Abstract
Importance of the field: Capsaicin and its receptor, TRPV1, occupy a central place in current neurophysiological studies regarding pain transmission and have opened new avenues for understanding the role of transient receptor potential (TRP) receptors in itch processing. Substantial efforts in drug discovery are at present directed at vanilloid receptors for finding new remedies for pain and itch.
Areas covered in this review: We provide an overview of the major clinical indications of capsaicin, primarily targeting pain and itch of various origins, with an emphasis on the usefulness of capsaicin in treating pruritus and dermatological conditions. In particular, we cover the most relevant findings in recent years, from 2000 onward (although seminal discoveries and studies are discussed irrespective of their date of publication if deemed essential for understanding capsaicin's actions).
What the reader will gain: Readers are offered a broad perspective on the areas of clinical application of capsaicin, emphasizing its usefulness in the treatment of neurophatic pain and pruritus of various origins.
Take home message: Capsaicin has been proven a truly exciting molecule and remains a valuable drug for alleviating pain and itch, widely surpassing its role as a simple spicy ingredient.
Keywords::
1. Introduction: historical notes
Capsaicin, the active pungent ingredient in hot chilli peppers has been in use for ages as a spicy additive, according to some reports as far back as 7000 bce. Its pharmacological adaptation, which started in the middle of the 19th century, is now being revived by the emergence of new FDA-approved, high-concentration patches.
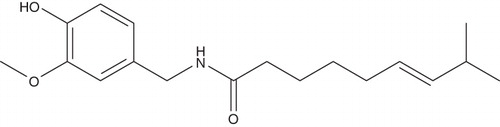
Capsaicin is a water-insoluble derivative of homovanillic acid, first extracted (in impure form) in 1816 by Christian F. Bucholz and obtained in a pure form in 1876 by John C. Thresh, who gave it the current name. The structure of capsaicin was elucidated by E. K. Nelson in 1919 (see ) and capsaicin was synthesized in 1930 by Spath and Darling () Citation[1].
Box 1. Drug summary.
Closely related analogs of capsaicin were isolated from chili peppers by Kosuge and Inagaki, who named them capsaicinoids. Capsaicin is the main capsaicinoid in hot chili peppers, seconded by dihydrocapsaicin and they are about twice as potent in pungency as the minor capsaicinoids nordihydrocapsaicin, homo-dihydrocapsaicin and homocapsaicin. There are at least six natural capsaicinoids and one synthetic member of this family. Several natural and synthetic analogs, agonists and antagonists of the capsaicin receptor (TRPV1) have been obtained and investigated because of the potential of these molecules in the treatment of pain and itch.
2. Chemical structure
Capsaicin is an acylamide of homovanillic acid presenting three functional moieties: vanillyl, acylamide and alkenyl. Capsaicin molecule contains a double bond; therefore, it can theoretically present cis and trans isomers. trans-Capsaicin is the naturally predominant isomer due to steric hindrance factors; made via rational synthesis the ‘trans’ form is the active compound used in high-potency NGX-4010 patches (Qutenza®, NeurogesX, Inc., San Mateo, CA). An intranasal formulation of the cis isomer called ‘zu-capsaicin’ (Civamide) is investigated as a therapy for cluster headache and in a topical cream formulation for osteoarthritis.
3. Mechanism of action
Capsaicin's actions can be classified into TRPV1-mediated actions and TRPV1-independent effects and mechanisms.
The specific action of capsaicin occurs via its interaction with TRPV1 receptors in primary sensory neurons found in polymodal C and Aδ mechano-heat nociceptors. Since TRPV1 is expressed in many cell types other than primary sensory neurons (keratinocytes, mast cells, glial cells, platelets) other biological actions of capsaicin could also work via a TRPV1-mediated mechanism (see Citation[2]). Capsaicin selectively activates TRPV1 receptors present on polymodal mechano- and heat-sensitive C nerve fibers and mechano heat-sensitive Aδ-fibers, which are referred to as ‘capsaicin-sensitive’ neurons. These nerve fibers can transmit both pain and itch; more specifically, C polymodal nociceptors can transmit experimental itch induced by cowhage spicules via release of the protease mucunain.
Initially, capsaicin binds cation channel TRPV1 receptor, which leads to channel opening, Ca2+ and Na+ entry and nerve depolarization, stimulating substance-P (SP) release and swiftly producing an intense burning and stinging sensation that can be perceived as painful or itchy (in the majority of subjects). Capsaicin induces an initial hypersensitization followed by a long-lasting nerve desensitization, which constitutes the basis of its therapeutic use. Substance P is not the only neuropeptide released, but TRPV1 activation induces the release of somatostatin, calcitonin gene related peptide (CGRP) and other neuromediators (neurokinin A, kassinin), leading to neurogenic inflammation. Capsaicin releases neuropeptides from sensory nerve endings via two mechanisms: (a) a secretory efferent function of TRPV1 neurons releases neuropeptides by exocytosis upon their depolarization; and (b) via an antidromic reflex stimulation of dorsal root ganglia (DRG) neurons Citation[3]. The long-term analgesic and antipruritic effects of prolonged capsaicin application are paradoxical, since capsaicin can induce initially both (burning) pain and itch. The beneficial analgesic action is explained by the subsequent, lasting desensitization. The stimulated release of substance P is soon followed by an exhaustion of substance P reserves which renders neurons desensitized or refractory. The mechanisms of desensitization may involve several stages and are not completely understood. The short-term desensitization is related to capsaicin's ability to block the intra-axonal transport of nerve growth factor (NGF), substance P and somatostatin Citation[4-6]. NGF controls the expression of neuropeptides via a NGF-responsive element in the preprotachykinin gene encoding substance P and neurokinin A (NKA) Citation[7], which explains how the depletion of NGF from the perykarya of sensory neurons induces a depletion of substance P (and neurokinin A; see Citation[2]).
4. Molecular mechanism of TRPV1 desensitization by capsaicin
To explain the relationship between substance P depletion and the ensuing desensitization, one has to examine the regulation of the TRPV1 receptor channel at the molecular level. TRPV1 activation by capsaicin binding induces an amplified release of substance P and CGRP upon neuronal depolarization, via exocytosis and antidromic reflexes. Substance P acts upon neurokinin-1 (NK-1) receptors (a G-protein-coupled receptor), which colocalize with TRPV1 receptors in TRPV1+ neurons. NK-1 receptors regulate the translocation and activation of PKCϵ, a kinase that is essential for the activation of TRPV1 via phosphorylation Citation[8]. Therefore, there is a positive feedback loop that increases the (hyper)sensitization of TRPV1 (manifested as hyperalgesia) and the sustained release of mediators, which in turn activates further the TRPV1+ neurons. The depletion of substance P is a consequence of this amplified response, which continues until the neuropeptide reserves are exhausted. The activation of TRPV1 is a result of complex regulatory mechanisms controlling phosphorykation/dephosphorylation states at two critical Serine residues and are dependent on intracellular calcium concentration, Ca–CaM binding to TRPV1, levels of IP3, ATP, CaM kinase II and the action of calcineurin (the latter deactivating TRPV1), among other factors Citation[9-11]. A depletion of SP induces a deactivation of TRPV1 due to the loss of phosphorylation primarily via downregulating the PKCϵ pathway, a major regulatory mechanism for TRPV1. When the activating factors are depleted, the equilibrium is shifted towards the dephosphorylated state and TRPV1 becomes inactivated (desensitized).
