?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Objective
Binge eating and alcohol consumption have been associated with attempts to reduce negative affect such as anger. Anger rumination has been associated with maintaining anger. The aim of the current study was to explore the association between anger rumination and binge eating and at‐risk alcohol use.
Method
Participants were 563 university students aged between 18 and 66-years who completed an online survey containing the Anger Rumination Scale (ARS), Eating Disorder Diagnosis Scale (EDDS), Alcohol Use Disorders Identification Test—Consumption (AUDIT‐C) and Depression, Anxiety, & Stress Scale (DASS‐21).
Results
The results showed that individuals who endorsed elevated levels of binge eating behaviour had increased levels of anger rumination, specifically angry afterthoughts and angry memories, compared to healthy controls. In contrast, individuals who engaged in at‐risk alcohol use without binge eating did not report significantly increased levels of anger rumination.
Conclusions
This study highlights anger rumination as a potential factor in maintaining binge eating behaviour and suggests that screening for and addressing anger rumination may be an important component of psychological treatment.
What is already known about this topic
Rumination is implicated in a range of psychopathologies
Links have been established between anger and impulsive behaviours, such as binge eating and excessive alcohol uses
However, less is known about links between anger rumination and binge eating and alcohol use
What this topic adds
Anger rumination was elevated in individuals who binge eat compared with healthy controls
Anger rumination in individuals with at‐risk alcohol use, without binge eating, was no different to healthy controls
Anger rumination may be a maintaining factor in binge eating behaviours
Rumination is a cognitive pattern characterised by repetitive thinking about problems without the generation of appropriate solutions. It has been considered a key factor in maintaining and increasing negative affect as part of the response styles theory of depression (Nolen‐Hoeksema, Citation2004), but also has been implicated in a range of psychopathologies (Nolen‐Hoeksema & Watkins, Citation2011; Nolen‐Hoeksema, Wisco, & Lyubomirsky, Citation2008). Anger rumination—a tendency to become occupied with an angry mood, thoughts about past anger‐inducing experiences, and the causes and consequences of anger—has been identified as one factor that may maintain anger (Sukhodolsky, Golub, & Cromwell, Citation2001), which in turn has been associated with poor health outcomes (Baum & Pozluszny, Citation1999; Jorgensen & Kolodziej, Citation2007; McKeen, Chipperfield, & Campwell, Citation2004; Williams et al., Citation2000). Individuals with a cognitive response style characterised by anger rumination are likely to experience more frequent, longer lasting, and intense episodes of anger (Ray, Wilhelm, & Gross, Citation2008; Rusting & Nolen‐Hoeksema, Citation1998; Sukhodolsky et al., Citation2001). In a multiple systems model, dispositional anger rumination has also been theorised to deplete cognitive resources and interfere with self‐control (Denson, Citation2012). Experimental research supports anger rumination as a mediating factor in the link between provocation and impulsive behaviours, such as aggression (Denson, Pedersen, Friese, Hahm, & Roberts, Citation2011). Consequently, anger rumination may be associated with other behaviours influenced by reduced self‐control capacity, such as impulsive drinking and eating (Denson et al., Citation2011).
The association between anger and alcohol consumption is well documented in men, but is less consistent in women (Brennan, Walfish, & Aubuchon, Citation1986; Harder, Ayer, Rose, Naylor, & Helzer, Citation2014; Leibsohn, Oetting, & Deffenbacher, Citation1994). Typically, more men than women engage in problematic alcohol use (Brennan et al., Citation1986; Hallet et al., Citation2012) and longitudinal research using a daily reporting method has found that increased anger predicted higher next day alcohol use in men only (Harder et al., Citation2014). However, experimental research has found that, when provoked to feel anger, women consumed more alcohol (Morrison, Noel, & Ogle, Citation2012). Furthermore, anger rumination has been associated with greater quantities of weekly drinking with no gender moderation effect (Ciesla, Dickson, Anderson, & Neal, Citation2011). The role of anger‐related constructs in risky alcohol consumption is therefore of interest in both genders.
