Abstract
Maxillary and mandibular bone mirror skeletal bone conditions. Bone remodeling happens at endosteal surfaces where the osteoclasts and osteoblasts are situated. More surfaces means more cells and remodeling. The bone turnover rate in the mandibular alveolar process is probably the fastest in the body; thus, the first signs of osteoporosis may be revealed here. Hormones, osteoporosis, and aging influence the alveolar process and the skeletal bones similarly, but differences in loading between loaded, half-loaded, and unloaded bones are important to consider. Bone mass is redistributed from one location to another where strength is needed. A sparse trabeculation in the mandibular premolar region (large intertrabecular spaces and thin trabeculae) is a reliable sign of osteopenia and a high skeletal fracture risk. Having dense trabeculation (small intertrabecular spaces and well-mineralized trabeculae) is generally advantageous to the individual because of the low fracture risk, but may imply some problems for the clinician.
Introduction
A large proportion of the population visit their dentist annually, and dental radiographs are routinely taken then. Dentists are highly experienced in interpreting radiographs, but use them chiefly for the diagnosis of caries, marginal and apical periodontitis, and before implant treatment. However, there is much more information available in periapical radiographs. Therefore, many research teams have tried to develop methods for using the jawbones to predict osteoporosis Citation1–Citation4 and fracture risk.Citation5–Citation9
Possible links between osteoporosis and the degree of periodontitis have been debated for years. Both diseases are multifactorial and have many risk factors in common. The aims of the present article are to describe parallels between skeletal bone and alveolar bone and to illuminate some aspects of hormone function, loading and aging, which may explain alveolar bone loss caused by osteoporosis and/or periodontitis.
Bone
Bone is a dynamic tissue. During childhood and adolescence, the formation of bone dominates over the resorption of bone, this is the modeling phase. In mature adults, there is a balance between bone formation and resorption, whereas bone resorption dominates after menopause, and in older males. Skeletal loading produces microcracks in bone, which are replaced by remodeling.Citation10 The remodeling process is regulated systematically by hormones and locally by growth factors and cytokines.Citation11,Citation12 It takes place at the endosteal surfaces of cortical and trabecular bone.Citation13 At first, osteoclasts identify a site for renewal and start resorption. After ~60 days, osteoblasts initiate bone formation. Although it takes 2 weeks to deposit ~60% of the mineral content of new bone, full mineralization takes several months. Remodeling occurs at ~1–2 million sites.Citation11 The osteocytes are imbedded in the mineralized bone; their role is to sense bone strains and communicate with neighboring osteoblasts and osteoclasts.
All bones are constructed with an envelope of compact bone (cortical bone), which encloses the trabecular bone and marrow spaces. The ratio between compact and trabecular bone varies with ~10% compact and 90% trabecular bone in both the spine and maxilla, whereas the ratio in the mandible is close to that of the distal radius and other long bones: 80% compact and 20% trabecular bone.Citation1 Because of its construction as a network of trabeculae, plates and rods, trabecular bone has a total surface ten times larger than compact bone. Consequentially, it has more endosteal surfaces, more cells, and more remodeling.Citation14
Bone turnover speed has been examined in adult dogs, where alveolar, trabecular bone remodeling in the mandible is double that in the maxilla (37%/year versus 19%/year) and six times faster than in the femur (6.4%/year).Citation15 In addition, the rate of alveolar bone turnover at the alveolar crest is twice the rate of bone turnover at the level of the mandibular canal and three to five times the rate of the mandible at the inferior compact border.Citation16 No exact remodeling rate has been established for human beings, but alveolar, trabecular bone remodels very quickly, especially in the mandible. The remodeling rate was estimated by the number of formation and resorption foci per area in autopsy materials.Citation1
Hormones