The short-term effect of vanilloid application is a downregulation of TRPV1 itself, a phenomenon labeled ‘phenotypic switch’ or defunctionalization Citation[2,12]. Ultimately, capsaicin induces a substantial decrease in the density of TRPV1-positive epidermal nerve endings, which explains the analgesia induced by capsaicin over extended periods of time (lasting up to several weeks). The significant neuronal degeneration observed following extended application of capsaicin is probably caused by vanilloid-mediated neuronal apoptosis and by capsaicin's direct neurotoxicity, reversible upon discontinuation of the drug. Topical capsaicin (0.075% or the 8% trans-capsaicin patch) produced a degeneration of epidermal nerve fibers that was correlated with the diminished pain sensation; upon discontinuation of the drug, the return of nociception in about 6 weeks was found to coincide with reinnervation. Citation[13,14].
The potential spectrum of action of capsaicin is wider than the effects elicited via TRPV1 interaction. Capsaicin exerts several other pharmacodynamic actions by targeting other molecular entities by vanilloid-independent mechanisms. We briefly note below the other mechanisms by which capsaicin may exert secondary actions, side-effects and (neuro)toxicity ().
Table 1. TRPV1-independent pharmacological actions of capsaicin.
5. The significance of capsaicin receptor (TRPV1) in physiology
Besides its use in alleviating pain and itch in clinical practice, capsaicin has a significant theoretical value. Capsaicin became a useful pharmacological tool for basic research helping to unearth the physiological function of the receptor it is acting upon. The discovery of a capsaicin-sensitive receptor has opened new avenues in pain and itch research. Now it is widely accepted that TRPV1 and the related vanilloid receptors are important relays for pain transmission (‘pain sensors’), and they play several physiological roles.
The cloned TRPV1 is a 95-kDa protein with intracellular N- and C-termini and the N-terminus presents three ankyrin domains. The structure of TRPV1 has six transmembrane domains with an additional intramembrane loop connecting the fifth and sixth transmembrane domains Citation[15]. TRPV1 can be activated by (noxious) temperature above 43°C (mediates pain hyperalgesia), low extracellular pH, eicosanoids and diverse endogenous lipid derivatives Citation[16-18]. TRPV1 is now found to be expressed at lower levels in the spinal cord, brain and a wide-range of non-neuronal cells such as epithelial cells (keratinocytes, urothelium, gastric epithelial cells, enterocytes, pneumocytes), in platelets, in vascular endothelium and cells of the immune system (T cells, mast cells) in smooth muscle, fibroblasts and hepatocytes Citation[19].
Insights for a physiological role of TRPV1 came from earlier studies that were linked to substance P dysregulation. A sequel of the treatment with vanilloid agonists was loss of hair and skin ulcerations Citation[20,21]; the damage was attributed to the depletion of substance P from dermal nerve endings Citation[22,23]. Alopecia areata was linked to a defect in vanilloid-sensitive nerve function and, indeed, recently a couple of studies have uncovered capsaicin's positive effect in stimulating hair growth. A capsaicin cream induced vellus hair regrowth in some patients with alopecia areata Citation[24,25], while a controlled randomized trial found capsaicin action in this regard superior to clobetasol (see below) Citation[26]. Substance P was also shown to facilitate hair growth in mice Citation[27]. TRPV1 agonists cause pain and itch in humans and pain behavior in animals, while the disruption of TRPV1 gene or a block of TRPV1 receptor by antagonists ameliorates thermal hyperalgesia Citation[28,29].
After more than 12 years of intense research on TRPV1 receptor since its discovery as capsaicin's primary target, the current general consensus is that TRPV1 plays a significant role in pain signaling; but it is not limited to sensory functions Citation[30,31]. TRPV1 is now considered to be involved in the following physiological or pathophysiological functions: it plays a major role in body-temperature maintenance Citation[32], regulation of feeding and body weight Citation[33], respiratory inflammation and disease Citation[34,35]; interestingly, the activation of TRPV1 by agonists exerts beneficial effects on cardiovascular and gastrointestinal functions Citation[36-39].
Endogenous ligands for TRPV1 have been recently identified that may indicate that capsaicin therapeutic action may depend on a competition with a range of endogenous players. Arachidonic acid derivatives and lypoxygenase products exert potent stimulatory effect on TRPV1 (e.g., arachidonyl-ethanolamide, anandamide previously known as a cannabinoid receptor 1 agonist; N-arachidonoyl dopamine and N-oleoyldopamine Citation[17]).
6. Absorbtion, pharmacokinetics and metabolism
When used in a topical formulation the lipophilic capsaicin penetrates the stratum corneum and is slowly delivered through the skin into systemic circulation at a rate of ∼ 2.71 μg/cm2/h Citation[40]. Capsaicin is metabolized by cytochromes P450 in the liver to dihydrocapsaicin and other hydroxylated metabolites (9 metabolites in total). Serum concentrations following the 8% dermal patch application are remarkably low and are detectable only in a small fraction of human subjects to whom capsaicin was applied topically. The maximum plasma concentration observed in any patient studied was 17.8 ng/ml. Capsaicin serum concentrations decline rapidly, with a mean population elimination half-life (t1/2) of 1.64 h. The mean area under the curve (AUC) and Cmax values after a 60-min application were 7.42 ng/h/ml and 1.86 ng/ml, respectively Citation[41]. Capsaicin is thought to be primarily eliminated via the renal route. A very slow inactivation by cleavage of the amide bond also occurs in the human skin following topical administration to yield vanillylamide and vanillic acid, but this process is considered largely inconsequential Citation[42].
7. Analogs of capsaicin
Topical capsaicin per se has a rather low therapeutic index by inducing a characteristic, initially strong, unpleasant burning and stinging sensation (irritation). Being not very well tolerated, capsaicin can easily render itself impractical to use, causing a high withdrawal rate during treatment (up to 30%) Citation[2,43]. Therefore several analogs are being sought and evaluated as safer, better-tolerated alternatives, both as agonists or antagonists of TRPV1.
Resiniferatoxin (RTX) is an improved TRPV1 agonist, first isolated in 1975, which was subsequently described as a highly potent vanilloid Citation[44,45]. Animal studies performed with RTX found a more favorable ratio of desensitization to irritation than capsaicin Citation[46-48]. RTX is more potent than capsaicin to induce nerve desensitization.
Rutaecarpine, a major quinazolinocarboline alkaloid isolated from Chinese herbal drug Wu-Chu-Yu, has long been used for the treatment of gastrointestinal disorders, headache, amenorrhea and postpartum hemorrhage in traditional Chinese medicine Citation[49]. The multiple pharmacological actions of rutaecarpine seem to be mediated by the released neurotransmitters such as CGRP and substance P through the activation of TRPV1 Citation[50].
Capsazepine was evaluated as one of other potential alternatives to capsaicin, serving as a TRPV1 antagonist, and was found to be beneficial in animal models of pain and inflammation Citation[51,52]. Several synthetic TRPV1 agonists and antagonists have been investigated and reviewed recently Citation[53].
