Abstract
Objective
Up to 22% of school age children have mental health problems. However, less than one quarter at risk of mental health problems access professional services. This study explored help seeking rates for early childhood mental health problems, as measured by the Child Behaviour Checklist, and predictors of parents accessing professional health services.
Method
733 children were recruited during a longitudinal population‐based Australian study. Follow up surveys were completed by the child's primary caregiver at age 1.5, 3, and 6 years.
Results
Prevalence rates ranged from 13% to 23% over the course of the follow up (1.5 to 6 years). Less than one quarter of children with mental health problems accessed general health services for mental health problems (10–21%), and still fewer received specialist mental health care (0–16%). The most consistent predictors of accessing professional help for a child were mothers' who had previously sought professional help for personal stress and recognising that their child's behaviour was problematic.
Conclusion
Few young children with mental health problems accessed professional health services and even less accessed specialist mental health services. Facilitators to parents seeking help were recognition that their young child is difficult to manage and prior experience seeking help for personal stress.
Elizabeth Oh and Megan Mathers are joint first authors.
Mental health is a significant population health issue, affecting up to 22% of school‐age children and adolescents internationally and in Australia (Canino, Bird, Rubio‐Stipec, & Bravo, Citation1995; Giel et al., Citation1981; Sawyer et al., Citation2001). Evidence suggests that as early as preschool age, an estimated 8–21% of young children have significant socio‐emotional difficulties (Briggs‐Gowan, Carter, Moye Skuban, & McCue Horwitz, Citation2001; Koot, Van Den Oord, Verhulst, & Boomsma, Citation1997; Lavigne et al., Citation1996). About half of established preschool problems tend to persist with stability over time (Campbell, Citation1995). Studies have shown that preschool age problems can predict anxiety disorders, depression, and aggression/delinquency into late childhood and adolescence (Bor, McGee, & Fagan, Citation2004; Lonigan & Phillips, Citation2001; Toumbourou, Williams, Letcher, Sanson, & Smart, Citation2011). Early intervention for young children's mental health may have potential to reduce future problems (Webster‐Stratton, Reid, & Hammond, Citation2004).
International studies have shown significant discrepancies between rates of mental health problems and professional service use in children, which range from 6% to 56% (Pihlakoski et al., Citation2004; Staghezza‐Jaramillo, Bird, Gould, & Canino, Citation1995). Similar gaps have been found in Australia, where less than a quarter of school‐age children with mental health issues accessed any professional service (Sawyer et al., Citation2001). Even fewer children received help from mental health professionals such as child and adolescent services, private psychologists, and psychiatrists. Despite an established public healthcare system in Australia, this rate of unmet need in children suggests that certain barriers still exist to parental help seeking for childhood mental health problems. A recent Australian study found that while health practitioners are generally well informed about preschool mental health problems, parents are less likely to be aware of mental health issues in early childhood and the need for early intervention (Alexander, Brijnath, & Mazza, Citation2013).
In the international literature to date, some key factors have been discussed in relation to parents seeking professional help for their child's mental health. Higher levels of child psychopathology have predicted service use within the same year (Sayal, Citation2004; Staghezza‐Jaramillo et al., Citation1995), as well as future service use (Pihlakoski et al., Citation2004). Parent and/or teacher recognition of problematic or difficult child behaviour is reported to be an important factor in professional help seeking (Ford, Hamilton, Meltzer, & Goodman, Citation2008; Pavuluri, Luk, & McGee, Citation1996; Staghezza‐Jaramillo et al., Citation1995). Some studies have also found a positive association between child mental health service use and maternal psychopathology (Ellingson, Briggs‐Gowan, Carter, & Horwitz, Citation2004), as well as parents' past service use for their own mental health issues (Dulcan et al., Citation1990; Zwaanswijk, van der Ende, Verhaak, Bensing, & Verhulst, Citation2005). In addition, parents who had previously sought help for their child's mental health were more likely to report positive intentions to seek help in the future (Starr, Campbell, & Herrick, Citation2002). Socio‐demographic factors such as income, parent education, and ethnicity have been found to have little or no impact on service use in countries where health care is publically funded (Burns et al., Citation1995; Verhulst & van der Ende, Citation1997; Zahner & Daskalakis, Citation1997).