At‐risk alcohol use has been shown to be commonly comorbid with eating disorders, especially those involving binge eating (Bulik et al., Citation2004; Ferriter & Ray, Citation2011; Gadalla & Piran, Citation2007). Binge eating has also been associated with anger (Engel et al., Citation2007; Fassino, Daga, Piero, Leombruni, & Rovera, Citation2001; Maxwell, Sukhodolsky, Chow, & Wong, Citation2005; Zeeck, Stelzer, Linster, Joos, & Hartman, Citation2011) and occurs generally in response to negative mood states such as depression and anxiety (Arnow, Kenardy, & Agras, Citation1995; Connolly, Rieger, & Caterson, Citation2007; Stice et al., Citation2001). However, the contexts in which individuals binge drink and binge eat differ. University students, especially, are likely to binge drink in social contexts (Clapp et al., Citation2003) and women consider binge drinking more socially acceptable than binge eating in public (Birch, Stewart, & Brown, Citation2007). In considering gender differences, binge eating is known to be associated with anger suppression in women (Milligan & Waller, Citation2000; Waller et al., Citation2003), and with state anger in men (Meyer et al., Citation2005). Consequently, women may binge eat to avoid expressing anger and men may binge eat to reduce anger. Given that anger rumination may occur before, during, or after episodes of anger (Sukhodolsky et al., Citation2001), there would not necessarily be reason to suspect gender differences in the relationship between anger rumination and binge eating.
To date, with the exception of the Ciesla et al. (Citation2011) study into anger rumination and alcohol use, no further published research has evaluated the association between anger rumination and binge drinking; additionally, no studies have assessed the association between anger rumination and binge eating. Given the relationship of binge eating and binge drinking with anger, along with the relationship between anger and anger rumination, the aim of this study was to examine the extent to which anger rumination was related to binge eating and drinking. The literature suggests that both binge eating and at‐risk drinking are associated with anger. Therefore, we hypothesised that individuals who engaged in binge eating and at‐risk alcohol use would demonstrate higher levels of anger rumination compared with individuals who engaged in healthier eating and alcohol use behaviours.
METHOD
Participants
Participants (N = 718) were recruited through an online questionnaire, distributed to students across all programs at a regional Australian university. Those who did not indicate consent, were under 18-years of age, or did not endorse having read the information sheet were excluded (n = 44) as were those who did not complete the survey fully (n = 100). Participants with a diagnosis of sub or full threshold anorexia nervosa were also excluded prior to group allocation (n = 11). The remaining participants formed the final sample (N = 563; 80% female), with ages ranging from 18 to 66-years (M = 26.55, standard deviation (SD) = 10.08). Demographic details are provided in Table .
Table 1. Demographic information according to group
Materials
Demographic questionnaire
The demographic questionnaire consisted of six items related to age, gender, occupation, student status, relationship status, and ethnicity.
Anger Rumination Scale (ARS)
The ARS is a 19‐item self‐report scale measuring the tendency to focus on angry moods, recall past anger experiences, and think about causes and consequences of anger episodes (Sukhodolsky et al., Citation2001). Individuals respond to items using a 4‐point scale ranging from 1 (almost never) to 4 (almost always). A total anger rumination score (range 19–76) and four subscale scores are obtained, with higher scores suggesting greater propensity towards anger rumination. The four subscales include Angry Afterthoughts (six items; repeated thoughts about a recent anger‐inducing episode, e.g., ‘Whenever I experience anger, I keep thinking about it for a while’); Thoughts of Revenge (four items; thoughts related to retribution, e.g., ‘I have difficulty forgiving people who have hurt me’); Angry Memories (five items; thoughts about past anger episodes, e.g., ‘I ruminate about my past anger experiences’); and Understanding of Causes (four items; thoughts about, and attempts to understand the causes of an anger event, e.g., ‘I analyze events that make me angry’).
Sukhodolsky et al. (Citation2001) reported high internal reliability (α = .93) and good test–retest reliability (r = .77) over a 1‐month period, for the total score. The ARS correlated moderately with measures of anger experience, anger expression, and negative affect (Sukhodolsky et al., Citation2001), has been validated cross‐culturally, and demonstrates adequate psychometric properties (Besharat & Shahidi, Citation2010; Maxwell et al., Citation2005; Ramos‐Cejudo, Salguero, Kannis‐Dymand, Garcia‐Sancho, & Love, Citation2017).
