ABSTRACT
Overweight and obesity in childhood are highly preventable and parents are key role models in the establishment of healthy behaviours. The aim of this study was to assess the effectiveness of family-based interventions for prevention of overweight and obesity in children aged 2–6 years. A systematic literature search was performed in the databases such as Medline, PsycInfo, Family Study Abstracts, Embase, and CINAHL, published between 2010 and May 2019. The eligible studies were preventive randomised controlled interventions targeting the child or the child’s caregivers. The primary outcome was body mass index (BMI).
Twelve trials were included with a total of 3506 participants. The overall follow-up rate in the intervention groups was 83% as compared to 82% in the control groups. Nine trials had a high or unclear risk of bias. The children were followed for between 6 weeks and 3 years. Four of the interventions showed significant intervention effects on BMI. Significant effects on children’s food intake were reported in one (of five) study, whereas no significant changes in physical activity were found (six studies). Two studies (of six) measuring sedentary behaviours and one (of three) measuring sleep showed significant differences between groups favouring the intervention group.
The current evidence for the effects of preventive family interventions is limited. The four trials showing positive effects on BMI were multicomponent interventions, lasting for a minimum of 12 weekly sessions.
KEYWORDS:
Background
The trends in childhood obesity are becoming a growing concern worldwide. According to the World Health Organization (WHO, Citation2016), it was estimated that over 41 million children under 5 years of age were classified as overweight or obese. Projections suggest that the number of overweight or obese young children will increase to 70 million by 2025 if current trends continue (CitationWorld Health Organization). Children who are overweight at the beginning of adolescence often have excessive weight as early as 3 years of age (Lagstrom et al. Citation2008). In addition, inflammatory markers have been associated with obesity in children as young as age three, causing more concern for the high prevalence of obesity among children in the 2–5 age groups (Skinner et al. Citation2010). In the USA, it has been highlighted that by the time children enrol in school, they have already been exposed to a variety of unhealthy foods and more than 20% of 2- to 5-year-old children are at risk of overweight, or are already overweight (Birch and Ventura Citation2009). High prevalence rates are evident in North America, Europe, and parts of the Western Pacific (Lobstein et al. Citation2004; Wang and Lobstein Citation2006). However, the WHO indicates that the most rapid rises are occurring in low- and middle-income countries (CitationWorld Health Organization).
Overweight and obesity are highly preventable and there have been various debates in literature about what may be the most effective approach to tackling childhood obesity. Birch and Ventura (Citation2009) highlight that the majority of obesity prevention interventions have been school-based, focusing on elements of decreasing sedentary behaviours, increasing physical activity, and reducing weight gain. Overall, these interventions have not yielded many significant results, irrespective of the fact that children spend most of their time at school. Meanwhile, it was postulated that childcare settings may prove an excellent catchment area to implement overweight and obesity prevention interventions targeting infants, toddlers, and pre-schoolers (Ward et al. Citation2010). Parents are most likely to act as role models to their children and influence physical activity, eating behaviours, and other habits of their offspring. Yavuz et al. (Citation2015) concluded that interventions targeting young children that require parental involvement are effective but only at short-term follow-up. Summerbell et al. (Citation2012) and Lopez-Dicastillo et al. (Citation2010) posit that interventions aimed at obesity prevention could include a parental component such as role modelling. Healthy nutrition in the first years of life is critical as food preferences and eating patterns are established early in life (Pearce and Langley-Evans Citation2013).
The prevailing risk factors for increased childhood overweight and obesity are both modifiable and non-modifiable. The modifiable include factors such as poor nutrition/dietary habits, sedentary behaviour, physical inactivity, increased maternal weight gain, smoking during gestation, suboptimal amounts of sleep, and shorter than the recommended duration of breastfeeding (French et al. Citation2001; Wojcicki and Heyman Citation2010; Yan et al. Citation2014; Felső et al. Citation2017). The non-modifiable include genetic variants and other obesogenic environments (environments that promote weight gain).
The risk of overweight and obesity can be passed from one generation to the next because of exposure to an unhealthy environment that encourages weight gain (Lake and Townshend Citation2006). Introduction of energy-dense and nutrient-poor food to infants and young children is identified as a key contributor to childhood overweight and obesity (CitationWorld Health Organization; Pearce and Langley-Evans Citation2013). Parental obesity also has an influence on childhood obesity (Reilly et al. Citation2005; McPherson et al. Citation2014). The subsequent trickle-down effects of childhood obesity in adult life pose greater health problems, with an overwhelming burden in medical care involved in treating the outcomes involved in treating the complications of obesity throughout adult life (Katzmarzyk et al. Citation2014). Obese children are at a higher risk of adverse health conditions such as type 2 diabetes, dyslipidaemia, fatty liver diseases, asthma, hypertension, as well other social and psychological challenges such as stigmatizations and depression (Lobstein et al. Citation2004; Taras and Potts-Datema Citation2005; Geier et al. Citation2007; Foltz et al. Citation2012). When compared to children with normal weight, obese children have lower health-related quality of life (Katzmarzyk et al. Citation2014). According to Geier et al. (Citation2007), obesity-related health problems account for absenteeism, and poor school performance among obese children.
There are few systematic literature reviews on prevention of early childhood obesity with focus on family-based interventions, defined as interventions directly targeting parents and/or their children, contrasting to interventions that are for example targeting teachers in schools or nurses in healthcare settings. According to this definition, “targeting children” may not necessarily mean that the child is physically present at the group sessions. Even studies where the child is approached indirectly, like when the parent is taught how to practice behaviour modification strategies to improve nutritional family habits, increase physical activity or reduce the child’s screen time, are defined as targeting parents and children. A review by Waters et al. (Citation2011) highlighted that there were beneficial effects on BMI of child obesity prevention intervention programmes that targeted children in the age ranges 6–12 years. Another review by Loveman et al. (Citation2015) focused on children aged 5–11 years indirectly, by only targeting their parents, and it concluded that parent-only interventions may be effective for overweight or obese children in this age range. A Cochrane review by Colquitt et al. (Citation2016) focused on employing diet, physical activity, and behavioural interventions for the treatment of overweight or obesity in preschool children up to the age of 6 years. The conclusions were that multicomponent interventions were more effective in terms of reducing BMI. A review by Ling et al. (Citation2016) examined the effects of prevention and management interventions on overweight/obesity among children aged 2–5 years and concluded that management interventions showed greater effects in weight loss as compared to prevention interventions. Further, a recent systematic review on prevention of obesity (Reilly et al. Citation2019) reported results for children aged 2–4 years old separately. In this review, including physical activity as intervention, 11 of 16 studies reported no effect on BMI. The trials showing effect had multiple components; physical activity was combined with interventions targeting diet and sedentary behaviour. In line with this, another recent review (Brown et al. Citation2019) found that multicomponent trials including a combined diet and physical activity intervention reduced BMI in children aged 2–5, while neither diet nor physical activity alone had any effect.
