Abstract
Age is a significant factor in modifying specific needs when it comes to medical aesthetic procedures. In this review we will focus on young adults in their third decade of life and review minimally invasive aesthetic procedures other than cosmetics and cosmeceuticals. Correction of asymmetries, correction after body modifying procedures, and facial sculpturing are important issues for young adults. The implication of aesthetic medicine as part of preventive medicine is a major ethical challenge that differentiates aesthetic medicine from fashion.
Introduction
Minimally invasive procedures are more often requested by adult patients of all ages. Nevertheless there are specific needs of different age groups. In two recent reviews, middle-aged women and women older than 60 years have been discussed.Citation1,Citation2 In the present paper, we wish to focus on young adult women and men in their third decade of life and address some of the more specific problems in this age group such as the treatment of acne scars, skin laxity, hyperkinetic facial wrinkles, and repair of tissue defects after earlobe piercing.
Although topical treatment may also contribute to improved appearance, we will exclude this from the present review except for medical peels.
Anatomical considerations and early signs of aging
In the third decade of life, anatomical changes are characterized by the development of maturity. Some of these changes are deeply influenced by pregnancy and lactation; others develop independently. In general, there is good skin elasticity and gravitational folds are uncommon. Hyperactive facial wrinkles are mainly seen on the glabella and forehead.
Minor changes of UV-related skin aging become visible such as pigmentary changes like actinic lentigines in Fitzpatrick skin type I and II. Solar elastosis or dermoheliosis may be seen when outdoor activity meets artificial tanning and heavy smoking. Since smoking has become more popular among younger females than males, we may observe a further increase in the next decade. Indeed, there are a growing number of patients younger than 30 years of age developing basal cell carcinoma.Citation3
The majority of patients are characterized by mild signs of aging but this may be comparable to the first grey hair found on ones head. These minor changes mark the transition of youth to initial signs of aging. Nevertheless, minimally aesthetic procedures in this particular age group have multiple indications, from improving acne scars and sculpturing facial parts to minimizing the adverse effects of piercing. Anti-aging is part of the spectrum but in contrast to middle-aged patients it does yet not play a major role.
Common aesthetic problems and solutions
Acne scars
Acne has developed from a disease of puberty to a disease expanding from adolescence into adult ages. The most disfiguring element of acne is the development of permanent visible scars. Acne scarring is common but difficult to treat. A descriptive, universally acceptable classification system of atrophic acne scars includes three scar types: ice pick, boxcar, and rolling. Erythema and, less often, pigmentary changes may be associated.Citation4
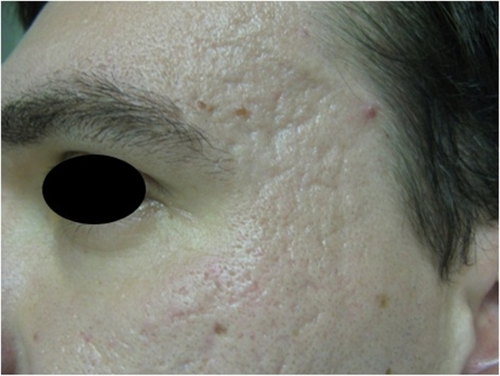
Ice pick and boxcar scars can be improved by several measures including chemical, mechanical, and laser peeling, fractional laser, subcision, dermal fillers, microneedling, excision, and a combination of procedures ( and ).Citation5–Citation10
Figure 1B Acne treatment by capryloyl salicylic acid peel (22-year-old male) after treatment. Reduction of large inflammatory cysts two weeks after a single treatment with 10% capryloyl salicylic acid.

Figure 2B Fractional CO2 laser for acne scars after two laser sessions with marked improvement of skin surface.
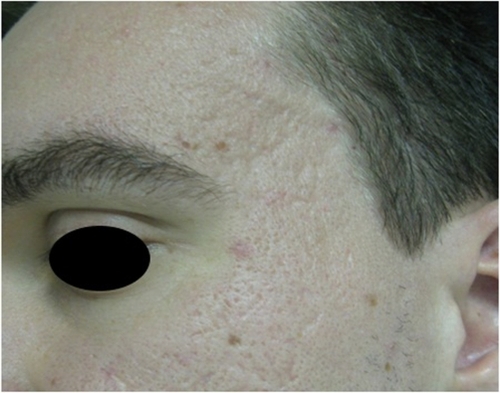
Ablative lasers such as CO2 and Erb:YAG are useful tools in the treatment of acne scars in fair-skinned patients only, as they have a higher risk of complications related to pigmentation. Prolonged post-treatment hyperemia is another unwanted side effect. Fractional lasers have less severe side effects but more moderate efficacy compared to ablative devices.