Alcohol Use Disorder Identification Test—Consumption (AUDIT‐C)
The AUDIT‐C consists of the first three items of the AUDIT, a 10‐item questionnaire developed by the World Health Organization to identify hazardous or harmful drinking (Saunders, Aasland, Babor, De La Fuente, & Grant, Citation1993). The AUDIT‐C assesses frequency of alcohol consumption, typical amounts consumed, and frequency of heavy episodic drinking (Bush, Kivlahan, McDonell, Fihn, & Bradley, Citation1998). Those who responded ‘never’ to the item, ‘How often do you have a drink containing alcohol?’, were not required to answer subsequent items, and obtained a score of 0 for those items. Otherwise, all items were scored from 0 (never) to 4 (daily, or almost daily), with a maximum possible score of 12 (Babor, Higgins‐Biddle, Saunders, & Monteiro, Citation2001).
The AUDIT‐C performs better than the AUDIT in the detection of at‐risk drinking in female university students and equally well in male students (DeMartini & Carey, Citation2012). Scores of 5 and above for female students, and 7 and above for male students have been recommended to optimise sensitivity and specificity in the detection of at‐risk alcohol use (DeMartini & Carey, Citation2012).
Depression, Anxiety & Stress Self‐report‐21 (DASS‐21)
Adapted from the full 42‐item version, the DASS‐21 is a valid and reliable instrument for identifying negative affect (Lovibond & Lovibond, Citation1995). It has three scales each with seven items: depression (DASSd); anxiety (DASSa); and stress (DASSs). Representative subscale items are ‘I couldn’t seem to experience any positive feelings at all’ (DASSd), ‘I felt scared without good reason (DASSa) and ‘I found it hard to wind down’ (DASSs). Items are rated on a 4‐point scale, ranging from 0 (did not apply to me at all) to 3 (applied to me very much, or most of the time).
The Eating Disorder Diagnostic Scale (EDDS)
The EDDS is a 22‐item scale for diagnosing anorexia nervosa, bulimia nervosa and binge eating disorder at both sub and full threshold levels, using DSM‐IV criteria. Items require either ‘Yes’ or ‘No’ responses, Likert‐type scale ratings, or short written responses. Reliable and valid psychometric properties have been demonstrated, including good test–retest reliability (.89) and internal consistency (α = .91; Stice, Telch, & Rizvi, Citation2000; Stice, Fisher, & Martinez, Citation2004).
Procedure
To commence the survey, participants responded to three eligibility questions that included: an age requirement of 18-years or older, agreement to consent by completion of the survey, and acknowledgement that the research information sheet had been read and understood. Eligible participants were then linked to a questionnaire package, containing the demographics questions, the ARS, AUDIT‐C, DASS‐21, and EDDS. Completion time was 15 to 20-min. The Human Research Ethics Committee of the home institution approved the study.
Statistical analysis
All analyses were performed using SPSS (version 20; SPSS Inc., Chicago, USA).
First, participants were allocated to one of four groups based on their AUDIT‐C and EDDS scores. The Healthy Control (HC) group (n = 285) comprised participants who did not meet criteria for at‐risk alcohol use (males ≤ 6 and females ≤ 4 on the AUDIT‐C) or obtained a sub or full threshold eating disorder diagnosis (0 on the EDDS). The At‐Risk Alcohol Use (ALC) group (n = 156) met criteria for at‐risk alcohol use (males ≥ 7 and females ≥ 5 on the AUDIT‐C) but did not obtain a diagnosis of an eating disorder. The Binge Eating (BE) group (n = 63) did not meet criteria for at‐risk alcohol use but did meet criteria for full or sub threshold Bulimia Nervosa or Binge Eating Disorder. The Binge Eating and At‐Risk Alcohol Use (BEALC) group (n = 59) met criteria for at‐risk alcohol use and had a diagnosis of full or sub‐threshold Bulimia Nervosa or Binge Eating Disorder.
Using G Power analysis (Faul, Erdfelder, Lang, & Buchner, Citation2007) for a multivariate analysis of variance (MANOVA; global effects) to test four groups on four outcome variables with a medium effect size and power of 0.80 determined that a minimum sample of 100 participants (i.e., four groups of 25 participants). Furthermore, G Power analysis for a fixed effects, omnibus ANOVA (with four groups and a medium effect size and power of 0.80) established that a minimum sample of 180 participants (i.e., 45 per group). Both estimations of sample size were less than the group sizes (n = 63–285; total sample n = 563) achieved in the current study.
