Abstract
Subcorneal pustular dermatosis (SPD) is a rare, chronic pustular dermatosis. The pathogenesis of SPD has not been fully elucidated, but some studies have found that tumor necrosis factor (TNF)-α may be associated with its pathogenesis. Some patients with multidrug-resistant SPD have improved significantly after treatment with the anti-TNF-α agent (adalimumab). We present a case of a 28-year-old female with severe SPD who responded rapidly to adalimumab (80mg/week) in combination with acitretin and methylprednisolone within a week. With adalimumab (40 mg next week and followed by 40mg every two weeks) and gradually ceasing other systemic medication, the patient’s condition continued to improve without relapse or side effects. The outcome of this case suggests that adalimumab might be an effective treatment option against multidrug-resistant SPD.
Introduction
Subcorneal pustular dermatosis (SPD) is a rare neutrophilic dermatosis first described by Sneddon and Wilkinson. It occurs at any age, more commonly in females, and usually presents as tiny pustules in the trunk, intertriginous areas, and flexural sites of the extremities.Citation1 It is often difficult to treat, and persisting disease may lead to morbidity and a decline in quality of life. Although oral dapsone represents the first-line therapy for SPD, relapses are common and alternative treatments, including corticosteroids, acitretin, and immunosuppressants (methotrexate and cyclosporine) may be required.Citation1 Due to the role of anti-tumor necrosis factor (TNF)-α in SPD pathology, several clinical reports have shown effective off-label therapy using anti-TNF-α agents (eg, infliximab, pentoxifylline, etanercept, and adalimumab) in resistant cases.Citation2,Citation3 This study presents a 28-year-old female with severe SPD who was successfully treated with adalimumab.
Case Report
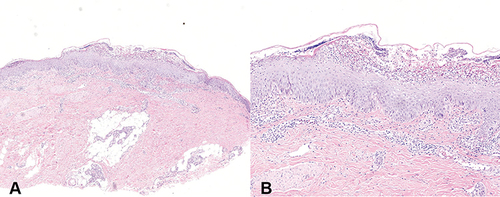
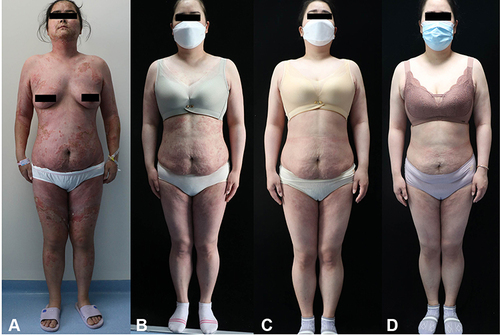
A 28-year-old woman presented to the dermatology clinic with complaints of severe, progressive pustular skin eruptions and burning sensation for the past three months. The lesions had begun as erythema and pustules on the patient’s left thigh and had aggravated and spread over the course of the next few days. The patient was diagnosed with eczema in the other hospital and did not respond to traditional Chinese medicine, oral glucocorticoid (methylprednisolone, 15–20 mg/day), antihistamines, or various topical treatments with corticosteroids and compound polymyxin B ointment. No past history of any skin disease or drugs intake, which causes the lesions. Clinical examination revealed multiple erythema and pustules were present on the face, trunk, and extremities (). The lesions tended to coalesce in annular or circinate pattern, with central clearing and raised margins and attached scaling and crusts. Nikolsky’s sign was negative. The patient complained of severe burning and tingling. The patient did not have any other related systemic symptoms. Abnormal laboratory findings included a slight elevation of leukocytes (21.8 x 10^9/L, normal:3.5–9.5x10^9/L), percentage of neutrophils (85.35%, normal:40–75%), and erythrocyte sedimentation rate (20mm/h, normal:<15mm/h), whereas immunoglobulins, thyroid profile, and biochemistry including liver and renal function were normal. A lesional skin biopsy showed a subcorneal pustule composed predominantly of neutrophils, with spongiosis in the granular and upper spine layer and infiltration of neutrophils and lymphocytes in the superficial dermis ( and ). Direct immunofluorescence with immunoglobulins IgG, IgA, IgM, and complement C3 were negative. A bacterial culture taken from the pustules did not reveal any bacterial infection. These clinicopathological findings led to the diagnosis of subcorneal pustular dermatosis. The patient was initially treated with methylprednisolone (40 mg/day for one week), cefixime (100 mg/day for one week), and omeprazole (40 mg/day for one week). She was also treated topically with corticosteroids, fusidic acid cream, and moisture cream on her lesions. Unfortunately, her skin lesions remained unchanged, even after routine laboratory examination and sedimentation rate had recovered, and did not respond to subsequent administration of the acitretin (0.6mg/kg/day for 1 week). Thus, after obtaining informed consent from the patient, we decided to introduce adalimumab at the induction dose of 80 mg one week, in combination with acitretin (0.6mg/kg/day) and methylprednisolone (40 mg/day). After administration, the skin lesions gradually improved within 1 week of the treatment (). Then, she continued to receive adalimumab (40 mg next week and followed by 40mg every two weeks), and the doses of acitretin and methylprednisolone were gradually tapered and finally withdrawn. After six weeks of follow-up, almost all the lesions subsided, with no new lesions or adverse reactions ().
