Abstract
Objective:
To investigate the long term smoking cessation behaviors in a population of Japanese current smokers (CS) and former smokers (FS).
Research design and methods:
Retrospective survey of Japanese men and women ≥20 years of age who were CS (those who smoked any number of cigarettes at the time of the survey, 24–27 June 2013) or FS (those who had smoked any number of cigarettes in the past but did not consider themselves smokers at the time of the survey). CS/FS were selected from a prescreened source population recruited by online advertisement that was age- and gender-matched, to represent Japanese smokers. Clinical and socio-demographic characteristics and smoking/smoking cessation history were assessed through a web-based questionnaire.
Main outcome measures:
Main outcome measures were number of past quit attempts and time to relapse; others included methods used to achieve smoking cessation, and reasons for wanting to quit.
Results:
Overall, 1261 Japanese subjects were surveyed (CS, n = 631; FS, n = 630). Nearly half (45.6%) of CS had never attempted to quit smoking. Of those who had attempted to quit smoking, one single quit attempt was the most common for both CS and FS (19.0 vs. 39.0%). Estimated median time to relapse was 105 days (FS and CS combined). Unaided smoking cessation was the most common method both for CS and FS (78.2 vs. 63.4%).
Conclusions:
In our survey, >70% of smokers used unaided smoking cessation methods, which may have resulted in a lower success rate. Participants relapsed after a median of 105 days of abstinence (25% within 7 days; the remainder had resumed smoking after 1260 days). As with all surveys, recall bias may have influenced the results. Our observations could be combined with other data in health economic models of smoking cessation to identify appropriate measures to reduce the prevalence of smoking in Japan.
Keywords::
Introduction
Smoking is the most common cause of morbidity and mortality in Japan, with 130,000 Japanese people estimated to die each year from smoking-related diseases (this figure excludes deaths due to second-hand smoking)Citation1. Scientific evidence on the relationship between smoking and health damage, such as increased risk of cancer and cardiovascular and respiratory disease, has been extensively documented worldwideCitation2,Citation3. Furthermore, approximately 6800 people in Japan alone are estimated to die every year from passive smokingCitation4, emphasizing that health damage, not only to the smokers themselves but also to people around them, is a significant issue. Decreased tobacco use has been shown to reduce the development of smoking-related diseases and death in smokersCitation5,Citation6 and also reduce exposure to passive smoking. In addition to an improvement of adverse health-related outcomes, smoking cessation also has a considerable financial impact, including reductions in healthcare costs for smoking-related diseases and loss of productivity associated with illness or smoking behavior itselfCitation7; anti-tobacco policies, therefore, are now a global issue. In Japan, the National Health Promotion Movement in the 21st Century (Healthy Japan 21 [Second Version]), pursuant to the Health Promotion Law, stipulates that adult smoking prevalence is to be reduced to 12% by 2022. This is the first time a specific target for the prevalence of smoking has been set. According to the National Health and Nutrition Examination Survey, however, the prevalence of smoking among Japanese people was 20.1% in 2011, up from 19.5% in 2010. Although for Japanese men the prevalence of smoking has been gradually decreasing (from 55.3% in 1989 to 34.1% in 2011), that for Japanese women has been fluctuating between 9% and 12% since 1989Citation8. After the enforcement of the 2002 Health Promotion Law and the 2004 Framework Convention on Tobacco Control legislation, various measures such as restricting smoking in public places and raising the tax on tobacco were implemented. However, in Japan, these measures have proven inadequate compared with other industrialized nationsCitation9.
In addition, support systems in Japan for those who wish to quit smoking are insufficient. The first clinical practice guidelines for smoking cessation therapy under the Japanese public health insurance system was issued in 2005/2006. Since then, the Japanese Circulation Society has issued clinical practice guidelines for smoking cessation pharmacotherapy and counseling (latest version: 5th version, 2012). According to the 2011 National Health and Nutrition Examination Survey, on average 32.8% of smokers expressed a desire to quit. Based on this survey and other population statistics, there would be an estimated 22 million smokers in Japan; hence, 6–7 million Japanese smokers are potentially willing to quit. Smoking cessation therapy covered by the public health insurance system includes pharmacotherapy (such as high-dose nicotine patches and varenicline; bupropion is not licensed for smoking cessation in Japan), as well as counseling. Nicotine patches (low dose) and nicotine gum are available without prescription. Counseling services are provided by physicians only; no quit line services are available in Japan. To be eligible for smoking cessation therapy under the public health insurance system, patients must meet several criteria for nicotine dependence as assessed by the Tobacco Dependence Screener (TDS), and nicotine use as assessed by the Brinkman Index. Based on the 2011 Survey of Medical Care Activities in Public Health InsuranceCitation10, only about 210,000 people annually initiate smoking cessation therapy under the public health insurance system. The lack of access to effective smoking cessation therapy thus interferes with the stated governmental goal of reducing the prevalence of smoking.