It can be deduced from above that there is a knowledge gap about the effectiveness of interventions targeting parents and/or children with the aim to prevent child obesity. How interventions should be designed and which behavioral changes to target remains unclear. Thus, increased knowledge about effective methods targeting families is important. This review builds on current literature and adds to the evidence-base on effectiveness of preventive interventions targeting children in the age span of 2–6 years with a focus on changing habits in children and their parents. This review involves assessing quantitative literature reporting on educational, behavioural, and health-promotion interventions.
Objectives
To assess the effectiveness of family-based interventions for prevention of overweight and obesity in children aged 2–6 years.
Method
Inclusion criteria
Randomized controlled trials, randomized either at cluster or individual level
Preventive lifestyle interventions, targeting parents and/or their children irrespective of the child being underweight, normal weight, overweight, or obese according to BMI percentile or zBMI-score
Age range of child 2–6 years
Exclusion criteria
Parents and/or children who were critically ill, or had serious psychiatric impairments
Interventions that were not targeting parents and/or children, for example school-based projects where the intervention was training teachers
Primary outcome
Changes in body mass index (BMI) and body weight, defined as changes in BMI (kg/m2) and body weight (kg) measured at baseline and at follow-up
Secondary outcomes
Behavioural change defined as validated measures of dietary intake, physical activity, sedentary behaviours and sleep time, measured at baseline and at follow-up
Adverse events, defined as an adverse outcome that occurred during or after the intervention but was not necessarily caused by it and is measured at baseline and follow-up
Search methods for identification of studies
The databases Medline, PsycInfo, Family Study Abstracts, Embase, and CINAHL were searched for electronic literature during the period 10 February 2016 to 29 February 2016. The search terms “overweight”, “obesity”, and “prevention” were used as key search terms for the searches conducted in the databases. The searches were limited to academic journals published in English between 2010 and 2016, with age limit 2–6 years. The search was later updated on 30 April 2019. Further details on searches made in the databases can be found in Appendix I.
Data selection and analysis
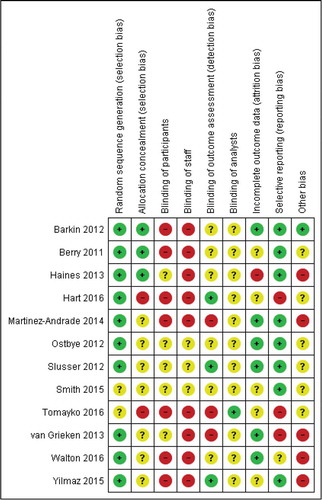
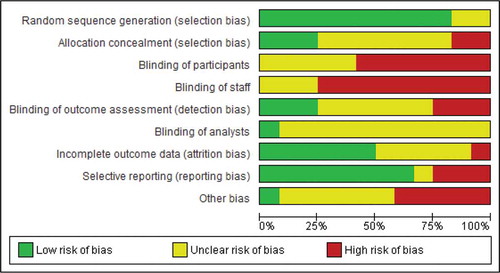
After the search in 2016, three of the four review authors (KL, AQ andIT) independently screened the titles and abstracts of the hits obtained after removal of duplicates. All potentially relevant studies were then assessed as full text. Comparisons of the selected studies were made independently by the authors. After the second search, conducted 2019, IT screened the titles, read abstracts and selected articles. KL assessed the selected articles in full text and discussed inclusion with all authors. Any disagreements arising were discussed collectively and resolved among the review authors. In , we present an adapted Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines (Moher et al. Citation2010) flow diagram showing the selection process. Data from the included trials were extracted by means of a data extraction form agreed upon by all four authors (KL, AQ, EH and IT), and based on the Consolidated Standard of Reporting Trials (CONSORT) checklist (Turner et al. Citation2012). Extracted information included author name and year, study design, participant characteristics, types of interventions, outcome measures. The Cochrane Handbook for Systematic Reviews of Interventions 5 (Higgins and Green Citation2011) was used in the risk of bias assessment of the selected studies. The included studies were assessed at six levels: randomizations, concealment of study intervention allocation, blinding, and the completeness of follow-up, selective outcome reporting, and other sources of bias. All six levels of assessment were judged either as having “Low risk of bias”, “High risk of bias”, or “Unclear risk of bias”, according to the guidelines given in the handbook. Due to variations in interventions, measures of outcome, and participants, it was inappropriate to combine the results statistically across studies. Instead, participant characteristics, intervention components, follow-up, and outcome measures were summarized for each study and results were reported narratively.
Results
Results of the search
shows the study flow diagram with the results of electronic and manual searches from 2016 and 2019. N = 7103 hits were retrieved from the databases and n = 4577 citations were left after removal of duplicates. Screening of titles and abstracts identified n = 263 initial eligible studies. N = 20 of the articles were not accessible and had to be ordered through the Lund University Library at the Health Science Centre in Lund. N = 51 full-text articles were retrieved. The reference lists of the full-text articles were screened to obtain n = 1 more article. Discussions about the eligibility of the articles were held among the review authors, and a final n = 12 articles (n = 10 from the first search and n = 2 from the second search) that fulfilled the inclusion criteria were included in the review.
Included studies
The characteristics of the included studies are presented in . The 12 included studies had 3506 participants, with 20.5% (731) of the participants from one trial (Smith et al. Citation2015). Further, 1797 of the participants were allocated to the intervention arm while the remaining 1709 were allocated to the control arm. It was not clearly indicated how many of the 56 participants in the trial by Berry et al. (Citation2011) were randomized to intervention and control groups. In considering the total number of randomized participants, the overall follow-up rate in the intervention groups was 83% as compared to 82% in the control groups for 10 of the trials. Number of completers in two of the trials (Berry et al. Citation2011; Smith et al. Citation2015) was not provided.
Table 1. Characteristics of included studies
Excluded studies
Of 51 full-text articles, 39 did not meet the inclusion criteria. The main reasons for exclusion were participant’s age at baseline and the study designs employed. See the characteristics of excluded studies in Appendix II for further details.
Settings
The interventions were conducted in a primary care setting in three of the trials (Slusser et al. Citation2012; van Grieken et al. Citation2013; Martínez-Andrade et al. Citation2014). Six trials were home-based (Østbye et al. Citation2012; Haines et al. Citation2013; Smith et al. Citation2015; Yilmaz et al. Citation2015; Tomayko et al. Citation2016; Hart et al. Citation2016). Three trials used community centres (Berry et al. Citation2011; Barkin et al. Citation2012; Walton et al. Citation2016). Seven of the studies were conducted in the USA (Berry et al. Citation2011; Barkin et al. Citation2012; Østbye et al. Citation2012; Slusser et al. Citation2012; Haines et al. Citation2013; Smith et al. Citation2015; Tomayko et al. Citation2016). One study was conducted in Mexico (Martinez-Andrade et al., Citation2014), one in Canada (Walton et al. Citation2016), one in the Netherlands (van Grieken et al. Citation2013), one in Turkey (Yilmaz et al. Citation2015) and one in Australia (Hart et al. Citation2016).
