Abstract
Despite recent improvements in the diagnosis and treatment of cryptococcosis, cryptococcal meningitis is responsible for > 600,000 deaths/year worldwide. The aim of this work is to provide an update on the developments in its epidemiology and management. Understanding the pathogenesis of Cryptococcus has improved, and new insights for the virulence of the fungus and the host response have enabled scientists to design new ways to confront this infection. Additionally, invertebrate model hosts have greatly facilitated the research in this field. Importantly, the epidemiology of Cryptococcus gattii has continued to evolve, and the emergence of this highly virulent species in immunocompetent populations, especially in Northwestern America and British Columbia, warrants increased awareness because delayed diagnosis and inappropriate antifungal therapy is associated with high mortality. Diagnosis remains a challenge, but new techniques for early and inexpensive identification of the pathogen are under development. Management can vary, based on the patient population (HIV-seropositive, organ transplant recipients or non-transplant/non-HIV). In most patients, amphotericin B with flucytosine continues to be the most appropriate induction therapy. However, in organ transplant recipients the use of liposomal amphotericin B improves mortality compared with deoxycholate amphotericin B. Also, the combination of amphotericin B with fluconazole seems to be a reasonable alternative, while fluconazole with flucytosine is superior to fluconazole monotherapy.
1. Introduction
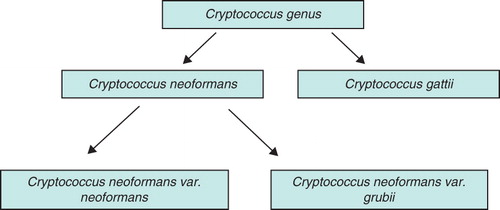
Cryptococcus is a pathogenic, encapsulated yeast, that mainly infects the central nervous system (CNS). The global burden of cryptococcal infection is high, especially in developing countries, and in 2007 the estimated number of deaths attributed to cryptococcal meningitis was 624 – 700 Citation[1]. In North America mortality is ∼ 9 – 20%, whereas in sub-Saharan Africa it can reach ≥ 70% () Citation[1]. Amongst numerous species of Cryptococcus, only a few can infect humans. Notable examples include Cryptococcus neoformans var. grubii and Cryptococcus neoformans var. neoformans, which more commonly infect immunocompromised patients, and Cryptococcus gattii, which affects immunocompetent and immunocompromised individuals, including patients with mild immune suppression (). In this review, we describe new research developments and therapeutic advances for cryptococcal meningitis and update our last review, which was published in this journal in 2007 Citation[2].
Figure 1. Burden of cryptococcal meningitis in North America compared to Sub-Saharan Africa Citation[1]
![Figure 1. Burden of cryptococcal meningitis in North America compared to Sub-Saharan Africa Citation[1]](/cms/asset/55d1a128-5986-409d-b5a1-dfef4f9ed7a3/ieop_a_658773_f0001_b.jpg)
2. Pathogenesis and virulence factors
The respiratory tract serves as a niche from which cryptococcal cells subsequently spread to the CNS through hematogenous seeding. More specifically, the pathophysiology of cryptococcal meningitis entails the inhalation of aerosolized C. neoformans (basidiospores) causing an often subclinical pneumonitis. Subsequently, fungal cells disseminate to the CNS causing meningoencephalitis. Cryptococcal invasion is mediated through multiple virulence factors, the most important of which are melanin, the polysaccharide capsule and the ability to grow at mammalian temperatures Citation[3].
Over the last 4 years, researchers have made a series of discoveries regarding cryptococcal virulence. De Jesus et al. studied the role of three essential components of the cryptococcal polysaccharide capsule and showed that galactoxylomannan (Ga1XM) is an essential capsule constituent, while mannoprotein and Ga1XM aid in the transportation to the extracellular space Citation[4]. Interestingly, Ga1XM has important immunomodulatory activities and researchers are now exploiting them for the development of a cryptococcal vaccine Citation[5].
Another important study demonstrated the importance of the myo-inositol transporter gene family in the virulence of C. neoformans and C. gattii. Single-gene deletion mutants of C. neoformans lacking the inositol 1-phosphate synthase gene INO1 were less virulent than the wild-type in a mouse infection model of cryptococcosis Citation[6]. Importantly, inositol, which is an abundant CNS substance, serves as an important carbon source for Cryptococcus, a finding that could partially explain the predilection of Cryptococcus for the CNS. An additional substance that is also found in the CNS is L-3, 4-dihydroxyphenylalanine (L-DOPA). L-DOPA is used as a precursor for the synthesis of melanin from Cryptococcus, a critical virulence factor. In a recent study, L-DOPA supplementation boosted cryptococcal melanin production and induced the transcription of various stress genes Citation[7].