When devising future measures to promote and successfully implement restrictions on tobacco use, it is pivotal to gather national data on smoking cessation behaviors and their consequences; achieving current goals requires the collection of data which reflect the actual behaviors of smokers. Several studies have looked into the effectiveness of smoking cessation aids and the usefulness of pharmacotherapy and counseling to improve smoking abstinence and prevent relapse after successful smoking cessationCitation11–13. For example, a recent study by Hagimoto et al.Citation11 used a postal questionnaire survey to identify predictors of relapse based on the most recent quit attempt (i.e., a single quit attempt). However, quitting is commonly a dynamic process with repeated quit attempts and repeated relapse from smoking abstinenceCitation14. Therefore, multiple quit attempts and multiple relapse episodes need to be considered in studies in order to mimic the actual behaviors of smokers. The long term natural course of smoking cessation behaviors has been reported in a US population of smokersCitation15,Citation16. However, in terms of an official smoking cessation policy, the US is somewhat ahead of Japan, and data obtained in the US cannot be directly applied to a Japanese scenario. Longitudinal data on multiple quit attempts are currently not available for the population of Japanese smokers.
The primary objective of this retrospective study was to investigate long term smoking cessation behaviors in a population of current smokers (CS) and former smokers (FS) through a web-based survey. In particular, we aimed to explore the number of attempts made to quit, and the time to relapse for unsuccessful attempts.
Patients and methods
Study design
An online web-based survey of a population of healthy Japanese men and women aged ≥20 years who were CS or FS was conducted from 24 to 27 May 2013 to assess smoking cessation behaviors. The source population was an online database comprising Japanese residents who following online advertisement had provisionally agreed to participate in online surveys (Anterio Inc., Japan). The protocol was prepared based on that previously reported for a similar US web-based survey conducted by Yeomans et al.Citation16. Prior to initiation of the study, the protocol was approved by the Ethics Review Committee, Health Outcome Research Institute.
Subjects who were registered in the online database as self-identified CS or FS of any tobacco product were prescreened for initial eligibility by Anterio Inc. and contacted via email for participation. Potentially eligible responders were asked to provide consent to participate in the survey after reading the objectives and a document explaining the protection of confidentiality on the survey website. Those who provided consent were given access to a web-based screening questionnaire. During this screening process, any subjects <20 years of age, non-smokers (those who had never smoked any cigarettes in their lifetime) and those who smoked any other tobacco product than cigarettes were excluded. Eligible participants were categorized at the time of survey screening according to their self-reported smoking status (CS or FS); CS were those who reported they smoked any number of cigarettes at the time of the survey, and FS were those who reported they had smoked any number of cigarettes in the past but did not consider themselves smokers at the time of the survey. The age and gender distributions of both CS and FS were adjusted according to vital statistics and the National Health and Nutrition Examination Survey of 2012, to ensure the representativeness of the survey subjects of a Japanese population of smokers. Enrollment of survey participants was to be continued until a minimum survey sample size of 600 CS and 600 FS was reached (i.e., enrollment was stopped once the minimum sample size was reached); this sample size was based on several factors, including the feasibility of recruitment and results from past surveys. Participants could withdraw from the survey at any time and/or skip any questions that they did not want to answer.
Data collection
The online questionnaire items were classified into three categories: (1) socio-demographic and clinical characteristics; (2) smoking patterns and smoking characteristics; (3) patterns of previous smoking cessation attempts. Each question used was adjusted according to whether it was intended for CS or FS.
Socio-demographic and clinical characteristics
Information was collected from participants on age, gender, body height, body weight, race, level of education and income, as well as the presence of diagnosed comorbidities, defined as the following 20 diseases/conditions: acid reflux, anxiety, arthritis, asthma, back pain, cancer (lung), cancer (other), chronic bronchitis, chronic obstructive pulmonary disease (COPD), coronary artery disease, depression, diabetes, emphysema, fibromyalgia/chronic fatigue, heart failure, hypertension, insomnia, migraine/headaches, stroke (of any severity); categories ‘other significant medical condition’ and ‘none in particular’ were also included. Those subjects who reported having cancer other than that of the lung were asked to specify its type. Survey participants were also asked about their alcohol intake over the past 28 days.
