common variants exert weak effects on the risk for autism spectrum disorders. Human molecular genetics. 2012;21(21):4781-92.
- Prandini P, Pasquali A, Malerba G, Marostica A, Zusi C, Xumerle L, et al. The association of rs4307059 and rs35678 markers with autism spectrum disorders is replicated in Italian families. Psychiatric genetics. 2012;22(4):177-81.
- Jones RM, Cadby G, Blangero J, Abraham LJ, Whitehouse AJO, Moses EK. MACROD2 gene associated with autistic-like traits in a general population sample. Psychiatric genetics. 2014;24(6):241-8.
- Kuo PH, Chuang LC, Su MH, Chen CH, Chen CH, Wu JY, et al. Genome-Wide Association Study for Autism Spectrum Disorder in Taiwanese Han Population. PloS one. 2015;10(9):e0138695.
- Namjou B, Marsolo K, Caroll RJ, Denny JC, Ritchie MD, Verma SS, et al. Phenome-wide association study (PheWAS) in EMR-linked pediatric cohorts, genetically links PLCL1 to speech language development and IL5-IL13 to Eosinophilic Esophagitis. Frontiers in genetics. 2014;5:401.
- Torrico B, Chiocchetti AG, Bacchelli E, Trabetti E, Hervas A, Franke B, et al. Lack of replication of previous autism spectrum disorder GWAS hits in European populations. Autism research: official journal of the International Society for Autism Research. 2017;10(2):202-11.
- Consortium AG. Meta-analysis of GWAS of over 16,000 individuals with autism spectrum disorder highlights a novel locus at 10q24.32 and a significant overlap with schizophrenia. Molecular autism. 2017;8:21.
- Piven J, Elison JT, Zylka MJ. Toward a conceptual framework for early brain and behavior development in autism. Molecular Psychiatry. 2017;23:165.
- Schopler E, Reichler RJ, DeVellis RF, Daly K. Toward objective classification of childhood autism: Childhood Autism Rating Scale (CARS). Journal of autism and developmental disorders. 1980;10(1):91-103.
- İncekaş S, Baykara B, Avcil S, Demiral Y. Validity and Reliability Analysis of Turkish Version of Childhood Autism Rating Scale. Turkish Journal of Psychiatry. 2016;27(4).
- Sucuoğlu B. The psychometric characteristics of the Turkish form of the aberrant behavior checklist. Turk Psikol Derg. 2003;18:77-9.
- Schmittgen TD, Livak KJ. Analyzing real-time PCR data by the comparative CT method. Nature Protocols. 2008;3:1101.
- Kang HJ, Kawasawa YI, Cheng F, Zhu Y, Xu X, Li M, et al. Spatio-temporal transcriptome of the human brain. Nature. 2011;478(7370):483-9.
- Ansel A, Rosenzweig JP, Zisman PD, Melamed M, Gesundheit B. Variation in Gene Expression in Autism Spectrum Disorders: An Extensive Review of Transcriptomic Studies. Frontiers in Neuroscience. 2016;10:601.
- Kessler, RC, et al., Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Archives of General Psychiatry, 2005. 62(6): p. 593-602.
- Kessler, RC. The costs of depression. Psychiatric Clinics, 2012. 35(1): p. 1-14.
- Türkçapar, H. Bilişsel terapi: Temel ilkeler ve uygulama. 2009: HYB Yayıncılık, 2002 (Medico Graphics Ofset).
- Hoyt, B. D. (2005). Sleep in patients with neurologic and psychiatric disorders. Primary care, 32(2), 535-48.
- Wilson, S., & Argyropoulos, S. (2012). Sleep in schizophrenia: time for closer attention. The British Journal of Psychiatry, 200(4), 273-274.
- YETKİN, S., & AYDIN, H. (2014). Psikotropik İlaçların Uyku Üzerine Etkileri. Turkiye Klinikleri Journal of Psychiatry Special Topics, 7(1), 36-42.