Participants
The trials enrolled children from 2 years of age, with a range up to age 4 (Berry et al. Citation2011; Slusser et al. Citation2012; Smith et al. Citation2015), age 5 (Østbye et al. Citation2012; Haines et al. Citation2013; Martínez-Andrade et al. Citation2014; Walton et al. Citation2016; Tomayko et al. Citation2016) or age 6 (Barkin et al. Citation2012; van Grieken et al. Citation2013; Yilmaz et al. Citation2015; Hart et al. Citation2016).
The BMI weight status of children in four of the trials (Smith et al. Citation2015; Yilmaz et al. Citation2015; Hart et al. Citation2016) was not specified in the inclusion criteria. Seven trials (Barkin et al. Citation2012; Østbye et al. Citation2012; Slusser et al. Citation2012; Haines et al. Citation2013; van Grieken et al. Citation2013; Martínez-Andrade et al. Citation2014; Tomayko et al. Citation2016) included children falling in the BMI weight categories of normal weight (<85th percentile), overweight (≥85th – <95th percentile), and obese (≥95th percentile). One trial (Berry et al. Citation2011) included children at any BMI percentile while two trials (Barkin et al. Citation2012; Østbye et al. Citation2012) further included children who were categorized as underweight. Martínez-Andrade et al. (Citation2014) used the WHO zBMI-score categories where normal = ≤1.0, risk of overweight = >1.0 – ≤2.0, and overweight = >2.0. One trial (Walton et al. Citation2016) described the weight status of children as normal, overweight, or obese according to WHO cut points. BMI weight statuses of parents were measured in (Barkin et al. Citation2012; Slusser et al. Citation2012; Haines et al. Citation2013; van Grieken et al. Citation2013; Hart et al. Citation2016; Tomayko et al. Citation2016) and parent being either overweight or obese were an inclusion criterium in two of the trials (Berry et al. Citation2011; Østbye et al. Citation2012).
Risk of bias in the included studies
The review authors’ judgements about each risk of bias per item presented as percentages across all included studies are presented in and the authors’ judgements about each risk of bias item for each included study are presented in . The authors’ detailed judgement and explanation for assessment of risk of bias are presented in Appendix III.
Effects of interventions
See the summary of findings for the main comparison in . The outcomes considered in this review fall into two main categories: physical health status and behavioural change. Physical health status, which is the primary outcome in this review, includes measures of BMI, BMI percentiles or zBMI (all 12 trials). Behavioural change, which is the secondary outcome in this review, includes measures related to food intake (five trials), physical activity (four trials), sedentary behaviour (six trials) and sleep time (three trials).
Table 2. Summary of main findings on primary outcome; BMI, BMI percentiles and BMI z score
Primary outcomes
BMI
In the 12 trials, 1797 participants were randomized to the intervention group whereas 1661 participants were randomized to the control group. One trial (Berry et al. Citation2011) did not specify how many participants were randomized to intervention and control groups. In general, compared with their respective control groups, four of the interventions (Berry et al. Citation2011; Barkin et al. Citation2012; Slusser et al. Citation2012; Smith et al. Citation2015) showed significant effects of the intervention on BMI, irrespective of the length of follow-up. Barkin et al. (Citation2012), found statistically significant effects of the intervention (12 weekly 90-minutes skill-building sessions) on absolute BMI post intervention, when covariates (child age at baseline, child gender, and baseline absolute BMI) were adjusted for. Focusing on changes in BMI across weight categories, Barkin et al. (Citation2012) found that the most pronounced difference in BMI change between treatment and control groups occurred among obese children. Similar trends were reported for those children who were overweight at baseline. Children initially categorized as normal weight at baseline in the intervention group decreased their BMI more than the normal weight children in the control group did. In the trial by Haines et al. (Citation2013), although change in BMI across weight categories was not reported, it was highlighted that child BMI had decreased in both the intervention and the control groups. In this study (Haines et al. Citation2013), the intervention group received motivational coaching during home visits and by telephone, mailed educational material and text messages while the control group received mailed information on developmental milestones. The Tomayko et al study (Citation2016), where the treatment group received 12 healthy behaviour toolkit lessons delivered by a mentor and the control group received the same kit by mail, found a significant decrease in BMI in both groups but no differences between groups. Smith et al. (Citation2015), having assessed BMI after a 3-year intervention including home visits and meal preparation, still found that there was a significant indirect effect of the intervention on the trajectory of BMI later in childhood. The intervention also prevented progression to overweight and obese status among at-risk children. In two of the trials with long-term follow-up (Berry et al. Citation2011; Slusser et al. Citation2012), there were significant differences in BMI between intervention and control groups. Children allocated to the intervention group stabilized their weight and significantly decreased their BMI percentile as compared to children in the control groups whose BMI increased (Berry et al. Citation2011; Slusser et al. Citation2012). In these studies, the intervention included nutrition and exercise education, coping skills training and physical activity (Berry et al. Citation2011) and nine class sessions designed to incorporate healthy nutrition and physical activity (Slusser et al. Citation2012).
Meanwhile, six of the trials (Østbye et al. Citation2012; Haines et al. Citation2013; Martínez-Andrade et al. Citation2014; Yilmaz et al. Citation2015; Tomayko et al. Citation2016; Walton et al. Citation2016) did not find any significant effects of the intervention on BMI either at short-term follow-up (Østbye et al. Citation2012; Haines et al. Citation2013; Martínez-Andrade et al. Citation2014; Tomayko et al. Citation2016; Walton et al. Citation2016) or long-term follow-up (van Grieken et al. Citation2013; Yilmaz et al. Citation2015; Walton et al. Citation2016). In the trial by Yilmaz et al. (Citation2015), there were increases in zBMI scores in both the intervention group (who received four components at two weeks intervals including printed material, interactive CDs and one counselling call aimed to reduce screen time) and in the control group (that constituted a wait-list group) but no differences between groups. The trial by van Grieken et al. (Citation2013), found no significant differences at follow-up with regard to BMI. However, mildly overweight children (BMI 17.25 and 17.50) allocated to the intervention that included information and motivational interviewing and three structured counselling sessions, had significantly smaller increases in BMI compared to children who were more overweight. There were no effects of the intervention that included group sessions related to parental roles in promoting healthy nutrition and activity on BMI in the trial by Walton et al. (Citation2016), either post intervention or at the 9-month follow-up.
Secondary outcomes
Food intake, location when eating and parental feeding behaviours
Five studies included dietary outcome measures (Østbye et al. Citation2012; Smith et al. Citation2015; Walton et al. Citation2016; Tomayko et al. Citation2016; Martinez-Andrade et al. Citation2014). These five studies included in total 831 families in the intervention groups and 810 families in the control groups. In total, 69% of the families completed follow-up in the intervention groups and 75% in the control groups. Data on completers in one of the trials (Smith et al. Citation2015) were not provided. One of the studies reported a short follow-up (6 months) (Martínez-Andrade et al. Citation2014) and the other four reported follow-up periods longer than 6 months.