Over the last years, the study of cryptococcal virulence has been aided by the study of evolutionarily preserved virulence factors and host responses in invertebrate model hosts such as Acathamoeba castellanii, Caenorhabditis elegans, Dictyostelium discoideum, Drosophila melanogaster and Galleria mellonella (reviewed in Citation[8]). Interestingly, there are extensive similarities between the pathogenesis in mammalian and invertebrate cryptococcal infection. In addition to the help of the C. elegans model on the study of cryptococcal virulence, it also contributes to the study of host responses to cryptococcosis. For example, researchers found that mammalian scavenger receptors like the CD36 and SAF1 (homologues to the C. elegans C03F11.3 and CED-1 receptors) are important for the ability of the nematode to survive cryptococcal infection. Subsequent analysis of the CD36 and SAF1 in mammalian models of infection, demonstrated that these receptors are involved in β-D-glucan binding Citation[9].
The reader is referred to the reports from the two recent international conferences on ‘Cryptococcus and cryptococcosis’ that took place in 2007 and 2011 in Nagasaki, Japan, and Charleston, USA, respectively, which outline the recent progress in cryptococcal pathogenesis.
3. Cryptococcus gattii as an emerging fungal pathogen
Substantial developments have been made on the study of the pathogenesis of C. gattii. Cryptococcus gattii is divided in to four molecular types (VGI – VGIV) Citation[10]. In our previous review, we discussed the outbreak of C. gattii disease in Vancouver Island, British Columbia, Canada Citation[11]. Since then, C. gattii has been spreading widely Citation[12]. Over the last decade, the VGI and VGII subtypes have caused infections in California (VGI) as well as Canada (VGII) and Pacific Northwest USA(VGII) Citation[10]. From 2004 to 2010, seventy cases of C. gattii cryptococcosis from the Pacific Northwest USA were reported to the Center for Disease Control and Prevention (CDC) Citation[13]. Among these 70 cases, 45 had reported outcomes and mortality was 20% Citation[13]. From the different genotypes of the VGII molecular type, two (VGIIa and VGIIc) are particularly virulent. VGIIa is associated with the Vancouver Island outbreak and in a murine model of cryptococcosis was found to be exceptionally virulent Citation[14]. Interestingly, the proposed mechanism for increased virulence is based on the highly tubular mitochondrial morphology that may protect the cell from mtDNA mutations and cell death Citation[15]. VGIIc is associated with cryptococcosis in Portland, Oregon, USA, and a study examining the virulence of VGIIc in a murine nasal inhalation killing assay showed that this new genotype is highly virulent and killed mice after 20.6 days on average, whereas the VGIIb strain, found in Australia and Vancouver Island, was less virulent, killing the mice after 46 days on average (p < 0.005) Citation[10].
4. Update on laboratory diagnosis and cryptococcal meningitis complications
Culture and India ink staining of cerebrospinal fluide (CSF) and cryptococcal polysaccharide antigen detection in the serum and CSF are the traditional diagnostic techniques for this infection. However, new and rapid diagnostic tests could reduce the expense of the treatment and the adverse drug effects associated with antifungal therapies. Lateral flow immunoassay (LFA) is a new and inexpensive diagnostic method of cryptococcosis, which shows comparable results to the widely approved enzyme immunoassay for cryptococcal antigen (EIA). Additional benefits of this assay include low cost and rapidity of results, which can offer an early therapeutic window. A possible LFA with the use of finger-stick blood could be a cheap and simple way to diagnose cryptococcosis in sub-Saharan Africa because the cost for a single test is less than $2.50 and requires minimal laboratory equipment. The LFA had a 90 – 96% agreement with the results of EIA when applied to sera of patients suffering from cryptococcosis Citation[16].
