Abstract
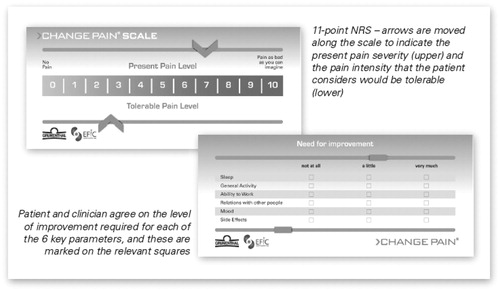
The major objectives of the CHANGE PAIN International Advisory Board are to enhance understanding of chronic pain and to develop strategies for improving pain management. At its second meeting, in November 2009, evidence was presented that around one person in five in Europe and the USA experiences chronic pain, and the delay before referral to a pain specialist is often several years. Moreover, physicians' pharmacological approach to chronic pain is inconsistent, as evidenced by the huge variation in treatment between different European countries. It was agreed that efficient communication between physician and patient is essential for effective pain management, and that efficacy/side-effect balance is a key factor in choosing an analgesic agent. The multifactorial nature of chronic pain produces various physical and psychological symptoms, so the management of chronic pain should be tailored to the individual. Pharmacological therapy must be matched to the causative mechanisms responsible, or it is likely to prove ineffective and risk the development of a ‘vicious circle’; doses are increased because of inadequate pain relief, but this increases side-effects so doses are reduced, pain relief is then inadequate, so doses are increased, and so on. Pain management decisions should not therefore be based solely on the severity of pain. Based on the concept of individual treatment targets (ITT), the CHANGE PAIN Scale was adopted – a simple, user-friendly assessment tool to improve communication between physician and patient. The 11-point NRS enables the patient to rate the current pain intensity and to set a realistic individual target level. On the reverse are six key parameters affecting the patient's quality of life; clinicians simply need to agree with patients whether improvement is needed in each one. Regular use can establish the efficacy and tolerability of pain management, and the rate of progress towards individual treatment targets.
Introduction
Epidemiological evidence indicates that a substantial proportion of adults in Europe and the USA suffer from chronic pain that seriously affects the quality of their social and working lives – and its inadequate management constitutes a major healthcare problemCitation1–4. Furthermore, the impact of chronic pain on national economies and healthcare resources can be considerableCitation5,Citation6. In November 2009, the international CHANGE PAIN consensus group of pain specialists met for the second time in Zurich. In addition to considering the reasons for inadequate pain management and discussing possible solutions, they evaluated a new approach aimed at improving communication between healthcare professionals and patients suffering from chronic pain. One objective is to optimise pharmacological treatment outcomes by moving the emphasis in pain management from symptom control to mechanism-orientated treatment.
Objectives of the CHANGE PAIN group
The wider aims of the CHANGE PAIN group are to enhance understanding of the needs of patients with chronic pain, and to develop strategies which will improve pain management. Important measures necessary to achieving such improvement have been identified: the consensus group is committed to supporting research that will provide a better understanding of physicians’ and patients’ perspectives, to publishing study results, and to contributing to the education of healthcare professionals. This will ultimately increase the knowledge of pain mechanisms and facilitate treatment decisionsCitation7.
Prevalence and impact of chronic pain
Chronic pain has a considerable effect on patients' quality of life, severely affecting their sleep, ability to exercise, walk, perform household chores, attend social activities and maintain an independent lifestyleCitation1. In order to improve treatment outcomes, it is important for healthcare professionals to appreciate the wider implications of chronic pain. Data regarding these aspects of chronic pain in Europe are available, particularly at a national level, but there are only a few pan-European sources. A telephone survey of 46 394 respondents in 15 European countries and Israel found that 19% of adults experienced moderate to severe chronic pain (≥5 on a 10-point Numeric Rating Scale; NRS; 1 = no pain and 10 = worst pain imaginable)Citation1. Approximately 20% of chronic pain sufferers said their doctor had never asked about their pain. Around half of these patients had constant pain, in approximately 20% of cases the pain had persisted for 20 years or more, and 40% felt their pain was inadequately managed, but only 2% of 4839 respondents who underwent in-depth interviews were currently being treated by a pain specialistCitation1.