Significant intervention effects between groups on children’s food intake were reported in one of the five studies (Martínez-Andrade et al. Citation2014). Martinez-Andrade et al. (Citation2014) found a significant increase in child intake of vegetables at 3 months follow-up, after 6 weeks intervention delivered at primary care setting with focus on obesity awareness and prevention for parents, no change between intervention and control group was maintained at 6-month follow-up. Positive but insignificant effects were reported for intake of sweet snacks and sugar-added drinks. Tomayko et al. 2016 reported a significant increase in child intake of fruits and vegetables in both intervention and the active control group at 1-year follow-up; however, no significant changes were seen between the groups receiving either a mentored or mailed intervention. No significant differences between groups were found in regard to children’s intake of sweet drinks (Østbye et al. Citation2012; Martínez-Andrade et al. Citation2014; Tomayko et al. Citation2016; Walton et al. Citation2016), fast food (Østbye et al. Citation2012; Martínez-Andrade et al. Citation2014), fruit and/or vegetables (Tomayko et al. Citation2016; Østbye et al. Citation2012), candy/sweet snacks/junk food (Martinez-Andrade et al. 2014; Tomayko et al. Citation2016) and nutrition risk score (Walton et al. Citation2016) in the five studies analysing dietary intake.
Besides changes in children’s food intake, the effect on children’s eating location and parental feeding behaviours was studied. Two studies reported a significant decrease in meals and snacks eaten in front of the television in the intervention group compared to the control group (Østbye et al. Citation2012; Hart et al. Citation2016). Significant intervention effects were reported for healthier parental feeding behaviours, including improved nutritional quality of served meals (Smith et al. Citation2015), reduced use of food as reward/instrumental feeding (Østbye et al. Citation2012; Walton et al. Citation2016; Hart et al. Citation2016), reduced emotional feeding (Østbye et al. Citation2012; Hart et al. Citation2016), reduced pressure to eat and weight restriction (Hart et al. Citation2016), increased self-efficacy for health-related behaviour changes (Tomayko et al. Citation2016) and improved nutrition knowledge (Berry et al. Citation2011).
Physical activity
No statistically significant changes in physical activity were found in the four trials that assessed physical activity (Østbye et al. Citation2012; Martínez-Andrade et al. Citation2014; Walton et al. Citation2016; Tomayako et al. Citation2016). These four studies included a total 464 families in the intervention groups, of whom 331 (71%) completed follow-up, and 469 families in the control groups, of whom 343 (73%) completed follow-up. In Østbye et al. (Citation2012) there were neither significant differences nor positive trends in physical activity at the 12-month follow-up. In Tomayako et al. (Citation2016) there were no significant differences between the intervention group who received home-visits and the control group who got the same program delivered by mail and no positive trend after 12 months. Likewise, there were no significant changes in physical activity behaviour in Martínez-Andrade et al. (Citation2014) at the 3-month follow-up. Rather, the usual care group had increased their physical activity more from baseline to the 3-month follow-up (9.5 hours/week compared to 2.9 hours/week in the intervention group). At the 6-month follow-up, the intervention group had caught up and reported 7.4 hours/week of physical activity compared to 6.7 hours in the usual care group. Walton et al. (Citation2016) reported a positive change for the intervention group in active play between baseline and post intervention, remaining at the 9-month follow-up, but the differences did not reach statistical significance.
Sedentary behaviours
Six studies (Østbye et al. Citation2012; Haines et al. Citation2013; Martínez-Andrade et al. Citation2014; Yilmaz et al. Citation2015; Tomayko et al. Citation2016; Walton et al. Citation2016) described outcome measurements of sedentary behaviours in terms of screen time or TV viewing. These six studies included a total of 737 families in the intervention groups where 573 (78%) completed follow-up, and 706 families in the control groups where 575 (81%) completed follow-up. The retention rate was <75% in three of the studies (Østbye et al. Citation2012; Martínez-Andrade et al. Citation2014; Tomayko et al. Citation2016). All six studies reported short follow-up (up to 6 months) while three of them also reported results at 9 months (Yilmaz et al. Citation2015; Walton et al. Citation2016) or at 2 years follow-up (Tomayko et al. Citation2016). Two studies (Haines et al. Citation2013; Yilmaz et al. Citation2015), with short follow-up, showed significant differences between groups favouring the intervention group. Three studies (Østbye et al. Citation2012; Martínez-Andrade et al. Citation2014; Walton et al. Citation2016), also with short follow-up, showed no differences between the intervention group and the control group. Of the three studies (Yilmaz et al. Citation2015; Tomayko et al. Citation2016; Walton et al. Citation2016) that reported on longer follow-up, one of them (Yilmaz et al. Citation2015) showed significant differences between intervention group and control group, where parents reported greater decrease of children’s screen time in the intervention group compared with the control group. One of the studies with longer follow-up periods (Tomayko et al. Citation2016) reported a significant decrease in screen time but there was no difference between the intervention group who received the toolkit by a mentor and the control group who received the toolkit by mail.
Sleep time
Three studies included outcome measurements of sleep duration (Haines et al. Citation2013; Martínez-Andrade et al. Citation2014; Walton et al. Citation2016), with short follow-up, and one of them also reported on longer follow-up at 9 months (Walton et al. Citation2016). The three studies included a total of 259 families in intervention groups, where 167 completed the follow-up (65%), and 222 families were included in control groups, where 173 (78%) completed follow-up. Haines et al. (Citation2013) showed a significant intervention effect for sleep duration, where child sleep duration increased in the intervention group who received motivational coaching, mailed educational materials and text messages, and decreased in the control group who received mailed material on child development. Martínez-Andrade et al. (Citation2014) showed no significant differences between the intervention group who participated in a program aimed to promote healthy habits and the control group who received usual care. Walton et al. (Citation2016) did not find any differences at the nine-month follow-up period between the intervention group who participated in group sessions focusing on weight-related topics and the control group who participated in group sessions focusing on child injury prevention.
Adverse events
None of the studies reported any adverse events.