No studies to date have provided a detailed understanding through the early childhood years on children with mental health problems and professional service use. The present Australian study is based on a longitudinal early childhood study spanning from infancy (7 months) through to school entry (age 5–6 years), beginning as a primary prevention initiative (Bayer, Hiscock, Ukoumunne, Price, & Wake, Citation2008; Hiscock et al., Citation2008). The study includes measures of child mental health and service use, parent mental health, parents' past help‐seeking behaviour for their own mental health problems as well as for the child, and socio‐demographic factors. We examine here the proportion of children with mental health problems (measured by the Child Behavior Checklist (CBCL)) from toddlerhood through to school‐entry age. We also examine the rates of service use in young children with mental health problems. Consistent with findings to date with older children, we anticipated that most young children with mental health problems would not have accessed professional assistance. Child, parent, and socio‐demographic predictors of professional service use for children are also explored. It was anticipated that higher levels of child psychopathology would predict both current and future professional service use and that parent recognition of their child's difficulties was likely to be key to help seeking. In addition, the influence of prior help‐seeking behaviour was examined.
Methods
Detailed description of the longitudinal study methods has been published previously (Bayer et al., Citation2008; Hiscock et al., Citation2008) and is reported briefly here.
Setting and participants
Participants were 733 children originally recruited at age 6–7 months from routine universal Maternal and Child Health (MCH) well‐child appointments. MCH nurses in six socio‐economically diverse Victorian local government areas (LGAs) consecutively invited, over a 2‐month period, all mothers of infants attending this visit to take part in the study. Mothers with insufficient English to complete brief questionnaires were excluded. Recruited participants represented 69% of eligible births attending the well‐child visit at 6–7 months in the trial's six LGAs. Questionnaires were completed by mothers at recruitment and followed through to school‐entry age at 6 years old (60% retention of the original sample).
Outcome variable
Service use for the child was measured by two questions at each time point (1.5, 3, and 6 years). At each data collection wave, parents were first asked about their child's service use for mental health problems in the past 12 months, ‘Since your child turned _ years old, have you sought help from anywhere for managing your child's behaviour?’ Parents who responded yes were asked to continue to the second question, ‘Where did you seek help or treatment for your child's behaviour problems?’ Parents could report their help seeking with a checklist that covered a wide range of sources. Parents' responses were classed into four categories: (1) specialist mental health services (psychologist and psychiatrist), (2) more general health services (general practitioner (GP), paediatrician, MCH nurse, and telephone counselling), (3) informal help sources (friends, family, teacher/day care staff, books, and videos/television), or (4) no help sought.
Predictor variables
At infancy
Socio‐demographic factors measured in infancy (7 months) included child gender, parents' education, cultural identity, parent employment status, family income and family living arrangements. Each family was assigned a local neighbourhood index score of relative disadvantage (Socio‐Economic Index for Areas (SEIFA)) by home address postal code (Australian Bureau of Statistics, Commonwealth of Australia Citation2001: population mean (standard deviation, SD) = 1000 (100)). Index scores are a weighted combination of Census variables for the identified area, with higher scores indicative of better socio‐economic status.
At 1.5 years
Child mental health problems were measured at age 1.5 years by the CBCL (preschool) (CBCL: 1.5–5, Achenbach & Rescorla, Citation2000) . The CBCL items employed a 1‐year time frame, and scales were dichotomised at the normal (vs. borderline/clinical) threshold (t score >60; 83–100 percentiles). Achenbach suggests that less conservative (borderline) scores on the total symptom scale can be considered within the deviant range because of the robustness of the scale. The CBCL was ‘designed to provide standardized descriptions of behaviours rather than diagnostic inferences’.