8. Current clinical uses of capsaicin
8.1 Overview
The counterirritation and the extended desensitization that follows topical capsaicin application are used in clinical practice in the amelioration of pain and itch. The recently FDA-approved use of 8% trans-capsaicin via dermal patches (NGX-4010, Qutenza) in single application is reviving the therapeutic use of capsaicin (see Section 8.5). Pharmacological ‘ablation’ of C-fibers by perineural capsaicin injection was also tried in cancer patients with untractable pain Citation[54].
We briefly list below the conditions for which capsaicin has been clinically tested and proven effective as an analgesic. We refer the reader to excellent reviews available on the use of capsaicin for neuropathic pain for a more in-depth analysis Citation[15,30,55] to emphasize the benefits of capsaicin in the relief of itch.
A particularly challenging condition, dually painful and pruritic, is postherpetic neuralgia (PHN), which presents pain and itch both generally and refractory to therapy Citation[56,57]. The recent Phase III trial using 8% synthethic trans-capsaicin patch has documented the amelioration of pain scores by 30%, 2 – 12 weeks after a single patch application for 1 h Citation[58]. However, the effect on the accompanying itch of PHN – which can be very severe and sometimes intractable – was not reported, apparently not being an end point of this study. We can only speculate that the positive results obtained in relieving pain of PHN promises this formulation can be effective as an antipruritic to a comparable degree.
Therapeutic application of the long-lasting desensitization induced by capsaicin has been documented since 1850. The first medicinal indication of capsaicin on record was for toothache Citation[59]. Eugenol and guaiacol, other vanilloid receptor ligands commonly used in dentistry, also seem to exert their analgesic activity via TRP receptors Citation[60,61]. Capsaicin is effective in ‘atypical odontalgia’ Citation[62], in ‘burning mouth’ syndrome Citation[63] and in vasomotor rhinitis Citation[64,65]. The intranasal application of a single dose of 30 mM capsaicin solution relieves nasal congestion in patients with allergic rhinitis Citation[66,67]. Capsaicin could reduce the size of nasal polyps and the intranasal administration is also reportedly effective in cluster headache Citation[68-71].
Capsaicin is used to relieve muscle pain in a variety of over-the-counter (OTC) formulations (Capsazin® Capsoderma®, Stimurub®, Heat®); their therapeutic effect is due to the secondary neurogenic inflammation, which produces an increase in microcirculation in the respective area; the mediators of this action seem to be CGRP and somatostatin Citation[72,73]. However, the full mechanism of ‘counterirritation’ is not well elucidated.
8.2 Major indications for capsaicin
Used as an adjuvant analgesic, capsaicin acts locally by inducing a lasting desensitization of peripheral nerve fibers. In topical formulations, capsaicin has been used in a variety of neuropathic pain conditions such as postherpetic neuralgia, a condition that presents severe, sometimes intractable itching Citation[74-77]; painful diabetic neuropathy Citation[78-79], postmastectomy pain syndrome Citation[80,81] and in joint disease (osteoarthritis and rheumatoid arthritis Citation[82,83]; see ).
Table 2. Clinical indications of topical capsaicin for pain relief.
A condition considered until recently refractory to topical capsaicin was HIV-related neuropathy. However, the high-concentration 8% dermal patch NGX-4010 (Qutenza) in a single 60-min administration was able to induce a 30% amelioration of pain, to a duration of up to 12 weeks Citation[84].
In a Phase III, placebo-controlled trial, 99 cancer patients with postsurgery neuropathic pain were given capsaicin cream 0.075% (or placebo) four times a day for 8 weeks. At the end of the 8 weeks, there was a 53% reduction in pain in the capsaicin group compared with 17% in the placebo group. As main adverse effects, there was significant burning and redness Citation[85].
8.2.1 Joint disease
It has been discovered that substance P and CGRP are important mediators for arthralgia. Since capsaicin has the long-term effect of depleting substance P and CGRP, it could therefore attenuate pain signaling in arthritis. It is also possible that counterirritation contributes to the analgesic effect. In experimental models of arthritis, capsaicin was able to reduce joint inflammation, although it is not totally clear whether topical capsaicin penetrates well to affect sensory nerve endings in joint structures. In a controlled study of 21 patients, a 0.075% capsaicin cream improved tenderness and pain in joints with osteoarthritis (a degenerative form of arthritis), but had no effect in patients with rheumatoid arthritis (an inflammatory form of arthritis) Citation[86]. However, in a similar study in which 70 patients with osteoarthritis and 31 patients with rheumatoid arthritis were treated with capsaicin 0.025% cream (or placebo) four times a day for 4 weeks, 80% of patients experienced a reduction in knee pain during treatment with capsaicin cream, while the placebo response was 48%; burning occured in 44% of patients Citation[82].
8.3 Topical capsaicin for the relief of itch
Since itch sensation is mediated by unmyelinated polymodal C nociceptors/pruritoceptors that can equally transmit pain, capsaicin can be rationally used as an antipruritic owing to the lasting desensitization of sensory nerve fibers it induces Citation[87-90]. In a similar fashion to relieving pain, capsaicin can block peripheral nerve transmission of itch. In such a way, capsaicin offers the advantage of a local therapy, practically ‘numbing’ the peripheral neuronal pathways transmitting itch, without the notable side effects associated with systemic agents, tricyclic antidepressants, opiate antagonists and neuroleptics. Capsaicin has been shown to have a beneficial antipruritic effect in different types of itch (), neuropathic itch (itch arising from damaged peripheral nerve fibers) Citation[91,92], in systemic itch (uremic pruritus in patients undergoing hemodialysis), as well as relieving pruritus of dermatological origin: psoriasis, lichen simplex chronicus and prurigo nodularis. In the majority of the placebo-controlled studies, capsaicin's effect was consistently more potent than the placebo.
Table 3. Indications of topical capsaicin to relieve itch and improve dermatological disorders.
8.3.1 Neuropathic itch
Topical capsaicin has been used successfully for the amelioration of itch of notalgia paresthetica, a condition characterized by pruritus in the scapular area caused by entrapment of the posterior branches of T2 – T6 nerves Citation[93-95], and in brachioradial pruritus, a peripheral neuropathic form of itch caused by entrapment of C4 – C7 cervical nerve fibers Citation[91].
8.3.2 Systemic itch
The cause of itch of uremic patients on hemodialysis is still not completely understood. Interestingly, capsaicin is effective in treating systemic itch occurring in chronic kidney patients undergoing hemodialysis Citation[100,101]. In a double-blind, placebo-controlled, crossover study, 19 hemodialysis patients with moderate to severe pruritus were examined. Fourteen out of the 17 patients who completed the study reported a marked relief and five patients had a complete remission of pruritus. Capsaicin was significantly more effective than placebo and the therapeutic effect antipruritic lasted 8 weeks.
8.3.3 Relief of itch of dermatological origin
8.3.3.1 Lichen simplex chronicus
Lichen simplex chronicus is a condition where chronic itching and scratching lead to thickening of the skin with potential scaling (lichenification). Patients with this condition reported improvement of the pruritus following capsaicin cream application; interestingly, however, 75% of patients who reported beneficial effects actually preferred placebo to capsaicin, probably because of the intense irritation induced by capsaicin Citation[98].
8.3.3.2 Prurigo nodularis
Prurigo nodularis, a typical pruritic disease characterized by appearance of itchy nodules or papules benefits from topical capsaicin therapy. In a double-blind, placebo-controlled study, 33 patients with prurigo nodularis were treated with varied doses of capsaicin cream 4 – 6 times daily for 2 weeks up to 10 months, and a complete remission was observed in all patients within 12 days. Sixteen out of 33 patients observed recurrence of pruritus within 2 months of completing treatment Citation[99].