Discussion
This systematic review summarized 12 RCTs examining the effect of family-based obesity preventive interventions. Eleven of the 12 trials were multicomponent interventions, targeting more than one behaviour, whereas only one trial was single-component study targeting only screen time (Yilmaz et al. Citation2015). Of these 11 multicomponent trials, only 4 trials showed significant effects of the interventions on reducing child BMI (Berry et al. Citation2011; Barkin et al. Citation2012; Slusser et al. Citation2012; Smith et al. Citation2015). The interventions in these four trials included 7−12 skill-building group sessions targeting more than one behaviour (Berry et al. Citation2011; Barkin et al. Citation2012; Slusser et al. Citation2012) or three sessions tailored to the needs of each family (Smith et al. Citation2015), supporting findings that interactive interventions are most effective (Yavuz et al. Citation2015). Neither the remaining seven multicomponent interventions nor the only single-component intervention showed any significant effects of the interventions. Of the four trials whose interventions had a significant effect on child BMI; however, three were assessed to have had an unclear risk of bias overall (Berry et al. Citation2011; Barkin et al. Citation2012; Smith et al. Citation2015), whereas only one trial (Slusser et al. Citation2012) had a low risk of bias. From the results in this review, it is not possible to conclude which parts of the multicomponent interventions that had effect. However, trials with interventions showing a significant difference between intervention and control groups had interventions with a minimum of 12 weeks, with each session lasting a minimum of 45 minutes, including more than one lifestyle behaviour, in line with Reilly et al. (Citation2019) and Brown et al. (Citation2019). Of the four trials showing effects on child BMI, two targeted both parents and children (Berry et al. Citation2011; Barkin et al. Citation2012) while two targeted the parents directly and the children indirectly (Slusser et al. Citation2012; Smith et al. Citation2015).
Interventions aimed to change children’s habits require parental involvement (Reilly et al. Citation2019). Such interventions have been shown to have effect only at short time follow-up, specifically if the intervention has many components (Yavuz et al. Citation2015). The majority of the studies had follow-up periods less than 12 months, a result in line with previous reviews of the targeted age group (Niemeier, Hektner and Enger., Citation2012; Peirson et al. Citation2015; Yavuz et al. Citation2015). It can be questioned if that is an adequate time to demonstrate significant change in BMI and one possible explanation could be that longer follow-up was not published due to failure to demonstrate significant results. Part of the results of this review, which show significant effects of multicomponent trials, must nevertheless be interpreted with caution due to unclear risk of bias. Despite having assessed trials as being of low quality, Colquitt et al. (Citation2016) and Brown et al. (Citation2019) concluded that reductions in zBMI-score were more evident in multicomponent intervention groups as compared to usual care.
Two of the studies included active interventions aimed to prevent obesity in the control groups which makes it difficult to evaluate the full effect of the interventions. In Tomayko et al. (Citation2016), the control group received the same 12 lessons as the intervention group by mail but without the mentor home visits and one of the control groups in Hart et al. (Citation2016) were provided a nutrition only resource, both with possible effects but assumed to have lesser effect than the intervention. Other interventions in the control groups were active but focused on topics other than prevention of obesity, for example a school readiness program including three group sessions (Barkin et al. Citation2012), monthly mailed packages on developmental milestones (Haines et al. Citation2013), nine group sessions on child injury prevention (Walton et al. Citation2016) or montly newsletters emphazising pre-reading skills (Østbye et al. Citation2012). Few studies used standard care (Slusser et al. Citation2012; van Grieken et al. Citation2013; Martínez-Andrade et al. Citation2014; Smith et al. Citation2015) or waitlist (Berry et al. Citation2011) as control. Among the four studies showing effect on BMI, two had chosen care as usual (Slusser et al. Citation2012; Smith et al. Citation2015) and one had wait list (Berry et al. Citation2011) as intervention in the control group. One of the studies showing effect had a program focusing on a topic other than obesity prevention (Barkin et al. Citation2012). This finding might guide the design of future studies.
Four out of five studies that included dietary outcome measures reported results of follow-up periods longer than 6 months (Østbye et al. Citation2012; Smith et al. Citation2015; Walton et al. Citation2016; Tomayko et al. Citation2016). The risk of bias was assessed to be high in two of these studies (Walton et al. Citation2016; Tomayko et al. Citation2016) and unclear in the two others (Østbye et al. Citation2012; Smith et al. Citation2015). Significant difference in children’s dietary intake between the intervention and control group was reported in one of the five studies including dietary outcome measures (Martínez-Andrade et al. Citation2014). The design of the intervention in this study included physical meetings in children’s centres with follow-up at 3 and 6 months (Martínez-Andrade et al. Citation2014). The results from this review highlight the difficulty of changing long-term dietary behaviours and more specifically the challenge of reducing children’s consumption of unhealthy foods. No significant intervention effects were reported for intake on unhealthy snacks (Martínez-Andrade et al. Citation2014), sugar (Martínez-Andrade et al. Citation2014), candy, junk food and fast food (Østbye et al. Citation2012; Tomayko et al. Citation2016). On the other hand, two out of five studies found increased consumption of fruits and/or vegetables (Martínez-Andrade et al. Citation2014; Tomayko et al. Citation2016) indicating that interventions focusing on increasing healthy foods have been more successful. In line with this, a smartphone-based study (Nyström et al. Citation2017), a study with 8 weeks’ intervention of home-based parental training on habit formation for healthy feeding behaviours (McGowan et al. Citation2013), and a web-based trial (Knowlden and Conrad Citation2018) reported changes in children´s dietary intake mainly resulting from increased intake levels of healthy foods. A trial targeting the home food environment of preschool children where parents in the intervention group received four weekly 30-minute telephone calls and written resources (Wyse et al. Citation2014) resulted in a significantly higher fruit and vegetable consumption of parents.
Several of the studies in the present review including dietary measures also reported significant improvements in parental feeding behaviours. This is promising since parental and family modelling of healthy eating behaviours and environments promoting healthy diets are suggested to be factors with great influence on children’s eating patterns (Mazarello Paes et al. Citation2015; DeCosta et al. Citation2017). However, a recent parent-focused eHealth study targeting parents to overweight children (Hammersley et al. Citation2019) provided parents in both groups with internet-based information on preventing obesity in preschoolers and added individual communication with a dietician and a facebook-chat with the dietician and other parents to the intervention group. The results showed improved dietary-related practices but no differences between groups in child BMI, indicating that targeting only the parents is not sufficient. Contrasting to Hammersley et al. (Citation2019), two of the studies in the present review including interventions where the children were not directly involved showed lower BMI in the children (Slusser et al. Citation2012; Smith et al. Citation2015). The results of this review, in terms of dietary measures, indicate that the studied interventions can be effective in changing families’ eating and feeding behaviours, especially by promoting increased intake of healthy foods. However, more knowledge is needed to draw conclusions on best practices and how to sustain long-term positive effects. Lacking evidence on the factors influencing obesogenic dietary habits in young children has also been stated in previous systematic reviews (Hesketh and Campbell Citation2010; De Craemer et al. Citation2012; Te Velde et al. Citation2012; Mazarello Paes et al. Citation2015).