A one‐way multivariate analysis of covariance (MANCOVA) was used to assess differences in the anger rumination subscales (Angry Afterthoughts, Thoughts of Revenge, Angry Memories, and Understanding of Causes) between the groups (HC, ALC, BE, and BEALC). The data were screened for multivariate outliers, resulting in removal of 15 outliers that exceeded a z‐score of 3.29 on relevant measures (Tabachnick & Fidell, Citation2001). Gender was entered as a covariate based on earlier research demonstrating that men typically report higher levels of anger rumination on the Angry Revenge subscale (Maxwell et al., Citation2005; Sukhodolsky et al., Citation2001). Negative affect (depression, stress, and anxiety) and age were also entered as covariates due to their potential confounding effects in the relationships between anger rumination and binge eating and alcohol use (Connolly et al., Citation2007). These factors also correlated with the ARS subscales (see Table ).
Table 2. Correlations between ARS, age, and DASS
RESULTS
Group characteristics
The four groups (HC, ALC, BE, and BEALC) differed significantly on gender chi‐square (3, n = 563) =14.44, p < .05, phi = 1.6, and age F(3, 559) = 9.865, p < .05. Post hoc comparisons revealed that the HC group (M = 27.9, SD = 10.77) was significantly older than the ALC group (M = 24.1, SD = 8.55) and the BEALC group (M = 22.9, SD = 6.87). The BE (M = 29.9, SD = 10.86) group was also significantly older than the ALC and BEALC groups. There were no significant differences in age between the HC and BE groups.
Differences in anger rumination according to binge eating and alcohol use status
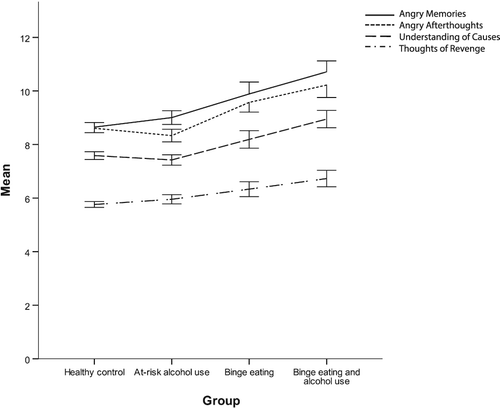
The MANCOVA showed a main effect for group F(12, 521) = 1.83, Pillai’s Trace = .04, p < .05, (see Fig. 1). Follow‐up analyses showed significant group differences for the Angry Afterthoughts subscale, F(3, 533) = 4.66, p < .05, . The HC group (M = 8.48, SD = 2.64) scored significantly lower for angry afterthoughts than the BE group (M = 9.56, SD = 2.80), t(344) = −2.76, p < .05, and BEALC group (M = 10.19, SD = 3.61), t(340) = −4.16, p < .05. The ALC group (M = 8.19, SD = 2.76) similarly scored significantly lower for angry afterthoughts than the BE group, t(216) = −3.12, p < .05, and BEALC group, t(216) = −4.23, p < .05.
There were also significant group differences for the Angry Memories subscale, F(3, 533) = 26.03, p < .05, . The HC group (M = 8.53, SD = 2.78) scored significantly lower for angry memories than the BE group (M = 9.93, SD = 3.57), t(345) = −3.11, p < .05, and BEALC group (M = 10.70, SD = 3.11), t(341) = −5.11, p < .05. The ALC group (M = 8.84, SD = 3.06) similarly scored significantly lower for angry memories than the BE group, t(216) = −1.98, p < .05, and BEALC group, t(212) = −3.744, p < .05. There were no main effects of group across Thoughts of Revenge or Understanding of Causes.
DISCUSSION
This study examined the relationship between anger rumination, binge eating, and at‐risk alcohol use. The hypothesis that anger rumination would be associated with binge eating and at‐risk alcohol use was partially supported. Particular elements of anger rumination were more prevalent in individuals with sub or full threshold diagnoses of bulimia nervosa or binge eating disorder. Specifically, individuals with binge eating endorsed significantly higher levels of anger rumination related to angry afterthoughts and angry memories than healthy controls or individuals who reported at‐risk alcohol use without binge eating. Past research has suggested that associations between anger and binge eating are questionable given the possible confounding effects of depression and anxiety (Connolly et al., Citation2007). However, the present study found that anger rumination was present in individuals with binge eating even when these factors were controlled.