- Miller, D. D. (2004). Atypical antipsychotics: sleep, sedation, and efficacy. Primary care companion to the Journal of clinical psychiatry, 6(suppl 2), 3.
- Yamashita H, Morinobu S, and Yamawaki S. et al. Effect of risperidone on sleep in schizophrenia: a comparison with haloperidol. Psychiatry Res. 2002 109:137–142. [PubMed]
- Collaborative Working Group on Clinical Trial Evaluations. Measuring outcome in schizophrenia: differences among the atypical antipsychotics. J Clin Psychiatry. 1998 59suppl 12. 3–9.
- Idzikowski C, Mills FJ, Glennard R. 5-Hydroxytryptamine-2 antagonist increases human slow wave sleep. Brain Res. 1986;378:164–168
- Kasper S, Lerman MN, McQuade RD, et al. Efficacy and safety of aripiprazole vs. haloperidol for long-term maintenance treatment followingacute relapse of schizophrenia. Int J Neuropsychopharmacol 2003; 6 (4): 325-37.
- Monti, J. M., Torterolo, P., & Perumal, S. R. P. (2017). The effects of second generation antipsychotic drugs on sleep variables in healthy subjects and patients with schizophrenia. Sleep medicine reviews, 33, 51-57.
- Xiang Y, Weng Y, Li W et al. Training patients with schizophrenia with the community re-entry module: a controlled study. Soc Psychiatry Psychiatr Epidemiol 2006; 41:464-469.
- Foruzandeh, N., & Parvin, N. (2013). Occupational therapy for inpatients with chronic schizophrenia: a pilot randomized controlled trial. Japan Journal of Nursing Science, 10(1), 136-141.
- Perilli, V., Stasolla, F., Maselli, S., & Morelli, I. (2018). Occupational Therapy and Social Skills Training for Enhancing Constructive Engagement of Patients with Schizophrenia: A Review.
- Karatay G, Kubilay G. Sosyoekonomik düzeyi farklı iki lisede madde kullanma durumu ve etkileyen faktörlerin belirlenmesi. Hemşirelikte Araştırma Geliştirme Dergisi, 1(2), 57-70, 2004.
- Karakaş SA, Ersöğütçü F. Madde Bağımlılığı ve Hemşirelik. Sağlık Bilimleri ve Meslekleri Dergisi, 3(2), 133-139, 2016.
- European Monitoring Centre for Drugs and Drug Addiction. (2018). European Drug Report: Trends and Developments, 2018.
- Tamar-Gurol D, Sar V, Karadag F, Evren C, Karagoz M. Childhood emotional abuse, dissociation, and suicidality among patients with drug dependency in Turkey. Psychiatry and Clinical Neurosciences, 62(5), 540-547, 2008.
- Bilici R, Beker ŞD, Süner Ö, Çıtak S, Izci F. Sociodemographic characteristics of Turkish patients who violated a supervised probation program. Journal of ethnicity in substance abuse, 17(3), 335-344, 2018.
- Şıpka H, Sönmez B, Karaca E, Vardar E. Bir üniversite hastanesi bağımlılık merkezinde yatarak tedavi gören hastaların profili: Bir yıllık AMATEM verilerinin incelenmesi. 50. Ulusal Psikiyatri Kongresi. Turk Psikiyatri Derg, 25, 32; 2014.
- Bulut M, Savaş HA, Cansel N, Selek S, Kap Ö, Yumru M, Vırıt O. Gaziantep Üniversitesi Alkol Ve Madde Kullanim Bozukluklari Birimine Başvuran Hastalarin Sosyodemografik Özellikleri. Journal of Dependence, 7, 65-70; 2006.
- Çakmak D, Kralı A, Akvandaz Y. Son beş yıl içinde AMATEM’e yatan bağımlıların özellikleri. 1996.