Parent‐related factors were also measured at 1.5 years. Parent recognition of difficult child behaviour was measured by the Australian Temperament Project's (Sanson, Oberklaid, Pedlow, & Prior, Citation1991) global rating scale ‘Compared to other children, I think my child is …’ The scale ranged from ‘much easier than average’ (1) to ‘much more difficult than average’ (5). Previous population research in Australia has demonstrated that the rating ‘more difficult than average’ was an important infancy predictor of adjustment problems (Sanson et al., Citation1991). We likewise dichotomised this scale into ‘difficult’ (4 or 5) versus all others (1–3). Maternal mental health was measured across at the same time points by the 21‐item Depression Anxiety Stress Scales (DASS: Lovibond & Lovibond, Citation1995). Three subscales are derived from each of the summed item scores for depression, anxiety, and stress. Each subscale comprised seven items each rated on a scale ranging from ‘did not apply at all’ (0) to ‘applied to me very much (3). Parents' service use for their own personal stress was measured by two questions at this time point. Parents were first asked about their own service use for mental health problems in the past 12 months, “Since your child turned 6 months old, have you sought help from anywhere for your own stress?” Parents who responded yes were asked to continue to the second question, “Where did you seek help or treatment for your own stress?” Parents could report their help seeking with a checklist that covered a wide range of sources. Parents’ responses were classed into four categories: (1) specialist mental health services (psychologist and psychiatrist), (2) more general health services (GP, paediatrician, MCH nurse, and telephone counselling), (3) informal help sources (friends, family, books, and videos/television), or (4) no help sought.
At 3 years
Child mental health problems were measured by the CBCL (preschool) (CBCL: 1.5–5, Achenbach & Rescorla, Citation2000). CBCL items employed a 1‐year time frame, and scales were dichotomised at the normal (vs. borderline/clinical) threshold (t score >60; 83–100 percentiles). Parent‐related factors measured at 1.5 years were repeated at the 3‐year wave. Parents' service use for their own personal stress at this time point was measured by the question, ‘Since your child turned 2 years old, have you sought help from anywhere for your own stress?’ Parents who responded yes were asked to continue to the second question, ‘Where did you seek help or treatment for your own stress?’
At 6 years
Child mental health problems were measured by the CBCL at 6 years (CBCL: 6–18, Achenbach & Rescorla, Citation2001). CBCL items employed a 1‐year time frame, and scales were dichotomised at the normal (vs. borderline/clinical) threshold (t score >60; 83 to 100 percentiles). Parent‐related factors measured at 1.5 and 3 years were repeated at the 6‐year wave. Parents' service use for their own personal stress in the past 12 months was measured by the question, ‘Since your child turned 5 years old, have you sought help from anywhere for your own stress?’ Parents who responded yes were asked to continue to the second question, ‘Where did you seek help or treatment for your own stress?’ In addition, parent employment status and family income were measured again at this time point.
Statistical analyses
Child mental health problem rates and service use rates were calculated at each time point (1.5, 3, and 6 years) using standard descriptive statistics. To ascertain the predictors of professional service use at each age, logistic regression analyses were performed. To examine the longitudinal impact of child psychopathology and previous help seeking for the child on current service use at 3 years old, the model included the CBCL total symptom score (1.5 years) and the professional service use variable (1.5 years). At the 6‐year‐old time point, the model included the age 1.5 CBCL total symptom score, the age 3 CBCL total symptom score, as well as the professional service use variable at ages 1.5 and 3 years. First, the association between explanatory variables and the service use variable were examined separately using bivariate logistic regression at each time point (1.5, 3, and 6 years). Significant predictors of service use were then included in a multivariate logistic regression model for each age. Analyses were carried out using SPSS 19.0 (SPSS for Windows, 2010, IBM Corp, Armonk, NY, USA).
Results
Sample characteristics
Figure 1 shows a flow chart of participant retention from infant recruitment through to school entry (as mentioned above). Table reports characteristics for the full sample and for the subsets that provided data analysed at the 1.5‐, 3‐, and 6‐year outcomes. Participants retained at school entry were broadly representative of the originally recruited sample. Families across all social strata were represented via SEIFA (mean ranges 1052–1055, SD ranges 76–77) and parents reporting a broad range of education levels and cultural backgrounds.