Similar results have been obtained by studies in individual countries. For example, Sjøgren et al. concluded that 20.2% of the adult Danish population suffer from chronic pain, and more than one-third of sufferers are dissatisfied with the examinations made and the treatment offeredCitation2. A postal survey of 4000 adults in Norway found the prevalence of chronic pain to be 24.2% and that in 65% of cases it had been present for more than 5 yearsCitation3.
Current treatment of chronic pain
A study in Germany found that the average time from onset of pain until the first consultation with a general practitioner was 3 years, and until referral to a specialised pain centre was 12 yearsCitation8. In 47% of these cases referral was at the request of the patient, and in 71% referral resulted in a change to the patient's medicationCitation8. The delay before referral illustrates that the ongoing management of chronic non-cancer pain often rests with community-based service providers, particularly general practitionersCitation9. In fact, back pain and joint problems together represent the largest workload of chronic disease seen in the primary care settingCitation10. Therefore, general practitioners are not only the initial point of contact with healthcare systems, but have a vital role in optimising pain management.
As part of the CHANGE PAIN initiative, a physician survey was conducted at the 2009 European Federation of IASP Chapters (EFIC) Congress and is still continuing across Europe. The objective is to gain a better insight into current pain management, and some results became available at the 3rd International Conference on Neuropathic Pain in May 2010Citation11. Preliminary results indicate widespread agreement among physicians that pain reduction and improvement in quality of life are the main treatment goals, making the balance between efficacy and side-effects a key factor in the choice of analgesic. The majority of respondents felt there was a limited awareness of the physiological differences between nociceptive and neuropathic pain in the medical community, but at the same time agreed that neuropathic pain was often more severe and difficult to treat.
A growing trend in healthcare, owing to spiralling costs and the shortage of providers, is an emphasis on self-management strategies or group education sessions for patients with chronic medical conditionsCitation12,Citation13. This is very different from the traditional treatment model centred around doctor/patient clinic visits. Studies in patients with heart failure have found that self-management programs decrease both overall hospital re-admissions and re-admissions for heart failureCitation14, and that patients who did not adopt these strategies were at high risk of death or re-admissionCitation12. In patients with upper back pain, daily exercises prescribed by a professional therapist to emphasise postural awareness and provide a basic understanding of the disorder have been shown to be as crucial to reducing pain and stiffness as hands-on therapy in a clinical settingCitation15. A related issue is self-medication by patients with over-the-counter (OTC) drugs, of which the physician may be unaware. The concern is that readily available agents such as NSAIDs may present safety issues, especially in groups such as the elderly frail population, who may not be properly informed about their use. These are not benign medications, even at low dosages, so physicians should routinely ask patients about all forms of self-medicationCitation16.
Another potential answer to the problem of increasing costs and lack of medically qualified staff could be an extension of non-medical prescribing, e.g. by nurse prescribers and pharmacists, particularly for special populations like frail elderly patients. Experience in the UK, predominantly from primary care, indicates that both patients and nurse prescribers are generally satisfied with the practiceCitation17, but the continuing professional development needs of nurse prescribers are frequently unmetCitation18 and a number of issues relating to the role remain unresolved; these include communication systems, clinical governance and the attitude of other professionals, particularly the need for support from multidisciplinary teamsCitation19,Citation20.
