Abstract
The ability to switch between yeast and hyphal growth forms (dimorphism) is one of the most discussed and best investigated virulence attributes of the human pathogenic fungus Candida albicans. Both morphological forms seem to be important for virulence and have distinct functions during the different stages of disease development, including adhesion, invasion, damage, dissemination, immune evasion and host response. In this review, we will provide an overview of the known and potential roles of C. albicans dimorphism and will discuss the potential benefit of drugs that can inhibit the morphological transition.
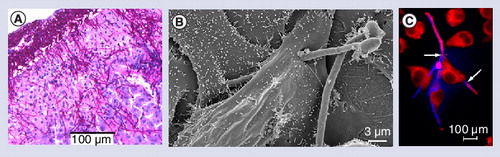
(A) Histological section showing C. albicans hyphae invading the murine liver 24 h after intraperitoneal infection. Scale bar = 100 µm. (B) Scanning electron microscopy of C. albicans invasion into oral epithelial cells after 3 h coincubation. A C. albicans hypha penetrates the epithelial cell, grows through the cell, exits the epithelial cell and invades another epithelial cell. The second hyphal cell is not invasive. Scale bar = 3 µm. Kindly provided by Gudrun Holland and Norbert Bannert (Robert Koch Institut, Berlin). (C) Fluorescence microscopy picture of human macrophages (J774) interacting with C. albicans cells after 2 h of coincubation. Red: macrophages; pink: extracellular C. albicans; blue: intracellular C. albicans. Two C. albicans hyphae have pierced a macrophage to escape (arrows). Scale bar = 100 µm.
Candida albicans is a polymorphic fungus that can grow as an ovoid budding yeast (named blastospores in older literature), as elongated ellipsoid cells that remain attached at a constricted separation site (pseudohyphae), or as parallel-sided true hyphae Citation[1]. The fungus can also form chlamydospores, spore-like structures, produced under distinct conditions, of as yet unknown biological function Citation[2,3], and undergo phenotypic switching between white and opaque morphologies – an event which is important for mating and biofilm formation Citation[4,5]. The transition between yeast and hyphal growth (named dimorphism) is tightly regulated by a network of signal transduction pathways in response to environmental stimuli (reviewed in Citation[6–9]).
C. albicans infections can be divided into at least four different stages: colonization, superficial infections, deep-seated infections and systemic infections Citation[10]. During colonization, C. albicans lives as a commensal, in equilibrium with the normal microbial flora on mucosal surfaces without causing harm to its host. The majority of the human population is asymptomatically colonized with C. albicans, but superficial infections can occur when the microbiotic balance is disturbed or the host immune system is compromised. Oral infections are extremely common among certain immunocompromised patients (e.g., HIV patients). In contrast, vaginal infections often occur in individuals without any clear sign of immune defects. Hospitalized patients with certain risk factors are predisposed to life-threatening systemic candidiasis Citation[11], characterized by dissemination via the bloodstream and infection of internal organs.
Proposed roles of yeast & hyphal morphologies of C. albicans
The role of the morphological transition for the different stages of C. albicans infections has been hotly debated for many years Citation[12]. It is generally accepted that hyphal cells are more invasive Citation[1] and indeed, most histological pictures of invading C. albicans cells show hyphae , while there are rare reports of invading yeast cells Citation[13–15]. Based on these observations, a popular view is that yeast are the noninvasive, commensal morphology, and some authors go even further, suggesting that hyphae are the pathogenic form while yeasts are the nonpathogenic form. This view is certainly oversimplified. Rather, it would appear that both morphological forms are of relevance during infection: yeast and hyphal cells are both found in infected organs Citation[16] and, depending on the organ, one or the other morphology predominates. For example, filamentation is regularly observed in the kidney, but not in the spleen or liver during invasive candidiasis Citation[17]. However, there is no clear evidence which morphology predominates during the commensal phase in humans.
It has been proposed that yeast cells, due to their ovoid dimension and smaller size, are important for dissemination within the bloodstream. Indeed, it appears logical that longer hyphae would not be disseminated as efficiently. However, if hyphae are the invasive form, how can yeast cells reach the bloodstream? If C. albicans reaches the bloodstream via the ‘natural’ route through penetration of epithelial cells from mucosal surfaces Citation[18], they likely reach the bloodstream as hyphae. It appears unlikely that these hyphae then switch to yeast cells in the blood, as serum components are amongst the strongest inducers of hyphal formation. In fact, we have shown that yeast cells in blood start to produce germ tubes very early, at least to a moderate extent (∼42% within 30 min Citation[19]). Complete hyphal formation is counteracted by neutrophils in the blood Citation[19]. However, neutrophils inhibit growth of C. albicans in general, and it cannot be concluded that neutrophils specifically stimulate yeast growth. Therefore, it seems unlikely that C. albicans undergoes a hyphal-to-yeast transition in the blood as part of a dissemination strategy. Another possibility is that invading hyphae provide a route for yeast cells to enter the bloodstream from the gastrointestinal tract.
In the vast majority of candidemia cases, however, iatrogenic routes enable C. albicans to reach the bloodstream. The presence of a central venous catheter, parenteral nutrition, burns and gastrointestinal surgery list among the leading risk factors for disseminated candidiasis Citation[11]. As C. albicans can grow as yeast in the gastrointestinal tract Citation[20] or on the skin Citation[21], these risk factors could certainly lead to hematogenous seeding with yeast cells. Biofilms on medical devices provide an alternative route; indeed, ‘disperser’ yeast cells can be produced from biofilms Citation[22], which could readily seed the bloodstream. Thus, yeast cells may indeed be an important morphology for dissemination.