Fractional CO2 laser with a laser fluence from 2.07–4.15 J/cm2 has been shown to increase tissue repair both clinically and on cytokine levels.Citation11 Efficacy and safety of an erbium-doped 1,550-nm fractional laser in the treatment of facial acne scars in Fitzpatrick skin types IV to VI was studied in a prospective, single-blind, randomized trial in 15 patients with acne scars. Patients were divided into two groups; one was treated with 10 mJ and the other with 40 mJ. Five monthly laser sessions were performed. During treatment there was a significant improvement in the acne scarring and overall appearance with no significant difference between the 10 and 40 mJ groups. Patients were highly satisfied with their results. Significant postinflammatory hyperpigmentation was seen in patients. Pain was significantly higher in darker skin.Citation12
More recently, nonablative laser systems have been introduced into acne scar treatment. The nonablative 1,550-nm erbium-doped fractional photothermolysis system has been effectively used for scar treatments in Asian skin, but it seems that several sessions of treatment must be delivered to achieve satisfactory improvement.Citation13
Fourteen patients with atrophic acne scars were treated by a combination of subcision and permanent dermal filler injection (Artefill®). Investigator ratings after eight months postprocedure indicated that 96% of the atrophic acne scars showed some degree of improvement. The majority of patients reported a moderate correction, correlating with a 51%–75% improvement in their acne scars at eight months. No adverse events or side effects were noted in this short study.Citation14 Since permanent filler may produce adverse reactions after many years, the risk may not outweigh the benefits in younger adults. Nonpermanent filler such as hyaluronic acid (HA) may be considered, but repeated application will be necessary.
Boxcar scars are mostly treated by excision or ablative procedures. In a recent trial, 24 subjects with punched-out acne scars were treated monthly for two months with four passes of various square pulse Er:YAG laser resurfacing using a 7-mm spot size and a fluence of 0.4 J/cm2. Subjects were divided into two groups and treated with two different pulse widths: 300 micros (short pulse) and 1,500 micros (extra-long pulse). In the short pulse group, skin smoothness improved significantly whereas in the extra-long pulse group, skin smoothness and scar volume improved significantly from baseline.Citation15 For rolling scars, but not icepick scars, the 1,550 nm Erb:Glass fractional laser three times with a 6-week interval showed efficacy.Citation16 Subcision is a reliable method for rolling scars. In a trial with 22 patients, subcision showed mild improvement in about 60% of patients and moderate improvement in about 40% of them.Citation17 Other laser types used successfully to improve acne scars include Erb:YAG and CO2 fractional lasers.
Microneedling is a relatively new and simple procedure for dermatology. In a study from Italy, 32 patients with acne rolling scars were enrolled. Each patient was treated in two sessions. Analysis of the patient photographs and of the degree of irregularity of the skin surface, supported by fast Fourier transformation, showed that after only two sessions, the severity grade of rolling scars in all patients was greatly reduced and there was an overall aesthetic improvement.Citation18
The aim of acne scar treatment is to stimulate wound healing and collagen neogenesis. Skin relaxation is addressed by subcision and related methods. It seems that effects can be long-lasting. The usual outcome is an improvement of 25%–75%, with most procedures achieving around 50%. Complete resolution is still impossible.Citation19
Chemical peeling can be used as an adjunct to acne treatment such as salicylic acid peels, but also for scar treatment. Chemical reconstruction of skin scars (CROSS) is a technique using high concentrations of trichloroacetic acid (TCA) focally on atrophic acne scars to induce inflammation followed by new collagen formation. This can lead to a reduction in the appearance of scars and cosmetic improvement. In an Indian pilot study, CROSS technique using 100% TCA was investigated for ice pick acne scars. Twelve patients were treated with the CROSS technique, using 100% TCA, applied with a wooden toothpick, at two weekly intervals for four treatments. More than 50% improvement was seen in all patients with eight out of ten patients achieving >70% improvement. Transient hypopigmentation and hyperpigmentation was an uncommon adverse effect. The CROSS technique with 100% TCA seems to be a safe, efficacious, cost-effective, and minimally invasive technique for the management of ice pick acne scars in Indian skin.Citation20
Possible adverse effects of scar treatment include hyperpigmentation, and less commonly, hypopigmentation, particularly in Asian skin. Temporary acneiform eruptions have been seen. Early effective acne therapy is the only way to avoid scarring.