Pain treatment: less than optimal
One factor that adversely affects pain therapy is poor communication. Successful pain management demands effective communication between physician and patient, to achieve a common understanding of the patient's condition and expectations, as well as the proposed therapy and achievable treatment goals. A good understanding reassures patients that the most appropriate analgesic therapy can be prescribed for their individual requirements. Effective communication is of particular importance with respect to the severity of pain, a highly individual experience, yet there is evidence that significant improvement is required, not only between physician and patient but also between healthcare professionals. For example, at the 2009 European Federation of IASP Chapters (EFIC) Congress, 403 respondents were asked to state where they believed severe pain began on an 11-point Numerical Rating Scale (NRS); answers mainly ranged from a score of 4 to 8Citation11. This demonstrates a wide variation in the individual interpretation of pain scales, and, therefore, in clinicians' perception of patients' experience of pain, potentially compromising any proposed treatment.
Poor communication between physician and patient has been demonstrated by a German study in which physicians and patients separately assessed pain intensity and pain-dependent impairment during rehabilitation training in chronic low back pain patients. Only 19.4% of physicians accurately rated patients' pain-related impairment. The relevance of adequate pain assessment is highlighted by the responder rate of 92.3% in this group (see )Citation21.
Figure 1. Differences between physicians' and patients' pain assessments: physicians frequently underestimate patients’ pain and impairment. [From Mueller-Schwefe, 2005].
![Figure 1. Differences between physicians' and patients' pain assessments: physicians frequently underestimate patients’ pain and impairment. [From Mueller-Schwefe, 2005].](/cms/asset/6b3ed396-3c84-4dd0-bfe6-d7e1ea6b12b8/icmo_a_545377_f0001_b.jpg)
Consensus point: efficient communication between physician and patient is crucial for a common understanding of chronic pain and its impact – the basis for adequate pain management.
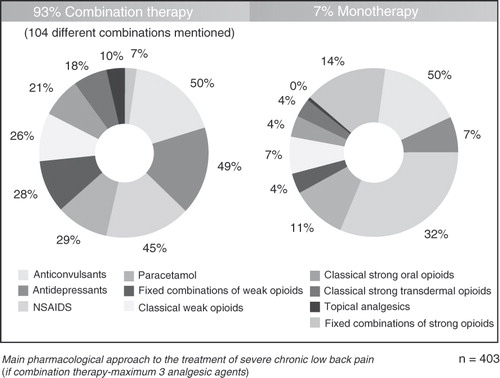
Management of chronic pain should be tailored to the individual. However, this treatment currently varies enormously, suggesting that it goes beyond the rational need for individualised treatment. This is exemplified by huge differences in the consumption of analgesics between different countries, in terms of both quantity and the type of agent prescribed. For example, data from the internationally accepted information provider IMS Health (International Medical Statistics) for 2008 showed that physicians in northern Europe are much more willing to prescribe opioids than those in the south and east. Of respondents to the CHANGE PAIN physician survey at the 2009 EFIC Conference, 93% stated combination therapy was their main pharmacological strategy for treating severe chronic low back pain and cited no fewer than 104 different combinationsCitation11 (see ). Thus, there is no consensus or consistency in physicians' pharmacological approach to chronic pain, and it may be concluded that clinical recommendations and guidelines are having little influence on treatmentCitation22,Citation23, which is probably less than optimal for some patientsCitation24.
The World Health Organization's three-step pain ladder was originally developed for treating cancer pain, but is now also used extensively for non-cancer painCitation25. It recommends non-opioid analgesics, weak opioids and strong opioids for Step I, Step II and Step III, respectively, depending solely on the intensity of the patient's painCitation25. However, chronic pain is related to multiple physiological causes or pathways, so it is rational to base pain management decisions not only on the severity of pain, but also on the underlying mechanisms responsibleCitation26. Unless these mechanisms are addressed, analgesic therapy is likely to prove ineffective. The tendency then is for the clinician to increase the dose of analgesics, which increases side-effects, so the dose is reduced, when pain relief again becomes inadequate, and so on. A ‘vicious circle’ may become established where the patient alternates between poor pain relief and avoidable side-effectsCitation7.