It is not clear whether any morphology is more abundant during the commensal stage. As the expression of hyphal-associated genes was detected during asymptomatic carriage Citation[23–25], it is possible that commensal cells grow in the hyphal form. However, this observation should be interpreted with caution, since hyphal-associated genes are expressed by yeast cells under certain conditions Citation[19,20,26,27]. Indeed, Kumamoto et al. have reported the expression of hyphal-associated genes by C. albicans colonizing the murine gastrointestinal tract (after removal of the bacterial flora), a niche where the dominant morphology was yeast cells Citation[20,28].
In contrast, it is generally accepted that C. albicans dimorphism is required for full virulence. The most convincing evidence of this is the fact that C. albicans mutants which are trapped either in the yeast (e.g., efg1Δ/cph1Δ, hgc1Δ) Citation[29,30] or a filamentous form (e.g., nrg1Δ) Citation[31] are attenuated in virulence.
There are numerous publications that deal with the morphological switch from yeast-to-hyphal growth and the multiple factors that regulate this process, such as Ras1, Efg1, Cph1, Tec1 and Rim101 (reviewed in Citation[6,7]). Less attention has been paid to factors that regulate the hyphal-to-yeast transition, such as the hyphal repressors Nrg1 or Tup1 Citation[31–33], or to factors that are important for maintenance or extension of hyphal growth, for example Cln1, Pes1, Eed1 or Ume6 Citation[34–38].
These factors not only govern morphology, but also regulate morphology-associated genes, for example, HWP1, SOD5, SAP4–6 or ALS3, the expression of which is linked to hyphal growth under most conditions. As will be discussed below, both the morphology and the expression of morphology-associated genes contribute to virulence.
Hyphal formation & adhesion
Adhesion and hyphal formation are fundamentally related: contact of C. albicans to abiotic surfaces or to host cells stimulates hyphal formation and the simultaneous induction of hyphal-associated adhesins. These events in turn enhance the adhesiveness of the fungus to surfaces. The reduced adhesion potential of mutants lacking key regulators of hyphal development (e.g., ras1Δ or efg1Δ) is likely to be largely due to the misregulation of hyphal-associated adhesins, as mutants lacking adhesins alone (such as Als3 or Hwp1) also exhibit strongly reduced adhesion.
Hyphal formation & invasion
Invasion of C. albicans into epithelial cells is mediated by two distinct processes: induced endocytosis and active penetration Citation[36,39,40]. Induced endocytosis is a host-driven process triggered predominantly by interaction between the C. albicans invasin, Als3, and host E-cadherin. This process results in clathrin-dependent uptake, similar to the internalin-E-cadherin dependent internalization of Listeria monocytogenesCitation[36,41,42]. Under standard laboratory growth conditions, Als3 is expressed on hyphal, but not yeast cell surfaces Citation[43]. Consequently, only hyphal cells were observed to be endocytosed by epithelial and endothelial cells Citation[36,41].
In contrast, active penetration is an exclusively fungal-driven process that is mediated by hyphal extension (controlled by Ume6 and Eed1) and hyphal-associated activities such as the production of secreted aspartic proteases (Sap4–6) Citation[35,39,40,44]. Extending hyphae are also essential for interepithelial dissemination: the penetration into adjacent epithelial cells following initial epithelial invasion. These subsequent invasion events may be responsible for the gross damage of epithelial tissues by the fungus Citation[36].
Hyphal formation & iron acquisition during oral infection
Inside oral epithelial cells, iron is stored within ferritin, and is therefore not usually accessible to pathogenic microbes. However, C. albicans has been shown to exploit host ferritin as an iron source during experimental infections of oral tissue Citation[43]. Interestingly, C. albicans hyphae, but not yeast cells, were found to bind ferritin, and this binding was crucial for iron acquisition from ferritin. Moreover, the ferritin receptor was found to be Als3, suggesting that this single hyphae-associated protein has multiple virulence attributes.
C. albicans escape from phagocytes
Invading and disseminating C. albicans cells are faced with phagocytic cells that constitute the first line of defense during infection. Patrolling macrophages and attracted neutrophils efficiently phagocytose C. albicans yeast cells and short hyphae. While neutrophils strongly inhibit growth (including the yeast-to-hyphal transition) of C. albicans and can efficiently kill the fungus Citation[19,45,46], yeast cells phagocytosed by macrophages may survive and produce hyphae, which pierce through the host membrane, rapidly killing the phagocyte and allowing C. albicans to escape Citation[19,47]. The higher expression level of SOD5 (encoding an extracellular superoxide dismutase) in hyphae may counteract the oxidative burst of phagocytic cells and thus may help to survive attack of monocytes, macrophages and neutrophils Citation[19,48,49]. Therefore, the hyphal transition is a critical event for escaping phagocytes.
C. albicans escape from the bloodstream
As mentioned above, yeast cells may enter the bloodstream via damage of natural barriers or as disperser cells from biofilms on medical devices, and a significant portion of yeast cells in human blood produces germ tubes to a moderate extent Citation[19]. Similar to the above discussed adhesion of hyphae to epithelial cells, germ tubes adhere strongly to endothelial cells. In addition, it has been shown that physical properties and an optimal length (neither too short nor too long) promote endothelial adhesion during flow conditions, similar to the conditions in the bloodstream Citation[50]. Differences in hyphal length may also explain why, in contrast to our results with germ tubes, Grubb et al. found yeast cells adhered better than hyphae Citation[51]. Furthermore, it should be noted that yeast cells dispersed from biofilms display increased adherence compared with their planktonic counterparts Citation[22]. A direct comparison of the adherence capability of dispersed yeast cells and hyphae, however, has not been performed as yet.