Figure 1. Flow chart of participants. *All loss to follow up due to failure to return questionnaires.
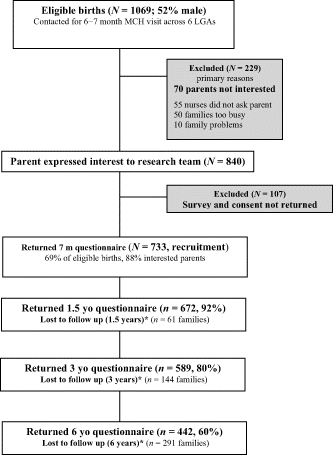
Table 1. Sample characteristics
Child mental health problems and professional health service use
Table presents the proportion of children with elevated CBCL total scores who accessed general health professional or specialist mental health services. Of toddler and preschool children (1.5–3 years), 13–19% had elevated CBCL scores. At school entry (6 years), nearly 20% of children had elevated CBCL scores.
Table 2. Proportion of young children with elevated CBCL total problem scores (≥60) and sources of help accessed
For toddler and preschool children in need, no help was sought from specialist mental health professionals. Of these very young children, 7–8% accessed general health professionals (e.g., MCH nurse, GP, paediatrician, and phone counselling). Help from informal sources was sought by 38–45% of parents with very young children in need (e.g., friends, family, books, and videos/television). Most notably, the majority of parents with very young children in need did seek any help at all (47–56%).
By 6 years of age, 16% of children with elevated CBCL scores received assistance from specialist mental health services. At this age, less than a quarter of children in need accessed general health services. In addition, more than one third of parents sought help from informal sources (i.e., family, friends, books, video/television, and teachers/day care staff). Again and importantly, more than half of parents whose 6 year old had an elevated CBCL score did not access any sort of help.
Predictors of professional health service use for children in need
Because of low numbers of young children receiving specialist mental health care (as seen in Table ), general and specialist mental health services were collapsed into a combined health professional service use category for the following analyses. Table presents the results of the bivariate logistic regression models predicting professional health service use at 1.5, 3, and 6 years of age.
Table 3. Variables significantly associated with professional service use in bivariate logistic regression
Results from the bivariate analyses indicated that accessing help from professional services at 1.5 years was more likely if the child had higher total symptom scores on the CBCL, if their mother had previously accessed services for their personal stress, if their mother recognised their child's behaviour as more difficult than average, and if their mother had higher scores on the DASS. At 3 years, only child symptoms scores at 3 years of age (compared with elevated symptom scores at 1.5 years) predicted professional service use at this time point. Mothers who had accessed professional help for their personal stress, mothers who recognised their child's difficult behaviour, and mothers who had elevated scores on the DASS were more likely to access professional help for their child when they were 3 years old. In addition, children who had received treatment for mental health‐related difficulties at 1.5 years old were more likely to receive professional help when they were 3 years old. At the 6‐year time point, elevated CBCL symptom scores at 3 years and 6 years of age predicted professional service use for the child. Maternal service use for personal stress, recognition of difficult child behaviour, and elevated maternal scores on the stress subscale of the DASS were also associated with professional service use at this age. Again, prior help seeking for child mental health problems at 1.5 years and 3 years of age predicted professional service use when the child was 6 years old.
Significant bivariate predictors were entered into a multivariate model at each time point (Table ). Across all time points, parent factors such as maternal help‐seeking behaviour for personal stress and recognition that their child's behaviour was more difficult than average were the strongest predictors of help seeking for children's mental health problems. This likelihood of seeking professional help for their child increased with the child's age. Furthermore, at the 6‐year time point, elevated child symptom scores reported within the year were also predictive of current professional service use for the child. The multivariate regression models explained substantial variance in professional service use for young children (11–50%).