No significant changes were found in the four trials that assessed physical activity (Østbye et al. Citation2012; Martínez-Andrade et al. Citation2014; Walton et al. Citation2016; Tomayko et al. Citation2016), indicating that introducing more physical activity is a challenge. All four studies were assessed to have high and/or unclear risks of bias as they were based on parental self-reports. Although one study (Walton et al. Citation2016) reported a positive but non-significant change in active play in the intervention group remaining at the 9-month follow-up, Østbye et al. (Citation2012) did not even find a positive trend in physical activity at the 12-month follow-up. Martínez-Andrade et al. (Citation2014) found a negative trend the first 3 months; physical activity actually increased more in the control group. These results are in line with a systematic review (Waters et al. Citation2011) where the effect of different interventions had no effect on increasing physical activity in any of the four studies including children 0–5 years and with two recent studies (Nyström et al. Citation2017; Knowlden and Conrad Citation2018). Waters et al. (Citation2011) concluded that it is important to conduct studies identifying how effective intervention components can be embedded within health. Interventions to increase physical activity in older children showed an effect in some studies, pointing towards a possibility of changing lifestyle towards healthier habits (Waters et al. Citation2011).
The six studies that included measurement of sedentary behaviours (Østbye et al. Citation2012; Haines et al. Citation2013; Martínez-Andrade et al. Citation2014; Yilmaz et al. Citation2015; Tomayko et al. Citation2016; Walton et al. Citation2016) and the three studies who also reported sleep time (Haines et al. Citation2013; Martínez-Andrade et al. Citation2014; Walton et al. Citation2016) were assessed to have both high and unclear risks of bias. Two studies showed significant differences in sedentary behaviour between groups, favouring the intervention group (Haines et al. Citation2013; Yilmaz et al. Citation2015). One of them (Haines et al. Citation2013) was a behavioural multicomponent intervention delivered over 9 weeks and the other one (Yilmaz et al. Citation2015) was a single-component intervention (over 6 weeks) with the focus on reducing screen time. The six studies that did not show any significant differences between groups differed in terms of how intense they were, the length, and focus of the intervention. The results of this review in terms of sedentary behaviour are inconsistent and we found no convincing evidence for the effectiveness of existing interventions. This result is in line with a recently published review of interventions targeting solely sedentary behaviour (Altenburg, Kist-van Holthe, & Chinapaw, Citation2016). However, a meta-analysis by (Biddle et al. Citation2014) showed that interventions aiming to reduce children’s sedentary behaviour had a small but significant effect, with a trend favouring interventions with children younger than 6 years.
An extensive search of RCTs aimed at childhood overweight and obesity prevention and fulfilling the review’s inclusion criteria was conducted. However, there may be a possibility that substantial information could have been missed from non-English publications, as only publications in English were selected, and from articles published before 2010. The evidence of studies in this review is generally applicable to the public health sector of developed countries, and it is not certain whether it is transferable to other countries. Future research may need to focus on developing countries. A number of other limiting factors were present based on the individual risk of bias in the included trials, the quality of the evidence was low due to possible factors observed in the risk assessments. Most of the trials provided clear descriptions of the randomization procedures as well as reporting of pre-specified outcome measures, therefore having a low risk of bias. Overall, most of the studies were assessed to have had an unclear risk of bias across a number of domains. The studies included BMI as an objective measure which could be said to have reduced the impact of the outcome assessors not being blinded. However, the fidelity of most parts of the interventions is unknown, and subjective measures of outcomes such as television viewing time, dietary habits, physical activity and sedentary time need to be interpreted with caution as they were based on parental self-reports, and in addition, staff and participants were not blinded in most of the trials. However, there were inconsistencies in the descriptions of how allocations were concealed, blinding of participants, staff, and outcome assessors. Only one study (Tomayko et al. Citation2016) reported on the blinding of analysts, which made it impossible to assess the impact on obtainable results. This presents more difficulties in the overall presentation of the data and thus highlights the need for more robust reporting of research methods.
Author’s conclusions
Implications for practice
The burden and long-term effects of childhood overweight and obesity are major public health concerns. Effective interventions aimed at preventing childhood obesity need to begin early in life, before children even begin school as such interventions may have meaningful long-term effects in preventing childhood obesity. It is crucial to target parents as role models and empower them to actively be part of childhood overweight and obesity prevention interventions. Also, multicomponent interventions might be an effective treatment in the prevention of childhood overweight and obesity, although more evidence is needed since only four of 12 trials showed a positive effect on BMI. The current evidence is limited as it is not clear what elements should constitute a multicomponent intervention, and most of the trials had an unclear risk of bias. Nevertheless, a common aspect among the four multicomponent trials showing positive effects is that they included an intervention with a minimum of 12 weeks, lasting for a minimum of 45 minutes per session, and focusing on more than one lifestyle behaviour. Since none of the trials reported adverse events, it is crucial for further research to investigate this outcome in the interventions.
The current evidence is limited as it is not clear what elements should constitute a multicomponent intervention.
However, a common aspect among the four multicomponent trials showing positive effects is that they included an intervention with a minimum of 12 weeks, lasting for a minimum of 45 minutes per session, and focusing on more than one lifestyle behaviour.
Acknowledgments
The authors would like to acknowledge Alexandra Forsberg and Matthias Bank (Library & ICT Unit, Faculty of Medicine, Lund University) for support in the development of search strategies. The study was supported by FORTE.
Disclosure statement
The authors report no conflict of interest.
Additional information
Funding
References
- Altenburg TM, Kist-van Holthe J, Chinapaw MJM. 2016. Effectiveness of intervention strategies exclusively targeting reductions in children’s sedentary time: a systematic review of the literature. Int J Behav Nut Phy Act. 13(1):65. doi:10.1186/s12966-016-0387-5.
- Barkin SL, Gesell SB, Po’e EK, Escarfuller J, Tempesti T. 2012. Culturally tailored, family-centered, behavioral obesity intervention for Latino-American preschool-aged children. Pediatrics. 445-456 412p. 130(3):445–456. doi:10.1542/peds.2011-3762.
- Berry D, Colindres M, Sanchez-Lugo L, Sanchez M, Neal M, Smith-Miller C. 2011. Adapting, feasibility testing, and pilot testing a weight management intervention for recently immigrated Spanish-speaking women and their 2- to 4-year-old children. 186-193 188p. Hispanic Health Care International. (4):9. doi:10.1891/1540-4153.9.4.186
- Biddle SJH, Petrolini I, Pearson N. 2014. Interventions designed to reduce sedentary behaviours in young people: a review of reviews. Brit J Sports Med. 48(3):182–186. doi:10.1136/bjsports-2013-093078.
- Birch LL, Ventura AK. 2009. Preventing childhood obesity: what works? Int J Obes (Lond). 33(Suppl 1):S74–81. doi:10.1038/ijo.2009.22.
- Brown T, Moore TH, Hooper L, Gao Y, Zayegh A, Ijaz S, Elwenspoek M, Foxen SC, Magee L, O’Malley C, et al. 2019. Interventions for preventing obesity in children. Cochrane Database of Systematic Reviews. 7. doi:10.1002/14651858.CD001871.pub4.