Skin laxity
Laxity of skin is related to biochemical chances within the connective tissue leading to a decrease of collagen and elastic fibres. Although the process becomes more visible in middle-aged subjects, weight loss and pregnancy may be associated with skin laxity also amongst younger patients.
Fine wrinkling around the eyes is often the first sign of facial aging. Whereas crow’s feet are caused by muscular activity, a major part of the wrinkling of lower eyelids is the development of skin laxity. Younger females in particular are looking for procedures that are noninvasive and don’t cause downtime. For skin tightening in this sensitive area, radiofrequency devices (monopolar or bipolar), laser, or ultra-pulsed light and infrared light devices have been used.Citation21,Citation22
One of the therapeutic principles used is dermal remodelling by stimulation of collagen synthesis. This can be achieved by heating the dermal tissue or wounding as with fractioned CO2 or Erb:YAG laser. Peak temperature, total time of exposure, and mechanical stress applied to the skin during the heating process affect the clinical results. Noninvasive radiofrequency and infrared devices seems to be more active on the looser and delicate skin such as eyelids ().Citation21
Figure 3A Monopolar radiofrequency treatment of lower eyelids before treatment. The usual treatment series is four to six applications.
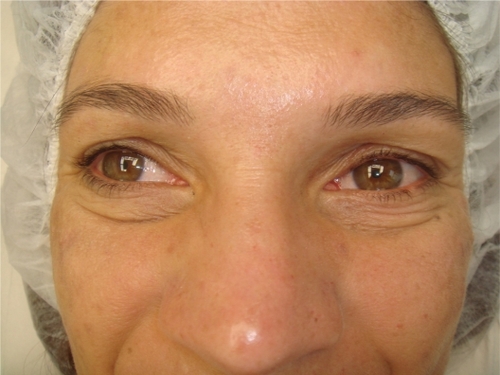
Figure 3B Monopolar radiofrequency treatment of lower eyelids after two treatments every other week.

Most studies demonstrate an improvement measured by clinical scores, high-frequency ultrasound, or confocal laser microscopy in the range of 30%–50% during one treatment series ().
Table 1 Improvement of skin laxity by radiofrequency
Hyperkinetic facial wrinkles
The major areas with facial wrinkles in the third decade of life are the forehead (frontalis muscle) and glabella (corrugator muscles). The most evidence-based data are available for the use of botulinum toxin type A. There are three approved products on the German market (from A to Z): Azzalure (Galderma, Paris, France/Medicis Aesthetics, Scottsdale, AZ), Bocouture (Merz, Frankfurt, Germany), and Vistabel (Allergan, Irvine, CA).
Both large multicenter trials and postmarketing surveillance clearly demonstrate that these drugs are safe and effective. There is no tachyphylaxis after repeated application. Adverse effects are mild and temporary as long as contraindications are not ignored. Injection pain and bruising may occur, others such as brow ptosis are mainly due to incorrect injection technique and are reduced by improved technique.Citation23–Citation25
The effects will last between five to six months with some interindividual variability. For advanced glabellar lines combining with a nonpermanent filler such as cross-linked HA gives longer lasting improvement. Recently, we described a new injection technique to correct the downturn of the corners of the mouth with botulinum toxin type A. We used a combination of platysma and depressor anguli oris modification by partial chemical denervation.Citation26
Fillers for younger skin
The use of dermal fillers has expanded over the last two decades. The major indication is volumizing and sculpturing (). Fillers can be used in younger females although the indications and products preferred may differ from those in more mature females.