Hyphal-associated gene expression & the concept of predictive adaptation
In summary, hypha formation and the expression of hyphal-associated genes mediate distinct virulence functions such as adhesion (HWP1, ALS3), invasion (ALS3), oxidative stress response (SOD5), proteolysis (SAP4–6), or ferritin binding (ALS3). Interestingly, many hyphal-associated genes are expressed counterintuitively in response to numerous (if not all) hyphae-inducing conditions. For example, SOD5 is expressed in the absence of oxidative stress and ALS3 is upregulated by planktonic hyphal cells in the absence of ferritin. As discussed in a previous review Citation[52], C. albicans gene expression seems to be dictated both by direct environmental responses and by discrete genetic programs (such as the yeast-to-hyphal transition). The former allows rapid adaptation to changing environmental conditions and is a hallmark of unicellular life. The latter may be analogous to predictive adaptation Citation[53] and prepare the fungus for subsequent stages of infection. Perhaps C. albicans has ‘learned’ that during invasive (hyphal) growth it will encounter reactive oxygen species (a common host response to infection), ferritin (the major intracellular iron storage molecule) and protein-derived nitrogen sources, and coordinates gene expression accordingly.
Recognition by & interaction with the immune system: yeast versus hyphae
Given the diverse functions and consequences of C. albicans dimorphism, it is intuitive that the morphological form also affects interactions with the immune system. However, we are only beginning to understand the full complexity of the immune response to C. albicans morphology in shaping the host response . In general, a robust host response, especially involving components of the innate immunity, is required for protection against superficial and systemic candidiasis. This is highlighted by the findings of Saville et al. who demonstrated that a C. albicans strain that is locked in the yeast form (via NRG1 overexpression) was avirulent in immunocompetent mice Citation[54]. However, the same nonfilamentous strain was capable of killing severely immunosuppressed mice. Similarly, severe immunosuppression is a prerequisite for lethal dissemination of C. albicans from the gastrointestinal tract in mice Citation[55]. On the other hand, an excessive proinflammatory response contributes to the development of sepsis in systemically infected immunocompetent mice Citation[56,57]. Finally, depending on the site of infection, C. albicans likely encounters different components of the immune system, adding to the complexity of possible interactions.
Superficial infections: the role of morphology in the immune response of epithelia towards C. albicans
For many years, epithelial cells lining mucosal surfaces were thought to be innocuous bystanders during the infection process. However, in the past decade it has become increasingly obvious that epithelial cells are key mediators of pathogen recognition and initiators of innate and adaptive immunity. However, an excessively strong inflammatory response can lead to substantial host tissue damage, which can exacerbate or even cause symptomatic clinical disease. Thus, it is essential that epithelia are able to discriminate between harmless commensals and dangerous pathogens. This is particularly pertinent for C. albicans, which can have both commensal and pathogenic lifestyles. So how do epithelial cells discriminate between C. albicans colonization and infection? Recently, Moyes et al. have begun to shed light on the molecular mechanisms for this discriminatory process, and their data indicates that both the morphological form of C. albicans and the fungal burden are crucial Citation[58]. Oral epithelial cells appear to orchestrate responses to C. albicans via NF-κB and a biphasic MAPK signaling mechanism. Activation of NF-κB and the initial MAPK response, which results in the activation of the c-Jun transcription factor, is independent of fungal morphology and can be elicited by both yeast and hyphae. However, stimulation of a secondary MAPK response, resulting in activation of the c-Fos transcription factor and the MAPK phosphatase MKP1, is specifically associated with hypha formation and correlates with proinflammatory cytokine responses. An important finding was that the hypha-mediated MAPK/MKP1/c-Fos response was strongly dose-dependent, indicating that a threshold level of activation needs to be reached before epithelial cells are fully activated. The resulting proinflammatory cytokine response appears to recruit and activate polymorphonuclear cells, which subsequently protect the oral mucosa against C. albicans infection via a mechanism that requires Toll-like receptor (TLR)4 Citation[59]. In summary, this epithelial MAPK-based activation pathway may comprise a ‘danger response’ mechanism, which may permit mucosal tissues to remain quiescent in the presence of low fungal burdens whilst responding specifically and strongly to damage-inducing hyphae when burdens increase. Therefore, this morphology-based detection mechanism may be critical in identifying when this normally commensal fungus has become pathogenic.
The interaction of yeast versus hyphae with professional immune cells
Although few studies have addressed the impact of C. albicans morphology on interaction with immune cells, there is evidence that the growth form influences both the type and the outcome of the interaction. For example, dendritic cells phagocytose both yeast and hyphae but kill yeast cells more efficiently Citation[60]. In contrast, neutrophils are more attracted to hyphae but kill yeast and hyphae at the same rate Citation[61,62]. Similarly, macrophages were shown to phagocytose a higher proportion of inactivated hyphae than yeast Citation[63]. However, using viable C. albicans cells in competition assays, Keppler-Ross et al. observed higher uptake of yeast than hyphae by macrophages Citation[64]. Thus, more research is needed to fully elucidate the role of fungal morphology in the interaction with macrophages.
Macrophages and dendritic cells not only mediate direct killing of C. albicans but also orchestrate the immune response via the production of chemokines and cytokines. The cytokine production of dendritic cells again differs depending on C. albicans morphology. Yeast cells stimulate priming of Th1 cells while hyphae lead to the production of IL-4 and inhibition of Th1 priming Citation[60]. Since Th1 and Th17 responses are thought to be beneficial for the host, the different responses of dendritic cells to yeast and hyphae may strongly influence the clinical course of infection. Morphology-dependent differences in cytokine production have also been demonstrated in macrophages Citation[65] and monocytes Citation[66].
