Abstract
More than 300 million individuals in industrialized countries suffer from allergic rhinitis. Rhinitis is a disease characterized by stuffy or runny nose, followed by red, itchy watering eyes and repeated sneezing. But more common problems for rhinitis patients are the overlooked social difficulties, with the majority reporting tiredness, feeling miserable or irritable. Often, medication is not able to adequately control symptoms and there is a need for other aids against the disease. Here, we describe the current situation after five trials using nasal filters in the remediation of seasonal allergic rhinitis.
The Allergic Rhinitis and its Impact on Asthma guidelines Citation[1] recommend a four-step process for treating allergic rhinitis. The first two steps are pharmacological interventions using nonsedating antihistamines and intranasal corticosteroids, although other approaches including leukotriene receptor antagonists and nasal decongestants are also recommended. The other two steps are patient education and prevention of exposure. In the case of exposure to airborne pollens, the most likely possibility is to stay indoors with closed windows at all times, which is not practical with most lifestyles. Additionally, 40% of people with rhinitis report that medications do not adequately control their symptoms Citation[2]. More than 50% of patients report trying ‘alternative therapies’, often without much success Citation[3]. Hence, the idea of a nasal filter seems to follow the logic of removing the main triggering event for symptoms.
The idea of filtering the air we inhale as a protection from health risks is not new. Ancient Greeks apparently used sponges for this purpose and medieval ‘plague doctors’ wore masks with hollow beak-shaped noses containing pungent plant materials to filter air and protect the wearer from the airborne miasma thought to spread diseases Citation[4].
Since the mid-19th century, various face masks containing either separate filters or themselves made of filtering cloth have been used to provide protection from inhaling gases, microbes and particles. The protective efficiency of these varies widely depending on the design of the mask and the nature of the material it is designed to protect against. Surgical masks were originally invented to prevent contamination of the surgical site by microbes expelled by the surgeon, but are now generally used for personal protection. However, the protection provided by surgical masks is relatively low compared with that of higher efficiency respirators (FFP2 in Europe, N95 in the USA), which provide >95% protection against approximately 0.3 µ particles, when tested on a rig though. In practice, this is not achieved due to leakage between the face and the edge of the mask. There are also number of hindrances with masks, ranging from mild hypercapnea from rebreathing the air in the dead space, overheating, rashes, resistance to breathing, interference with both verbal and nonverbal communications and the alteration to personal appearance and identity.
Of the three most important allergic diseases, asthma, rhinitis and eczema, rhinitis is the one where inhaled allergen exposure is most clearly related to immediate disease symptoms and, therefore, the most amenable to using personal allergen filtration as a protective approach. The conceptual idea of moving the filtration into the nose itself, particularly when acute exposures to large particles such as pollens are involved, has obvious appeal. Further filtering of the nasal airflow might have a beneficial effect on allergic rhino-conjunctivitis, due to the nasal–ocular reflex Citation[5].
Two early patents for nasal filters (US701538 in 1901 and UK28819 in 1905) demonstrate the principles of mechanical impingement/filtration and impaction that remain as features of many current designs. A search of the patent literature finds over 100 patents for nasal filters prior to 2000, suggesting many of the inventive steps are likely to already be prior art.
Despite the many attempts to provide practical solution to pollen exposure, there are no established or dominant brands of nasal filters on the market, and only a few publications deal with them. A Google search found more than a dozen brands currently for sale (Breathe-Ezy, Protection Plus, Air breathe, First defence, Nose Mask, Nosk, WoodyKnows, Healthnaso, BreathePure, Ultra Breathable, Respira, Sanispira, Inhalefresh, NasalAir Guard and Breathe Thru). With one exception, all these appear to involve mechanical filtration of the airstream (i.e., like a ‘tea-strainer’) using a fibrous or porous mesh.
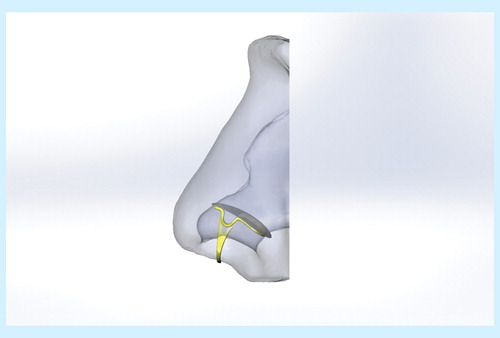
However, there are only a handful of papers describing nasal filters in the medical literature. These include those homemade from foam Citation[6], hand-made filters using a fine wire mesh Citation[7], impaction-based filters Citation[5], those with a spiral air path Citation[8] and those with a thin layer of filter material supported by a flexible frame fitting inside the nasal cavity Citation[9]. Clinical information is published for four; one of anecdotal experience Citation[7]; one of an open clinical study Citation[8]; and two of placebo-controlled, double-blind trials using either natural Citation[5] or laboratory pollen challenge Citation[9], see as an example of such a filter.
All these studies support the concept, although none show stellar performance. In the open clinical study Citation[8], the total Rhinoconjunctivitis Quality of Life Questionnaire symptoms scores over the day and night decreased significantly from 60 to 23 and 10, respectively, over 18 days; in the field study challenge Citation[5], the major complex of rhinitis symptoms increased by approximately half in the placebo group and decreased by half in the active group (difference p = 0.0076); while in the laboratory challenge study Citation[9], the mean daily but not maximum total nasal symptoms scores were reduced by 21% with active filter compared with placebo (p = 0.049). Most or all of the participants found the devices comfortable. Without more information, it is only possible to speculate that the less aesthetically acceptable filters Citation[5] provided greater protection because they sealed better in the nose; however, other issues such as the type, time, pattern and dose of exposure also differed. Both the challenge studies show the importance of rigorous evaluation of both the clinical aspects and user responses.