Table 4. Variables significantly associated with professional service use in multivariate logistic regression
Discussion
Central findings of this study are threefold. First, in this population‐based sample of young children (1.5–6 years), the rates of mental health problems on a behavioural screening measure (CBCL: 1.5–5, Achenbach & Rescorla, Citation2000; CBCL: 6–18, Achenbach & Rescorla, Citation2001) were consistent with known prevalence rates at older ages (Sawyer et al., Citation2001). Second, the majority of young children with elevated CBCL scores did not receive any help from professional services. There appears to be underutilisation of professional services relative to community need with regard to early childhood mental health. Third, the strongest predictors of parents accessing professional health care for their young children were (1) recognising their child's behaviour as more difficult than average and (2) having previously accessed professional services for their own personal stress.
The rates of need as measured by the CBCL in this Australian study at the 6‐year wave (20%) were comparable with internationally reported prevalence rates of ∼20% (Canino et al., Citation1995; Giel et al., Citation1981). Likewise, the present study found prevalence rates in toddler and preschool‐age children (13–19%) were consistent with prior international reports of around ∼15% (Briggs‐Gowan et al., Citation2001; Koot et al., Citation1997; Lavigne et al., Citation1996). Current findings indicating that relatively few children in need accessed professional health services for their mental health problems are also consistent with previous literature (Ford, Goodman, & Meltzer, Citation2003; Pihlakoski et al., Citation2004; Staghezza‐Jaramillo et al., Citation1995). The findings focusing specifically on the early childhood period significantly extend knowledge in the field. Importantly, less than one sixth of preschool children with elevated CBCL scores received any help from a health professional—and none from a mental health specialist. In Australia, child and adolescent health services can involve a variety of professionals including maternal child health nurses, general practitioners, and paediatricians. These professionals along with education providers often act as the gatekeepers for referrals to mental health services for school‐age children. However, the existing early childhood mental health services are currently under resourced, tending to only accept referrals with high levels of risk. In addition, despite the existence of several early intervention programmes targeting younger children with mental health difficulties (Bayer et al., Citation2009), parents often struggle to access these services.
Prior research found that predictors of older children accessing professional help were teacher and parent recognition that the child had a problem, as well as parental well‐being (Pihlakoski et al., Citation2004; Staghezza‐Jaramillo et al., Citation1995). Likewise, the current findings with young children highlight parents' perceptions as key, in the sense that mothers identify their child more ‘difficult’ than average. Also importantly in the present findings and extending prior knowledge, mothers who had previously been able to access services for their own personal stress were then more likely to do this for their child. This finding suggests that a recent history of service use regardless of the focal patient may in fact facilitate help seeking for a child. Given that many barriers reported by parents who did not seek help revolved around not knowing who or where to go and uncertainty as to the helpfulness of treatment (Ford et al., Citation2003), familiarity with referral pathways and positive past experiences with services could assist with this help‐seeking process. Another possibility for this present finding could be that health professionals treating a parent may be more likely to ask about their family functioning and thus pick up on concerns regarding the child. While prior literature has pointed to the influence of symptom severity in service use for children's mental health problems (Sayal, Citation2004), this factor was only predictive of service use at 6 years of age. In addition, the strength of association between child psychopathology and professional service use at 6 years was comparably less than parent recognition and prior service use for personal stress.
Strengths of this study were its socio‐demographically broad population‐based sample, repeatedly assessed at time points from infancy to school entry, measuring child, family, and service use aspects, and applying psychometrically sound measures. The present study also had a few limitations. First, the sample was not representative of all Australian families with young children, as only 69% of eligible births were recruited. Because of the longitudinal nature of the study, around 68% of participants were retained at age 6 years. Although a recruitment rate of 69% from birth records is a high rate for population surveys (Bayer, Hiscock, Morton‐Allen, Ukoumunne, & Wake, Citation2007), 30% of babies of unknown risk status were not included. Families recruited into the study were also slightly more likely to be retained at age 6 years if English was the main language spoken in the home, parents had completed tertiary education, and household income was above $AUD60,000 per annum. The low service use rates highlight that even for health‐oriented parents from a higher socio‐economic background, accessing professional help for young children's mental health problems is uncommon. A second limitation is that service use research regarding child mental health tends to be conducted in countries (including Australia) where health care is publicly funded. Socio‐economic factors may appear to play a less important role in such studies than in countries with less publicly funded health care. However, we found that maternal employment was a positive facilitator of help seeking. Nevertheless, even in this Australian study there were some indicators that maternal employment may facilitate service use when in need. The third limitation was that so few parents were found to access specialist mental health care for young children in need that analysing predictors of general versus specialist health care was precluded (although initially planned for this study).