Delayed puberty decreases bone mineral density (BMD) and spinal growth. Males with late puberty have longer legs and lower bone density than those with early puberty.Citation17 Males retain hormone protection throughout life and suffer half as many fractures as females.Citation18 In females, early menarche and early menopause are considered to have a strong relationship with high and low BMD, respectively.Citation19 Early menarche is associated with a significant decrease in fracture risk, whereas delayed menarche, as seen in amenorrheic athletes, increases fracture risk.Citation20 Age-related (nonsex-hormone dependent) bone loss may begin in the third decade of life in both sexes at the spine and a decade later at the appendicular sites. With aging, compact bone strength is diminished by approximately 15%–20% and trabecular bone strength by ~50%.Citation10
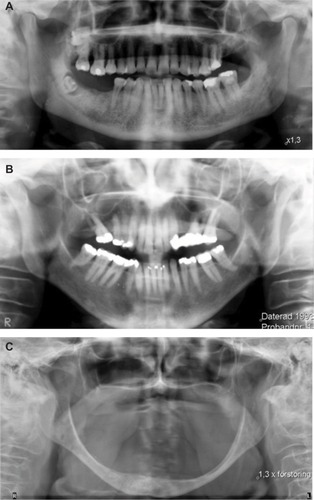
The estrogen-related bone loss in females takes place predominantly in the trabecular bone with its larger endosteal surfaces, followed by a slower loss of both trabecular and cortical bone. Decreasing levels of estrogen are thought to be responsible for increased bone resorption and decreasing testosterone levels for decreased bone formation.Citation11,Citation21 Testosterone is associated with bone apposition periosteally even in aged males, and, therefore, what is lost endosteally may be compensated periosteally in males, but not in females.Citation22 In , the large variations of bone loss and gain in 80 years olds are shown. illustrates dense trabecular bone and extremely thick basal compact bone in an old male. demonstrates the sparser trabeculation, larger intertrabecular spaces, and the thin, eroded basal bone in an old female. In , the extremely resorbed mandible in an edentulous female, also 80 years old, is presented. Age is strongly correlated with BMD in females but not in males, whereas bone size is more correlated with BMD in males than females.Citation23
Figure 1 The three panoramic radiographs show the large variation in bone mass, trabeculation, and basal cortex in persons 79- or 80-years-old.
Hormones influence the jaws and the rest of the skeleton to the same extent but with dissimilarities concerning loading, which, besides genetic factors and hormones, is the strongest factor influencing bone density.Citation11,Citation21
Loading
Weight-bearing physical activities increase skeletal bone mass,Citation24 whereas space flight decreases bone mass.Citation25 Increased loading leads to periosteal apposition (on the outer surface of compact bone), thereby increasing the cross-sectional area in the vertebraeCitation26 and long bones.Citation27 The legs and spine are “loaded” bones, the arms and the mandible half-loaded, and the skull relatively unloaded. As an example, weight-lifters have 3% higher BMD for the total body and 12% for the hip, whereas BMD for the upper part of the skull was 10% lower than in controls.Citation28 Furthermore, after hip fracture, BMD decreases in legs and spine, remains the same in the arms, and increases in the skull.Citation29
Exercise by the elderly (>65 years) is associated with improved muscle strength, coordination, balance, and decreased fall frequency, and there is an association between continued physical activity throughout life and lower hip fracture risk.Citation20
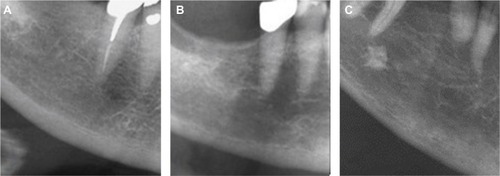
Effects of loading are seen in the same way in the jaws, where the alveolar bone mass and the cross-sectional dimension of the alveolar bone in growing rats increase with increasing functional loading.Citation30,Citation31 Bone mass can be redistributed to the most loaded sites to fortify the bone where it is most needed. When vertical trabeculae are resorbed, the horizontal trabeculae may be fortified (). Bone around human molars is generally denser than the bone around premolars and canines, which can be explained by the findings that the highest biting force is recorded in the molar area.Citation32
Figure 2 The radiograph is of a 48-year-old osteoporotic female. The trabecular network is disrupted in two locations around the second premolar.

After tooth extraction, reduced function leads to local bone loss,Citation33,Citation34 and great interindividual variation in the remodeling pattern of the edentulous areas, with some individuals losing little bone, and others undergoing extensive resorption ().Citation35–Citation37 However, no association, or only a weak one, has been found between skeletal bone mass and residual ridge resorption.Citation37–Citation39
Local factors, such as occluding tooth pairs and the size of the masseter muscles, influence the distal area of the mandible. In patients with heavy occlusion, bruxism, the jaw bone may be denser than the skeletal bones, and therefore symptoms of skeletal osteopenia may become masked in the jaws.Citation40 However, if trabeculation is sparse in areas with occluding teeth (areas under bridge pontics excluded), it is an indication that something is “wrong”, bone formation may be impaired, and fracture risk increased.Citation41,Citation42 Thus, mandibular bone often reflects the condition of the skeleton but differences in loading should be considered.