8.3.3.3 Other dermatological indications
Topical capsaicin reduces not only the severity of pruritus in psoriasis but also reduced scaling and erythema, possibly improving the overall progression of this disease Citation[100,101], presumably due to its synergistic anti-inflammatory effects. We have also documented cases where capsaicin was effective in the treatment of refractory, painful lipodermatosclerosis and lobular panniculitis, in which other treatments failed Citation[102].
A recent randomized study of 50 patients compared the efficacy of capsaicin versus clobetasol in the treatment of alopecia areata and found that capsaicin was superior to the potent corticosteroid, although the differences were not statistically significant. It is postulated that capsaicin works by blocking the inhibition of hair growth Citation[26].
8.3.4 Miscellaneous forms of itch
Topical capsaicin is also successful in the relief of idiopathic itch (pruritus sine materia) Citation[103] in the alleviation of localized itch (e.g., perianal pruritus, vulvar vestibulitis) Citation[104,105] and of aquagenic pruritus Citation[106].
8.4. Placebo effect, blinding and compliance issues
8.4.1 The difficulty of “blinding” participants in controlled studies
In general, the therapeutic value of capsaicin in neuropathic itch and pain was considered difficult to evaluate since controlled capsaicin trials versus placebo are difficult to impossible to blind owing to the typical intense burning and stinging sensation elicited by capsaicin Citation[2]. An interesting solution was used in Phase II and III trials testing the efficacy of high-concentration NGX-4010 (trans-capsaicin dermal patches 8%), whereby, instead of placebo, a positive control of 0.04% capsaicin formulation (patch) was used to ensure ‘blinding’ Citation[58,84]. Previously, a high placebo response rate (17 – 48%) was reported in several controlled trials and, paradoxically, the placebo may induce a better response than capsaicin in isolated cases (see Citation[2]).
8.4.2 Compliance issues
A low compliance rate is a serious drawback hampering the beneficial long-term action of topical capsaicin, since a high number of patients discontinue treatment because of the irritation, which is not easily tolerable. The documented withdrawal rates are approximately 30% or higher Citation[43,107-109]. The mixed results reported previously with capsaicin are basically due to an unfavorable ratio of irritation (‘burning’ sensation) to desensitization Citation[2]. New capsaicin derivatives with an improved desensitization-to-irritation ratio would be of higher clinical relevance. To overcome the initial burning sensation, pretreatment with local anesthetic EMLA (eutectic mixture of lidocaine and prilocaine) cream has been successfully used. EMLA reduced the burning sensation from capsaicin also attenuating heat hyperalgesia. EMLA-pretreated skin after 1 and 5 days of treatment displayed a significantly higher warmth sensation detection threshold Citation[110].
8.5 Recent studies
The recent FDA approval of high-concentration (8%) dermal patches indicates a revival in the use of capsaicin for pain therapy. A practical approach to increase the effectiveness of capsaicin is to use high doses (8 – 10%) following regional anesthesia Citation[111] or to deliver capsaicin via a single-application dermal patch – the NGX-4010 formulations (Qutenza), preceded by local anesthesia induced with lidocaine ointments Citation[58,84].
NGX-4010, a high-concentration (8%) synthetic trans-capsaicin dermal patch, was recently developed to treat patients with neuropathic pain. In a randomized, double-blind, multicenter, 12-week study testing the efficacy and safety of one application of Qutenza, patients with PHN received one 60-min application of (8%) capsaicin or a low-concentration control patch (0.04% capsaicin). Patients who received NGX-4010 had a significantly greater reduction of pain during weeks 2 – 8 and weeks 2 – 12 than did the patients who received the control patch. A ‘rapid and sustained’ pain relief in patients with postherpetic neuralgia was documented, the mean changes of pain scores reported being −29.6 versus −19.9% (positive control). No adverse events were associated with the treatment, except for local reactions at the site of application and those related to treatment-associated pain Citation[58,112].
In a related placebo-controlled, double-blind, multicenter trial, NGX-4010 was found effective in the treatment of painful HIV-associated distal sensory polyneuropathy (HIV-DSP). Participants with painful HIV-DSP received either NGX-4010 or a control (a low-concentration capsaicin patch). NGX-4010 or control was applied once to painful areas on the feet. A single 90-min application resulted in a mean pain reduction of 23% during weeks 2 – 12, compared with an 11% reduction for control. One-third of NGX-4010-treated patients reported 30% pain decrease from baseline compared with 18% for controls. The single NGX-4010 application was considered safe and provided at least 12 weeks of pain reduction in patients with HIV-DSP Citation[84]. These findings improved capsaicin's record, since the efficacy of 0.075% capsaicin in patients with HIV-associated distal symmetrical peripheral neuropathy (DSPN), studied earlier in a multicenter, controlled trial indicated that a 0.075% capsaicin cream was ineffective in relieving this type of neuropathic pain Citation[113].
9. Potential ethnic factors involved in the efficacy and mechanism of action of capsaicin
We have noticed for many years in our practice that African Americans seem not to respond well to topical capsaicin and neither do they complain of burning or stinging sensations. Examining the effect of capsaicin on thermal detection thresholds and skin blood flow, we recently confirmed that capsaicin 0.075% produced a limited hyperalgesia and neurogenic inflammation in African Americans, in sharp contrast with three other ethnic groups. Rating continuously the intensity of pain, burning and stinging intensity post-capsaicin, we found that African Americans displayed the lowest intensity ratings for pain, burning or stinging Citation[114]. Intriguingly, capsaicin did significantly increase the warmth detection threshold in African Americans, a sensation mediated via TRPV3 receptors, but significantly decreased this threshold in Hispanics, the latter being the only group reporting significant itching after capsaicin application, which could suggest an involvement of TRPV3 receptors in the modulation of itch.
10. Other biological actions and potential uses of capsaicin
Capsaicin has been proposed as a therapeutic agent in several other areas (e.g., prevention of aspiration pneumonia, etc.). It exerts several effects on lipid and carbohydrate metabolism and may have a positive role in weight control, decreasing the excess caloric intake in humans. Capsaicin provides protection against gastroduodenal ulcer in experimental models and it is bactericidal against Helicobacter pylori. The intravesical instillation of capsaicin solution is successfully used in the treatment of neurogenic hyperactive bladder disorder. TRPV1 antagonists have been suggested as cough-suppressing agents.
Capsaicin could have a potential role as an anticoagulant as it inhibits platelet aggregation and the activity of clotting factors VIIIc and IX in vitro Citation[115]. However, the overall effect on blood clotting in humans remains disputed.
Interestingly, capsaicin could exert an anticarcinogenic action Citation[116]. It seems that capsaicin's action may consist in blocking the metabolic activation of pro-carcinogens. A recent observation is that capsaicin can inhibit the growth of a number of transformed cell lines Citation[117]. Another mechanism proposed for capsaicin's antitumor activity is via induction of apoptosis Citation[118].