With regard to clinical and practical implications, findings of this research indicate a need to improve parents' awareness of significant problematic behaviour in young children as well as the best pathways to access specialised care for young children in need. Effective early intervention programmes for young children's mental health exist and could be better integrated into public health and education service systems (Bayer et al., Citation2009). Prior familiarity with health service pathways appeared relevant to families accessing services for young children in need. It seemed that when mothers had been able to access professional help for their own personal stress, they were more likely to find suitable referrals when their children were in need. Early childhood staff (at child care, preschool, and medical practices) could also facilitate referrals by helping to inform parents when a young child's behaviour is more problematic than same‐age peers.
Conclusions
During the early childhood years, up to one in five young children faces mental health related challenges. Few young children receive any professional health care for these problems. Of children in need whose parents access help, a small proportion consult with general health professionals, and still fewer receive any specialist mental health care. A significant gap exists between young children's mental health‐related needs and services received. Key predictors of accessing help when in need appear to include parents having previously accessed professional help for their own stress and parents viewing their child as more ‘difficult’ than their peers. Future research can explore in detail parents' beliefs and attitudes that contribute to decision making about seeking help for young children's mental health.
Acknowledgements
We would like to thank families of the Victorian Cities of Glen Eira, Greater Geelong, Kingston, Maribyrnong, Nillumbik, and Stonnington who took part in this research.
This follow‐up study was supported by an Australian Postgraduate Award, an Equity Trustees Grant, an Australian Rotary Health Postdoctoral Fellowship, National Health and Medical Research Council (NHMRC) Public Health Capacity Building Grant Postdoctoral Fellowships, and an NHMRC Career Development Award.
Additional information
Funding
Notes
Elizabeth Oh and Megan Mathers are joint first authors.
References
- Achenbach, T. M., & Rescorla, L. A. (2000). Manual for the ASEBA Preschool Forms & Profiles. Burlington VT: ASEBA, University of Vermont, Research Center for Children, Youth, and Families.
- Achenbach, T. M., & Rescorla, L. A. (2001). Manual for the ASEBA School Age Forms & Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, and Families.
- Alexander, K., Brijnath, B., & Mazza, D. (2013). ‘Can they really identify mental health problems at the age of three?’ Parent and practitioner views about screening young children's social and emotional development. The Australian and New Zealand Journal of Psychiatry, 47(6), 538–545. doi:https://doi.org/10.1177/0004867413476756
- Australian Bureau of Statistics, Commonwealth of Australia (2001). Socioeconomic Indexes for Areas. Canberra, ACT: ABS.
- Bayer, J. K., Hiscock, H., Morton‐allen, E., Ukoumunne, O. C., & Wake, M. (2007). Prevention of mental health problems: Rationale for a universal approach. Archives of Disease in Childhood, 92(1), 34–38. doi:https://doi.org/10.1136/adc.2006.100776
- Bayer, J. K., Hiscock, H., Ukoumunne, O. C., Price, A., & Wake, M. (2008). Early childhood aetiology of mental health problems: A longitudinal population‐based study. Journal of Child Psychology and Psychiatry, 49(11), 1166–1174. doi:https://doi.org/10.1111/j.1469‐7610.2008.01943.x
- Bayer, J. K., Hiscock, H., Scalzo, K., Mathers, M., Mcdonald, M., Morris, A., … Wake, M. (2009). Systematic review of preventive interventions for children's mental health: What would work in Australian contexts? The Australian and New Zealand Journal of Psychiatry, 43(8), 695–710.