Bone size and alveolar process width
In females, the mandibular alveolar bone thickness is correlated with BMD.Citation43 The alveolar bone is mostly thicker in the apical part in females with normal BMD compared to the crestal part, whereas it is significantly thinner in osteopenic and osteoporotic females.Citation43
A decreased bone size with time seems to be specific to the alveolar process, as it has not been recorded in any other bone. Not only has it been seen in edentulous regionsCitation35,Citation36 but also in dentate areas,Citation44 where the largest decrease after 5 years was found in perimenopausal females. A decreased buccolingual dimension in the dentate alveolar process may be caused by periosteal resorption of this area, and the largest size changes correspond to areas where resorption was most evident in the modeling process during mandibular growth in young individuals.Citation45
Skeletal bone loss/osteoporosis
Osteoporosis occurs when bone mass decreases faster than it is replaced. It is a multifactorial disease characterized by low bone mass and deterioration of bone microarchitecture, leading to bone fragility and a subsequent increase in fracture risk.Citation46 Osteoporosis may be the result of a deficiency of sex hormone, hyperparathyroidism, hyperthyroidism, chronic renal failure, posttransplantation, or medication with glucocorticosteroids.Citation46
Fracture risk increases exponentially with age, due not only to a decrease in BMD but also to the increased rate of falls among the elderly. Relatively, osteoporotic females have more fractures than nonosteoporotic, but up to 70% of all fractures, in absolute numbers, occur in osteopenic females.Citation47 In a 15-year follow-up, the best predictors of future fracture were a previous fracture and glucocorticoid medication followed by alveolar bone texture, rheumatoid arthritis, gastrointestinal disease, and secondary osteoporosis.Citation7 All variables, except alveolar bone texture, are identical with those identified by the large meta-analyses, on which the World Health Organization Fracture Risk Assessment Tool is based.Citation48 Also included in the Fracture Risk Assessment Tool are age, sex, height, weight, smoking, alcohol, and parents with fractured hip.Citation48
Osteoporosis affects ~75 million people in the Western world, causing >2.3 million fractures a year in Europe and the US.Citation48 Osteoporotic fractures lead to a high morbidity and mortality rate, and BMD predicts survival for subjects over 70 years of age.Citation49 Bone strength depends on the degree of mineralization, bone size, and microstructural features, such as relative trabecular volume, trabecular spacing, and connectivity.Citation50
Measurements of compact bone in the mandible for assessment of osteoporosis
Measurements of bone mass and density in the mandible have been performed since the 1980sCitation1 with different techniques, but most are not useful in the dental clinic, being too complicated, costly, or having an excessively high radiation dose. The dual X-ray absorptiometry method, which is the gold standard for diagnosis of osteoporosis, has low radiation, but for the jawbones, it is only applicable in edentulous individuals, and therefore other methods have been developed.
Maxillary bone consists mostly of trabecular bone, and compact bone is too thin for use as an osteoporosis indicator. Maxillary trabecular bone has been assessed but not as frequently as the mandible due to the difficulty of finding a standard site.Citation51,Citation52
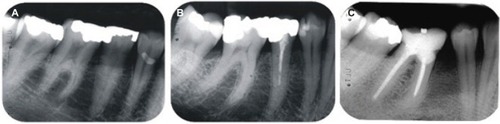
The largest proportion of mandibular compact bone is situated in the inferior cortex, which is well imaged on panoramic radiographs. The mandibular cortical index (MCI) is the most frequently used method in osteoporosis studies.Citation53–Citation56 Compact bone lying distal to the mental foramen is categorized by three groups (): normal cortex (MCI-1) having a relatively even endosteal margin; moderately eroded cortex (MCI-2) with semilunar defects, and severely eroded cortex (MCI-3) with heavy endosteal porosities. A severely eroded compacta is associated with osteoporosis,Citation5,Citation55–Citation57 but not consistently with fracture.Citation8,Citation57 Compact bone loss is seen ~20 years later than trabecular bone loss, which can be seen in females as young as 38 years old.Citation8,Citation9
Figure 3 Visual index for assessment of cortical shape.