The differentiation between the C. neoformans and C. gattii species can be achieved with two different laboratory techniques; first, with the use of the inexpensive and commercially available canavanine glycine bromothymol blue (CGB) agar. The color of the agar changes to blue from green in the presence of C. gattii. A drawback to its use is the long time needed for a positive result (about 5 days). PCR can be also used for the identification of Cryptococcus species. PCR methods need specific molecular targets, are fast but also expensive and cannot be widely used from most labs. Unfortunately, although the agar is commercially available and some laboratories differentiate between the C. neoformans and C. gattii species, most do not.
A substantial portion of HIV-infected patients with cryptococcosis experience a transient paradoxical response with worsening of symptoms upon initiation of antiretroviral therapy, which is attributed to the immune reconstitution inflammatory syndrome (IRIS). IRIS is relatively common among HIV-infected patients with cryptococcosis, with an incidence of 8 – 50% Citation[17]. Patients with high concentrations of serum cryptococcal antigen are at increased risk for IRIS, while the timing of antiretroviral therapy does not seem to affect the incidence of IRIS according to a recent research work Citation[18].
Another complication of cryptococcal meningitis is a very high increase in intracranial pressure (ICP). In cryptococcal meningoencephalitis ICP should be kept ≤ 20 cm H2O by a daily therapeutic drainage of CSF. When indicated, high volume CSF drainage not only has a clear role in preventing neurological sequelae and also aids in the rapid clearance of the cryptococcal capsular polysaccharide antigen (CRAG), which has been shown to be a causative factor of the increased ICP Citation[19,20]. The results of an interesting research showed that to clear CRAG more effectively from the CSF high-volume CSF drainage (> 100 ml over 2 weeks) was superior to low-volume drainage (< 25 ml over 2 weeks; p = 0.05) Citation[20].
5. Management
According to the updated guidelines of the Infectious Disease Society of America (IDSA) published in 2010, patients are divided into three risk groups Citation[21]. The first includes HIV-infected patients, the second includes patients after organ transplantation and the third includes nontransplant/non-HIV patients (). This classification facilitates therapeutic decisions, since each group responds better to specific therapeutic strategies. For example, deoxycholate amphotericin B is still recommended for treating nontransplant/non-HIV patients. However, lipid formulations of amphotericin B, including liposomal and lipid complex amphotericin B, are recommended for solid organ transplant recipients, not only because these formulations reduce nephrotoxicity but also because they may improve survival in this patient population (). This change is based on research by Sun et al. that compared the activity of lipid formulations of amphotericin B to deoxycholate amphotericin B in patients who developed cryptococcal meningitis after solid organ transplantation. During the study, the mortality after 90 days was 10.9% in the group of patients treated with lipid formulation of amphotericin B and 40% in the group treated with deoxycholate amphotericin B (p = 0.007) Citation[22]. Nevertheless, lipid formulations of amphotericin B can be used instead of deoxycholate amphotericin B in the case of adverse effects during the therapy of any patient with cryptococcosis. Successful management of cryptococcosis requires an effective and prompt clearance of the CNS from the Cryptococcus, and induction therapy with amphotericin B and flucytosine is the best induction therapy in this regard.
Table 1. IDSA management guidelines Citation[21].
Table 2. Commonly used antifungal compounds and examples of important adverse effects.
Additionally, the new IDSA guidelines specifically focus on the management of C. gattii infection. Patients infected with C. gattii are more likely to present with symptoms due to inflammatory lesions in the brain or lung (cryptococcomas) and they are more prone to neurological symptoms such as cranial nerves palsies and seizures. As a result, prolonged therapy and surgical excision of the lesion are often necessary Citation[23,24]. Overall, the therapeutic plan is the same to that of C. neoformans infection. Therefore, although identification of the species is very helpful from the epidemiology standpoint, it is not needed for the management of cryptococcosis. Nevertheless, the guidelines highlight the need to monitor for complications of the disease, such as hydrocephalus. Notably, surgery is indicated as an option if medical therapy fails to control cryptococcomas.
In addition, the recent guidelines address the management plan in resource-limited areas. Depending on the availability of antifungal compounds, monotherapy with fluconazole, the combination of fluconazole with flucytosine or deoxycholate amphotericin B and monotherapy with deoxycholate amphotericin B are the available options. If available, amphotericin B is preferable to fluconazole for the induction therapy. A recent study compared the efficacy between amphotericin B plus flucytosine and amphotericin B plus fluconazole and showed no difference in the clearance rate of CSF from cryptococcal colony-forming units (CFU) between the two management groups. In detail, the first treatment group included 21 patients treated with amphotericin B (0.7 – 1 mg/kg/day) plus flucytosine (25 mg/kg 4 times/day) and the second included 22 patients treated with amphotericin B (0.7 – 1 mg/kg/day) plus fluconazole (800 mg/day; p = 0.6) Citation[25]. Of note is that the combination therapy of fluconazole with flucytosine is shown to be superior to fluconazole monotherapy in the clearance of Cryptococcus from the CSF Citation[26].