Most pain specialists now agree that the balance between adequate pain relief and acceptable tolerability is best achieved, with fewest adverse effects, by matching the pharmacological action to the causative mechanisms involvedCitation27. This may require combination therapy, since most commonly available analgesic drugs predominantly affect a single pain mechanismCitation28. More recent guidelinesCitation29–31 focus on identifying causative mechanisms in order to institute the most appropriate treatment, but – although it is the urgent duty of all concerned with pain relief to translate new knowledge of pain mechanisms into improved patient careCitation32 – these have not so far gained universal acceptanceCitation22,Citation23.
Consensus point: successfully treating severe chronic pain requires balancing analgesia with acceptable tolerability, but side-effects may limit the effective dose that can be tolerated – a vicious circle.
Mechanism-orientated pain treatment
Most pain is multifactorial in nature. Furthermore, the pain experience can be modulated by the limbic system and cerebral cortex, acting via a descending transmission system to produce inhibition or facilitation. Many different mechanisms can be involvedCitation26, and a better understanding of these mechanisms allows a more targeted approach to the choice of analgesic. This offers advantages over the conventional practice of grouping patients on the basis of a common aetiology or disease, which ignores the fact that a single aetiological factor can produce pain by diverse mechanisms that may occur singly, sequentially, or simultaneouslyCitation26.
Chronic pain (e.g., severe chronic low back pain) may be predominantly nociceptive, predominantly neuropathic, or a combination of both. Nociceptive pain is essentially a transient response to a noxious stimulus such as heat or pressure, and is reversibleCitation33, while neuropathic pain is not necessarily associated with a noxious stimulus and arises from an abnormality of the somatosensory system. This distinction has important clinical implications because of the different mechanisms involved. Neuropathic pain (e.g., post-herpetic neuralgia, trigeminal neuralgia) is associated with more intense and prolonged pain, more severe co-morbidity and poorer quality of lifeCitation34,Citation35, as a result of trophic and structural changes and central sensitisationCitation36. These patients experience persistent, spontaneous, lancinating pain caused by ectopic discharge, primarily in Aβ fibres, while central sensitisation may cause hyperalgesia and allodyniaCitation33. Recommended first-line treatments for neuropathic pain include tricyclic antidepressants and dual reuptake inhibitors of serotonin and noradrenaline, gabapentin and pregabalin, and topical lidocaineCitation30. Opioids are generally recommended for second-line treatment, but can be considered for first-line use in certain clinical circumstances, such as acute neuropathic pain or neuropathic cancer painCitation30. The early, effective treatment of acute pain is important in order to prevent its becoming chronic and consequently more complex to treat.
Ideally, clinicians would be able to identify the specific causative mechanisms underlying each patient's symptoms, and then prescribe the most appropriate therapy. For example, N-methyl-d-aspartate (NMDA) receptor antagonists could be given for the hyperalgesia caused by central sensitisation, or sodium channel blockers for the spontaneous pain caused by ectopic dischargesCitation37. However, such identification is difficult in practice, because one mechanism can produce different symptoms and one symptom can be produced by different mechanismsCitation38. Nevertheless, clinicians should be aware of the distinction between nociceptive and neuropathic pain, the causative mechanisms involved in each, and their contribution to treatment response. This background knowledge will help them to understand their patients' pain and guide treatment decisions.
Pain suspected of having several causative mechanisms should be managed by addressing each of the possible mechanisms, i.e. by multi-modal analgesia. This may include both pharmacological and non-pharmacological therapies such as physiotherapy or neuromodulation – for example, transcutaneous electrical nerve stimulation (TENS) or acupuncture. As most analgesic drugs are mono-modal (have a single mechanism of action), combinations of two or more may often be required simultaneously. This offers the potential for lower doses of the constituent drugs, improved pain relief as a result of additive or synergistic actions, and less severe adverse effectsCitation39. However, the drugs may exert their effects independently, or interact to potentiate or antagonise each other, affecting both analgesic efficacy and tolerability. Randomised controlled trials of a few drug combinations have shown encouraging results in terms of efficacy, tolerability and safety, but rigorous supportive evidence is limited and much more research is required into the wide range of combinations currently used to treat chronic painCitation40–42.