- Alpay N, Maner F, Kalyoncu A. AMATEM’de 1990 yılında yatırılan madde bağımlılarının demografik özellikleri ve geçmiş yıllarla kıyaslanması. 27. Ulusal Psikiyatri Kongresi Program ve Bildiri Özetleri Kitabı, 177. 1991
- Türkiye Uyuşturucu ve Uyuşturucu Bağımlılığı İzleme Merkezi. Türkiye Uyuşturucu Raporu. Ankara: Yazar. 2018.
- Galea S, Vlahov D. Social determinants and the health of drug users: socioeconomic status, homelessness, and incarceration. Public health reports, 117(Suppl 1), S135. 2002.
- Sherba RT, Coxe KA, Gersper BE, Linley JV. Employment services and substance abuse treatment. Journal of substance abuse treatment, 87, 70-78; 2018.
- Arria AM, Topps-II Interstate Cooperative Study Group. Drug treatment completion and post-discharge employment in the TOPPS-II interstate cooperative study. Journal of Substance Abuse Treatment, 25(1), 9–18. 2003.
- Vaillant GE. What can long-term follow-up teach us about relapse and prevention of relapse in addiction? British Journal of Addiction, 83(10), 1147–1157. 1988.
- Ritter A, Cameron J. A review of the efficacy and effectiveness of harm reduction strategies for alcohol, tobacco and illicit drugs. Drug and Alcohol Review, 25(6), 611–624. 2006.
- Harrison PA, Asche SE. Outcomes monitoring in Minnesota: treatment implications, practical limitations. Journal of Substance Abuse Treatment, 21(4), 173-183. 2001.
- Manuel JI, Yuan Y, Herman DB, Svikis DS, Nichols O, Palmer E, Deren S. Barriers and facilitators to successful transition from long-term residential substance abuse treatment. Journal of Substance Abuse Treatment, 74, 16–22. 2017
- Ahern J, Stuber J, Galea S. (2007). Stigma, discrimination and the health of illicit drug users. Drug and Alcohol Dependence, 88(2-3), 188–196. 2007.
- Ertüzün E, Uyaroğlu AK, Demirel B, Koçak E. Boş Zaman Aktivitelerinin Madde Bağımlılığı Sürecindeki Rolüne İlişkin Nitel Bir Çalışma. Spor Bilimleri Dergisi, 27(2), 49-58. 2016.
- Gundogmus, İ., Algul, A., Karagöz, A. and Kıyançiçek, M. PDW and RDW are new parameters for bipolar episodes and unipolar depression. Psychiatry and Clinical Psychopharmacology 2018;4: 1-7.
- Erzin, G., Kotan, V.O., Topçuoğlu, C., Özkaya, G., Erel, Ö., Yüksel, R.N., Ürer, E., Aydemir, M.Ç. and Göka, E. Thiol/disulphide homeostasis in bipolar disorder. Psychiatry research 2018;261: 237-242.
- Usta, M.B., Karabekiroglu, K., Sahin, B., Aydin, M., Bozkurt, A., Karaosman, T., Aral, A., Cobanoglu, C., Kurt, A.D., Kesim, N. and Sahin, İ., 2018. Use of machine learning methods in prediction of short-term outcome in autism spectrum disorders. Psychiatry and Clinical Psychopharmacology 2018;16:1-6.
- Soygür H. Psikofarmakolojinin Tarihsel Gelişimi. Yüksel N, editor. Temel Psikofarmakoloji. Ankara: Türkiye Psikiyatri Derneği Yayınları; 2010. s: 1–15.
- Glennon J, Purper-Ouakil D, Bakker M, et al. Paediatric European Risperidone Studies (PERS): context, rationale, objectives, strategy, and challenges. Eur Child Adolesc Psychiatry. 2014;23(12):1149–1160. Published online 2013 Dec 15.