6. Expert opinion
Management of cryptococcal meningoencephalitis poses a triple challenge. First, clinicians should be able rapidly to categorize patients (as detailed in the IDSA guidelines) and administer appropriate antifungal treatment. Second, identification of the fungus to the species level has become clinically important as C. gattii infection, as noted above, is linked to a higher risk of cryptococcomas and more neurological sequelae. Although infection with C. gattii has similar management to C. neoformans, the presence of brain or lung cryptococcomas necessitates prolonged management and the length of induction therapy is not definitive. Third, clinicians should monitor immunocompromised and immunocompetent patients for the development of IRIS.
Regarding antifungal therapy in resource-limited areas, combination of deoxycholate amphotericin B with fluconazole is acceptable; however, fluconazole monotherapy is often the only option. Lipid formulations of amphotericin B are preferred in organ transplant recipients, but the relative efficacy of the different formulations in other patient populations has not been studied systematically. In particular, data on the efficacy of antifungal regiments among pregnant patients are limited. Amphotericin B is of minimal harm to the fetus and is safe to use during breastfeeding. However, fluconazole and flucytosine are contraindicated during pregnancy. Finally, initiation of antiretroviral therapy among HIV patients should not be significantly delayed for fear of the development of IRIS, and the IDSA guidelines suggest highly active antiretroviral therapy (HAART) initiation 2 – 10 weeks after the onset of cryptococcal treatment. Of note, antiretroviral-naive HIV patients have an increased risk for the development of IRIS and should be closely monitored.
Importantly, data demonstrate that C. gattii is spreading at an alarming rate. From the outbreak in British Columbia, Canada, in the late 1990s, cases have been reported in Seattle, Washington and Portland, Oregon, USAAt present, C. gattii is considered endemic in the Pacific Northwest region and C. gattii is expected to continue spreading across northwestern America; this expansion will be aided by human traveling and animal relocation. Therefore, public health services should be ready to inform local healthcare officials. In addition, intense genotyping of cryptococcal strains globally will aid in understanding the complex epidemiology of C. gattii.
In summary, the epidemiology of cryptococcal meningitis is changing by involving an increasing amount of immunocompetent individuals. Therefore, enhanced surveillance and more efficacious diagnostic techniques are needed. Management of cryptococcal meningitis remains a challenge and, even though mortality rates are decreasing in the developed world, resource-limited areas face a significant challenge because of unavailability of antifungal regiments. The development of inexpensive and more effective antifungal drugs, as well as cryptococcal vaccines, will probably decrease the global cryptococcal burden and improve mortality even more.
Declaration of interest
The authors declare no conflict of interest. This work was supported by the National Institutes of Health through an R21 award (AI070569) to E Mylonakis.