Consensus point: pain management decisions should focus mainly on the underlying mechanisms and not only on intensity of pain.
To increase understanding of these causative mechanisms, and their importance in achieving effective management of severe chronic pain, the CHANGE PAIN initiative involves conducting surveys, analysing published data, and communicating the results via electronic and printed media. This educational remit extends to continuous medical education (CME). Several interactive e-learning modules supported by the CHANGE PAIN group are currently under development by an independent agency, financed by an educational grant from Grünenthal. The first educational modules, which have been CME-accredited by the Union Européenne Des Médécins Spécialistes (UEMS), cover the following topics: assessing pain and patient/physician communication, multi-modal management of chronic pain, and mechanism-orientated pharmacological pain therapy. The modules can be accessed via the CHANGE PAIN website (www.change-pain.com).
The new CHANGE PAIN Scale
The poor management of chronic pain partly results from clinicians' inadequate communication and assessment skillsCitation43,Citation44. In a survey of 897 physicians dealing with cancer patients, 76% cited their own sense of low competence in patient assessment as the major barrier to effective pain managementCitation45. In addition, all healthcare practitioners exhibit a degree of assessment bias, which can lead to under-assessment of pain and a disparity between patients' and clinicians' ratings of pain intensityCitation44.
The use of standardised instruments can improve communication between physicians and patients, providing a greater insight into their pain and an indication of the level of pain relief they regard as acceptable. This is important not only for diagnosis and treatment, but also for its influence on the attitude of chronic pain patients; one of the strongest unique predictors of treatment satisfaction is patients' belief that their pain has been thoroughly evaluatedCitation46. As part of its commitment to improving physician/patient communication, the CHANGE PAIN group has produced a simple tool based on the concept of individual treatment targets (ITTs) developed by G. Mueller-Schwefe and M.A. UeberallCitation47. The CHANGE PAIN Scale can be used quickly and easily in the primary care setting to record pain intensity, define individualised treatment goals, and provide insight into ways of improving patients’ quality of life.
Numerous scales exist to measure the severity of pain, such as the visual analogue scale (VAS), the numeric rating scale (NRS) and the verbal rating scale (VRS), with the object of ‘quantifying’ it. Use of these scales is established in clinical trials and constitutes an effective means of monitoring changes in pain intensity over time. Acute pain can be reliably assessed, both at rest and during movement, by one-dimensional tools such as the VAS and NRS, but chronic pain assessment and its impact on physical, emotional and social functions require multi-dimensional qualitative tools and health-related quality of life instrumentsCitation48. A survey conducted in 2003 by Institute TNS Emnid of Bielefeld, Germany, suggested that fewer than 10% of patients who consult a physician because of pain are asked to demonstrate the intensity of their pain using a pain scale, or to complete a pain questionnaire.
Patients also differ enormously in what they consider to be an acceptable level of pain; very few expect complete pain relief and many will be happy with low levels of chronic pain, but a small proportion will readily tolerate much higher levels. Identifying these levels is an important factor in successful pain management. Pain scales can therefore play a role in establishing individual treatment targets (ITTs) and measuring patients' progress towards them.
To select the most appropriate therapy, physicians need a clear idea not only of a patient's level of pain and ITT, but also of the impact that pain has on the patient's quality of life. Several detailed questionnaires (e.g., Short Form-36/Short Form-12, Western Ontario and McMaster Universities Osteoarthritis Index, Brief Pain Inventory) are available to help assess this impact. They ask questions about the limitation of daily activities, emotional health, social life and energy levels, in order to build up an overall picture of the effect of chronic pain on the patient. Instruments such as pain diaries and questionnaires may also be used by patients to record their pain and its effect on their lives. Pain management can be improved by the detailed documentation of pain and its effect on quality of life using these methods, but they are comparatively involved and time-consuming. Consequently, they are suitable for pain specialists but rarely used by general practitioners and other primary care physicians. Thus, there is a requirement for a simple, user-friendly assessment tool which can be used in a short consultation and focuses on the most important aspects of chronic pain, simultaneously directing history-taking not only towards pain intensity, but also towards the patient's quality of life and expectations of treatment, which do not feature in the standard VAS and NRS scales.