- Arabgol F, Panaghi L, Nikzad V. Risperidone versus Methylphenidate in Treatment of Preschool Children With Attention-Deficit Hyperactivity Disorder. Iran J Pediatr. 2015 Feb;25(1):e265. Published online 2015 Feb 21.
- Garfield LD, Brown DS, Allaire BT, Ross RE, Nicol GE, Raghavan R. Psychotropic Drug Use Among Preschool Children in the Medicaid Program From 36 States. Am J Public Health. 2015 March;105(3):524–529. Published online 2015 March. doi: 10.2105/AJPH.2014.302258
- Johnston AN, Bu W, Hein S, Garcia S, Camacho L, Xue L, et al. Hyperprolactinemia-inducing antipsychotics increase breast cancer risk by activating JAK-STAT5 in precancerous lesions. Breast Cancer Res. 2018;20:42. Published online 2018 May 19.
- Corkum P, Tannock R, Moldofsky H. Sleep disturbances in children with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 1998;37:637–646.
- Miano S, Parisi P, Villa MP. The sleep phenotypes of attention deficit hyperactivity disorder: The role of arousal during sleep and implications for treatment. Medical Hypotheses 2012;79:147–153.
- Weiss MD, Salpekar J. Sleep problems in the child with attention-deficit hyperactivity disorder. CNS drugs. 2010;24(10):811–828.
- Corbetta M, Patel G, Shulman GL. The reorienting system of the human brain: from environment to theory of mind. Neuron 2008;58(3):306–324.
- Eklund A, Nichols TE, Knutsson H. Cluster failure: why fMRI inferences for spatial extent have inflated false-positive rates. Proc Natl Acad Sci U S A 2016;113(28):7900–7905.
- Kim BN, Lee JS, Shin MS, Cho SC, Lee DS. Regional cerebral perfusion abnormalities in attention deficit/hyperactivity disorder. Eur Arch Psychiatry Clin Neurosci 2002;252(5):219–225.
- Lee JS, Kim BN, Kang E, Lee DS, Kim YK, Chung JK, Lee MC, Cho SC. Regional cerebral blood flow in children with attention deficit hyperactivity disorder: comparison before and after methylphenidate treatment. Human Brain Mapp. 2005;24(3):157–164.
- O’Gorman RL, Mehta MA, Asherson P, Zelaya FO, Brookes KJ, Toone BK, Alsop DC, Williams SC. Increased cerebral perfusion in adult attention deficit hyperactivity disorder is normalised by stimulant treatment: a non-invasive MRI pilot study. Neuroimage 2008;42(1):36–41.
- Uzbay TI. Pharmacological importance of agmatine in brain. Neurosci Biobehav Rev. 2012; 36:502–519.
- Uzbay T. A new target for diagnosis and treatment of CNS disorders: Agmatinergic system. Curr Med Chem. 2012b;19:5116–5121.
- Reis DJ, Regunathan S. Agmatine: an endogenous ligand at imidazoline receptors may be a novel neurotransmitter in brain. J Auton Nerv Syst. 1998;72:80–85.
- Madai VI, Poller WC, Peters D, et al. Synaptic localisation of agmatinase in rat cerebral cortex revealed by virtual pre-embedding. Amino Acids. 2012;43:1399–1403.
- Halaris A, Plietz J. Agmatine. CNS drugs. 2007;21:885–900.
- Auguet M, Viossat I, Marin JG, Chabrier PE. Selective inhibition of inducible nitric oxide synthase by agmatine. Jpn J Pharmacol. 1995;69:285–287.
- Feng Y, LeBlanc MH, Regunathan S. Agmatine reduces extracellular glutamate during pentylenetetrazole-induced seizures in rat brain: a potential mechanism for the anticonvulsive effects. Neurosci Lett. 2005;390:129–133.
- Galea E, Regunathan S, Eliopoulos V, Feinstein DL. Inhibition of mammalian nitric oxide synthases by agmatine, an endogenous polyamine formed by decarboxylation of arginine. Biochem J. 1996;316:247–249.