Smoking patterns and smoking characteristics
Questions on smoking history included the age at which participants had started smoking, the total number of years they had spent smoking, and the number of packs of cigarettes smoked per day and per year (a pack being defined as 20 cigarettes). Based on the number of packs of cigarettes smoked per day, the subjects were classified at baseline as heavy (≥1 pack/day) or light (<1 pack/day) smokers. The level of nicotine dependence was assessed using the Fagerström Test for Nicotine Dependence (FTND) questionnaire (six questions; scores 1–10)Citation17. In this study, a score of 0 to 2 was defined as low, 3 to 6 as moderate, and 7 to 10 as high nicotine dependenceCitation18. FTND scores were assessed for both CS and FS and were used in the analyses. For FS, the subjects were asked about the period when they had smoked. Participants were also asked about their smoking environments, e.g., whether they were cohabiting with other smokers, or currently had family members, colleagues or friends who smoked.
Patterns of smoking cessation attempts
All participants (i.e., both CS and FS) were asked about the number of times they had attempted to quit smoking in the past (0 [never attempted smoking cessation], 1, 2, 3, 4, 5, 6–10, or >11 times), and the smoking cessation methods they had used for each attempt to quit (back to the fifth most recent attempt). The options were: oral anti-smoking therapy (varenicline), nicotine replacement therapy (patch or gum), counseling, acupuncture, aromatherapy, Chinese traditional herbal medicine (Kampo), unaided cessation only (‘cold turkey’ or self-help). The categories ‘other’ and ‘do not recall’ were also included, the year and season of each quit attempt, the duration of each cessation method used (time to abstinence), and the duration of the ensuing actual smoking-free period (time to relapse). Bupropion was not licensed in Japan at the time of the survey and therefore not included in the options for smoking cessation methods. For the duration of smoking cessation (time to abstinence plus time to relapse), categorical intervals were set to minimize recall bias (never stopped smoking, <1 week, 1–4 weeks, 1–6 months, 7–11 months, 1–2 years, 3–5 years, >5 years, and ‘do not recall’). Those who had attempted to stop smoking were also asked about their reason(s) for wanting to quit. Options for reason(s) to quit smoking were: a current health problem, general health concerns, expenses associated with smoking, concerns about exposing others to passive smoking, wanting to set a good example, bad breath, smell or taste, pressure from family, friends or colleagues, advice from a doctor or dentist, illness or death of a family member, or friend/acquaintance, smoking restrictions in the workplace, or other.
In addition, the participants were asked about the overall most typical time to relapse, the longest smoking-free period they had ever experienced, and the types of cessation methods used since becoming a smoker.
Statistical analysis
Analyses were conducted for the CS and FS subgroups as well as for the total sample. Descriptive statistics were used for socio-demographic and clinical characteristics, smoking modalities, and smoking cessation modalities, with mean values and standard deviation (SD). In addition, median and minimum/maximum values are reported for continuous variables, and frequencies and proportions for categorical variables. Time to relapse and time to next quit attempt after relapse were also calculated; when calculating the duration of smoking cessation, the final attempt to quit (successful attempt) of the FS was excluded.
Time to relapse data were stratified according to FTND scores (low, moderate or high nicotine dependence), smoking cessation attempts (first, second, third, fourth and fifth most recent attempts, excluding the final attempt to quit for FS), smoking cessation methods (unaided cessation only or any cessation method), and age at the time of smoking cessation (≤29, 30–39, 40–49, 50–59, or ≥60 years). The duration of smoking cessation was presented as categorical ranges (<1 week, 1–4 weeks, 1–6 months, 7–11 months, 1–2 years, 3–4 years, or >5 years). When calculating each period, the end and median points of each range were adopted as representative values, and mean differences between each pairs were calculated using the Steel–Dwass test. Stratified analyses were performed on the total survey sample only. Survival analyses were performed to estimate time to relapse and time to next quit attempt after relapse employing the Kaplan–Meier method, allowing censoring of data (for CS, time to next quit attempt after the most recent relapse were regarded as censored data).
Statistical analyses in this study were carried out using JMP Pro 10 (SAS Institute). Analyses using Wilcoxon rank-sum tests were done in Stata 13 (Stata Corp LP).
Results
The survey was conducted over 4 days, at which time a sufficient numbers of participants had been enrolled into the study. Among the 23,370 subjects who were originally recruited via online advertisement by Anterio Inc. Japan, 10,537 were contacted for possible inclusion into the survey. Of a population of 1551 initial responders who completed the screening questionnaire, and that were age- and gender-matched to be representative of the Japanese population of smokers, the first 1261 eligible subjects were included into the survey; 631 CS and 630 FS. Median and mean times participants spent completing the questionnaire were 5.0 and 19.4 min, respectively.