Our findings for binge eating align with previous findings suggesting that binge eating may act as a coping strategy to escape from aversive self‐focused attention, such as rumination (Naumann, Tuschen‐Caffier, Voderholzer, Caffier, & Svaldi, Citation2015; Nolen‐Hoeksema & Watkins, Citation2011). Notably, only angry afterthoughts and angry memories were elevated in the participants with binge eating. The remaining subscales, thoughts of revenge and understanding of causes, have been considered more oriented towards resolving the anger problem, either through meaningful understanding of the situation or gaining retribution (Sukhodolsky et al., Citation2001). This may suggest that binge eating is associated with the tendency to replay thoughts of past anger‐inducing experiences without consideration of ways to resolve the anger emotion. The present study did not determine the nature of the relationship between anger rumination and binge eating; that is, the proximity of anger rumination to these behaviours in terms of being an antecedent, consequence, or moderator was not established. However, the findings can be considered within recent transdiagnostic conceptualisations of rumination. For example, Nolen‐Hoeksema and Watkins (Citation2011) reported that rumination predicts various psychopathologies, that is, rumination being a risk factor for multifinality and divergent trajectories, including excessive food intake. Furthermore, Denson’s (Citation2012) multiple systems model of anger rumination posits that, at an executive control level angry rumination contributes to poor executive functioning and reduced self‐control. In considering the present findings, it may be that a disposition towards anger rumination reduces inhibitory control, contributing to vulnerability to excessive food consumption.
Anger rumination was not significantly associated with at‐risk alcohol use, but was present for those reporting both binge eating and at‐risk alcohol use. These findings contrast with past research that found anger rumination was associated with greater weekly alcohol consumption (Ciesla et al., Citation2011) as well as suggestions that alcohol use could be an avoidance coping strategy for rumination (Hilt, Armstrong, & Essex, Citation2015; Nolen‐Hoeksema & Watkins, Citation2011). Potentially, individuals who engage in risky alcohol use differ from individuals who also binge eat. Within our university sample, it is possible that risky drinking was explained predominately by the social context of drinking for such populations (Clapp et al., Citation2003) and related social norms (Christiansen, Vik, & Jarchow, Citation2002). Further research would be necessary to determine whether risky social drinking masked effects of anger rumination on alcohol use.
Several limitations should be considered. First, the correlational design precludes causal inferences, and a longitudinal design would be beneficial to determine the direction of associations. Second, the sample consisted predominantly of female university students from one location, and few men reported binge eating particularly. Therefore, caution about the generalisability of the results to other populations, including clinical groups, is needed. Third, anger rumination and trait anger are strongly correlated constructs. This study did not distinguish between variance due to each of these constructs and future studies should therefore consider the extent to which binge drinking is associated with anger rumination as opposed to trait anger.
To the best of our knowledge, this is the first study to demonstrate an association between rumination specific to anger and binge eating. The strength of this study is that it provides evidence of an association between aspects of anger rumination and binge eating, while controlling for anxiety, stress, and depression. It also suggests that anger rumination is a specific risk factor in binge eating and may perpetuate ongoing binge behaviours. In clinical settings, anger rumination could be assessed efficiently through brief self‐report measures, to indicate whether anger rumination is a contributing factor to individuals’ self‐regulatory difficulties. Individuals with high levels of anger rumination may benefit from focused interventions that target this cognitive style. Metacognitive therapy, rumination‐focused‐CBT, and mindfulness‐based CBT have demonstrated efficacy in treating depressive rumination (Dammen, Papageorgiou, & Wells, Citation2015; Watkins, Citation2015; Wells et al., Citation2012). Therefore, anger rumination may benefit from such treatment modalities and research is warranted that investigates anger rumination in clinical populations.
ACKNOWLEDGEMENT
The authors wish to thank Ben Lane, research assistant.