Figure 1 (A) Multiple erythemas and pustules with central clearing and crusted edge located on the face, trunk, and extremities upon initial evaluation. (B) Regression of skin lesions one week after treatment with Adalimumab (80mg/week). (C and D) Regression of skin lesions three weeks and six weeks after treatment with Adalimumab.
Discussion
SPD has been classically described in women, mainly affecting the intertriginous and flexural areas; however, our patient complained of severe lesions involvement throughout the body.Citation1 Histopathologically, the SPD hallmark is neutrophil infiltration of the subcorneal layer of the epidermis, with occasional eosinophils,Citation1,Citation4 as in our patient. Although the superficial sterile pustules and neutrophil accumulation are considered as characteristic hallmarks of SPD, its exact pathomechanism remains unclear. Dapsone remains the first-line treatment for SPD, but since it was not available in our hospital, we started with oral corticosteroids (methylprednisolone, 40 mg/day). Some cases improve with oral corticosteroids,Citation1,Citation5 although steroids are generally ineffective even at medium to high doses,Citation6,Citation7 as in this case. Thus, oral corticosteroids in combination with other systemic drugs (dapsone, acitretin, and cyclosporine) have been recommended.Citation1,Citation8 The action of acitretin in SPD is unclear but may be owing to the inhibition of neutrophil function.Citation9 Symptoms may tend to resolve within 8–15 days of treatment with an oral acitretin.Citation1 Due to poor control of the disease after treatment with oral corticosteroids and no fertility requirements, we started a therapeutic trial with acitretin (0.6mg/kg/day for one week). Despite this therapy, similar to the previous reports,Citation2,Citation10 our patient experienced progressive pustular eruptions and progressive reduced general condition. One of the theories considers that SPD is a neutrophilic dermatosis, and some chemotactic factors have participated in neutrophil recruitment and invasion, including the proinflammatory cytokine TNF.Citation1,Citation11 GrobCitation12 et al reported that both levels of serum TNF-a and intramuscular TNF-a in SPD were higher than normal values. These findings correspond well with previous reports of effective off-label anti-TNF-α agents in the previous casesCitation3,Citation11,Citation13,Citation14 that were refractory to therapy of dapsone, corticosteroids, acitretin, phototreatment, and cyclosporin. Adalimumab is an entirely human anti-TNF monoclonal antibody and can reduce epidermal neutrophil infiltration by inhibiting TNF-α to treat SPD. In this case, the patient was successfully treated with adalimumab after failing to respond to systematic, topical corticosteroids and acitretin. EncarnacaoCitation11 et al reported a patient with SPD did not respond to combined treatment of acitretin (25 mg twice daily) and deflazacort (0.6 mg/kg/day), but the skin lesions were significantly improved after adding adalimumab treatment. These findings, together with the recalcitrant clinical course, have led to consider adalimumab as a valuable therapy in multi-drug-resistant cases. Besides, it was reported that the responsiveness of SPD to systemic glucocorticosteroids and acitretin was restored after the treatment of anti-TNF-α agents (infliximab).Citation10 Thus, concomitant use of acitretin, glucocorticoids, and adalimumab may be more effective than single adalimumab treatment and then receiving maintenance therapy with acitretin or glucocorticoids without additional anti-TNF-α agents. However, the exact mechanism needs further research to prove.
All the current reportsCitation3,Citation11,Citation13,Citation14 suggest the effectiveness of adalimumab in treating SPD, but this may have a publication bias, as only successful cases were published. SoderCitation15 et al reported that a 48-year-old woman with rheumatoid arthritis, four months after treatment with adalimumab only, had developed SPD. Interestingly, TNF-a is related to the pathogenesis of SPD, and the use of TNF-a inhibitors may induce the development of SPD. Besides, it was reported that raised levels of other neutrophils and chemoattractants such as interleukin (IL)-8, IL-1beta, IL-6, leukotriene B4, and C5a been detected in the pustules and serum of SPD patients.Citation1,Citation15 TNF-a antagonists reduce TNF-a levels but may also disturb homeostatic mechanisms and increase the risk of a second autoimmune disorder.Citation11,Citation15 The mechanism of this side effect of TNF-a remains controversial. Though adalimumab shows efficiency in cases of multidrug-resistant SPD, the detection of patient prognosis and adverse reactions is more critical in treating this off-label therapy. Further clinical trials and accumulating cases may demonstrate the efficacy of adalimumab in the optional treatment of SPD.