Socio-demographic and clinical characteristics
All 1261 eligible subjects were Japanese, 29.4% (n = 371) were female, mean age (SD) was 47.9 (10.5) years, and mean body mass index (BMI) (SD) was 23.0 (3.9) kg/m2 (). The proportion of participating females was lower than that of men, since recruitment into the survey was adjusted according to age/gender distributions in line with official vital statistics and official smoking rates for Japan. Among CS (n = 631) a slightly lower proportion were females than among FS (n = 630; 26.1 vs. 32.7%), and mean age (SD) was slightly lower too (47.1 [9.8] years vs. 48.7 [11.1] years, respectively). Mean BMI values (SD) (23.0 [4.0] vs. 23.0 [3.8] kg/m2, respectively) were similar.
Table 1. Socio-demographic and clinical characters of current and former Japanese smokers.
Among FS, the proportion with a higher education (i.e., university graduate or postgraduate degree) was greater than among CS, and the proportion of FS with lung cancer, COPD, stroke or coronary artery disease was also higher than that of CS. For both CS and FS, the most commonly diagnosed comorbidity was hypertension.
Smoking patterns and smoking characteristics
The mean ages (SD) at which CS and FS had started smoking were similar (21.1 [6.8] vs. 20.5 [6.8] years, ). The mean age (SD) at which FS had quit smoking (i.e., the age at the start of the final cessation attempt) was 36.8 (11.3) years. A greater proportion of CS than FS (70.4 vs. 63.8%; p < 0.05) described themselves as being heavy smokers (≥1 pack/day) in their last 12 months of smoking. Overall, 49.5% had moderate (3–6) FTND scores, and the proportion with moderate nicotine dependence was higher among CS than FS (55.9 vs. 43.0%; p < 0.0001). A larger proportion of CS than FS (32.5 vs. 21.0%; p < 0.0001) were cohabiting with other smokers. In addition, a larger proportion of CS than FS also reported having family members, friends or colleagues who smoked (p < 0.0001; see also Supplemental file).
Table 2. Smoking patterns and characteristics, including potential sources of passive smoking exposure, for current and former Japanese smokers.
Patterns of smoking cessation attempts
The most common reason for wanting to quit smoking differed between FS and CS. Among FS, the most common reason was health concerns, whereas for CS it was the expense associated with smoking. Nearly half (45.6%) of CS had never attempted to quit smoking. Of those who had attempted to quit smoking, the number of quit attempts was significantly higher for FS than for CS, and one single quit attempt was the most common for both CS and FS (19.0 vs. 39.0%; with 15.5 vs. 24.1%, 9.0 vs. 18.1%, and 11.0 vs 18.7% having attempted quitting 2, 3, and ≥4 times; p < 0.001 [Wilcoxon rank-sum test] for CS vs. FS at each attempt). A constant proportion of CS had attempted unaided cessation (‘cold turkey’ or self-help only) at each quit attempt (); the same trend was observed in FS, although a higher proportion of FS than CS attempted unaided smoking cessation (78.2 vs. 63.4%; p < 0.0001), which was the most common method overall (72.7%); other methods included nicotine gum or patches (13.7%), anti-smoking therapy (varenicline; 3.8%), counseling (1.1%) and other (including herbal medicine, aromatherapy and acupuncture; 8.8%). The proportion that had a smoking-free period of ≥1 year was similar for those who had used unaided cessation compared with those who had used aided cessation (e.g., anti-smoking/nicotine replacement therapy, herbal medicine, acupuncture, aromatherapy, counseling, etc.; 17.8 vs. 14.7%; ). Only 7.7% of all subjects (using unaided cessation) compared with 7.5% (using aided cessation) had a smoking-free period ≥5 years. The proportion of subjects who claimed to have experienced a smoking-free period was slightly higher for those who used aided compared with unaided cessation (78.8 vs. 73.3%; p < 0.05). The vast majority (83.5%) of FS had not smoked for more than a year ().
Figure 1. Proportion of Japanese current and former smokers who had attempted to quit smoking without assistance during the past five quit attempts. For former smokers, the final quit attempt was excluded.
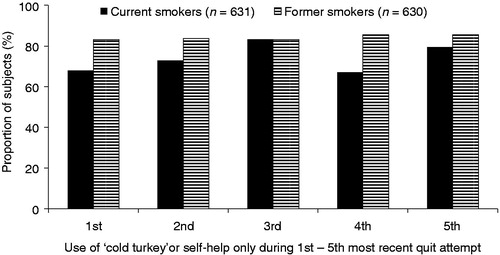
Table 3. Proportion of Japanese subjects (current and former smokers combined) who attempted aided and unaided smoking cessation and their duration of abstinence from smoking.