REFERENCES
- Arnow, B., Kenardy, J., & Agras, W. S. (1995). The Emotional Eating Scale: The development of a measure to assess coping with negative affect by eating. International Journal of Eating Disorders, 18, 79–90. https://doi.org/10.1002/1098-108X(199507)18:1<79::AID-EAT2260180109>3.0.CO;2-V
- Babor, T. F., Higgins‐biddle, J. C., Saunders, J. B., & Monteiro, M. G. (2001). AUDIT—The Alcohol Use Disorders Identification Test: Guidelines for use in primary care. (2nd ed.). Geneva, Switzerland: World Health Organisation.
- Baum, A., & Pozluszny, D. M. (1999). Health psychology: Mapping biobehavioural contributions to health and illness. Annual Review of Psychology, 50, 137–163. https://doi.org/10.1146/annurev.psych.50.1.137
- Besharat, M. A., & Shahidi, S. (2010). Perfectionism, anger, and anger rumination. International Journal of Psychology, 45, 427–434. https://doi.org/10.1080/00207594.2010.501336
- Birch, C. D., Stewart, S. H., & Brown, C. G. (2007). Exploring differential patterns of situational risk for binge eating and heavy drinking. Addictive Behaviors, 32, 433–448.
- Brennan, A. F., Walfish, S., & Aubuchon, P. (1986). Alcohol use and abuse in college students. A review of individual and personality correlates, International Journal of the Addictions, 21, 449–474. https://doi.org/10.3109/10826088609083536
- Bulik, C. M., Klump, K., Thornton, L., Kaplan, A. S., Devlin, B., Fichter, M. M., … Kaye, W. H. (2004). Alcohol use disorder comorbidity in eating disorders: A multicenter study. Journal of Clinical Psychiatry, 65, 1000–1006. https://doi.org/10.4088/JCP.v65n0718
- Bush, K., Kivlahan, D. R., Mcdonell, M. B., Fihn, S. D., & Bradley, K. A. (1998). AUDIT alcohol consumption questions (AUDIT‐C): An effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Archives of Internal Medicine, 158, 1789–1795. https://doi.org/10.1001/archinte.158.16.1789
- Christiansen, M., Vik, P. W., & Jarchow, A. (2002). College student heavy drinking in social contexts versus alone. Addictive Behaviors, 27, 393–404. https://doi.org/10.1016/S0306-4603(01)00180-0
- Ciesla, J. A., Dickson, K. S., Anderson, N. L., & Neal, D. J. (2011). Negative repetitive thought and college drinking: Angry rumination, depressive rumination, co‐rumination, and worry. Cognitive Therapy and Research, 35, 142–150. https://doi.org/10.1007/s10608-011-9355-1
- Clapp, J. D., Lange, J., Min, J. W., Shillington, A., Johnson, M., & Voas, R. (2003). Two studies examining environmental predictors of heavy drinking by college students. Prevention Science, 4, 99–108. https://doi.org/10.1023/A:1022974215675
- Connolly, A. M., Rieger, E., & Caterson, I. (2007). Binge eating tendencies and anger coping: Investigating the confound of trait neuroticism in a non‐clinical sample. European Eating Disorders Review, 15, 479–486. https://doi.org/10.1002/erv.765
- Dammen, T., Papageorgiou, C., & Wells, A. (2015). An open trial of group metacognitive therapy for depression in Norway. Nordic Journal of Psychiatry, 69, 126–131. https://doi.org/10.3109/08039488.2014.936502
- Demartini, K. S., & Carey, K. B. (2012). Optimizing the use of the AUDIT for alcohol screening in college students. Psychological Assessment, 24, 954–963. https://doi.org/10.1037/a0028519
- Denson, T. F. (2012). The multiple systems model of angry rumination. Personality and Social Psychology Review, 17, 103–123. https://doi.org/10.1177/1088868312467086
- Denson, T. F., Pedersen, W. C., Friese, M., Hahm, A., & Roberts, L. (2011). Understanding impulsive aggression: Angry rumination and reduced self‐control capacity are mechanisms underlying the provocation‐aggression relationship. Personality and Social Psychology Bulletin, 37, 850–862. https://doi.org/10.1177/0146167211401420
- Engel, S. G., Boseck, J. J., Crosby, R. D., Wonderlich, S. A., Mitchell, J. E., Smyth, J., … Steiger, H. (2007). The relationship of momentary anger and impulsivity to bulimic behavior. Behavior Research and Therapy, 45, 437–447. https://doi.org/10.1016/j.brat.2006.03.014
- Fassino, S., Daga, G. A., Piero, A., Leombruni, P., & Rovera, G. G. (2001). Anger and personality in eating disorders. Journal of Psychosomatic Research, 51, 757–764. https://doi.org/10.1016/S0022-3999(01)00280-X
- Faul, F., Erdfelder, E., Lang, A. G., & Buchner, A. (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39, 175–191.