The first step in the interaction of professional immune cells and pathogens is the recognition of pathogen-associated molecular patterns on the pathogen surface by pathogen recognition receptors (PRRs) on immune cells. Since the C. albicans cell wall composition is highly flexible Citation[67], it appears plausible that differences in the cell wall composition and accessibility of pathogen-associated molecular patterns on C. albicans yeasts and hyphae lead to the observed differences in immune cell interaction. C. albicans cell surface mannans, β-glucans and chitin are recognized by innate immune cells such as macrophages and neutrophils via various PRRs, including mannose receptor, dectin-1 and dectin-2, TLR2, TLR4 and CR3 (reviewed in Citation[68,69]). In dendritic cells, distinct sets of PRRs are involved in recognition of either C. albicans yeast or hyphae and affect phagocytic killing and cytokine production Citation[70]. In vivo, β-glucan exposure changes during infection and, interestingly, treatment with caspofungin selectively unmasks β-glucans on hyphae Citation[71]. Since unmasking of β-glucans enhances macrophage cytokine production Citation[72], this mechanism might influence the outcome of infection. Furthermore, distinct yeast or hyphal-specific surface proteins may be specifically recognized by immune cells and act as indicators of fungal morphology for the immune system Citation[73].
Is inhibition of the yeast-to-hyphal transition a therapeutic option?
Traditionally, antimicrobial drugs have been developed to interfere with essential biological processes to either kill a microbe or to inhibit its growth. More recently, specifically targeting virulence rather than essential fungal processes has been discussed as a ‘new’ paradigm for the development of antibacterial and antifungal agents Citation[74,75]. The modulation of morphogenesis may provide a way to specifically target virulence of C. albicansCitation[76].
Targeting virulence factors
There are both major advantages and disadvantages to targeting specific virulence factors for therapeutic purposes. Virulence factors are often highly specific, and targeting any specific virulence attribute may not act against any other pathogen. Such an approach would therefore require very precise, reliable and rapid diagnostics, which are often not available (particularly in the case of fungal infections). Furthermore, such a therapeutic strategy may not be attractive to large pharmaceutical companies, who may prefer to create a universal antifungal. Moreover, non-albicans species (including non-hyphae-producing species) now account for approximately half the cases of disseminated candidiasis Citation[11]. Therefore, inhibition of hypha formation as a prophylactic strategy or as empirical antifungal therapy for disseminated candidiasis (even upon positive diagnosis of candidiasis), would currently be undesirable.
On the other hand, when highly effective diagnostics are in place, therapeutically targeting microbial virulence, such as the yeast-to-hyphal transition, will have significant advantages. For example, targeting pathogen-specific factors may allow for a very specific action with few side effects and a reduced incidence of microbial resistance. Such a strategy may also help to specifically keep an opportunistic pathogen in check, rather than wiping out the entire microbial population – a concern when dealing with potentially beneficial probiotic microbes. Indeed, we cannot exclude that C. albicans colonization has beneficial effects, for example, by training and stimulating our immune system.
Targeting the morphological switch
In the future, targeted inhibition of the morphological switch from yeast-to-hyphal growth would be a very attractive option for specifically controlling C. albicans infections, both prophylactically and as a treatment. As discussed above, such an inhibition could prevent adhesion, invasion and damage of epithelial and endothelial cells, may prevent escape from macrophages and from the bloodstream, and may reduce the iron acquisition capacity of the fungus.
Furthermore, such a targeted inhibition may be used to modulate the immune response, avoiding excessive inflammation during superficial infections, or over-reaction and potentially fatal sepsis during systemic candidiasis. For example, it has been suggested that protection against C. albicans vaginitis coincides with a noninflammatory innate immune response, whereas symptomatic infections correlate with neutrophil infiltrates in the vaginal lumen and an elevated fungal burden Citation[77]. Thus, rather than being caused by deficient (lowered) immunity, symptomatic vaginitis can be considered to be the result of an overly aggressive innate immune response. It is likely that hyphae play a key role in eliciting such aggressive immune responses, and if hyphal formation could be inhibited, the response would be downregulated accordingly.
In addition to inhibiting fungal filamentation and the expression of hyphae-associated proteins, it may also be possible to directly target those hyphae-specific proteins or moieties that activate epithelial cells and innate immune responses, or that are responsible for damaging these cells. Alternatively, the host’s recognition system may be targeted. For example, increasing the threshold level at which epithelial cells are activated may decrease the chance of a runaway immune response. Thus, identification of the epithelial cell receptors that initiate immune activation could lead to an interesting therapeutic target Citation[78]. This may also apply to systemic infections. Although the contribution of yeast-to-hyphal transition to the development of C. albicans sepsis is not yet clear, indirectly modulating the host response by controlling C. albicans filamentation may have therapeutic potential.
In fact, as a proof of principle, it has been shown experimentally that blocking filamentation in C. albicans attenuates its virulence in vivoCitation[79], although not every deletion mutant with defects in filamentation is attenuated Citation[80].
Can the yeast-to-hyphal transition be inhibited?
As discussed in an excellent review by Shareck and Belhumeur Citation[76], a large number of small molecules, such as farnesol, fatty acids, rapamycin, geldanamycin, histone deacetylase inhibitors, and cell cycle inhibitors have been reported to modulate the yeast-to-hyphal transition in C. albicans. Few of these substances have been tested in vivo, but protection against mucosal candidiasis has been shown by, for example, geldanamycin, farnesol and nizin Z Citation[81–83]. However, it should be mentioned that many of the small molecules which inhibit filamentation also negatively affect fungal viability or growth. The relative contributions of cytotoxicity and inhibition of filamentation by these compounds to protection against candidiasis has not yet been fully elucidated.
Even established antifungals, such as azoles, can specifically inhibit hyphal growth. In our laboratory, we examined the effects of low levels of azoles on the ability of C. albicans to adhere, invade and damage vaginal epithelial cells. These low levels of azoles did not influence yeast growth, but effectively inhibited extensive hyphal elongation Citation[84]. Interestingly, although adhesion to and invasion of vaginal epithelial cells were not affected, the damage caused to these cells was greatly reduced upon azole treatment, and this was most likely due to reduced hyphae formation. These data provide evidence that low levels of azoles influence specific activities of C. albicans during distinct stages of epithelial infections and provide a proof of principle that inhibition of hypha formation can be used as a therapeutic option.