11. Adverse effects, toxicity and mutagenesis
11.1 Adverse effects
The most obvious adverse effects of capsaicin are the initial pain, itch, burning and stinging sensation and the erythema that arises from the neurogenic inflammation Citation[43,107]. Capsaicin also typically produces a hypersensitivity to heat stimuli and heat pain (thermal hyperalgesia). High-concentration dermal patches can also induce pain and itch (42 and 6% of cases, respectively) Citation[58,84,112]. Sweat and heat aggravate the burning sensation induced by capsaicin. The unpleasant sensations can be minimized by lidocaine administration or pretreatment with EMLA without compromising the desired long-term therapeutic effect (i.e., desensitization) Citation[110].
The possibility of respiratory symptoms (coughing and sneezing) has been raised Citation[119,120], which could be eliminated by bathing after the topical application Citation[121]. Capsaicin may induce airway congestion, coughing and shortness of breath in healthcare workers applying capsaicin cream (especially in asthmatics), who were therefore advised to wear masks or respirators. Capsaicin is hazardous in cases of direct skin or eye contact, ingestion or inhalation. Special care has to be given to application of capsaicin in the proximity of mucosal areas (especially eyes), in perianal and perigenital areas where irritation can be unbearable. Capsaicin is notably used as the active repellent agent in pepper spray, which represents a significant source of exposure in the field of law enforcement. Severe overexposure to pure capsaicin can result in death Citation[122-124]. Because of its documented neurotoxicity and intense hyperalgesic effects, agonists of TRPV1 with lower toxicity are intensively sought as better alternatives to capsaicin.
11.2 Mutagenesis
Since humans are broadly exposed to capsaicin (from diet) the possibilities that capsaicin could be mutagenic, tumorigenic or carcinogenic were exhaustively investigated and critically reviewed Citation[2]. There seems to be a consensus that capsaicin's liver metabolites may be the actual hazardous species Citation[125,126]; however, topical capsaicin is considered safe to use. Following long-term intravesical instillation of capsaicin, no premalignant or malignant changes were found Citation[127]. Capsaicin is not mutagenic unless it is metabolized in liver microsomes. Capsaicin metabolites are weak mutagens and only at high concentration. In regard to capsaicin's carcinogenetic potential, many studies have focused on this topic, but have yielded conflicting results.
12. Conclusion
Although pharmacological treatment for neuropathic pain and itch has improved over the last decade, many patients do not reach full analgesia from systemic therapies (such as tricyclical antidepressants, neuroleptics and opioids), which are marred by potentially serious adverse effects. Therefore, topical capsaicin, by targeting peripheral nerves, provides a local approach for the relief of pain and itch exerting a complementary therapeutic action through a sui generis mechanism. A current drawback is the low compliance rate for commercial over-the-counter preparations due to the high incidence of burning sensation elicited. Based on our experience, we recommend EMLA as a pretreatment to limit the occurrence of burning sensation and pain.
13. Expert opinion
The recently FDA-approved, high-concentration dermal patches showed an increased therapeutic benefit over the low-concentration formulations, for relieving pain of neuropathic origin including PHN and notably HIV neuropathy, a condition where low-dose capsaicin was shown previously ineffective. In light of recent findings regarding ethnic differences in hyperalgesic and neurogenic inflammatory responses to capsaicin Citation[114], it would be of interest to examine whether there are functional gene polymorphisms in the TRPV1 genes affecting the response to this drug, which would enable assessment of which individuals would respond well to this therapy. New analogs of capsaicin, not inducing pain themselves but having potent analgesic and antipruritic effects, may further ignite the excitement for the therapeutic potential of this medicine, for the benefit of millions of patients with neuropathic pain and itch.
Declaration of interest
The authors state no conflict of interest and have received no payment in preparation of this manuscript.
Bibliography
- Spath E, Darling SF. Synthesis of capsaicin. Ber Chem Ges 1930;63B:737-40
- Szallasi A, Blumberg PM. Vanilloid (Capsaicin) receptors and mechanisms. Pharmacol Rev 1999;51:159-212
- Li D, Ren Y, Xu X, Sensitization of primary afferent nociceptors induced by intradermal capsaicin involves the peripheral release of calcitonin gene-related peptide driven by dorsal root reflexes. J Pain 2008;9:1155-68
- Gamse R, Petsche U, Lembeck F, Jancso G. Capsaicin applied to the peripheral nerve inhibits axoplasmic transport of substance P and somatostatin. Brain Res 1982;238:447-62
- Miller MS, Buck SH, Sipes IG, Regulation of substance P by nerve growth factor: disruption by capsaicin. Brain Res 1982;250:193-6
- Taylor DCM, Pierau Fr-K, Szolcsanyi J. Long-lasting inhibition of horseradish peroxidase (HRP) transport in sensory nerves induced by capsaicin pretreatment of the receptive field. Brain Res 1984;298:45-9
- Gilchrist CA, Morrison CF, Chapman KE, Harmar AJ. Identification of nerve growth factor-responsive sequences within the 5′ region of the bovine preprotachy-kiningene. DNA Cell Biol 1991;10:743-9
- Zhang H, Cang CL, Kawasaki Y, Neurokinin-1 receptor enhances TRPV1 activity in primary sensory neurons via PKC epsilon: a novel pathway for heat hyperalgesia. J Neurosci 2007;27:12067-77
- Vyklický L, Nováková-Tousová K, Benedikt J, Calcium dependent desensitization of vanilloid receptor TRPV1: a mechanism possibly involved in analgesia induced by topical application of capsaicin. Physiol Res 2008;57:S59-68
- Mohapatra DP, Nau C. Regulation of Ca2+-dependent desensitization in the vanilloid receptor TRPV1 by calcineurin and cAMP-dependent protein kinase. J Biol Chem 2005;280:13424-32
- Tominaga M, Numazaki M, Iida T, Regulation mechanisms of vanilloid receptors. Novartis Found Symp 2004;261:4-12; discussion 12-8,47-54
- Szallasi A, Blumberg PM. Vanilloid receptor loss in rat sensory neurons associated with long term desensitization to resiniferatoxin. Neurosci Lett 1992;136:51-4