Ethics Statement
The patient gave written informed consent for publication of clinical information and photographs. No ethical committee approval was required because the data were analyzed in a retrospective manner.
Disclosure
The authors declare no conflict of interest.
Additional information
Funding
References
- Watts PJ, Khachemoune A. Subcorneal pustular dermatosis: a review of 30 years of progress. Am J Clin Dermatol. 2016;17:653–671. doi:10.1007/s40257-016-0202-8
- Romagnuolo M, Muratori S, Cattaneo A, et al. Successful treatment of refractory Sneddon-Wilkinson disease (subcorneal pustular dermatosis) with infliximab. Dermatol Ther. 2022;35:e15552. doi:10.1111/dth.15552
- Guerin CJ, Beylot-Barry M, Frouin E, et al. Treatment of subcorneal pustular dermatosis (Sneddon-Wilkinson disease) with anti-tumor necrosis factor alpha. Cureus. 2021;13:e17147. doi:10.7759/cureus.17147
- Caraballo L, Mahapatra S, Dimov V, et al. The striking appearance of a rare skin condition: “half-half” blisters (subcorneal pustular dermatosis). J Allergy Clin Immunol Pract. 2020;8:732–733. doi:10.1016/j.jaip.2019.09.018
- Ranieri P, Bianchetti A, Trabucchi M. Sneddon-Wilkinson disease: a case report of a rare disease in a nonagenarian. J Am Geriatr Soc. 2009;57:1322–1323. doi:10.1111/j.1532-5415.2009.02337.x
- Kretschmer L, Maul JT, Hofer T, et al. Interruption of Sneddon-Wilkinson subcorneal pustulation with infliximab. Case Rep Dermatol. 2017;9:140–144. doi:10.1159/000468917
- Borgia F, Campitiello A, Di Bartolomeo L, et al. Subcorneal pustular dermatosis successfully treated with low-dose doxycycline. Int J Dermatol. 2021;60:e375–6. doi:10.1111/ijd.15530
- Zachariae CO, Rossen K, Weismann K. An unusual severe case of subcorneal pustular dermatosis treated with cyclosporine and prednisolone. Acta Derm Venereol. 2000;80:386–387.
- Canpolat F, Akpinar H, Cemil BC, et al. A case of subcorneal pustular dermatosis in association with monoclonal IgA gammopathy successfully treated with Acitretin. J Dermatolog Treat. 2010;21:114–116. doi:10.3109/09546630902882071
- Voigtlander C, Luftl M, Schuler G, et al. Infliximab (anti-tumor necrosis factor alpha antibody): a novel, highly effective treatment of recalcitrant subcorneal pustular dermatosis (Sneddon-Wilkinson disease). Arch Dermatol. 2001;137:1571–1574. doi:10.1001/archderm.137.12.1571
- de Encarnacao RDF, Dias CJ, Macedo FA, et al. Subcorneal pustular dermatosis treated successfully with Adalimumab. Eur J Dermatol. 2010;20:512–514. doi:10.1684/ejd.2010.0957
- Grob JJ, Mege JL, Capo C, et al. Role of tumor necrosis factor-alpha in Sneddon-Wilkinson subcorneal pustular dermatosis. A model of neutrophil priming in vivo. J Am Acad Dermatol. 1991;25:944–947. doi:10.1016/0190-9622(91)70290-I
- Garcia DP, Agudo-Mena JL, Gomez-Sanchez ME, et al. Recalcitrant pyoderma gangrenosum and subcorneal pustular dermatosis successfully treated with Adalimumab. Actas Dermosifiliogr. 2020;111:887–889. doi:10.1016/j.ad.2019.02.028
- Versini M, Mantoux F, Angeli K, et al. [Sneddon-Wilkinson disease: efficacy of intermittent Adalimumab therapy after lost response to infliximab and etanercept]. Ann Dermatol Venereol. 2013;140:797–800. French. doi:10.1016/j.annder.2013.07.012
- Sauder MB, Glassman SJ. Palmoplantar subcorneal pustular dermatosis following Adalimumab therapy for rheumatoid arthritis. Int J Dermatol. 2013;52:624–628. doi:10.1111/j.1365-4632.2012.05707.x