Small amounts of fillers may be useful in the correction of glabellar folds as mentioned earlier. Laterally placed filler in a fanning technique may be used to enhance the brows. Occasional minor irregularities may occur, but these can be smoothed out by massage or blended by further injection. Results lasting between six months and two years are reported depending on the type of filler. Some brow configurations that falsely project emotional states, such as anxiety, may also be corrected.Citation27
Liquid lift of the middle and lower face is realized by deep, periostal placement of higher crosslinked monophasic HA fillers in the cheekbone area. By this placement, the filler depot has a longer durability compared to nasolabial folds or cheeks because of the limited movements in this region. There is also a mild effect on upper lip position.Citation28 In nasolabial fold treatment, biodegradable microparticle injectables, including Radiance (BioForm, San Mateo, CA) or Radiesse (Merz) provide longer lasting results. Microscopically new collagen formation was observed around the microparticles consisting of calcium hydroxylapetite.Citation29–Citation31
Lip contouring by filler injection is often requested. Short-term effects may be favorable when soft HA fillers are placed along the vermillion border to underline the upper lip. The Cupid’s bow should not be touched. In the case of lip contouring with smaller filler volumes, a cool pack may provide sufficient pain relief. Lip contouring effects may last for three to six months.
Volumizing the lip is a more painful procedure and local anesthetics are recommended. Overtreatment gives an unnatural look and increases the risk of adverse effects such as granuloma formation and others. It is important to investigate the fine motions of the lips before treatment. Filler placement should not result in a loss of such fine movements to avoid an artificial touch perceived by others. As skin laxity becomes more prominent, lip volumizing creates not only additional volume but also weight. This can lead to less satisfying results. The less the better as a rule.Citation31
Indications of lip volumizing by fillers in young females may be genetically thin lips and posttraumatic irregularities. A tool for objective evaluation of the individual situation and the enhancement by filler is the lip index. Adding upper and lower lip indices resulted in the overall lip index, which was found to be approximately 50 in average females of Caucasian descent, about 100 in females of Asian descent, and nearly 200 in females of African descent.Citation28 It is noteworthy, that volumizing treatment of nasolabial folds and cheeks can result in an improvement in upper lip position.Citation1,Citation2
Partial or whole face injection with uncrosslinked HA gels to provide a rapid but temporary improvement of skin smoothness and hydration is performed by syringes and other technical devices as part of mesotherapy. Long-term outcome has not been analyzed scientifically. Nevertheless, the combination of multiple punctures with HA injection leads to a mild oedema and may induce dermal wound healing responses but further studies are needed.Citation32
Aesthetic procedures to correct piercing and piercing complications
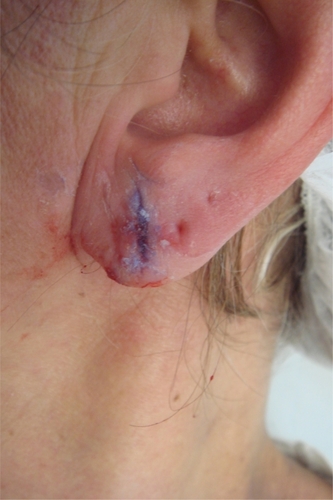
While earlobe piercing has been socially and widely accepted for females over many decades, body piercing has not. Recently body piercing has become very popular in young adults, in particular young women. The prevalence of body piercing in the UK is 10%. Nearly half the women aged 16–24 reported having had a piercing.Citation33 In a US survey, 14% of adults had body piercings. Body piercing was more common among women. Local medical complications were present in one-third of those with body piercings.Citation34 The situation is comparable to other Western countries.Citation35 Complications of these body modifying procedures often warrant medical treatment ( and ).
Figure 5 Piercing, tunnelling and tattoo in a 24-year-old female. Skin inflammation tunnelling site.

Reconstruction of earlobes and other parts after piercing is being increasingly requested by patients. A more common problem with earlobe piercing is the development of keloids. There seems to be a genetic background for the risk of keloid formation. Permanent clearing of keloids is not simple. Stahl et alCitation36 used the “sandwich” technique protocol with extralesional excision and external-beam radiotherapy given a day before and a day after the operation. In a retrospective evaluation of their patients (average age 24 years; 57% males), recurrence rates were 25% and 27% for low- and high-risk patients, respectively. Overall, patient satisfaction was high.