- Wang WP, Iyo AH, Miguel-Hidalgo J, Regunathan S, Zhu MY. Agmatine protects against cell damage induced by NMDA and glutamate in cultured hippocampal neurons. Brain Res. 2006;1084:210–216.
- Wang XF, Wu N, Su RB, Lu XQ, Liu Y, Li J. Agmatine modulates neuroadaptations of glutamate transmission in the nucleus accumbens of repeated morphine-treated rats. Eur J Pharmacol. 2011;650:200–205.
- Javitt DC, Zukin SR. Recent advances in the phencyclidine model of schizophrenia. Am J Psychiatry. 1991;148:1301–1308.
- Treen D, Batlle S, Mollà L, et al. Are there glutamate abnormalities in subjects at high risk mental state for psychosis? A review of the evidence. Schizophren Res. 2016;171:166–175.
- Weinberger DR, McClure RK. Neurotoxicity, neuroplasticity, and magnetic resonance imaging morphometry: what is happening in the schizophrenic brain? Arch Gen Psychiatry. 2002;59:553–558.
- Yao JK, Leonard S, Reddy RD. Increased nitric oxide radicals in postmortem brain from patients with schizophrenia. Schizophren Bull. 2004;30:923–934.
- Yao JK, Reddy R. Oxidative stress in schizophrenia: pathogenetic and therapeutic implications. Antioxid Redox Signal. 2001;15:1999–2002.
- Shim S, Shuman M, Duncan E. An emerging role of cGMP in the treatment of schizophrenia: a review. Schizophren Res. 2016;170:226–231.
- Garthwaite J. Glutamate, nitric oxide and cell-cell signalling in the nervous system. Trends Neurosci. 1991;14:60–67.
- Uzbay IT, Oglesby MW. Nitric oxide and substance dependence. Neurosci Biobehav Rev. 2001;25:43–52.
- Hallak JE, Maia-de-Oliveira JP, Abrao J, et al. Rapid improvement of acute schizophrenia symptoms after intravenous sodium nitroprusside: a randomized, double-blind, placebo-controlled trial. JAMA Psychiatry. 2013;70:668–676.
- Liu P, Jing Y, Collie ND, Dean B, Bilkey DK, Zhang H. Altered brain arginine metabolism in schizophrenia. Transl Psychiatry. 2016;6:e871.
- Uzbay T, Kayir H, Goktalay G, Yildirim M. Agmatine disrupts prepulse inhibition of acoustic startle reflex in rats. J Psychopharmacol. 2010;24:923–929.
- Kotagale NR, Taksande BG, Wadhwani PJ, et al. Psychopharmacological study of agmatine in behavioral tests of schizophrenia in rodents. Pharmacol Biochem Behav. 2012;100:398–403.
- Pålsson E, Fejgin K, Wass C, Klamer D. Agmatine attenuates the disruptive effects of phencyclidine on prepulse inhibition. Europ J Pharmacol. 2008;590:212–216.
- Uzbay T, Goktalay G, Kayir H, et al. Increased plasma agmatine levels in patients with schizophrenia. J Psychiatric Res. 2013;47:1054–1060.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington (DC): American Psychiatric Association; 2013.
- Yang KC, Reis DJ. Agmatine selectively blocks the N-methyl-D-aspartate subclass of glutamate receptor channels in rat hippocampal neurons. J Pharmacol Exp Ther. 2004;288:544–549.
- Tsai G, Coyle JT. Glutamatergic mechanisms in schizophrenia. Annu Rev Pharmacol Toxicol. 2002;42:165–791.
- Lindsley CW, Shipe WD, Wolkenberg SE, et al. Progress towards validating the NMDA receptor hypofunction hypothesis of schizophrenia. Curr Top Med Chem. 2006;6:771–785.