The CHANGE PAIN Scale (see ) has been proposed to meet this requirement. The primary care physician or pain specialist can use it initially to identify the key elements of successful pain management, and subsequently to record patient-centred perception of changes in well-being. A major design criterion has been ease of use. The 11-point NRS on the front enables the patient's current pain intensity to be quickly established and a realistic target level to be set in collaboration with the patient. Six key parameters that affect patients' quality of life appear on the back; these are based on the Brief Pain Inventory and their importance has been indirectly confirmed by other studiesCitation1. Clinicians simply need to agree with patients whether and what level of improvement is needed in each of these. Results at subsequent appointments can be compared to establish the efficacy and tolerability of the chosen pain management strategy, and the rate of progress towards patients' ITTs.
The wider perspective
Better communication and patient assessment skills will help improve and tailor pain management, but other measures are also important and these depend upon advances in medical education. Firstly, a greater emphasis needs to be placed upon pain management in the medical undergraduate curriculum. For example, a recent report by the Pain Education Special Interest Group of the British Pain Society described the pain education of healthcare undergraduates in the UK as ‘woefully inadequate’; the median time spent on pain management by a medical student was 13 hours, with some spending only 6 hoursCitation49. Furthermore, the subject was taught piecemeal, as a part of other topics, rather than as a discrete moduleCitation49. Secondly, the focus of chronic pain education should change from symptom control to mechanism-based multi-modal pain management. This approach is endorsed by bodies such as EFIC, which organises and runs postgraduate courses, supports educational initiatives, and is working towards pan-European training and certification standards in pain medicine. Thirdly, the shift in focus should be accompanied by initiatives to boost the education of healthcare professionals on the adequate use of analgesics, non-pharmacological approaches and encouragement to follow the latest guidelines on pain relief. Widespread adoption of these measures could contribute significantly not only to the alleviation of individual suffering, but also to reducing the economic burden of chronic pain and lessening its considerable impact on healthcare resources.
Transparency
Declaration of funding
This article was based on a meeting held in Zurich, Switzerland, November 6–7, 2009, supported by an unrestricted educational grant from Grünenthal GmbH, Aachen, Germany.
Declaration of financial/other relationships
G.M-S., W.J., B.M., E.K., M.S., F.C., F.H., M.K-K., A.C.M., C.M., K.A., P.M., E.A., B.C., D.A., A.N., J.P. and G.V. have disclosed that they received honoraria to attend the meeting in Zurich.
Acknowledgement
The authors thank Derrick Garwood Ltd, Cambridge, UK, for editorial support, which was sponsored by Grünenthal GmbH, Aachen, Germany.