Time to relapse
The estimated median time to relapse overall was 105 days (FS and CS combined, based on the Kaplan–Meier curve, ); overall 25% of subjects relapsed and began smoking again within 7 days, and 75% had resumed smoking by 1260 days (3.5 years, ).
Figure 2. Kaplan–Meier curves of (a) time to relapse and (b) time to next quit attempt in Japanese subjects (current and former smokers combined).
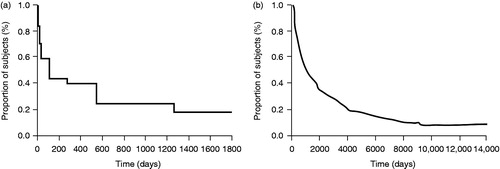
Table 4. Estimated time to next attempt to quit smoking and the estimated time to next smoking abstinence relapse in current and former Japanese smokers.
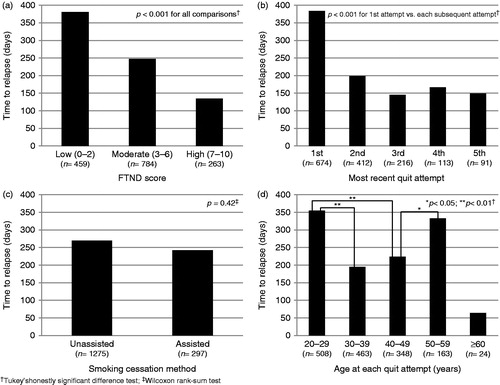
The mean time to relapse was significantly longer for those with lower FTND scores (0–2) than for those with moderate (3–6) and high scores (7–10, ). In addition, the mean time to relapse for the first most recent quit attempt was significantly longer than those for the second to fifth most recent attempts (). There was no significant difference in the mean time to relapse between unaided compared with aided cessation methods (). When analyzing all quit attempts (first to fifth most recent attempt), a significant difference in time to relapse was noted between those aged ≤29 years and 40–49 years, but there was no apparent overall trend between time to relapse and age ().
Figure 3. The mean time to relapse according to (a) Fagerström Test for Nicotine Dependence (FTND) score, (b) each recent attempt to quit smoking, (c) use of smoking cessation methods, and (d) age at most recent quit attempt in Japanese subjects (current and former smokers combined). Assisted smoking cessation methods included: anti-smoking therapy (varenicline), nicotine replacement therapy (gum/patches), counseling, acupuncture, aromatherapy, Chinese herbal medicine (Kampo) and others; unaided smoking cessation included: ‘cold turkey’ or self-help only.
Time to next quit attempt
The estimated median time to next quit attempt overall was 1006 days (2.8 year years) (based on the Kaplan–Meier curve, ), and overall 25% of the subjects had attempted to quit smoking after 356 days (1.0 years), and 75% after 3288 days (9.0 years, ).
Discussion
This study provided a variety of important background data on a population of current and former smokers in Japan, including FTND scores and smoking history, as well as information on their smoking cessation behaviors such as methods used, number of recent quit attempts made, and time to relapse between attempts.
The results confirm that although more than half of the smokers had attempted to quit, mainly for reasons such as the harmful effects of smoking on health and the expense associated with the habit, most failed to remain abstinent and had a relapse. Over 60% of those who experienced a relapse on their first attempt tried to quit smoking again after a certain period of time, with the mean time to relapse for the first recent quit attempt being significantly longer than those of subsequent attempts (second to fifth recent attempt; 384 days vs. 198, 145, 167, 150 days, respectively; p < 0.001). The majority of those who relapsed into smoking within 1 year after a quit attempt did not attempt to quit again for another 3 years. These findings imply that the time horizon needs to be set longer to allow multiple quit attempts to be incorporated when constructing health economic models that mimic actual behaviors of smokers in Japan.
Various methods were used to achieve smoking cessation. Regardless of the number of quit attempts, the majority (73%) of smokers did not use any therapy or assistance. Few data are available in Japan regarding the success rates for unaided smoking cessation. However, Nakayama conducted a clinical trial comparing the success rate of short-term advice on smoking cessation during medical check-ups vs. a control group receiving no adviceCitation19. Among those receiving no cessation advice, only 4.0% succeeded in quitting smoking, even among those willing to quit (defined as those who had considered quitting in the prior 6 months). In Nakayama’s trial, participants who did not actively try to quit smoking were included, but since they were categorized as ‘willing to quit’, presumably most of them could also be considered as ‘trying to quit’. Hence, it is reasonable to assume that the success rate for unaided cessation, although it could be expected to be slightly higher than 4.0%, is still fairly low. A high proportion of unaided quit attempts may result in a lower smoking cessation rateCitation20,Citation21, and poor access to effective treatment may be a hurdle for successful smoking cessationCitation22; in Japan, only 210,000 out of the 6–7 million smokers who wanted to quit have attempted to do so with smoking cessation treatment covered by public health insurance.