- Harrison PJ. Metabotropic glutamate receptor agonists for schizophrenia. Br J Psychiatry. 2008;192:86–87.
- Knox LT, Jing Y, Collie ND, Zhang H, Liu P. Effects of acute phencyclidine administration on arginine metabolism in the hippocampus and prefrontal cortex in rats. Neuropharmacol. 2014;81:195–205.
- Djordjević VV, Stojanović I, Stanković-Ferlež D, et al. Plasma nitrite/nitrate concentrations in patients with schizophrenia. Clin Chem Lab Med. 2010;48:89–94.
- Yilmaz N, Herken H, Cicek HK, Celik A, Yürekli M, Akyol Ö. Increased levels of nitric oxide, cortisol and adrenomedullin in patients with chronic schizophrenia. Med Princip Practic. 2007;16:137–141.
- Baba H, Suzuki T, Arai H, Emson PC. Expression of nNOS and soluble guanylate cyclase in schizophrenic brain. Neuroreport 2004;15:677–680.
- Lauer M, Johannes S, Fritzen S, Senitz D, Riederer P, Reif A. Morphological abnormalities in nitric-oxide-synthase-positive striatal interneurons of schizophrenic patients. Neuropsychobiol. 2005;52:111–117.
- Gupta N, Jing Y, Collie ND, Zhang H, Liu P. Ageing alters behavioural function and brain arginine metabolism in male Sprague–Dawley rats. Neuroscience. 2012;226:178–196.
- Rushaidhi M, Jing Y, Kennard JT, et al. Aging affects l-arginine and its metabolites in memory-associated brain structures at the tissue and synaptoneurosome levels. Neurosci. 2012;209:21–31.
- Liu P, Zhang H, Devaraj R, Ganesalingam GS, Smith PF. A multivariate analysis of the effects of aging on glutamate, GABA and arginine metabolites in the rat vestibular nucleus. Hearing Res. 2010;269:122–133.
- Liu P, Chary S, Devaraj R, et al. Effects of aging on agmatine levels in memory-associated brain structures. Hippocampus. 2008;18:853–856.
- Esnafoglu E, Irende I. Decreased plasma agmatine levels in autistic subjects. J Neural Transmiss. 2018;125:735–740.
- Chen GG, Almeida D, Fiori L, Turecki G. Evidence of reduced agmatine concentrations in the cerebral cortex of suicides. Int J Neuropsychopharmacol. 2018; doi: 10.1093/ijnp/pyy058
- Maia-de-Oliveira JP, Lobão-Soares B, Ramalho T, et al. Nitroprusside single-dose prevents the psychosis-like behavior induced by ketamine in rats for up to one week. Schizophr Res. 2015;162:211–215.
- Deutsch SI, Rosse RB, Schwartz BL, Fay-McCarthy M, Rosenberg PB, Fearing K. Methylene blue adjuvant therapy of schizophrenia. Clin Neuropharmacol. 1997;20:357–363.
- Goodwin RD, et al., Epidemiology of Mood Disorders. 2006.
- Simon GE, et al., An international study of the relation between somatic symptoms and depression. N Engl J Med. 1999;341(18):1329–1335.
- Terre L, et al., Do somatic complaints predict subsequent symptoms of depression? Psychother Psychosom. 2003;72(5):261–267.
- Pennebaker JW. Emotion, disclosure, and health: An overview. 1995.
- Hirokawa K, Yagi A, Miyata Y. An examination of the effects of stress management training for Japanese college students of social work. Int J Stress Manag. 2002;9(2):113–123.
- American Psychiatric Association. Attention-deficit/hyperactivity disorder. In: Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington (VA): American Psychiatric Association; 2013. p. 59.
- DuPaul GJ, Stoner G. ADHD in the Schools. Assessment and Intervention Strategies. New York: Guilford Press; 2003.