Conclusion
The yeast-to-hyphal transition of C. albicans is linked to a number of properties: adhesion to epithelial and endothelial cells; primary and intercellular invasion via induced endocytosis and active penetration; specific iron acquisition from intracellular host sources; escape from phagocytes and immune evasion; promotion of immune activation at mucosal tissues and triggering of specific sepsis-like immune responses during systemic infection. Thus, dimorphism is essential for pathogenicity at both superficial and systemic levels. The pathogenic potential of hypha formation is due to both the fungal morphology and the expression of a hypha-specific transcriptional program; moreover, the immune system is able to discriminate between yeast and hyphal growth. This specific recognition of C. albicans morphology, together with detection of fungal burden and damage caused by invading hyphae may be the key for host discrimination between colonization and infection. Despite the general limitations of targeted inhibition of distinct virulence attributes of microbial pathogens, there are also clear advantages, and targeted inhibition of the yeast-to-hyphal transition or modulation of the immune response associated with dimorphism may therefore be very attractive options for controlling C. albicans infections in the future.
Expert commentary & five-year view
Although few of the compounds known to inhibit the yeast-to-hyphal transition have been evaluated in vivo, and some may be cytotoxic Citation[76], it is likely that a compound will be identified that specifically inhibits filamentation without major side effects. It may even be possible that C. albicans ‘anti-dimorphism’ compounds may be active against other fungi. For example, the quorum-sensing molecule farnesol also affects various developmental processes in other Candida spp. and in unrelated pathogenic fungi such as Aspergillus spp., Fusarium graminearum and Paracoccidioides brasiliensisCitation[76,85].
In the next years, further genes, factors and activities involved in the morphological switch of C. albicans will be discovered and our knowledge of the regulatory networks governing morphology will be extended. This will include the regulation of the yeast-to-hyphal transition as well as the, less well studied, reverse switch – the hypha-to-yeast transition.
In addition to cell density, temperature, serum compounds, oxygen or carbon dioxide concentrations and metabolism, we will discover further unexpected relationships between the host environment and the regulation of morphology. Importantly, we need to know more about the role of the yeast and hyphal morphologies in pathogenesis and the specific responses of host cells. We need to understand how the different host cells recognize yeast and hyphae and how each cell type is activated by either morphology. It is very likely that the consequences of this activation are different in different host cell types (e.g., in epithelial cells and in phagocytes). Based on this information, we may then be in a position to target either fungal or host factors (or both) to control and manage a particular infection.
Table 1. Examples of morphology-dependent activities of Candida albicans during infection.
Table 2. Examples of morphology-dependent interaction of host cells with Candida albicans.
Key issues
• Candida albicans is a polymorphic fungus that can grow as yeasts, pseudohyphae or hyphae.
• C. albicans can colonize mucosal surfaces, or cause superficial, deep-seated or systemic infections.
• Yeast cells, hyphae and the morphology-associated genes play distinct roles during infection depending on the host niche and stage of infection.
• Yeast cells may favor dissemination.
• The morphology of asymptomatic colonizing cells in humans remains unknown.
• Hyphal formation is associated with adhesion, invasion, damage, iron acquisition, and escape from phagocytes and the bloodstream.
• Invasion of hyphae occurs via induced endocytosis and active penetration. Only active penetration causes damage.
• Hyphae-associated gene expression is an example of predictive adaptation.
• Yeast and hyphae are differentially recognized by different host cells.
• The host may differentiate between colonizing and infecting cells via differential recognition of noninvasive and nondamaging yeast cells versus invasive and damaging hyphae.
• There are both advantages and disadvantages to targeting virulence factors as therapeutic options.
• Targeting the morphological switch is a therapeutic option, and proof of principles exist that such therapy blocks damage in vitro and may attenuate virulence in vivo.
• Compounds already exist that can inhibit yeast-to-hypha transition.
Financial & competing interests disclosure
The authors’ research is supported by the Hans Knöll-Institut, the Federal Ministry of Education and Research (BMBF: ERA Net PathoGenoMics FUNPath 0313931B and CandiCol 0315901B, PET-CT 0314108, Integrated Research and Treatment Center, Sepsis und Sepsisfolgen, Center for Sepsis Control and Care), the Deutsche Forschungsgemeinschaft (DFG Hu 528/14, 15, 16 and 17), the European Union (CaInfectome PIEF-GA-2008-219406, FinSysB MCRTN FP7-214004), the companies Biolitec and Bayer Vital, NIDCR (DE017514; to JR Naglik) and the Department of Health via the National Institute for Health Research comprehensive Biomedical Research Centre award to Guy’s & St Thomas’ NHS Foundation Trust in partnership with King’s College London (to JR Naglik). The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
References
- Berman J, Sudbery PE. Candida albicans: a molecular revolution built on lessons from budding yeast. Nat. Rev. Genet.3(12), 918–930 (2002).
- Martin SW, Douglas LM, Konopka JB. Cell cycle dynamics and quorum sensing in Candida albicans chlamydospores are distinct from budding and hyphal growth. Eukaryot. Cell4(7), 1191–1202 (2005).
- Citiulo F, Moran GP, Coleman DC, Sullivan DJ. Purification and germination of Candida albicans and Candida dubliniensis chlamydospores cultured in liquid media. FEMS Yeast Res.9(7), 1051–1060 (2009).
- Miller MG, Johnson AD. White-opaque switching in Candida albicans is controlled by mating-type locus homeodomain proteins and allows efficient mating. Cell110(3), 293–302 (2002).