- Nolano M, Simone DA, Wendelschafer-Crabb G, Topical capsaicin in humans: parallel loss of epidermal nerve fibers and pain sensation. Pain 1999;81:135-45
- Simone DA, Nolano M, Johnson T, Intradermal injection of capsaicin in humans produces degeneration and subsequent reinnervation of epidermal nerve fibers: correlation with sensory function. J Neurosci 1998;18:8947-59
- Nagy I, Sántha P, Jancsó G, Urbán L. The role of the vanilloid (capsaicin) receptor (TRPV1) in physiology and pathology. Eur J Pharmacol 2004;500:351-69
- Liu L, Simon SA. Capsaicin, acid and heat-evoked currents in rat trigeminal ganglion neurons: relationship to functional VR1 receptors. Physiol Behav 2000;69:363-78
- De Petrocellis L, Di Marzo V. Lipids as regulators of the activity of transient receptor potential type V1 (TRPV1) channels. Life Sci 2005;77:1651-66
- Dhaka A, Uzzell V, Dubin AE, TRPV1 is activated by both acidic and basic pH. J Neurosci 2009;29:153-8
- Khairatkar-Joshi N, Szallasi A. TRPV1 antagonists: the challenges for therapeutic targeting. Trends Mol Med 2008;15:14-22
- Maggi CA, Borsini F, Santicioli P, Cutaneous lesions in capsaicin-treated rats. A trophic role of capsaicin-sensitive afferents? Naunyn-Schmiedeberg's Arch Pharmacol 1987;336:538-45
- Carrillo P, Camacho M, Manzo J, Cutaneous wounds produced by capsaicin treatment of newborn rats are due to trophic disturbances. Neurotoxicol Teratol 1998;20:75-81
- Gamse R, Holzer P, Lembeck P. Decrease of substance P in primary sensory neurons and impairment of neurogenic plasma extravasation by capsaicin. Br J Pharmacol 1980;68:207-13
- Gamse R, Molnar A, Lembeck F. Substance P release from spinal cord slices. Life Sci 1981;25:629-36
- Rossi R, Del Bianco E, Isolani D, Possible involvement of neuropeptidergic sensory nerves in alopecia areata. Neuroreport 1997;8:1135-8
- Hordinsky M, Ericson M. Autoimmunity: alopecia areata. J Investig Dermatol Symp Proc 2004;9:73-8
- Ehsani A, Toosi S, Seirafi H, Capsaicin vs. clobetasol for the treatment of localized alopecia areata. J Eur Acad Dermatol Venereol 2009;23(12):1451-3
- Paus R, Heinzelmann T, Schultz KD, Hair growth induction by substance P. Lab Invest 1994;71:134-40
- Roberts LA, Connor M. TRPV1 antagonists as a potential treatment for hyperalgesia. Recent Pat CNS Drug Discov 2006;1:65-76
- Willis WD Jr. The role of TRPV1 receptors in pain evoked by noxious thermal and chemical stimuli. Exp Brain Res 2009;196:5-11
- Knotkova H, Pappagallo M, Szallasi A. Capsaicin (TRPV1 agonist) therapy for pain relief: farewell or revival? Clin J Pain 2008;24:142-54
- Lambert DG. Capsaicin receptor antagonists: a promising new addition to the pain clinic. Br J Anaesth 2009;102:153-5
- Gavva NR. Body-temperature maintenance as the predominant function of the vanilloid receptor TRPV1. Trends Pharmacol Sci 2008;29:550-7
- Leung FW. Capsaicin-sensitive intestinal mucosal afferent mechanism and body fat distribution. Life Sci 2008;83:1-5
- Geppetti P, Materazzi S, Nicoletti P. The transient receptor potential vanilloid 1: role in airway inflammation and disease. Eur J Pharmacol 2006;533:207-14
- Takemura M, Quarcoo D, Niimi A, Is TRPV1 a useful target in respiratory diseases? Pulm Pharmacol Ther 2008;21:833-9
- Hu CP, Li NS, Peng J, Involvement of vanilloid receptors in heat stress-induced delayed protection against myocardial ischemia-reperfusion injury. Neuropeptides 2003;37:233-8
- Hu CP, Li NS, Xiao L, Involvement of capsaicin-sensitive sensory nerves in cardioprotection of rutaecarpine in rats. Regul Pept 2003;114:45-9
- Nozawa Y, Nishihara K, Yamamoto A, Distribution and characterization of vanilloid receptors in the rat stomach. Neurosci Lett 2001;309:33-6
- Wang L, Wang DH. TRPV1 gene knockout impairs postischemic recovery in isolated perfused heart in mice. Circulation 2005;112:3617-23
- Babbar S, Marier JF, Mouksassi MS, Pharmacokinetic analysis of capsaicin after topical administration of a high-concentration capsaicin patch to patients with peripheral neuropathic pain. Ther Drug Monit 2009;31:502-10
- Fang J-Y, Wu P-C, Huang YB, Tsai YH. In vitro permeation study of capsaicin and its synthetic derivatives from ointment bases using various skin types. Int J Pharm 1995;126:119-28
- Chanda S, Bashir M, Babbar S, In vitro hepatic and skin metabolism of capsaicin. Drug Metab Dispos 2008;36:670-5
- Carter RB. Topical capsaicin in the treatment of cutaneous disorders. Drug Dev Res 1991;22:109-23
- Hergenhahn M, Adolf W, Hecker E. Resiniferatoxin and other esters of novel polyfunctional diterpenes from Euphorbia resinifera and unispina. Tetrahedron Lett 1975;19:1595-8
- De Vries DJ, Blumberg PM. Thermoregulatory effects of resiniferatoxin in the mouse: comparison with capsaicin. Life Sci 1989;44:711-15
- Szallasi A, Blumberg PM. Minireview. Resiniferatoxin and analogs provide novel insights into the pharmacology of the vanilloid (capsaicin) receptor. Life Sci 1990;47:1399-408
- Szallasi A, Blumberg PM. Specific binding of resiniferatoxin, an ultrapotent capsaicin analog, by dorsal root ganglion membranes. Brain Res 1990;524:106-11
- Szallasi A, Blumberg PM. [3H]Resiniferatoxin binding by the vanilloid receptor: species-related differences, effects of temperature and sulfhydryl reagents. Naunyn Schmiedeberg's Arch Pharmacol 1993;347:84-91
- Deng PY, Ye F, Cai WJ, Stimulation of calcitonin gene-related peptide synthesis and release: mechanisms for a novel antihypertensive drug, rutaecarpine. J Hypertens 2004;22:1819-29
- Hu CP, Xiao L, Deng HW, Li YJ. The cardioprotection of rutaecarpine is mediated by endogenous calcitonin related-gene peptide through activation of vanilloid receptors in guinea-pig hearts. Planta Med 2002;68:705-9
- Santos ARS, Calixto JB. Antinociceptive actions of tachykinin and capsaicin antagonists on neurogenic pain induced by formalin and capsaicin in mice. In: Abstracts of Tachykinins 1995: From Basic Science to Clinical Applications. Fondazione Internazionale Menarini, Florence, Italy; 1995. p. 163
- Progress in pain research and management. In: Jensen TS, editor. Proceedings of the 8th world congress on pain. (Volume 8); 17-22 August. Turner and Zsuzsanna Wiesenfeld-Hallin, IASP Press, Vancouver, BC, Canada; 1997
- Szallasi A, Cortright DN, Blum CA, Eid SR. The vanilloid receptor TRPV1: 10 years from channel cloning to antagonist proof-of-concept. Nat Rev Drug Discov 2007;6:357-72