- Uzbay İT. Bağımlılık yapan maddeler ve özellikleri. MİSED (Türk Eczacıları Birliği Meslek İçi Sürekli Eğitim Dergisi). 2009;Aralık(21-22):16–33.
- Türkcan A. Alkolün Biyolojik Etkileri, Farmakolojisi, Emilimi, Dağılımı, Metabolizması ve Organ Sistemleri Üzerine Etkileri. Turkiye Klinikleri J Psychiatry Special Top. 2010;3(3):30–36.
- İT U. Alkol, Farmakolojik özellikleri ve alkol bağımlılığının nörofarmakolojik yönü. Ege Psikiyatri Sürekli Yayınları (Alkol kullanım bozuklukları ve tedavisi). 1996;1(2):227–254.
- Türkyılmaz M, Özsüt H. Direnci Azalmış Konaklarda Görülen İnfeksiyonlar:Alkol Bağımlılarında Görülen İnfeksiyonlar ve Ateş. Klimik Dergisi. 2018;31:145–148.
- Kilic E, Rezvani A, Toprak AE, Erman H, Ayhan SK, Poyraz E, et al. Evaluation of neutrophil to lymphocyte and platelet to lymphocyte ratios in rheumatoid arthritis. Dicle Med J. 2016;43(2):241–247.
- Yilmaz A, Can Y, Bozkurt M, Evren C. Alkol ve Madde Bagimliliginda Remisyon ve Depresme/Remission and Relapse in Alcohol and Substance Addiction. Psikiyatride Guncel Yaklasimlar. 2014;6(3):243.
- Guzel D, Yazici AB, Yazici E, Erol A. Alterations of the hematologic cells in synthetic cannabinoid users. J Clin Lab Anal. 2017;31(6):e22131.
- Guzel D, Yazici AB, Yazici E, Erol A. Evaluation of Immunomodulatory and Hematologic Cell Outcome in Heroin/Opioid Addicts. J Addict. 2018;2018:2036145. PubMed PMID: 30631635.
- Jesse S, Brathen G, Ferrara M, Keindl M, Ben-Menachem E, Tanasescu R, et al. Alcohol withdrawal syndrome: mechanisms, manifestations, and management. Acta Neurol Scand. 2017 Jan;135(1):4–16. PubMed PMID: 27586815. Pubmed Central PMCID: PMC6084325. Epub 2016/09/03. eng.
- Becker HC. Alcohol dependence, withdrawal, and relapse. Alcohol Res Health J Natl Inst Alcohol Abuse Alcohol. 2008;31(4):348–361. PubMed PMID: 23584009.
- Antonopoulos, CN, Kadoglou, NP, 2016. Biomarkers in silent traumatic brain injury. Curr Pharm Des. 22, 680-7.
- Al-Ayadhi, LY, Mostafa, GA., 2012. A lack of association between elevated serum levels of S100B protein and autoimmunity in autistic children. J Neuroinflammation. 16, 9-54.
- Nelson, PG., Kuddo, T, Song, EY, Dambrosia, JM, Kohler, S, Satyanarayana, G, Vandunk, C, Grether, JK, Nelson, KB, 2006. Selected neurotrophins, neuropeptides, and cytokines: developmental trajectory and concentrations in neonatal blood of children with autism or Down syndrome. Int J Dev Neurosci. 24,73-80.
- Mabunga DF, Gonzales EL, Kim JW, Kim KC, Shin CY. Exploring the Validity of Valproic Acid Animal Model of Autism. Exp Neurobiol 2015;24(4):285-300.
- Crawley JN. Mouse behavioral assays relevant to the symptoms of autism. Brain Pathol 2007;17(4):448-59.
- Wink LK, Adams R, Horn PS, Tessier CR, Bantel AP, Hong M, et al. A Randomized Placebo-Controlled Cross-Over Pilot Study of Riluzole for Drug-Refractory Irritability in Autism Spectrum Disorder. J Autism Dev Disord 2018;48(9):3051-3060.