- Daniels KJ, Srikantha T, Lockhart SR, Pujol C, Soll DR. Opaque cells signal white cells to form biofilms in Can. Albicans. EMBO J.25(10), 2240–2252 (2006).
- Biswas S, Van Dijck P, Datta A. Environmental sensing and signal transduction pathways regulating morphopathogenic determinants of Candida albicans. Microbiol. Mol. Biol. Rev.71(2), 348–376 (2007).
- Whiteway M, Bachewich C. Morphogenesis in Candida albicans. Ann. Rev. Microbiol.61, 529–553 (2007).
- Shapiro RS, Cowen L. Coupling temperature sensing and development: Hsp90 regulates morphogenetic signalling in Candida albicans. Virulence1(1), 45–48 (2010).
- Sudbery PE. Growth of Candida albicans hyphae. Nat. Rev. Microbiol.9(10), 737–748 (2011).
- Odds FC. Candida species and virulence. ASM News60, 313–318 (1994).
- Perlroth J, Choi B, Spellberg B. Nosocomial fungal infections: epidemiology, diagnosis, and treatment. Med. Mycol.45(4), 321–346 (2007).
- Gow NA, Brown AJ, Odds FC. Fungal morphogenesis and host invasion. Curr. Opin. Microbiol.5(4), 366–371 (2002).
- Pope LM, Cole GT. Comparative studies of gastrointestinal colonization and systemic spread by Candida albicans and nonlethal yeast in the infant mouse. Scan. Electron. Microsc. (Pt 4), 1667–1676 (1982).
- Ray TL, Payne CD. Scanning electron microscopy of epidermal adherence and cavitation in murine candidiasis: a role for Candida acid proteinase. Infect. Immun.56(8), 1942–1949 (1988).
- Saville SP, Lazzell AL, Monteagudo C, Lopez-Ribot JL. Engineered control of cell morphology in vivo reveals distinct roles for yeast and filamentous forms of Candida albicans during infection. Eukaryot. Cell2(5), 1053–1060 (2003).
- Odds FC. Morphogenesis in Candida, with special reference to C. albicans. In: Candida and Candidosis. A Review and Bibliography. Odds FC (Ed.). Ballière Tindall, London, UK, 42–59 (1988).
- Lionakis MS, Lim JK, Lee CC, Murphy PM. Organ-specific innate immune responses in a mouse model of invasive candidiasis. J. Innate. Immun.3(2), 180–199 (2011).
- Mavor AL, Thewes S, Hube B. Systemic fungal infections caused by Candida species: epidemiology, infection process and virulence attributes. Curr. Drug Targets6(8), 863–874 (2005).
- Fradin C, De Groot P, MacCallum D et al. Granulocytes govern the transcriptional response, morphology and proliferation of Candida albicans in human blood. Mol. Microbiol.56(2), 397–415 (2005).
- White SJ, Rosenbach A, Lephart P et al. Self-regulation of Candida albicans population size during GI colonization. PLoS Pathog.3(12), e184 (2007).
- Lachke SA, Lockhart SR, Daniels KJ, Soll DR. Skin facilitates Candida albicans mating. Infect. Immun.71(9), 4970–4976 (2003).
- Uppuluri P, Chaturvedi AK, Srinivasan A et al. Dispersion as an important step in the Candida albicans biofilm developmental cycle. PLoS Pathog.6(3), e1000828 (2010).
- Naglik JR, Fostira F, Ruprai J, Staab JF, Challacombe SJ, Sundstrom P. Candida albicans HWP1 gene expression and host antibody responses in colonization and disease. J. Med. Microbiol.55(Pt 10), 1323–1327 (2006).
- Naglik JR, Rodgers CA, Shirlaw PJ et al. Differential expression of Candida albicans secreted aspartyl proteinase and phospholipase B genes in humans correlates with active oral and vaginal infections. J. Infect. Dis.188(3), 469–479 (2003).
- Mochon AB, Ye J, Kayala MA et al. Serological profiling of a Candida albicans protein microarray reveals permanent host-pathogen interplay and stage-specific responses during candidemia. PLoS Pathog.6(3), e1000827 (2010).
- Sosinska GJ, de Groot PW, Teixeira de Mattos MJ et al. Hypoxic conditions and iron restriction affect the cell-wall proteome of Candida albicans grown under vagina-simulative conditions. Microbiology (Read. Engl.),154(Pt 2), 510–520 (2008).
- Andaluz E, Ciudad T, Gomez-Raja J, Calderone R, Larriba G. Rad52 depletion in Candida albicans triggers both the DNA-damage checkpoint and filamentation accompanied by but independent of expression of hypha-specific genes. Mol. Microbiol.59(5), 1452–1472 (2006).
- Rosenbach A, Dignard D, Pierce JV, Whiteway M, Kumamoto CA. Adaptations of Candida albicans for growth in the mammalian intestinal tract. Eukaryot. Cell9(7), 1075–1086 (2010).
- Lo HJ, Kohler JR, DiDomenico B, Loebenberg D, Cacciapuoti A, Fink GR. Nonfilamentous C. albicans mutants are avirulent. Cell90(5), 939–949 (1997).
- Zheng X, Wang Y. Hgc1, a novel hypha-specific G1 cyclin-related protein regulates Candida albicans hyphal morphogenesis. EMBO J.23(8), 1845–1856 (2004).
- Murad AM, Leng P, Straffon M et al.NRG1 represses yeast-hypha morphogenesis and hypha-specific gene expression in Candida albicans. EMBO J.20(17), 4742–4752 (2001).
- Braun BR, Kadosh D, Johnson AD. NRG1, a repressor of filamentous growth in C. albicans, is down-regulated during filament induction. EMBO J.20(17), 4753–4761 (2001).