- Ferriter, C., & Ray, L. A. (2011). Binge eating and binge drinking: An integrative review. Eating Behaviors, 12, 99–107. https://doi.org/10.1016/j.eatbeh.2011.01.001
- Gadalla, T., & Piran, N. (2007). Co‐occurrence of eating disorders and alcohol use disorders in women: A meta‐analysis. Archives of Women’s Mental Health, 10, 133–140. https://doi.org/10.1007/s00737-007-0184-x
- Hallet, J., Howat, P. M., Maycock, B. R., Mcmanus, A., Kypri, K., & Dhaliwal, S. (2012). Undergraduate student drinking and related harms at an Australian university: Web‐based survey of a large random sample. BMC Public Health, 12, 37. https://doi.org/10.1186/1471-2458-12-37
- Harder, V. S., Ayer, L. A., Rose, G. L., Naylor, M. R., & Helzer, J. E. (2014). Alcohol, moods and male‐female differences: Daily interactive voice response over 6 months. Alcohol and Alcoholism, 49, 60–65. https://doi.org/10.1093/alcalc/agt069
- Hilt, L. M., Armstrong, J. M., & Essex, M. J. (2015). Rumination and moderators of multifinality: Predicting internalizing symptoms and alcohol use during adolescence. Journal of Clinical Child & Adolescent Psychology, 46, 746–753. https://doi.org/10.1080/15374416.2015.1070354
- Jorgensen, R. S., & Kolodziej, M. E. (2007). Suppressed anger, evaluative threat, and cardiovascular reactivity: A tripartite profile approach. International Journal of Psychophysiology, 66, 102–108. https://doi.org/10.1016/j.ijpsycho.2007.03.015
- Leibsohn, M. T., Oetting, E. R., & Deffenbacher, J. L. (1994). Effects of trait anger on alcohol consumption and consequences. Journal of Child and Adolescent Substance Abuse, 3, 17–23. https://doi.org/10.1300/J029v03n03_02
- Lovibond, S. H., & Lovibond, P. F. (1995). Manual for the Depression Anxiety Stress Scales. (2nd ed.). Sydney, Australia: Psychology Foundation.
- Maxwell, J. P., Sukhodolsky, D. G., Chow, C. C. F., & Wong, C. F. C. (2005). Anger rumination in Hong Kong and Great Britain: Validation of the scale and a cross‐cultural comparison. Personality and Individual Differences, 39, 1147–1157. https://doi.org/10.1016/j.paid.2005.03.022
- Mckeen, N. A., Chipperfield, J. G., & Campwell, D. W. (2004). A longitudinal analysis of discrete negative emotions and health‐services use in elderly individuals. Journal of Aging and Health, 16, 204–227. https://doi.org/10.1177/0898264303262648
- Meyer, C., Leung, N., Waller, G., Perkins, S., Paice, N., & Mitchell, J. (2005). Anger and bulimic psychopathology: Gender differences in a nonclinical group. International Journal of Eating Disorders, 37, 69–71. https://doi.org/10.1002/eat.20038
- Milligan, R. J., & Waller, G. (2000). Anger and bulimic psychopathology among nonclinical women. International Journal of Eating Disorders, 28, 446–450. https://doi.org/10.1002/1098-108X(200012)28:4<446::AID-EAT13>3.0.CO;2-J
- Morrison, P. M., Noel, N. E., & Ogle, R. L. (2012). Do angry women choose alcohol?. Additive Behaviours, 37, 908–913.
- Naumann, E., Tuschen‐caffier, B., Voderholzer, U., Caffier, D., & Svaldi, J. (2015). Rumination but not distraction increases eating‐related symptoms in anorexia and bulimia nervosa. Journal of Abnormal Psychology, 124, 412–420. https://doi.org/10.1037/abn0000046
- Nolen‐hoeksema, S. (2004). The response styles theory. In C. Papageorgiou, & A. Wells, (Eds.), Depressive rumination: Nature, theory, and treatment (pp. 107–124). New York: Wiley.