References
- Breivik H, Collett B, Ventafridda V, et al. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain 2006;10:287-333
- Sjøgren P, Ekholm O, Peuckmann V, et al. Epidemiology of chronic pain in Denmark: an update. Eur J Pain 2009;13:287-92
- Rustoen T, Wahl AK, Hanestad BR, et al. Prevalence and characteristics of chronic pain in the general Norwegian population. Eur J Pain 2004;8:555-65
- Coda BA, Bonica JJ. General considerations of acute pain. In: Loeser JD, Butler SH, Chapman CR, Turk DC, eds. Bonica’s Management of Pain, 3rd edn. Philadelphia, PA: Lippincott Williams & Wilkins, 2001:222-40
- Blyth FM, March LM, Nicholas MK, et al. Chronic pain, work performance and litigation. Pain 2003;103:41-7
- Jensen MK, Sjøgren P, Ekholm O, et al. Identifying a long-term/chronic, non-cancer pain population using a one-dimensional verbal pain rating scale: an epidemiological study. Eur J Pain 2004;8:145-52
- Varrassi G, Müller-Schwefe G, Pergolizzi J, et al. Pharmacological treatment of chronic pain - the need for CHANGE. Curr Med Res Opin 2010;26:1055-69
- Schulte E, Hermann K, Berghöfer A, et al. Referral practices in patients suffering from non-malignant chronic pain. Eur J Pain 2009 [Epub ahead of print]
- Review of chronic pain management Advisory Group. Department of Human Services, Victoria, Australia, 2008. Available at: http://www.health.vic.gov.au/chronicpain/downloads/advisory-group-tor.pdf [Last accessed 30/3/2010]
- Dziedzic KS, Hill JC, Porcheret M, et al. New models for primary care are needed for osteoarthritis. Phys Ther 2009;89:1371
- Varrassi G, Nossol S, Wiemer S. CHANGE PAIN Physician Survey at EFIC 2009 -- Physicians' perception on management of severe chronic non-cancer pain. Abstracts of the 3rd International Congress on Neuropathic Pain. Athens, 2010
- Wright SP, Walsh H, Ingley KM, et al. Uptake of self-management strategies in a heart failure management programme. Eur J Heart Fail 2003;5:371-80
- Davies S, Quintner J, Parsons R, et al. Preclinic group education sessions reduce waiting times and costs at public pain medicine units. Pain Med 2010;doi:10.1111/j.1526-4637.2010.01001.x [Epub ahead of print]
- Jovicic A, Holroyd-Leduc JM, Strause SE. Effects of self-management intervention on health outcomes of patients with heart failure: a systematic review of randomized controlled trials. BMC Cardiovasc Disord 2006;6:43
- Pesco MS, Chosa E, Tajima N. Comparative study of hands-on therapy with active exercises vs education with active exercises for the management of upper back pain. J Manipulative Physiol Ther 2006;29:228-35
- Thomas J, Straus WL, Bloom BS. Over-the-counter nonsteroidal anti-inflammatory drugs and risk of gastrointestinal symptoms. Am J Gastroenterol 2002;97:2215-19
- Latter S, Courtenay M. Effectiveness of nurse prescribing: a review of the literature. J Clin Nurs 2004;13:26-32
- Courtenay M, Carey N, Burke J. Independent extended and supplementary nurse prescribing practice in the UK: A national questionnaire survey. Int J Nurs Stud 2007;44:1093-101
- Walsh J. Non-medical prescribing in nurse-led community leg ulcer clinics. Br J Nurs 2006;15:S14-16
- Bradley E, Hyman B, Nolan P. Nurse prescribing: Reflections on safety in practice. Soc Sci Med 2007;65:599-609
- Mueller-Schwefe GHH, Ueberall MA. Pain intensity of patients with chronic low-back pain-induced restrictions to follow standardized rehabilitation programs are frequently underestimated by physicians and physiotherapists – results of a prospective German quality assurance program. WIP Poster 2, Proceedings of World Institute of Pain Conference, Barcelona, 2004
- Andersson GB. Epidemiological features of chronic low-back pain. Lancet 1999;354:581-5
- Pergolizzi J, Böger RH, Budd K, et al. Opioids and the management of chronic severe pain in the elderly: consensus statement of an international expert panel with focus on the six clinically most often used World Health Organization step III opioids (buprenorphine, fentanyl, hydromorphone, methadone, morphine, oxycodone). Pain Pract 2008;8:287-313