- Bor, W., Mcgee, T. R., & Fagan, A. A. (2004). Early risk factors for adolescent antisocial behaviour: An Australian longitudinal study. The Australian and New Zealand Journal of Psychiatry, 38(5), 365–372. doi:https://doi.org/10.1111/j.1440‐1614.2004.01365.x
- Briggs‐gowan, M. J., Carter, A. S., Moye skuban, E., & Mccue horwitz, S. (2001). Prevalence of social‐emotional and behavioral problems in a community sample of 1‐ and 2‐year‐old children. Journal of the American Academy of Child and Adolescent Psychiatry, 40(7), 811–819. doi:https://doi.org/10.1097/00004583‐200107000‐00016
- Burns, B., Costello, E., Angold, A., Tweed, D., Stangl, D., Farmer, E. M., & Erkanli, A. (1995). Children's mental health service use across service sectors. Health Affairs, 14, 147–159.
- Campbell, S. B. (1995). Behavior problems in preschool children: A review of recent research. Journal of Child Psychology and Psychiatry, 36(1), 113–149.
- Canino, G., Bird, H. R., Rubio‐stipec, M., & Bravo, M. (1995). Child psychiatric epidemiology: What we have learned and what we need to learn. International Journal of Methods in Psychiatric Research, 5(2), 79–92.
- Dulcan, M. K., Costello, E. J., Costello, A. J., Edelbrock, C., Brent, D., & Janiszewski, S. (1990). The pediatrician as gatekeeper to mental‐health‐care for children—Do parents concerns open the gate. Journal of the American Academy of Child and Adolescent Psychiatry, 29(3), 453–458. doi:https://doi.org/10.1097/00004583‐199005000‐00018
- Ellingson, K. D., Briggs‐gowan, M. J., Carter, A. S., & Horwitz, S. M. (2004). Parent identification of early emerging child behavior problems: Predictors of sharing parental concern with health providers. Archives of Pediatrics and Adolescent Medicine, 158(8), 766–772. doi:https://doi.org/10.1001/archpedi.158.8.766
- Ford, T., Goodman, R., & Meltzer, H. (2003). Service use over 18 months among a nationally representative sample of British children with psychiatric disorder. Clinical Child Psychology and Psychiatry, 8(1), 37–51. doi:https://doi.org/10.1177/1359104503008001006
- Ford, T., Hamilton, H., Meltzer, H., & Goodman, R. (2008). Predictors of service use for mental health problems among British schoolchildren. Child and Adolescent Mental Health, 13(1), 32–40. doi:https://doi.org/10.1111/j.1475‐3588.2007.00449.x
- Giel, R., de Arango, M. V., Climent, C. E., Harding, T. W., Ibrahim, H. H., Ladrido‐ignacio, L., … Younis, Y. O. (1981). The classification of psychiatric disorder: A reliability study in the WHO Collaborative Study on Strategies for Extending Mental Health Care. Acta Psychiatrica Scandinavica, 63(1), 61–74. doi:https://doi.org/10.1111/j.1600‐0447.1981.tb00651.x
- Hiscock, H., Bayer, J. K., Price, A., Ukoumunne, O. C., Rogers, S., & Wake, M. (2008). Universal parenting programme to prevent early childhood behavioural problems: Cluster randomised trial. British Medical Journal, 336(7639), 318–321. doi:https://doi.org/10.1136/bmj.39451.609676.AE
- Koot, H. M., Van den oord, E. J. C. G., Verhulst, F. C., & Boomsma, D. I. (1997). Behavioral and emotional problems in young preschoolers: Cross‐cultural testing of the validity of the Child Behavior Checklist/2–3. Journal of Abnormal Child Psychology, 25(3), 183–196. doi:https://doi.org/10.1023/a:1025791814893
- Lavigne, J. V., Gibbons, R. D., Christoffel, K., Arend, R., Rosenbaum, D., Binns, H. J., … Isaacs, C. (1996). Prevalence rates and correlates of psychiatric disorders among preschool children. Journal of the American Academy of Child and Adolescent Psychiatry, 35(2), 204–214. doi:https://doi.org/10.1097/00004583‐199602000‐00014
- Lonigan, C. J., & Phillips, B. M. (2001). Temperamental influences on the development of anxiety disorders. In M. W. Vasey & M. R. Dadds (Eds.), The developmental psychopathology of anxiety (pp. 60–91). New York: Oxford University Press.