- Braun BR, Johnson AD. Control of filament formation in Candida albicans by the transcriptional repressor TUP1 Sci.277(5322), 105–109 (1997).
- Shen J, Cowen LE, Griffin AM, Chan L, Kohler JR. The Candida albicans pescadillo homolog is required for normal hypha-to-yeast morphogenesis and yeast proliferation. Proc. Natl Acad. Sci. USA105(52), 20918–20923 (2008).
- Martin R, Moran GP, Jacobsen ID et al. The Candida albicans-specific gene EED1 encodes a key regulator of hyphal extension. PLoS One6(4), e18394 (2011).
- Zakikhany K, Naglik JR, Schmidt-Westhausen A, Holland G, Schaller M, Hube B. In vivo transcript profiling of Candida albicans identifies a gene essential for interepithelial dissemination. Cell Microbiol.9(12), 2938–2954 (2007).
- Banerjee M, Thompson DS, Lazzell A et al.UME6, a novel filament-specific regulator of Candida albicans hyphal extension and virulence. Mol. Biol. Cell19(4), 1354–1365 (2008).
- Loeb JD, Sepulveda-Becerra M, Hazan I, Liu H. A G1 cyclin is necessary for maintenance of filamentous growth in Candida albicans. Mol. Cell Biol.19(6), 4019–4027 (1999).
- Dalle F, Wachtler B, L’Ollivier C et al. Cellular interactions of Candida albicans with human oral epithelial cells and enterocytes. Cell. Microbiol.12(2), 248–271 (2010).
- Wächtler B, Wilson D, Haedicke K, Dalle F, Hube B. From attachment to damage: defined genes of Candida albicans mediate adhesion, invasion and damage during interaction with oral epithelial cells. PLoS One6(2), e17046 (2011).
- Phan QT, Myers CL, Fu Y et al. Als3 is a Candida albicans invasin that binds to cadherins and induces endocytosis by host cells. PLoS Biol.5(3), e64 (2007).
- Moreno-Ruiz E, Galan-Diez M, Zhu W et al.Candida albicans internalization by host cells is mediated by a clathrin-dependent mechanism. Cell Microbiol.11(8), 1179–1189 (2009).
- Almeida RS, Brunke S, Albrecht A et al. The hyphal-associated adhesin and invasin Als3 of Candida albicans mediates iron acquisition from host ferritin. PLoS Pathog.4(11), e1000217 (2008).
- Naglik JR, Challacombe SJ, Hube B. Candida albicans secreted aspartyl proteinases in virulence and pathogenesis. Microbiol. Mol. Biol. Rev.67(3), 400–428 (2003).
- Rubin-Bejerano I, Fraser I, Grisafi P, Fink GR. Phagocytosis by neutrophils induces an amino acid deprivation response in Saccharomyces cerevisiae and Candida albicans. Proc. Natl Acad. Sci. USA100(19), 11007–11012 (2003).
- Fradin C, Kretschmar M, Nichterlein T, Gaillardin C, d’Enfert C, Hube B. Stage-specific gene expression of Candida albicans in human blood. Mol. Microbiol.47(6), 1523–1543 (2003).
- Lorenz MC, Bender JA, Fink GR. Transcriptional response of Candida albicans upon internalization by macrophages. Eukaryot. Cell3(5), 1076–1087 (2004).
- Martchenko M, Alarco AM, Harcus D, Whiteway M. Superoxide dismutases in Candida albicans: transcriptional regulation and functional characterization of the hyphal-induced SOD5 gene. Mol. Biol. Cell15(2), 456–467 (2004).
- Frohner IE, Bourgeois C, Yatsyk K, Majer O, Kuchler K. C. albicans cell surface superoxide dismutases degrade host-derived reactive oxygen species to escape innate immune surveillance. Mol. Microbiol.71(1), 240–252 (2008).
- Wilson D, Hube B. Hgc1 mediates dynamic Candida albicans-endothelium adhesion events during circulation. Eukaryot. Cell9(2), 278–287 (2010).
- Grubb SE, Murdoch C, Sudbery PE, Saville SP, Lopez-Ribot JL, Thornhill MH. Adhesion of Candida albicans to endothelial cells under physiological conditions of flow. Infect. Immun.77(9), 3872–3878 (2009).
- Hube B. From commensal to pathogen: stage- and tissue-specific gene expression of Candida albicans. Curr. Opin. Microbiol.7(4), 336–341 (2004).
- Mitchell A, Romano GH, Groisman B et al. Adaptive prediction of environmental changes by microorganisms. Nature460(7252), 220–224 (2009).
- Saville SP, Lazzell AL, Chaturvedi AK, Monteagudo C, Lopez-Ribot JL. Use of a genetically engineered strain to evaluate the pathogenic potential of yeast cell and filamentous forms during Candida albicans systemic infection in immunodeficient mice. Infect. Immun.76(1), 97–102 (2008).
- Koh AY, Kohler JR, Coggshall KT, Van Rooijen N, Pier GB. Mucosal damage and neutropenia are required for Candida albicans dissemination. PLoS Pathogens4(2), e35 (2008).
- MacCallum DM. Massive induction of innate immune response to Candida albicans in the kidney in a murine intravenous challenge model. FEMS Yeast Res.9(7), 1111–1122 (2009).
- MacCallum DM, Castillo L, Brown AJ, Gow NA, Odds FC. Early-expressed chemokines predict kidney immunopathology in experimental disseminated Candida albicans infections. PLoS One,4(7), e6420 (2009).
- Moyes DL, Runglall M, Murciano C et al. A biphasic innate immune MAPK response discriminates between the yeast and hyphal forms of Candida albicans in epithelial cells. Cell Host Microbe8(3), 225–235 (2010).