- Victor TW, Alvarez NA, Gould E. Opioid prescribing practices in chronic pain management: guidelines do not sufficiently influence clinical practice. J Pain 2009;10:1051-7
- World Health Organization. Cancer Pain Relief with a Guide to Opioid Availability, 2nd edn. Geneva, Switzerland: World Health Organization, 1996
- Woolf CJ, Max MB. Mechanism-based pain diagnosis: issues for analgesic drug development. Anesthesiology 2001;95:241-9
- Raffa RB, Tallarida RJ, Pergolizzi JV. The determination and application of fixed-dose analgesic combinations for treating multimodal pain. J Pain 2010;11:701-9
- Raffa RB. Pharmacological aspects of successful long-term analgesia. Clin Rheumatol 2006;25(Suppl 1):S9-15
- Attal N, Cruccu G, Haanpää M, et al. EFNS guidelines on pharmacological treatment of neuropathic pain. Eur J Neurol 2006;13:1153-69
- Dworkin R, O'Connor AB, Backonja M, et al. Pharmacologic management of neuropathic pain: evidence-based recommendations. Pain 2007;132:237-51
- Dworkin RH. Introduction: recommendations for the diagnosis, assessment and treatment of neuropathic pain. Am J Med 2009;122(10 Suppl):S1-2
- Macrae WA, Davies HTO, Crombie IK. Pain: paradigms and treatments. Pain 1992;49:289-91
- Woolf CJ, Salter MW. Neuronal plasticity: increasing the gain in pain. Science 2000;288:1765-69
- Freynhagen R, Baron R, Gockel U, et al. painDETECT: A new screening questionnaire to identify neuropathic components in patients with back pain. Curr Med Res Opin 2006;22:1911-20
- Schmidt CO, Schweikert B, Wenig CM, et al. Modelling the prevalence and cost of back pain with neuropathic components in the general population. Eur J Pain 2009;13:1030-5
- Costigan M, Scholz J, Woolf C. Neuropathic pain: a maladaptive response of the nervous system to damage. Annu Rev Neurosci 2009;32:1-32
- Costigan M, Woolf CJ. Pain: molecular mechanisms. J Pain 2000;1(Suppl 1):35-44
- Woolf CJ, Mannion RJ. Neuropathic pain: aetiology, symptoms, mechanisms, and management. Lancet 1999;353:1959-64
- Kehlet H, Dahl B. The value of “multimodal” or “balanced analgesia” in postoperative pain treatment. Anesth Analg 1993;77:1048-56
- Besson M, Piguet V, Dayer P, et al. New approaches to the pharmacotherapy of neuropathic pain. Expert Rev Clin Pharmacol 2008;15:683-93
- Gilron I, Bailey JM, Tu D, et al. Morphine, gabapentin, or their combination for neuropathic pain. N Engl J Med 2005;352:1324-34
- Hanna M, O'Brien C, Wilson MC. Prolonged-release oxycodone enhances the effects of existing gabapentin therapy in painful diabetic neuropathy patients. Eur J Pain 2008;6:804-13
- Glajchen M. Chronic pain: treatment barriers and strategies for clinical practice. J Am Board Fam Pract 2001;14:211-18
- Berry PH, Katz JA, Chapman CR, et al. Pain: Current Understanding of Assessment, Management, and Treatments. National Pharmaceutical Council and the Joint Commission for the Accreditation of Healthcare Organizations, VA, USA, 2001
- Von Roenn JH, Cleeland CS, Gonin R, et al. Physician attitudes and practice in cancer pain management. A survey from the Eastern Cooperative Oncology Group. Ann Intern Med 1993;119:121-6
- McCracken LM, Evon D, Karapas ET. Satisfaction with treatment for chronic pain in a specialty service: preliminary prospective results. Eur J Pain 2002;6:387-93
- Ueberall MA, Mueller-Schwefe GHH. Individual treatment targets in chronic pain management. Proceedings of the 5th Congress of The European Federation of the IASP Chapters (EFIC), Istanbul, 2006
- Breivik H, Borchgrevink PC, Allen SM, et al. Assessment of Pain. Br J Anaesth 2008;101:17-24
- Survey of undergraduate pain curricula for healthcare professionals in the United Kingdom: a short report. The Pain Education Special Interest Group of the British Pain Society. The British Pain Society, London, UK, 2009. Available at: http://www.britishpainsociety.org/members_sig_edu_short_report_survey.pdf [Last accessed 22nd January 2010]