In terms of assisted smoking cessation, Japan has seemingly fallen behind other industrialized countriesCitation10. According to Nakamura, the proportion who attempted to quit smoking using cessation aids in Japan was less than half of those in the US and UK (16.6 vs. 40.5 and 47.2%, respectively)Citation23. Even though more effective measures for giving up tobacco use have become available in Japan, such as smoking cessation therapy at medical institutions and over-the-counter cessation aids, they are not commonly used. This is partly due to a low awareness of these aids among Japanese smokers but also the restricted accessibility through the healthcare system. In our study, among those who achieved smoking abstinence, no difference was seen in the type of methods used to quit. However, the proportion of subjects who had experienced a smoking-free period was slightly higher for those who used cessation aids than for those who had tried to quit without assistance (78.8 vs. 73.3%). It would seem that those using cessation aids when trying to quit smoking have a better chance of achieving their goal.
Our data indicate that CS are more likely to a have social circle consisting of smokers than FS. While it is conceivable that the smoking status of one’s social circle may affect one’s smoking habits and quit pattern, we cannot ascertain any causality from our data.
We investigated the actual smoking cessation behaviors in a Japanese population in accordance with the survey method employed by an earlier study in the USCitation16, thus allowing data from the two countries to be compared. In both studies, the majority of subjects attempted unaided smoking cessation, which evidence suggests may be a relatively ineffective strategy; the proportion attempting unaided smoking cessation was higher among Japanese compared with American subjects (72.7 vs. 52.1%). While the study by Yeoman et al. showed that in a US population this proportion steadily decreased as the number of repeated attempts to quit rose (for CS, from 76.1% through 66.9, 54.5, 54.0, and 43.9%; for FS, from 79.3% through 67.8, 63.5, 57.4, and 50.3%), the proportion of Japanese subjects attempting unaided smoking cessation remained high with multiple attempts to quit (for CS, from 68.0% through 72.9, 83.4, 67.1, and 79.6%; for FS, from 83.2% through 83.8, 83.2, 85.5, and 85.5%). The time to relapse was substantially longer in Japanese than in American subjects (median 15 vs. 4 weeks, respectively), with smoking abstinence more likely to be maintained by Japanese than by American subjects; however, the time to next quit attempt was nearly three times as long for Japanese as for American subjects (median 33 vs. 12 months, respectively). Such a long time to next quit attempt after relapse may well be an obstacle to successful lowering of smoking prevalenceCitation24,Citation25.
Due to the web-based nature of the survey, inevitable limitations are the inability to achieve a random probability-based sample and potential selection bias. In our study, FS and CS volunteered for participation, and it is conceivable that those who chose to register might well be more aware of their health than those who did not and, as with other web-based surveys, those lacking internet access were unable to participate. There was no specified time frame of abstinence used for the categorization of FS. Instead this was based solely on the respondents’ replies to the questionnaire (in line with the method used by Yeomans et al.Citation16 for the US survey). Hence, subjects who had quit smoking within days prior to participating in the survey may have been categorized as either CS or FS dependent on their own judgment. However, this was thought to apply to only a limited number of participants with negligible impact on the overall results. Also, the questionnaire allowed for multiple answers for smoking cessation methods used (i.e., subjects who had used methods in combination) in order to be reflective of actual practice, but in the analysis of these data all methods were counted independently. However, the number of subjects with multiple answers was small relative to the total number of subjects (14 of 630 FS). Thus, the effect of overlapping numbers of cessation methods on the final results is likely to have been minimal.
Another limitation in our research is recall bias and accuracy, since our survey was based on self-reporting by the participants. Recall bias may have been more pronounced for FS in terms of their recollection of smoking cessation methods used and past smoking habits, especially for those FS who had quit smoking some time ago. In order to minimize the recall bias of participating subjects, categorical ranges were used whenever possible. The diagnosed comorbidities reported were not otherwise validated (against claims data or medical records). Hence, comorbidity data were only included for baseline characteristics and not used for the stratified analyses. Furthermore, the interpretation of questions and understanding of applicable smoking cessation methods might have varied among the participants depending on their educational level, personal experiences and surrounding environments.
In our study, we found that overall more FS than CS had suffered serious diseases, which may have been a strong motivator for them to quit smoking and potentially may have introduced selection bias between the CS and FS groups. However, only the diagnosis of hypertension (and stroke; data not shown) was significantly different between the groups and the impact on the overall results of any potential bias was considered negligible. FS might also have been more likely to have been afflicted by tobacco-associated diseases; however, further research would be needed to fully elucidate confounding comorbidity issues.