The thickness of the basal compacta increases up to the age of 50 years and decreases significantly thereafter.Citation8 A cortex thickness <3 mm is associated with osteoporosisCitation57–Citation60 but not fracture.Citation8,Citation57 The severely eroded inner cortex in MCI-3 creates difficulties when measuring cortex thickness. Therefore, a computer-based method has been developed.Citation60
Measurements of trabecular bone in the mandible for assessment of osteoporosis
Mandibular trabecular bone becomes denser in the jaws from puberty to middle age,Citation61 thereafter, alveolar trabecular bone becomes sparser in most females,Citation1,Citation8,Citation62 whereas males more often maintain their trabecular pattern ().
Trabecular bone structure can be assessed on radiographs by the thickness of the trabeculae, the spacing between the trabeculae, trabecular connectivity,Citation62–Citation64 and by measuring trabecular volume by computed tomography and magnetic resonance. However, the cost and complexity of these methods limit their utility for routine use.Citation63–Citation66 Therefore, a simple three-step visual index has been introduced. It was initially meant for bone evaluation before implant treatment,Citation67 but the index has been proven a valuable indicator for osteoporosis riskCitation4,Citation23,Citation41,Citation42,Citation51 and for fracture risk assessment.Citation6–Citation9
The index classifies the mandibular premolar bone, which is the standard site, as having either sparse, mixed dense plus sparse, or dense trabecular bone ().Citation41,Citation67 Sparse trabeculation has large intertrabecular spaces in most of the alveolar processes, especially in the crestal, dentate, and premolar area. Dense trabeculation has small intertrabecular spaces and well-mineralized trabeculae in the entire radiographed area. Mixed dense plus sparse trabeculation is mostly dense crestally and sparse apically. In case of uncertainty, the mixed category is chosen. Most important is identifying individuals with sparse trabeculation because of their high fracture risk. Dense trabeculation is protective. Most individuals have mixed dense and sparse trabeculation in the mandible; BMD varies greatly in this trabeculation group and fracture risk is moderate. The older the participants, the better the fracture prediction.Citation8,Citation9
Figure 4 Visual index for assessment of trabecular bone.
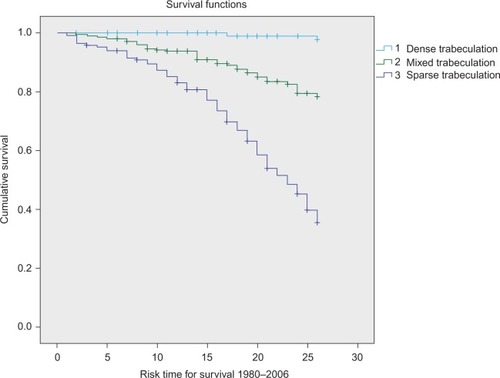
The Kaplan–Meier curve in shows the graded association between trabecular density and fracture risk.Citation9 All participants start free of fracture. The upper curve describing dense trabeculation remains relatively stable, which means ~90% of those with dense trabeculation stay free of fracture during the period 1980–2006, whereas the lowest curve describing sparse trabeculation dives distinctly; only 25% remained fracture free. The curve in between for mixed dense plus sparse also dives, illustrating ~62% free of fracture at the end of the 26-year follow-up. The hazard ratio of future fracture for sparse trabeculation compared to mixed trabeculation was 2.9 (95% CI: 2.2–3.8, P<0.0001) and for dense versus mixed trabeculation 0.21 (95% CI: 0.1–0.4, P<0.0001).Citation9
Figure 5 Kaplan–Meier survival curve showing cumulative “fracture” survival and risk time for fracture in three different trabeculation groups.