- Nolen‐hoeksema, S., & Watkins, E. R. (2011). A heuristic for developing transdiagnostic models of psychopathology explaining multifinality and divergent trajectories. Perspectives on Psychological Science, 6, 589–609. https://doi.org/10.1177/1745691611419672
- Nolen‐hoeksema, S., Wisco, B. E., & Lyubomirsky, S. (2008). Rethinking rumination. Perspectives on Psychological Science, 3, 400–424.
- Ramos‐cejudo, J., Salguero, J. M., Kannis‐dymand, L., Garcia‐sancho, E., & Love, S. (2017). Anger rumination in Australia and Spain: Validation of the Anger Rumination Scale. Australian Journal of Psychology. Advance online publication. https://doi.org/10.1111/ajpy.12154
- Ray, R. D., Wilhelm, F. H., & Gross, J. J. (2008). All in the mind's eye? Anger rumination and reappraisal. Journal of Personality and Social Psychology, 94, 133–145.
- Rusting, C. L., & Nolen‐hoeksema, S. (1998). Regulating responses to anger: Effects of rumination and distraction on angry mood. Journal of Personality and Social Psychology, 74, 790–803. https://doi.org/10.1037/0022-3514.74.3.790
- Saunders, J. B., Aasland, O. G., Babor, T. F., De la fuente, J. R., & Grant, M. (1993). Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption—II. Addiction, 88, 791–804. https://doi.org/10.1111/j.1360-0443.1993.tb02093.x
- Stice, E., Agras, W. S., Telch, C. F., Halmi, K. A., Mitchell, J. E., & Wilson, T. (2001). Subtyping binge eating‐disorder women along dieting and negative affect dimensions. International Journal of Eating Disorders, 30, 11–27. https://doi.org/10.1002/eat.1050
- Stice, E., Fisher, M., & Martinez, E. (2004). Eating Disorder Diagnostic Scale: Additional evidence of reliability and validity. Psychological Assessment, 16, 60–71. https://doi.org/10.1037/1040-3590.16.1.60
- Stice, E., Telch, C. F., & Rizvi, S. L. (2000). Development and validation of the Eating Disorder Diagnostic Scale: A brief self‐report measure of anorexia, bulimia, and binge‐eating disorder. Psychological Assessment, 12, 123–131. https://doi.org/10.1037/1040-3590.12.2.123
- Sukhodolsky, D. G., Golub, A., & Cromwell, E. N. (2001). Development and validation of the anger rumination scale. Personality and Individual Differences, 31, 689–700. https://doi.org/10.1016/S0191-8869(00)00171-9
- Tabachnick, B. G., & Fidell, L. S. (2001). Using multivariate statistics. (4th ed.). Boston, MA: Little Brown.
- Waller, G., Babbs, M., Milliagan, R., Meyer, C., Ohanian, V., & Leung, N. (2003). Anger and core beliefs in the eating disorders. International Journal of Eating Disorders, 34, 118–124. https://doi.org/10.1002/eat.10163
- Watkins, E. (2015). Psychological treatment of depressive rumination. Current Opinion in Psychology, 4, 32–36. https://doi.org/10.1016/j.copsyc.2015.01.020
- Wells, A., Fisher, P., Myers, S., Wheatley, J., Patel, T., & Brewin, C. R. (2012). Metacognitive therapy in treatment‐resistant depression: A platform trial. Behaviour Research and Therapy, 50, 367–373. https://doi.org/10.1016/j.brat.2012.02.004
- Williams, J. E., Patton, C. C., Siegler, I. C., Eigenbrodt, M. L., Nieto, F. J., & Tyroler, H. A. (2000). Anger proneness predicts incident coronary heart risk: Prospective analysis from the Atherosclerosis Risk in Communities (ARIC) Study. Circulation, 101, 2034–2039. https://doi.org/10.1161/01.CIR.101.17.2034
- Zeeck, A., Stelzer, N., Linster, H. W., Joos, A., & Hartman, A. H. (2011). Emotion and eating in binge eating disorder and obesity. European Eating Disorders Review, 19, 426–437. https://doi.org/10.1002/erv.1066s