Incomplete earlobe clefts are another possible complication of piercing and the wearing of jewellery in this area. There are surgical and nonsurgical procedures available to deal with this problem. Brazilian authors presented a nonsurgical procedure for incomplete earlobe cleft repair using trichloroacetic acid 90%. They assessed 32 patients with a total of 53 earlobes to be noninvasively repaired. The complete treatment varied from 2 to 50 days with repeated application of trichloroacetic acid 90%. No recurrences were observed during one year of follow-up. All of the clefts were totally repaired, and all of the patients were satisfied with the aesthetic results. The procedure resulted in good functional and cosmetic results, with low costs, minimum risks, and was easy to apply.Citation37
Another option is the excision of the epithelium by radiofrequency and immediate application of acrylate-based tissue glue (). Many surgical techniques have been described for the correction of ear lobe clefts, such as direct suturing, zetaplasty, ritidoplasty with ear lobe correction, V-shaped flaps, L-shaped flaps, and “surgery of the ear ring”.Citation38
Conclusion
Patients in their third decade of life can benefit from minimally aesthetic procedures either to delay minor signs of facial aging or to repair acquired disfigurements. Identification of those patients who suffer from body dysmorphic disorder and psychiatric illness is important. Careful communication to patients about gains and risks is of the greatest importance. Furthermore, overtreatment should be avoided. A natural look is of particular importance for this age group. Aesthetic medical procedures are considered an integral part of ethical medicine, not, as suggested by mass media, a part of fashion.Citation39
Disclosure
No conflicts of interest were declared in relation to this paper.
References
- WollinaUPayneCRAgeing well – the role of minimally invasive aesthetic dermatological procedures in women over 65J Cosmet Dermatol201091505820367673
- GoldmanAWollinaUFacial rejuvenation for middle-aged women: a combined approach with minimally invasive proceduresClin Interv Aging2010529329920924438
- WollinaUAddiction to tanning – a new cause of early onset of nonmelanoma skin cancerOpen Dermatol J200938688
- JansenTPoddaMTherapy of acne scarsJ Dtsch Dermatol Ges20108Suppl 1S81S8820482696
- LeeJWKimBJKimMNLeeCKTreatment of acne scars using subdermal minimal surgery technologyDermatol Surg20103681281128720573176
- ManuskiattiWTriwongwaranatDVarothaiSEimpunthSWanitphakdeedechaREfficacy and safety of a carbon-dioxide ablative fractional resurfacing device for treatment of atrophic acne scars in AsiansJ Am Acad Dermatol201063227428320633798
- KutlubayZGokdemirGTreatment of atrophic facial acne scars with the Er:YAG laser: a Turkish experienceJ Cosmet Laser Ther2010122657220331342
- WollinaUCapryloyl salicylic acid (CSA) peel for acne and actinic damageKosmet Med2009304142145
- GargVKSinhaSSarkarRGlycolic acid peels versus salicylic-mandelic acid peels in active acne vulgaris and post-acne scarring and hyperpigmentation: a comparative studyDermatol Surg2009351596519076192
- KempiakSJUebelhoerNSuperficial chemical peels and microdermabrasion for acne vulgarisSemin Cutan Med Surg200827321222018786500
- PrignanoFCampolmiPBonanPFractional CO2 laser: a novel therapeutic device upon photobiomodulation of tissue remodelling and cytokine pathway of tissue repairDermatol Ther200922SupplS8S1519891690
- MahmoudBHSrivastavaDJanigaJJYangJJLimHWOzogDMSafety and efficacy of erbium-doped yttrium aluminum garnet fractionated laser for treatment of acne scars in type IV to VI skinDermatol Surg201036560260920384757
- ChoSBLeeSJKangJMKimYKChungWSOhSHThe efficacy and safety of 10,600-nm carbon dioxide fractional laser for acne scars in Asian patientsDermatol Surg200935121955196119708872
- EpsteinRESpencerJMCorrection of atrophic scars with artefill: an open-label pilot studyJ Drugs Dermatol2010991062106420865835
- KimHJKimTGKwonYSParkJMLeeJHComparison of a 1,550 nm erbium: glass fractional laser and a chemical reconstruction of skin scars (CROSS) method in the treatment of acne scars: a simultaneous split-face trialLasers Surg Med200941854554919639620
- WanitphakdeedechaRManuskiattiWSiriphukpongSChenTMTreatment of punched-out atrophic and rolling acne scars in skin phototypes III, IV, and V with variable square pulse erbium: yttrium-aluminum-garnet laser resurfacingDermatol Surg20093591376138319549185