- Colquitt JL, Loveman E, O’Malley C, Azevedo LB, Mead E, Al-Khudairy L, … Rees K. 2016. Diet, physical activity, and behavioural interventions for the treatment of overweight or obesity in preschool children up to the age of 6 years. Cochrane Database Syst Rev. 3:Cd012105. doi:10.1002/14651858.cd012105
- De Craemer M, De Decker E, De Bourdeaudhuij I, Vereecken C, Deforche B, Manios Y, Cardon G. 2012. Correlates of energy balance‐related behaviours in preschool children: a systematic review. Obesity Reviews. 13(s1):13–28.
- DeCosta P, Moller P, Frost MB, Olsen A. 2017. Changing children’s eating behaviour - A review of experimental research. Appetite. 113:327–357. doi:10.1016/j.appet.2017.03.004
- Felső R, Lohner S, Hollódy K, Erhardt É, Molnár D. 2017 Sep. Relationship between sleep duration and childhood obesity: systematic review including the potential underlying mechanisms. Nutr Metab Cardiovasc Dis. 27(9):751–761. Epub 2017 Jul 25. doi:10.1016/j.numecd.2017.07.008.
- Foltz JL, May AL, Belay B, Nihiser AJ, Dooyema CA, Blanck HM. 2012. Population-level intervention strategies and examples for obesity prevention in children. Annu Rev Nutr. 32(391–415):325p. doi:10.1146/annurev-nutr-071811-150646.
- French SA, Story M, Jeffery RW. 2001. Environmental influences on eating and physical activity. Annu Rev Public Health. 22:309–335. doi:10.1146/annurev.publhealth.22.1.309
- Geier AB, Foster GD, Womble LG, McLaughlin J, Borradaile KE, Nachmani J, … Shults J. 2007. The relationship between relative weight and school attendance among elementary schoolchildren. Obesity (Silver Spring). 15(8):2157–2161. doi:10.1038/oby.2007.256.
- Haines J, McDonald J, O’Brien A, Sherry B, Bottino CJ, Schmidt ME, Taveras EM. 2013. Healthy habits, happy homes: randomized trial to improve household routines for obesity prevention among preschool-aged children. JAMA Pediatrics, 167 (11),1072-10791078p. doi:10.1001/jamapediatrics.2013.2356
- Hammersley ML, Okely AD, Batterham MJ, Jones RA. 2019. An internet-based childhood obesity prevention program (Time2bHealthy) for parents of preschool-aged children: randomized controlled trial. J Med Internet Res. 21(2):e11964.
- Hart LM, Damiano SR, Paxton SJ. 2016. Confident body, confident child: a randomized controlled trial evaluation of a parenting resource for promoting healthy body image and eating patterns in 2- to 6-year-old children. Int J Eat Disord. 49:458–472.
- Hesketh KD, Campbell KJ. 2010. Interventions to prevent obesity in 0–5 year olds: an updated systematic review of the literature. Obesity. 18(S1):S27–S35.
- Higgins JP, Green S. 2011. Cochrane handbook for systematic reviews of interventions. Vol. 4. Chichester , UK: John Wiley & Sons.
- Katzmarzyk PT, Barlow S, Bouchard C, Catalano PM, Hsia DS, Inge TH, … Yanovski JA. 2014. An evolving scientific basis for the prevention and treatment of pediatric obesity. Int J Obes. 38(7): 887-905 819p doi: 10.1038/ijo.2014.49.
- Knowlden AP, Conrad E. 2018. Two-year outcomes of the enabling mothers to prevent pediatric obesity through web-based education and reciprocal determinism (EMPOWER) randomized control trial. Health Educ Behav. Apr. 45(2):262–276. doi:10.1177/1090198117732604.
- Lagstrom H, Hakanen M, Niinikoski H, Viikari J, Ronnemaa T, Saarinen M, … Simell O. 2008. Growth patterns and obesity development in overweight or normal-weight 13-year-old adolescents: the STRIP study. Pediatrics. 122(4):e876–883. doi:10.1542/peds.2007-2354.
- Lake A, Townshend T. 2006. Obesogenic environments: exploring the built and food environments. J R Soc Promot Health. 126(6):262–267.
- Ling J, Robbins LB, Wen F. 2016. Interventions to prevent and manage overweight or obesity in preschool children: A systematic review. Int J Nurs Stud. 53:270–289. doi:10.1016/j.ijnurstu.2015.10.017
- Lobstein T, Baur L, Uauy R. 2004. Obesity in children and young people: a crisis in public health. Obes Rev. 5(Suppl 1):4–104. doi:10.1111/j.1467-789X.2004.00133.x.
- Lopez-Dicastillo O, Grande G, Callery P. 2010. Parents’ contrasting views on diet versus activity of children: implications for health promotion and obesity prevention. Patient Education & Counseling. 78(1): 117-123 117p doi: 10.1016/j.pec.2009.05.019.
- Loveman E, Al-Khudairy L, Johnson RE, Robertson W, Colquitt JL, Mead EL, … Rees K. 2015. Parent-only interventions for childhood overweight or obesity in children aged 5 to 11 years. Cochrane Database Syst Rev. 12:Cd012008. doi:10.1002/14651858.cd012008
- Martínez-Andrade GO, Cespedes EM, Rifas-Shiman SL, Romero-Quechol G, González-Unzaga MA, Benítez-Trejo MA, … Gillman MW. 2014. Feasibility and impact of Creciendo Sanos, a clinic-based pilot intervention to prevent obesity among preschool children in Mexico City. BMC Pediatr. 14(1): 77-77 71p doi: 10.1186/1471-2431-14-77.
- Mazarello Paes V, Ong KK, Lakshman R. 2015. Factors influencing obesogenic dietary intake in young children (0-6 years): systematic review of qualitative evidence. BMJ Open. 5(9):e007396. doi:10.1136/bmjopen-2014-007396.
- McGowan L, Cooke LJ, Gardner B, Beeken RJ, Croker H, Wardle J. 2013. Healthy feeding habits: efficacy results from a cluster-randomized, controlled exploratory trial of a novel, habit-based intervention with parents. Am J Clin Nutr. 98(3):769–777. doi:10.3945/ajcn.112.052159.
- McPherson AC, Leo J, Church P, Lyons J, Chen L, Swift J. 2014. An environmental scan of weight assessment and management practices in paediatric spina bifida clinics across Canada. J Pediatr Rehabil Med. 7(3):207–217. doi:10.3233/PRM-140290.
- Moher D, Liberati A, Tetzlaff J, Altman DG. 2010. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 8(5):336–341. doi:10.1016/j.ijsu.2010.02.007.
- Niemeier BS, Hektner JM, Enger KB. 2012 Jul. Parent participation in weight-related health interventions for children and adolescents: a systematic review and meta-analysis. Prev Med.55(1):3–13.
- Nyström CD, Sandin S, Henriksson P, Henriksson H, Trolle-Lagerros Y, Larsson C, Maddison R, Ortega FB, Pomeroy J, Ruiz JR, et al. 2017. Mobile-based intervention intended to stop obesity in preschool-aged children: the MINISTOP randomized controlled trial. Am J Clin Nutr, Jun. 105(6):1327–1335. doi:10.3945/ajcn.116.150995.