We did not include a direct comparison of the various smoking cessation methods used by participants. Our aim was to assess which methods smokers were using to help quit smoking; it was not to compare success rates and/or smoke-free periods obtained with the various methods. Also, the proportion of unaided attempts was large compared with the proportion of aided attempts and a direct comparison between each smoking cessation methods would not have been statistically meaningful. Additional research into the efficacy of various smoking cessation methods is needed to facilitate increasing smoking abstinence in Japan, since our study indicates that Japanese smokers are currently more likely to attempt to quit smoking unaided, which is associated with lower success rates.
Several effective anti-smoking treatment options are available in Japan but further efforts are needed to mitigate existing barriers to access these under public health coverage. Physician’s counseling with or without pharmacotherapy can, when certain requirements are met, be covered by public health insurance. However, it is not yet common for smokers in Japan to visit their physician to get help with quitting tobacco. This is partly due to lack of information among the general population. For young smokers, it would be difficult to get access to smoking cessation assistance under public health insurance, since the Brinkman Index needs to be >200 according to the qualifying criteria. In addition, smoking cessation pharmacotherapy and counseling cannot be provided for smokers who are already hospitalized. Hospitals and clinics that want to provide anti-smoking counseling as a service are required to be tobacco-free. As a consequence, only 13.8% of medical institutions in Japan (May 2014)Citation26 provide smoking cessation therapy under the coverage of the public health insurance. Moreover, if smokers fail to quit after having received counseling, they are not eligible for any other smoking cessation therapy for another 12 months. Over the counter medications, including nicotine patches and nicotine gums, is not commonly used by Japanese smokers, and quit line services that have proven effective in adjacent countries, such as Korea, are not available in Japan.
No data are currently available that show the quitting patterns and behaviors of the Japanese smoking population over time. As most smokers usually make several attempts to quit smoking, our findings may be useful for predicting and mimicking actual behavior of smokers, and facilitate further analyses using economic modeling of smoking cessation interventions in Japan, with the ultimate goal of reducing smoking prevalence by providing a more accurate picture of smoker behaviors.
Transparency
Declaration of funding
This research was funded by Pfizer Japan Inc. The authors are solely responsible for the opinions and research findings published in this article. Specific contributions – A.I.: study design/conduct/data collection, data analysis and interpretation, writing of manuscript; S.N.: data analysis and interpretation, writing of manuscript; R.G.: data analysis and interpretation, writing of manuscript; K.S.: study conduct/data collection, writing of manuscript.
Declaration of financial/other relationships
K.S. has disclosed that she is an employee of Pfizer Japan Inc. A.I. and R.G. have disclosed that they received a research grant from Pfizer Japan Inc. in connection with the conduct of this study. In addition, A.I. has disclosed that he received research support from CLS Behring Japan Inc., served as an advisor/consultant to Abbvie GK., Novartis Pharma K.K., CRECON Research and Consulting Inc., Sony Inc., Kantor Health Inc., and Pfizer Japan Inc., been on a speakers bureau for Abbvie GK., Abbott Japan Co. Ltd, Boehringer Ingelheim Japan Inc., Chugai Pharmaceutical Co. Ltd, Novartis Pharma K.K., Sandoz Japan Inc., Takeda Pharmaceutical Co. Ltd, and Pfizer Japan Inc., and been employed in a laboratory funded by TOWA Pharmaceuticals Co. Ltd. S.N. has disclosed that he has no significant relationships with or financial interests in any commercial companies related to this study or article.
CMRO peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Supplementary Material
Download PDF (14.3 KB)Acknowledgments
Editorial support was provided by Anne Jakobsen of Engage Scientific Solutions and funded by Pfizer Japan Inc. The web-based survey was conducted by Yuka Tone of Anterio Inc. and funded by Pfizer Japan Inc. Independent statistical analysis was conducted by Koji Shimamoto of MdiStatLab Co. Ltd and funded by Pfizer Japan Inc.