- Lovibond, P. F., & Lovibond, S. H. (1995). The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the beck depression and anxiety inventories. Behaviour Research and Therapy, 33(3), 335–343.
- Pavuluri, M. N., Luk, S., & Mcgee, R. (1996). Help‐seeking for behavior problems by parents of preschool children: A community study. Journal of the American Academy of Child and Adolescent Psychiatry, 35(2), 215–222.
- Pihlakoski, L., Aromaa, M., Sourander, A., Rautava, P., Helenius, H., & Sillanpaa, M. (2004). Use of and need for professional help for emotional and behavioral problems among preadolescents: A prospective cohort study of 3‐ to 12‐year‐old children. Journal of the American Academy of Child and Adolescent Psychiatry, 43(8), 974–983. doi:https://doi.org/10.1097/01.chi.0000127574.41662.fa
- Sanson, A., Oberklaid, F., Pedlow, R., & Prior, M. (1991). Risk indicators: Assessment of infancy predictors of pre‐school behavioural maladjustment. Journal of Child Psychology and Psychiatry, 32(4), 609–626.
- Sawyer, M. G., Arney, F. M., Baghurst, P. A., Clark, J. J., Graetz, B. W., Kosky, R. J., … Zubrick, S. R. (2001). The mental health of young people in Australia: Key findings from the child and adolescent component of the national survey of mental health and well‐being. The Australian and New Zealand Journal of Psychiatry, 35(6), 806–814.
- Sayal, K. (2004). The role of parental burden in child mental health service use: Longitudinal study. Journal of the American Academy of Child and Adolescent Psychiatry, 43(11), 1328–1333. doi:https://doi.org/10.1097/01.chi.0000138353.83357.fa
- Staghezza‐jaramillo, B., Bird, H. R., Gould, M. S., & Canino, G. (1995). Mental health service utilization among Puerto Rican children ages 4 through 16. Journal of Child and Family Studies, 4(4), 399–418. doi:https://doi.org/10.1007/bf02237271
- Starr, S., Campbell, L. R., & Herrick, C. A. (2002). Factors affecting use of the mental health system by rural children. Issues in Mental Health Nursing, 23(3), 291–304.
- Toumbourou, J. W., Williams, I., Letcher, P., Sanson, A., & Smart, D. (2011). Developmental trajectories of internalising behaviour in the prediction of adolescent depressive symptoms. Australian Journal of Psychology, 63(4), 214–223. doi:https://doi.org/10.1111/j.1742‐9536.2011.00023.x
- Verhulst, F. C., & van der Ende, J. (1997). Factors associated with child mental health service use in the community. Journal of the American Academy of Child & Adolescent Psychiatry, 36(7), 901–909. doi:https://doi.org/10.1097/00004583‐199707000‐00011
- Webster‐stratton, C., Reid, M. J., & Hammond, M. (2004). Treating children with early‐onset conduct problems: Intervention outcomes for parent, child, and teacher training. Journal of Clinical Child and Adolescent Psychology, 33(1), 105–124. doi:https://doi.org/10.1207/S15374424JCCP3301_11
- Zahner, G. E., & Daskalakis, C. (1997). Factors associated with mental health, general health, and school‐based service use for child psychopathology. American Journal of Public Health, 87(9), 1440–1448. doi:https://doi.org/10.2105/ajph.87.9.1440
- Zwaanswijk, M., van der Ende, J., Verhaak, P. F., Bensing, J. M., & Verhulst, F. C. (2005). Help‐seeking for child psychopathology: Pathways to informal and professional services in the Netherlands. Journal of the American Academy of Child and Adolescent Psychiatry, 44(12), 1292–1300. doi:https://doi.org/10.1097/01.chi.0000181038.98712.c6