- FabbrociniGFardellaNMonfrecolaAProiettiIInnocenziDAcne scarring treatment using skin needlingClin Exp Dermatol200934887484919486041
- BalighiKRobatiRMMoslehiHRobatiAMSubcision in acne scar with and without subdermal implant: a clinical trialJ Eur Acad Dermatol Venereol200822670771118341538
- OrtizAETremaineAMZacharyCBLong-term efficacy of a fractional resurfacing deviceLasers Surg Med201042216817020166157
- BhardwajDKhungerNAn assessment of the efficacy and safety of cross technique with 100% TCA in the management of ice pick acne scarsJ Cutan Aesth Surg2010329396
- SadickNTissue tightening technologies: fact or fictionAesthet Surg J200828218018819083525
- MonicaEPeriorbital skin tightening with a broadband infrared device: preliminary study resultsJ Cosmet Laser Ther2010121384120020836
- HeviaORetrospective review of 500 patients treated with abobotulinumtoxin AJ Drugs Dermatol2010991081108420865838
- RubinMDoverJMaasCNestorMAn analysis of safety data from five phase III clinical trials on the use of botulinum neurotoxin type A-ABO for the treatment of glabellar linesAesthet Surg J2009296 SupplS50S5619945005
- CohenJLSchlessingerJCoxSELinXReloxin Investigational GroupAn analysis of the long-term safety data of repeat administrations of botulinum neurotoxin type A-ABO for the treatment of glabellar linesAesthet Surg J2009296 SupplS43S4919945004
- GoldmanAWollinaUElevation of the corner of the mouth using botulinum toxin type AJ Cutan Aesthet Surg20103314515021430826
- LambrosVVolumizing the brow with hyaluronic acid fillersAesthet Surg J200929317417919621494
- WollinaUGoldmanABergerUAbdel-NaserMBEsthetic and cosmetic dermatologyDermatol Ther200821211813018394086
- TzikasTLEvaluation of Radiance FN soft tissue filler for facial soft tissue augmentationArch Facial Plast Surg20046423423915262717
- Moers-CarpiMVogtSSantosGPlanasJVallveSHowellDA multicenter randomized trial comparing calcium hydroxlyapetite to two hyaluronic acids for the treatment of nasolabial foldsDermatol Surg200733Suppl 2S144S15118086052
- NewmanJReview of soft tissue augmentation in the faceClin Cosmet Investig Dermatol20092141150
- AtiyehBSIbrahimAEDiboSACosmetic mesotherapy: between scientific evidence, science fiction, and lucrative businessAesthetic Plast Surg200832684284918663517
- LemperleGAndersonRKnappTRAn index for quantitative assessment of lip augmentationAesthet Surg J201030330131020601553
- BoneANcubeFNicholsTNoahNDBody piercing in England: a survey of piercing at sites other than earlobeBMJ200833676581426142818556275
- LaumannAEDerickAJTattoos and body piercings in the United States: a national data setJ Am Acad Dermatol200655341342116908345
- StahlSBarneaYWeissJTreatment of earlobe keloids by extralesional excision combined with preoperative and postoperative “sandwich” radiotherapyPlast Reconstr Surg2010125113514120048606
- De MendonçaMCde OliveiraARAraújoJMSilvaMGGamonalANonsurgical technique for incomplete earlobe cleft repairDermatol Surg200935344645019250307
- PatrocínioLGMoraisRMPereiraJEPatrocínioJAEarlobe cleft reconstructive surgeryBraz J Otorhinolaryngol200672444745117143422
- Gadebusch BondioMMedical aesthetics [German]Wilhelm Fink VerlagMunich2005
- WilleyAKilmerSNewmanJElastometry and clinical results after bipolar radiofrequency treatment of skinDermatol Surg201036687788420618372
- Alexiades-ArmenakasMRosenbergDRentonBDoverJArndtKBlinded, randomized, quantitative grading comparison of minimally invasive, fractional radiofrequency and surgical face-lift to treat skin laxityArch Dermatol2010146439640520404228
- BogleMAUbelhoerNWeissRAMayoralFKaminerMSValuation of the multiple pass, low fluence algorithm for radiofrequency tightening of the lower faceLasers Surg Med200739321021717304562
- YuCSYeungCKShekSYTseRKKonoTChanHHCombined infrared light and bipolar radiofrequency for skin tightening in AsiansLasers Surg Med200739647147517659587
- SadickNSAlexiades-ArmenakasMBitterPJrHruzaGMulhollandRSEnhanced full-face skin rejuvenation using synchronous intense pulsed optical and conducted bipolar radiofrequency energy (ELOS): introducing selective radiophotothermolysisJ Drugs Dermatol20054218118615776775
- DoshiSNAlsterTSCombination radiofrequency and diode laser for treatment of facial rhytides and skin laxityJ Cosmet Laser Ther200571111516020210