References
- Ikeda N, Inoue M, Iso H, et al. Adult mortality attributable to preventable risk factors for non-communicable diseases and injuries in Japan: a comparative risk assessment. PLoS Med 2012;9:1001-60
- A Study Meeting on Smoking and Health Problems: New Version: Smoking and Health (in Japanese). Tokyo: Hokendohjinsha Inc., 2002
- U.S. Department of Health and Human Services. The Health Consequences of Smoking – 50 Years of Progress: A Report of the Surgeon General 2014. Rockville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, 2014
- Katanoda K, Mochizuki Y, Saika K, et al. Estimation of the number of deaths attributable to passive smoking in Japan. J Health Welfare Stat 2010;57:14-20
- Glantz S, Gonzalez M. Effective tobacco control is key to rapid progress in reduction of non-communicable diseases. Lancet 2011;379:1269-71
- Starr G, Rogers T, Schooley M, et al. Key outcome indicators for evaluating comprehensive tobacco control programs. Atlanta, GA: Centers for Disease Control and Prevention, 2005. Available at: http://www.cdc.gov/tobacco/tobacco_control_programs/surveillance_evaluation/key_outcome/ [Last accessed December 2013]
- Institute for Health Economics and Policy. Study on the Modality of Smoking Cessation Policy – Estimation of Costs Associated with Smoking (in Japanese). Institute for Health Economics and Policy, 2010
- Ministry of Health, Labour and Welfare. 2011 National Health and Nutrition Examination Survey (in Japanese). Ministry of Health, Labour and Welfare, 2013
- WHO report on the global tobacco epidemic, 2013. Enforcing bans on tobacco advertising, promotion and sponsorship. MPOWER, 2013
- Ministry of Health, Labour and Welfare. 2011 Survey of Medical Care Activities (in Japanese). Ministry of Health, Labour and Welfare, 2012
- Hagimoto A, Nakamura M, Morita T, et al. Smoking cessation patterns and patterns and predictors of quitting smoking among the Japanese general population: a 1-year follow-up study. Addiction 2009;105:164-73
- Hajek P, Stead LF, West R, et al. Relapse prevention interventions for smoking cessation. Cochrane Database Syst Rev 2013;8:CD003999
- Nakamura M, Oshima A, Ohkura M, et al. Predictors of lapse and relapse to smoking in successful quitters in a varenicline post hoc analysis in Japanese smokers. Clin Ther 2014;36:918-27
- Cohen S, Lichtenstein E, Prochaska JO, et al. Debunking myths about self-quitting. Evidence from 10 prospective studies of persons who attempt to quit smoking by themselves. Am Psychol 1989;44:1355-65
- Borland R, Partos TR, Yong HH, et al. How much unsuccessful quitting activity is going on among adult smokers? Data from the International Tobacco Control Four Country cohort survey. Addiction 2012;107:673-82
- Yeomans K, Payne KA, Marton JP. Smoking, smoking cessation and smoking relapse patterns: a web-based survey of current and former smokers in the US. Int J Clin Pract 2011;65:1043-54
- Heatherton TF, Kozlowski LT, Frecker RC, et al. The Fagerstrom test for nicotine dependence: a revision of the Fagerstrom tolerance questionnaire. Br J Addict 1991;86:1119-27
- Ministry of Health, Labour and Welfare, Health Service Bureau, Cancer Control and Health Promotion Division, ed. Manual for Smoking Cessation Support (The second edition). Tokyo (Japan): Ministry of Health, Labour and Welfare, Health Service Bureau, Cancer Control and Health Promotion Division. 2013 [In Japanese]
- Nakayama, T. Study of the development and institutionalization of a smoking cessation policy in cancer screening. In: Health and Labor Sciences Research Grant, The third General Strategy Against Cancer Research Project 2013. Study of institutionalization for the development and dissemination of an effective smoking cessation policy to reduce cancer risk (PI: Nakamura, M). 2013:3
- Raupach T, West R, Brown J. The most ‘successful’ method for failing to quit smoking is unassisted cessation. Nicotine Tob Res 2013;15:748-9
- Kasza KAI, Hyland AJ, Borland R, et al. Effectiveness of stop-smoking medications: findings from the International Tobacco Control (ITC) Four Country Survey. Addiction 2013;108:193-202
- Marti J. Successful smoking cessation and duration of abstinence – an analysis of socioeconomic determinants. Int J Environ Res Public Health 2010;7:2789-99
- Nakamura, M. Current condition and future issues of smoking cessation policy in Japan. J Jap Med Assoc 2012;141:1917-22
- Wetter DW, Cofta-Gunn L, Fouladi RT, et al. Late relapse/sustained abstinence among former smokers: a longitudinal study. Prev Med 2004;39:1156-63
- Gilpin EA, Pierce JP, Farkas AJ. Duration of smoking abstinence and success in quitting. J Natl Cancer Inst 1997;89:572-6
- Japan society for tobacco control. The number of medical institutes in which smoking cessation therapy can be provided under public health insurance system in Japan [In Japanese]. Available from: http://www.eonet.ne.jp/~tobaccofree/hoken/sokei.htm, accessed on 30 Jun 2014