- Weindl G, Naglik JR, Kaesler S et al. Human epithelial cells establish direct antifungal defense through TLR4-mediated signaling. J. Clin. Invest.117(12), 3664–3672 (2007).
- d’Ostiani CF, Del Sero G, Bacci A et al. Dendritic cells discriminate between yeasts and hyphae of the fungus Candida albicans. Implications for initiation of T helper cell immunity in vitro and in vivo. J. Exp. Med.191(10), 1661–1674 (2000).
- Wozniok I, Hornbach A, Schmitt C et al. Induction of ERK-kinase signalling triggers morphotype-specific killing of Candida albicans filaments by human neutrophils. Cell Microbiol.10(3), 807–820 (2008).
- Urban CF, Reichard U, Brinkmann V, Zychlinsky A. Neutrophil extracellular traps capture and kill Candida albicans yeast and hyphal forms. Cell Microbiol.8(4), 668–676 (2006).
- Marcil A, Gadoury C, Ash J, Zhang J, Nantel A, Whiteway M. Analysis of PRA1 and its relationship to Candida albicans- macrophage interactions. Infect. Immun.76(9), 4345–4358 (2008).
- Keppler-Ross S, Douglas L, Konopka JB, Dean N. Recognition of yeast by murine macrophages requires mannan but not glucan. Eukaryot. Cell9(11), 1776–1787 (2010).
- Netea MG, Gijzen K, Coolen N et al. Human dendritic cells are less potent at killing Candida albicans than both monocytes and macrophages. Microbes Infect.6(11), 985–989 (2004).
- Torosantucci A, Chiani P, Cassone A. Differential chemokine response of human monocytes to yeast and hyphal forms of Candida albicans and its relation to the β-1,6 glucan of the fungal cell wall. J. Leukoc. Biol.68(6), 923–932 (2000).
- Chaffin WL. Candida albicans cell wall proteins. Microbiol. Mol. Biol. Rev.72(3), 495–544 (2008).
- Netea MG, Brown GD, Kullberg BJ, Gow NA. An integrated model of the recognition of Candida albicans by the innate immune system. Nat. Rev. Microbiol.6(1), 67–78 (2008).
- Jouault T, Sarazin A, Martinez-Esparza M, Fradin C, Sendid B, Poulain D. Host responses to a versatile commensal: PAMPs and PRRs interplay leading to tolerance or infection by Candida albicans. Cell Microbiol.11(7), 1007–1015 (2009).
- Romani L, Montagnoli C, Bozza S et al. The exploitation of distinct recognition receptors in dendritic cells determines the full range of host immune relationships with Candida albicans. Int. Immunol.16(1), 149–161 (2004).
- Wheeler RT, Kombe D, Agarwala SD, Fink GR. Dynamic, morphotype-specific Candida albicans β-glucan exposure during infection and drug treatment. PLoS Pathogens4(12), e1000227 (2008).
- Wheeler RT, Fink GR. A drug-sensitive genetic network masks fungi from the immune system. PLoS Pathogens2(4), e35 (2006).
- Pietrella D, Rachini A, Pandey N et al. The Inflammatory response induced by aspartic proteases of Candida albicans is independent of proteolytic activity. Infect. Immun.78(11), 4754–4762 (2010).
- Alksne LE, Projan SJ. Bacterial virulence as a target for antimicrobial chemotherapy. Curr. Opin. Biotechnol.11(6), 625–636 (2000).
- Gauwerky K, Borelli C, Korting HC. Targeting virulence: a new paradigm for antifungals. Drug Discov. Today14(3–4), 214–222 (2009).
- Shareck J, Belhumeur P. Modulation of morphogenesis in Candida albicans by various small molecules. Eukaryot. Cell10(8), 1004–1012 (2011).
- Fidel PL Jr. History and update on host defense against vaginal candidiasis. Am. J. Reprod. Immunol.57(1), 2–12 (2007).
- Moyes DL, Naglik JR. Mucosal immunity and Candida albicans infection. Clin. Dev. Immunol.2011, 346307 (2011).
- Saville SP, Lazzell AL, Bryant AP et al. Inhibition of filamentation can be used to treat disseminated candidiasis. Antimicrob. Agents Chemother.50(10), 3312–3316 (2006).
- Spiering MJ, Moran GP, Chauvel M et al. Comparative transcript profiling of Candida albicans and Candida dubliniensis identifies SFL2, a C. albicans gene required for virulence in a reconstituted epithelial infection model. Eukaryot. Cell9(2), 251–265 (2010).
- Cowen LE, Singh SD, Kohler JR et al. Harnessing Hsp90 function as a powerful, broadly effective therapeutic strategy for fungal infectious disease. Proc. Natl Acad. Sci. USA106(8), 2818–2823 (2009).
- Akerey B, Le-Lay C, Fliss I, Subirade M, Rouabhia M. In vitro efficacy of nisin Z against Candida albicans adhesion and transition following contact with normal human gingival cells. J. Appl. Microbiol.107(4), 1298–1307 (2009).
- Hisajima T, Maruyama N, Tanabe Y et al. Protective effects of farnesol against oral candidiasis in mice. Microbiol. Immunol.52(7), 327–333 (2008).
- Wächtler B, Wilson D, Hube B. Candida albicans adhesion to and invasion and damage of vaginal epithelial cells: stage-specific inhibition by clotrimazole and bifonazole. Antimicrob. Agents Chemother.55(9), 4436–4439 (2011).
- Langford ML, Atkin AL, Nickerson KW. Cellular interactions of farnesol, a quorum-sensing molecule produced by Candida albicans. Future Microbiol.4(10), 1353–1362 (2009).
- Phan QT, Belanger PH, Filler SG. Role of hyphal formation in interactions of Candida albicans with endothelial cells. Infect. Immun.68(6), 3485–3490 (2000).