There are numerous constraints on the design of nasal filters. Ideally, to be discreet, they should be small enough to completely fit within the first portion of the nostrils (the nares). The interior shape of the nose is highly individual and is partly determined by age, sex and ethnicity. Nasal filters need to fit into an approximately tear-drop shaped space about 15–20 mm long by 6–10 mm wide, with a maximum height of around 10 mm. The cross-sectional area is about 1.5 cm2/nostril, depending on the individual. They also need to seal so that unfiltered air does not pass around them (this bypass occurs easily if the filters have some flow resistance and results in an erroneous perception that they are ‘easy to breathe through’), effectively filter out the airborne particles, have negligible airflow resistance to allow comfortable breathing and be safe. They need to be easy to manage, aesthetic and comfortable to wear.
Nasal filters have generally been advertised as providing protection against the allergens causing rhinitis, air pollutants and virus exposures, and they have also been used to study personal exposure by collecting exactly what people inhale Citation[10,11]. The size of particles carrying these allergens differs; most pollens causing rhinitis are roughly spherical and between 16 and 30 µm in diameter, whereas the size of particle carrying indoor allergens (mite, cockroach, cat and dog) varies depending on factors associated with dust disturbance. Under conditions of recent and high disturbance, most of these allergens are carried by ‘large’ particles or aggregates of particles, 10–40 µm in diameter, whereas after about 20 min or under less disturbed conditions, smaller particles carry most of the allergens. In particular, a considerable amount of cat and dog allergen is associated with small flakes <5 µm. In a house with a resident cat, this allergen can remain airborne for extended periods and can cause symptoms in a sensitive person even without dust disturbance. Similarly, in the absence of high local disturbance, most air pollutant particulates are smaller than 2–3 µm, whereas infectious particles are classified as being either >5 µm and <5 µm in diameter. This distribution of the size is important for filter design, as larger particles (>5 µm) are much easier to remove mechanically or by impaction than smaller particles, without introducing a penalty of higher air flow resistance.
Exposure to most aeroallergens is intermittent in time and variable in dose. The peak in exposure may only involve a short period, such as on a golf course, when symptom-free concentration is required; this is in contrast to the use of intranasal steroids that require repeated administration over days to be fully effective. Even if not recommended by current guidelines Citation[1], nasal filters may have a novel adjunct role in situations of high acute exposures where medications are insufficient, produce side effects or have a delayed onset of action.
The opportunities for developing better health products are only limited by available technology and imagination. Certainly, rhinitis and air pollution provide a massive and global market where there is considerable dissatisfaction with current pharmaceutical approaches and the use of face masks. The removal of relatively large airborne particles from a typical inhaled airstream with an acceptable increase in nasal air flow resistance is not technically difficult. However, there remain considerable and multiple restraints in addressing the issues of individual variation among people which affects sizing, sealing and comfort in the nose. With recent advances in 3D scanning and the availability of 3D printing using soft and human-safe materials, there now appears to be an opportunity to make novel custom-fit nasal filters, which are specifically made to the shape of the individual nasal cavity. This could be a translational and innovative outcome integrating the fields of design, medicine and biomedical engineering and have a profound impact on how rhinitis would be managed in future.
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
Notes
References
- Brozek JL, Bousquet J, Baena-Cagnani CE, et al. Allergic rhinitis and its impact on asthma (ARIA) guidelines: 2010 revision. J Allergy Clin Immunol 2010;126(3):466-76
- Mullol J, Bartra J, Del CA, et al. Specialist-based treatment reduces the severity of allergic rhinitis. Clin Exp Allergy 2013;43(7):723-9
- Storms WW. Treatment of allergic rhinitis: effects of allergic rhinitis and antihistamines on performance. Allergy Asthma Proc 1997;18(2):59-61
- Miklós V. An illustrated history of gas masks. Available from: http://io9.com/an-illustrated-history-of-gas-masks-504296785 [Last accessed on 5 May 2014]
- O’Meara TJ, Sercombe JK, Morgan G, et al. The reduction of rhinitis symptoms by nasal filters during natural exposure to ragweed and grass pollen. Allergy 2005;60(4):529-32
- Arora P. The nasal filter as a simple treatment for inhalant allergy. Nurs J India 1976;67(4):85-6
- Pasricha JS. Use of nasal filters in naso-bronchial allergy. Indian J Pediatr 1981;48(390):47-50
- D’Amato G, D’Amato M, Rumi G, et al. Improvement of quality of life in allergic rhinoconjunctivitis patients using nasal filters, a preliminary study. Eur Ann Allergy Clin Immunol 2013;45(5):167-75
- Kenney P, Hilberg O, Pedersen H, et al. Nasal filters for the treatment of allergic rhinitis: a randomized, double-blind, placebo-controlled crossover clinical trial. J Allergy Clin Immunol 2014;133(5):1477-80
- Renstrom A, Karlsson AS, Tovey E. Nasal air sampling used for the assessment of occupational allergen exposure and the efficacy of respiratory protection. Clin Exp Allergy 2002;32(12):1769-75
- Tovey E, Lucca SD, Poulos L, O’Meara T. The Halogen assay – a new technique for measuring airborne allergen. Methods Mol Med 2008;138:227-46