- Østbye T, Krause KM, Stroo M, Lovelady CA, Evenson KR, Peterson BL, … Zucker NL. 2012. Parent-focused change to prevent obesity in preschoolers: results from the KAN-DO study. Prev Med. 55(3):188–195. doi:10.1016/j.ypmed.2012.06.005.
- Pearce J, Langley-Evans SC. 2013. The types of food introduced during complementary feeding and risk of childhood obesity: a systematic review. Int J Obes. 37(4): 477-485 479p doi: 10.1038/ijo.2013.8.
- Peirson L, Fitzpatrick-Lewis D, Morrison K, Warren R, Usman AM, Raina P. 2015. Treatment of overweight and obesity in children and youth: a systematic review and meta-analysis. CMAJ Open. 3(1):E35–E46.
- Reilly JJ, Armstrong J, Dorosty AR, Emmett PM, Ness A, Rogers I, … Sherriff A. 2005. Early life risk factors for obesity in childhood: cohort study. BMJ. 330(7504):1357. doi:10.1136/bmj.38470.670903.E0.
- Reilly JJ, Hughes AR, Gillespie J, Malden S, Martin A. 2019. Physical activity interventions in early life aimed at reducing later risk of obesity and related non‐communicable diseases: A rapid review of systematic reviews. Obesity Reviews. 20:61–73.
- Skinner AC, Steiner MJ, Henderson FW, Perrin EM. 2010. Multiple markers of inflammation and weight status: cross-sectional analyses throughout childhood. Pediatrics. 125(4):e801–809. doi:10.1542/peds.2009-2182.
- Slusser W, Frankel F, Robison K, Fischer H, Cumberland WG, Neumann C. 2012. Pediatric overweight prevention through a parent training program for 2-4 year old Latino children. Child Obes. 8(1):52–59. doi:10.1089/chi.2011.0060.
- Smith JD, Montaño Z, Dishion TJ, Shaw DS, Wilson MN. 2015. Preventing weight gain and obesity: indirect effects of the Family Check-Up in early childhood. Prevention Science. 16(3):408–419. doi:10.1007/s11121-014-0505-z.
- Summerbell CD, Moore HJ, Vögele C, Kreichauf S, Wildgruber A, Manios Y, … Gibson EL. 2012. Evidence-based recommendations for the development of obesity prevention programs targeted at preschool children. An Off J Int Associ Study Obe. 13(Suppl 1):129–132. doi:10.1111/j.1467-789X.2011.00940.x.
- Taras H, Potts-Datema W. 2005. Obesity and student performance at school. J Sch Health. 75(8):291–295. doi:10.1111/j.1746-1561.2005.00040.x.
- Te Velde S, Van Nassau F, Uijtdewilligen L, Van Stralen M, Cardon G, De Craemer M, … Chinapaw M. 2012. Energy balance‐related behaviours associated with overweight and obesity in preschool children: a systematic review of prospective studies. Obesity Reviews. 13(s1):56–74.
- Tomayko EJ, Prince RJ, Cronin KA, Adams AK. 2016. The Healthy Children, Strong Families intervention promotes improvements in nutrition, activity and body weight in American Indian families with young children. Public Health Nutr. Oct. 19(15):2850–2859. doi:10.1017/S1368980016001014.
- Turner L, Shamseer L, Altman DG, Weeks L, Peters J, Kober T, … Moher D (2012). Consolidated standards of reporting trials (CONSORT) and the completeness of reporting of randomised controlled trials (RCTs) published in medical journals. Cochrane Database Syst Rev, 11, Mr000030. doi:10.1002/14651858.MR000030.pub2
- van Grieken A, Veldhuis L, Renders CM, Borsboom GJ, van der Wouden JC, Hirasing RA, Raat H. 2013. Population-based childhood overweight prevention: outcomes of the ‘Be active, eat right’ study. PLoS One. 8(5):e65376. doi:10.1371/journal.pone.0065376.
- Walton K, Filion AJ, Gross D, Morrongiello B, Darlington G, Randall Simpson J, … Haines J. 2016. Parents and Tots Together: pilot randomized controlled trial of a family-based obesity prevention intervention in Canada. Can J Public Health. 106(8):e555–562. doi:10.17269/cjph.106.5224.
- Wang Y, Lobstein T. 2006. Worldwide trends in childhood overweight and obesity. Int J Pediatr Obes. 1(1):11–25.
- Ward DS, Vaughn A, McWilliams C, Hales D. 2010. Interventions for increasing physical activity at child care. Med Sci Sport Exe. 42(3): 526-534 529p. doi: 10.1249/MSS.0b013e3181cea406.
- Waters E, de Silva-sanigorski A, Hall BJ, Brown T, Campbell KJ, Gao Y, … Summerbell CD. 2011. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 12:CD001871.
- Wojcicki JM, Heyman MB. 2010. Let’s Move–childhood obesity prevention from pregnancy and infancy onward. N Engl J Med. 362(16):1457–1459. doi:10.1056/NEJMp1001857.
- World Health Organization. Obesity and Overweight. Retrieved September 13, 2016, from (WHO) website, http://www.who.int/mediacentre/factsheets/fs311/en/
- Wyse R, Campbell KJ, Brennan L, Wolfenden L. 2014. A cluster randomised controlled trial of a telephone-based intervention targeting the home food environment of preschoolers (The Healthy Habits Trial): the effect on parent fruit and vegetable consumption. Int J Behav Nutr Phys Act. Dec. 24;11:144. doi:10.1186/s12966-014-0144-6.
- Yan J, Liu L, Zhu Y, Huang G, Wang PP. 2014. The association between breastfeeding and childhood obesity: a meta-analysis. BMC Public Health. 14(1):1267. doi:10.1186/1471-2458-14-1267.
- Yavuz HM, van Ijzendoorn MH, Mesman J, van der Veek S. 2015. Interventions aimed at reducing obesity in early childhood: a meta-analysis of programs that involve parents. J Child Psych Psychi. 56(6):677–692. doi:10.1111/jcpp.12330.
- Yilmaz G, Demirli Caylan N, Karacan CD. 2015. An intervention to preschool children for reducing screen time: a randomized controlled trial. Child Care Health Dev. 41(3):443–449. doi:10.1111/cch.12133.
Appendix I
Database search history
Appendix II
Characteristics of excluded studies
Appendix III
Assessment of risk of bias
Barkin et al. (Citation2012)
Berry et al. (Citation2011)
Haines et al. (Citation2013)
Hart et al. (Citation2016)
Martinez-Andrade
Østbye et al. (Citation2012)
Slusser et al. (Citation2012)
Smith et al. (Citation2015)
Tomayko et al. (Citation2016)
van Grieken (2013)
Walton et al. (Citation2016)
Yilmaz et al. (Citation2015)