- Jancso G, Ambrus A. Capsaicin sensitivity of primary sensory neurones and its regulation. In: Besson JM, Guilbaud G, Ollat H, editors, Peripheral neurons in nociception: physio-pharmacological aspects. John Libbey Eurotext, Paris; 1994. p. 71-87
- Cortright DN, Szallasi A. TRP channels and pain. Curr Pharm Des 2009;15:1736-49
- Oaklander AL. The density of remaining nerve endings in human skin with and without postherpetic neuralgia after shingles. Pain 2001;92:139-45
- Binder A, Koroschetz J, Baron R. Disease mechanisms in neuropathic itch. Nat Clin Pract Neurol 2008;4:329-37
- Backonja M, Wallace MS, Blonsky ER, NGX-4010 C116 Study Group. NGX-4010, a high-concentration capsaicin patch, for the treatment of postherpetic neuralgia: a randomised, double-blind study. Lancet Neurol 2008;7:1106-12
- Turnbull A. Tincture of capsaicin as a remedy for chilblains and toothache. Dublin Free Press 1850;1:95-6
- Ohkubo T, Kitamura K. Eugenol activates Ca-permeable currents in rat dorsal root ganglion cells. J Dent Res 1997;76:1737-44
- Ohkubo T, Shibata M. The selective capsaicin antagonist capsazepine abolishes the antinociceptive action of eugenol and guaiacol. J Dent Res 1997;76:848-51
- Vickers ER, Cousins MJ, Walker S, Chisholm K. Analysis of 50 patients with atypical odontalgia. A preliminary report on pharmacological procedures for diagnosis and treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1998;85:24-32
- Huang W, Rothe MJ, Grant-Kels JM. The burning mouth syndrome. J Am Acad Dermatol 1996;34:91-8
- LaCroix JS, Buvelot JM, Bolla BS, Lundberg JM. Improvement of symptoms of non-allergic chronic rhinitis by local treatment with capsaicin. Clin Exp Allergy 1991;21:595-600
- Marabini S, Ciabatti PG, Polli G, Beneficial effects of intranasal applications of capsaicin in patients with vasomotor rhinitis. Eur Arch Otorhinolaryngol 1991;248:191-4
- Filiaci F, Zambetti G, Ciofalo A, A local treatment of aspecific nasal hyperreactivity with capsaicin. Allergol Immunopathol 1994;22:264-8
- Filiaci F, Zambetti G, LuceMand Ciofalo A. Local treatment of nasal polyposis with capsaicin: preliminary findings. Allergol Immunopathol 1996;24:13-8
- Sicuteri F, Fusco BM, Marabini S, Beneficial effect of capsaicin application to the nasal mucosa in cluster headache. Clin J Pain 1989;5:49-53
- Fusco BM, Geppetti P, Fanciullacci M, Sicuteri F. Local application of capsaicin for the treatment of cluster headache and idiopathic trigeminal neuralgia. Cephalalgia 1991;11:234-5
- Marks DR, Rapoport A, Padla D, A double-blind, placebo-controlled trial of intranasal capsaicin for cluster headache. Cephalalgia 1993;13:114-6
- Stjärne P, Lundblad L, änggård A, Lundberg JM. Local capsaicin treatment of the nasal mucosa reduces symptoms in patients with nonallergic nasal hyperreactivity. Am J Rhinol 1991;5:145-51
- Holzer P. Local effector functions of capsaicin-sensitive sensory nerve endings: involvement of tachykinins, calcitonin gene-related peptide and other neuropeptides. Neuroscience 1988;24:739-68
- Szolcsányi J, Pintér E, Helyes Z, Systemic anti-inflammatory effect induced by counter-irritation through a local release of somatostatin from nociceptors. Br J Pharmacol 1998;125:916-22
- Bernstein JE, Bickers DR, Dahl MV, Roshal JY. Treatment of chronic postherpetic neuralgia with topical capsaicin. J Am Acad Dermatol 1987;17:93-6
- Bucci FA, Gabriels CF, Krohel GB. Succesful treatment of postherpeticneuralgia with capsaicin. Am J Ophthalmol 1988;106:758-9
- Oaklander AL. Mechanisms of pain and itch caused by herpes zoster (shingles). J Pain 2008;9(1 Suppl 1):S10-18
- Watson CP, Oaklander AL. Postherpetic neuralgia. Pain Pract 2002;2:295-307
- Ross DR, Varipapa RJ. Treatment of diabetic neuropathy with topical capsaicin. N Engl J Med 1989;321:474-5
- Basha KM, Whitehouse FW. Capsaicin: a therapeutic option for painful diabetic polyneuropathy. Henry Ford Hosp Med J 1991;39:138-40
- Watson CPN, Evans RJ. The postmastectomy pain syndrome and topical capsaicin: a randomized trial. Pain 1992;51:375-9
- Watson CPN, Evans RJ, Watt VR. The postmastectomy pain syndrome and the effect of topical capsaicin. Pain 1989;38:177-86
- Deal CL, Schnitzer TJ, Lipstein E, Treatment of arthritis with topical capsaicin: a double-blind trial. Clinic Ther 1991;13:383-95
- Matucci-Cerinic M, McCarthy G, Lombardi A, Editorial. Neurogenic influences in arthritis: potential modification by capsaicin. J Rheumatol 1995;22:1447-9
- Simpson DM, Brown S, Tobias J. NGX-4010 C107 Study Group. Controlled trial of high-concentration capsaicin patch for treatment of painful HIV neuropathy. Neurology 2008;70:2305-13
- Ellison N, Loprinzi CL, Kugler J, Phase III placebo-controlled trial of capsaicin cream in the management of surgical neuropathic pain in cancer patients. J Clin Oncol 1997;15:2974-80
- McCarty GM, McCarty DJ. Effect of topical capsaicin in the therapy of painful osteoarthritis of the hands. J Rheumatol 1992;19:604-7
- Schmelz M. Itch and pain. Neurosci Biobehav Rev 2010;34:171-6
- Handwerker HO, Schmelz M. Pain: itch without pain – a labeled line for itch sensation? Nat Rev Neurol 2009;5:640-1
- Sikand P, Shimada SE, Green BG, LaMotte RH. Similar itch and nociceptive sensations evoked by punctuate cutaneous application of capsaicin, histamine and cowhage. Pain 2009;144:66-75
- Simone DA, Zhang X, Li J, Comparison of responses of primate spinothalamic tract neurons to pruritic and algogenic stimuli. J Neurophysiol 2004;91:213-22
- Yosipovitch G, Greaves MW, Fleischer AB Jr, McGlone F (eds). Neuropathic pruritus in “Itch. Basic Mechanism and Therapy”. New York, Marcel Dekker, 2004;231-9
- Yosipovitch G, Samuel LS. Neuropathic and psychogenic itch. Dermatol Ther 2008;21:32-41
- Wallengren J. Treatment of notalgia paresthetica with topical capsaicin. J Am Acad Dermatol 1991;24:286-8
- Leibsohn E. Treatment of notalgia paresthetica with capsaicin. Cutis 1992;49:335-6
- Wallengren J, Klinker M. Successful treatment of notalgia paresthetica with topical capsaicin: vehicle-controlled, double-blind, crossover study. J Am Acad Dermatol 1995;32:287-9
- Tarng D-C, Cho Y-L, Liu H-N, Huang T-P. Hemodialysis-related pruritus: a double-blind, placebo-controlled, crossover study of capsaicin 0.025% cream. Nephron 1996;72:617-22
- Breneman DL, Cardone JS, Blumsack RF, Topical capsaicin for treatment of hemodialysis-related pruritus. J Am Acad Dermatol 1992;26:91-4
- Kantor GR, Resnik KS. Treatment of lichen simplex chronicus with topical capsaicin cream. Acta Derm Venereol (Stockh) 1996;76:161