Bibliography
- Park BJ, Wannemuehler KA, Marston BJ, Estimation of the current global burden of cryptococcal meningitis among persons living with HIV/AIDS. AIDS 2009;23:525-30
- Pukkila-Worley R, Mylonakis E. Epidemiology and management of cryptococcal meningitis: developments and challenges. Expert Opin Pharmacother 2008;9:551-60
- Liu OW, Chun CD, Chow ED, Systematic genetic analysis of virulence in the human fungal pathogen Cryptococcus neoformans. Cell 2008;135:174-88
- De Jesus MD, Nicola AM, Chow SK, Glucuronoxylomannan, galactoxylomannan, and mannoprotein occupy spatially separate and discrete regions in the capsule of Cryptococcus neoformans. Virulence 2010;1:500-8
- Chow SK, Casadevall A. Evaluation of Cryptococcus neoformans galactoxylomannan-protein conjugate as vaccine candidate against murine cryptococcosis. Vaccine 2011;29:1891-8
- Xue C, Liu T, Chen L, Role of an expanded inositol transporter repertoire in Cryptococcus neoformans sexual reproduction and virulence. mBio 2010;1:e00084-10
- Eisenman HC, Chow SK, Tse KK, The effect of L-DOPA on Cryptococcus neoformans growth and gene expression. Virulence 2011;2:329-36
- Mylonakis E, Casadevall A, Ausubel FM. Exploiting amoeboid and non-vertebrate animal model systems to study the virulence of human pathogenic fungi. PLoS Pathog 2007;3:e101
- Means TK, Mylonakis E, Tampakakis E, Evolutionarily conserved recognition and innate immunity to fungal pathogens by the scavenger receptors SCARF1 and CD36. J Exp Med 2009;206:637-53
- Byrnes EJ III, Li W, Lewit Y, Emergence and pathogenicity of highly virulent Cryptococcus gattii genotypes in the northwest United States. PLoS Pathog 2010;6:e1000850
- Hoang LM, Maguire JA, Doyle P, Cryptococcus neoformans infections at Vancouver hospital and health sciences centre (1997 – 2002): epidemiology, microbiology and histopathology. J Med Microbiol 2004;53:935-40
- Byrnes EJ III, Marr KA. The outbreak of Cryptococcus gattii in western North America: epidemiology and clinical issues. Curr Infect Dis Rep 2011;13:256-61
- Centers for Disease Control and Prevention. Emergence of Cryptococcus gattii – Pacific Northwest, 2004 – 2010. MMWR Morb Mortal Wkly Rep 2010;59:865-8
- Fraser JA, Giles SS, Wenink EC, Same-sex mating and the origin of the Vancouver Island Cryptococcus gattii outbreak. Nature 2005;437:1360-4
- Ma H, Hagen F, Stekel DJ, The fatal fungal outbreak on Vancouver Island is characterized by enhanced intracellular parasitism driven by mitochondrial regulation. Proc Natl Acad Sci USA 2009;106:12980-5
- Lindsley MD, Mekha N, Baggett HC, Evaluation of a newly developed lateral flow immunoassay for the diagnosis of cryptococcosis. Clin Infect Dis 2011;53:321-5
- Shelburne SA III, Darcourt J, White AC Jr, The role of immune reconstitution inflammatory syndrome in AIDS-related Cryptococcus neoformans disease in the era of highly active antiretroviral therapy. Clin Infect Dis 2005;40:1049-52
- Sungkanuparph S, Filler SG, Chetchotisakd P, Cryptococcal immune reconstitution inflammatory syndrome after antiretroviral therapy in AIDS patients with cryptococcal meningitis: a prospective multicenter study. Clin Infect Dis 2009;49:931-4
- Bicanic T, Brouwer AE, Meintjes G, Relationship of cerebrospinal fluid pressure, fungal burden and outcome in patients with cryptococcal meningitis undergoing serial lumbar punctures. AIDS 2009;23:701-6
- Wijewardana I, Jarvis JN, Meintjes G, Large volume lumbar punctures in cryptococcal meningitis clear cryptococcal antigen as well as lowering pressure. J Infect 2011;63:484-6
- Perfect JR, Dismukes WE, Dromer F, Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the infectious diseases society of america. Clin Infect Dis 2010;50:291-322
- Sun HY, Alexander BD, Lortholary O, Lipid formulations of amphotericin B significantly improve outcome in solid organ transplant recipients with central nervous system cryptococcosis. Clin Infect Dis 2009;49:1721-8
- Byrnes EJ III, Bartlett KH, Perfect JR, Heitman J. Cryptococcus gattii: an emerging fungal pathogen infecting humans and animals. Microbes Infect 2011;13:895-907
- Lee YC, Wang JT, Sun HY, Chen YC. Comparisons of clinical features and mortality of cryptococcal meningitis between patients with and without human immunodeficiency virus infection. J Microbiol Immunol Infect 2011;44:338-45
- Loyse A, Wilson D, Meintjes G, Comparison of the early fungicidal activity of high-dose fluconazole, voriconazole, and flucytosine as second-line drugs given in combination with amphotericin B for the treatment of HIV-associated cryptococcal meningitis. Clin Infect Dis 2011; 54(1):121-8
- Nussbaum JC, Jackson A, Namarika D, Combination flucytosine and high-dose fluconazole compared with fluconazole monotherapy for the treatment of cryptococcal meningitis: a randomized trial in Malawi. Clin Infect Dis 2010;50:338-44