- Stander S, Luger T, Metze D. Treatment of prurigo nodularis with topical capsaicin. J Am Acad Dermatol 2001;44:471-8
- Bernstein JE. Capsaicin in dermatologic diseases. Semin Dermatol 1988;7:304-9
- Ellis CN, Berberian B, Sulica VI, A double-blind evaluation of topical capsaicin in pruritic psoriasis. J Am Acad Dermatol 1993;29:438-42
- Yosipovitch G, Mengesha Y, Facliaru D, David M. Topical capsaicin for the treatment of acute lipodermatosclerosis and lobular panniculitis. J Dermatolog Treat 2005;16:178-80
- Tuerk MJ, Koo J. A practical review and update on the management of pruritus sine materia. Cutis 2008;82:187-94
- Lysy J, Sistiery-Ittah M, Israelit Y, Topical capsaicin - a novel and effective treatment for idiopathic intractable pruritus ani: a randomised, placebo controlled, crossover study. Gut 2003;52:1323-6
- Steinberg AC, Oyama IA, Rejba AE, Capsaicin for the treatment of vulvar vestibulitis. Am J Obstet Gynecol 2005;192:1549-53
- Lotti T, Teofoli P, Tsampau D. Treatment of aquagenic pruritus with topical capsaicin cream. J Am Acad Dermatol 1994;30:232-5
- Rumsfield JA, West DP. Topical capsaicin in dermatologic and peripheral pain disorders. DIPC Ann Pharmacother 1991;25:381-7
- Watson CPN. Topical capsaicin as an adjuvant analgesic. J Pain Symptom Manag 1994;9:425-33
- Rains C, Bryson HM. Topical capsaicin. A review of its pharmacological properties and therapeutic potential in post-herpetic neuralgia, diabetic neuropathy and osteoarthritis. Drugs Aging 1995;7:317-28
- Yosipovitch G, Maibach HI, Rowbotham MC. Effect of EMLA pre-treatment on capsaicin-induced burning and hyperalgesia. Acta Derm Venereol 1999;79:118-21
- Robbins WR, Staats PS, Levine J, Treatment of intractable pain with topical large-dose capsaicin: preliminary report. Anesth Analg 1998;86:579-83
- Noto C, Pappagallo M, Szallasi A. NGX-4010, a high-concentration capsaicin dermal patch for lasting relief of peripheral neuropathic pain. Curr Opin Investig Drugs 2009;10:702-10
- Paice JA, Ferrans CE, Lashley FR, Topical capsaicin in the management of HIV-associated peripheral neuropathy. J Pain Symptom Manage 2000;19:45-52
- Wang H, Papoiu AD, Coghill RC, Ethnic differences in pain, itch and thermal detection in response to topical capsaicin: African Americans display a notably limited hyperalgesia and neurogenic inflammation. Br J Dermatol 2010. [Epub ahead of print]
- Murray JA, Ahujaa KD, Geraghtya DP. Effect of capsaicin and dihydrocapsaicin on in vitro blood coagulation and platelet aggregation. Thromb Res 2009;124:721-3
- Miller CH, Zhang Z, Hamilton SM, Teel RW. Effects of capsaicin on liver microsomal metabolism of the tobacco-specific nitrosamine NNK. Cancer Lett 1993;75:45-52
- Morré DJ, Chueh PJ, Morré DM. Capsaicin inhibits preferentially the NADH oxidase and growth of transformed cells in culture. Proc Natl Acad Sci USA 1995;92:1831-5
- Mori A, Lehmann S, O'Kelly J, Capsaicin, a component of red peppers, inhibits the growth of androgen-independent, p-53 mutant prostate cancer cells. Cancer Res 2006;66:3222-29
- Scheffler NM, Sheitel PL, Lipton MN. Treatment of painful diabetic neuropathy with capsaicin. J Am Podiatr Med Assoc 1991;81:288-93
- Ellis JL, Sham JSK, Undem BJ. Tachykinin-independent effects of capsaicin on smooth muscle in human isolated bronchi. Am J Respir Crit Care Med 1997;155:751-5
- Marciniak BH, Brown B, Peterson B, Adverse consequences of capsaicin exposure in health care workers. J Am Geriatr Soc 1995;43:1181-2
- Olajos E, Salem H. Riot control agents: pharmacology, toxicology, biochemistry and chemistry. J Appl Toxicol 2001;21:355-91
- Busker RW, van Helden HP. Toxicologic evaluation of pepper spray as a possible weapon for the Dutch police force: risk assessment and efficacy. Am J Forensic Med Pathol 1998;19:309-16
- Capsaicin MSDS, Sciencelab.com, Inc. Houston, Texas. Available from: http://www.sciencelab.com/xMSDS-Capsaicin_Natural-9923296
- Surh Y-J, Lee SS. Capsaicin, a double-edged sword: toxicity, metabolism, and chemopreventive potential. Life Sci 1995;56:1845-55
- Surh Y-J, Lee SS. Capsaicin in hot chili pepper: carcinogen, co-carcinogen or anticarcinogen? Food Chem Toxicol 1996;34:313-16
- Dasgupta P, Chandiramani V, Parkinson MC, Treating the human bladder with capsaicin: Is it safe? Eur J Urol 1998;33:28-31
- Dubois JM. Capsaicin blocks one class of K1 channels in the frog node of Ranvier. Brain Res 1982;245:372-5
- Petersen M, LaMotte RH. Effects of protons on the inward current evoked by capsaicin in isolated dorsal root ganglion cells. Pain 1993;54:37-42
- Kehl SJ. Block by capsaicin of voltage-gated K1 currents in melanotrophs of the rat pituitary. Br J Pharmacol 1994;112:616-24
- Kuenzi FM, Dale N. Effect of capsaicin and analogues on potassium and calcium currents in Xenoupus embryo spinal neurones. Br J Pharmacol 1996;119:81-90
- Shimomura Y, Kawada T, Suzuki M. Capsaicin and its analogs inhibit the activity of NADH-Coenzyme Q oxidoreductase of the mitochondrial respiratory chain. Arch Biochem Biophys 1989;270:573-7
- Meddings JB, Hogaboam CM, Tran K, Capsaicin effects on non-neuronal plasma membrane. Biochim Biophys Acta 1991;1070:43-50
- Aranda F, VillalaIn J, Gomez-Fernandez JC. Capsaicin affects the structure and phase organization of phospholipid membranes. Biochim Biophys Acta 1995;1234:225-34
- Hogaboam CM, Wallace JL. Inhibition of platelet aggregation by capsaicin. An effect unrelated to actions on sensory afferent neurons. Eur J Pharmacol 1991;202:129-31
- Cochereau C, Sanchez D, Bourhaoui A, Creppy EE. Capsaicin, a structural analog of tyrosine, inhibits the aminoacylation of tRNA(Tyr). Toxicol Appl Pharmacol 1996;141:133-7
- Cochereau C, Sanchez D, Creppy EE. Tyrosine prevents capsaicin-induced protein synthesis inhibition in cultured cells. Toxicology 1997;117:133-9
- Ritter S, Dinh TT. Capsaicin-induced degeneration in rat brain and retina. In: Wood JN, editor, Capsaicin in the study of pain. Academic Press, San Diego, CA; 1993. p. 105-38
- Morgenlander JC, Hurwitz BJ, Massey EW. Capsaicin for the treatment of pain in Guillain-Barré syndrome. Ann Neurol 1990;28:199
- Kroenke K, Krebs EE, Bair MJ. Pharmacotherapy of chronic pain: a synthesis of recommendations from systematic reviews. Gen Hosp Psychiatry 2009;31:206-19
- Rayner HC, Atkins RC, Westerman RA. Relief of local stump pain by capsaicin cream. Lancet 1989;2:1276-7
- Weintraub M, Golik A, Rubio A. Capsaicin for treatment of post-traumatic amputation stump pain. Lancet 1990;336:1003-4