When the visual trabecular pattern was tested in males, it was not a significant factor for the prediction of osteoporosis,Citation23 but significant for fracture prediction.Citation6
Trabeculation does not change visually after 5 years,Citation42 but radiographs of females performed after 12 and 24 years show a gradual transformation with increased intertrabecular spaces and less mineralized trabeculae.Citation8,Citation9 Similar bone changes to those that could be seen after 12 years in the mandible could be measured in the radius after 1 year using three-dimensional, high-resolution, peripheral quantitative computed tomography.Citation6 In females (mean age 77 years), total density and trabecular number decreased, while trabecular thickness, separation, and heterogeneity increased.Citation68
Both the trabecular visual index and the automated methods work best on intraoral radiographs, which are most widely used in dental practices. With training, the visual trabecular index can be used on panoramic radiographs but the noise level is larger.Citation69
Periodontitis
Periodontitis is induced by specific bacteria from biofilms on tooth surfaces, which triggers an immunoinflammatory response in the adjacent bone tissue. Bacteria are required to initiate the disease process where host proteolytic enzymes mediate direct destruction of the periodontal tissue.Citation70 The progression of periodontitis is influenced by factors such as genetics, general health, smoking, and diet. Furthermore, education and socioeconomic factors are determinants.Citation70 Severe periodontitis is linked to some systemic diseases, for example, diabetes mellitus,Citation71–Citation73 cardiovascular disease,Citation74–Citation76 rheumatoid arthritis,Citation77 and adverse pregnancy outcomes.Citation78
Periodontitis and osteoporosis both progress with advancing age, smoking, estrogen deficiency, and family history.Citation79 Current knowledge regarding the effects of osteoporosis or osteopenia on periodontal disease and alveolar bone loss is inconclusive.Citation12,Citation80–Citation91 Some previous studies have indicated a relationship between periodontal disease and osteoporosis,Citation83–Citation87 while others have not shown any significant relationship.Citation88,Citation89 The lack of consistency in the results may be due to differences in the alveolar bone structure and thickness, which were not considered. This could be supported by the fact that individuals with high mineral levels in the skeleton seem to retain their teeth with deep periodontal pockets more easily than those with osteoporosis.Citation91 Furthermore, individuals with broad, dense jaws have more bone substances to lose than those with thin jaws, and therefore the size of an individual may play an important role for the vertical changes of the alveolar process.Citation91
The multifactorial etiology and confounding factors have limited the understanding of the relationship between osteoporosis and periodontitis. The coarseness of trabeculation may be one such confounding factor. In a new report, the group with sparse trabeculation had more skeletal bone loss, lower BMD, and larger marginal bone level decrease after 5 years than those with not-sparse trabeculation, but surprisingly the little group with dense trabeculation experienced both the greatest 5-year skeletal bone loss and marginal bone level decrease.Citation92 The reason may be that dense trabeculation implies the greatest trabecular endosteal bone surface, and consequently the largest number of bone cells and remodeling sites. Negative events may lead to the most negative responses in dense trabecular bone but research is warranted to clarify whether dense trabeculation leads to the best results after appropriate treatment?
Estrogen deficiency influences BMD,Citation21,Citation93,Citation94 and the remodeling of the alveolar process negatively, whereas treatment with hormone replacement therapy ameliorates the periodontal condition and local bone mass.Citation85,Citation95
Patients with cancer and bisphosphonate-related osteonecrosis of the jaw have significantly fewer teeth, and lower average bone height compared to controls after adjusting for the number of bisphosphonate infusions.Citation96 The antiresorptive effect of bisphosphonates is therapeutic when used in treatment of osteoporosis for a limited period, but the problem is the extremely long elimination time due to large accumulations of bisphosphonate in bone, diminishing bone turnover and preventing bone renewal.Citation16
Clinical relevance
To maintain quality of life for the elderly, targeting individuals with high fracture risk is an important challenge to the dentist. An assessment of the trabecular bone can easily be included in an annual examination.
The trabeculation pattern is of direct interest to the dental profession, since a dense trabeculation indicates a need to exercise prudence when drilling for implants because of increased heating and consequently increased risk of local necrosis.Citation97 A periapical radiograph revealing sparse trabeculation may indicate a need for cortical fixation and long duration of the healing process before the implant can be loaded.Citation98
In adult orthodontics, a different tissue reaction could be expected when teeth are moved with sparse or dense trabeculation. This could be supported by the findings that rats with lower initial bone density have a faster orthodontic tooth movement than rats with significantly higher initial bone density.Citation99 Orthodontic tooth movement is faster in lactating rats on a calcium-deficient diet than in rats on a normal diet.Citation100 Dense trabeculation implies that extraction and surgical extirpation of wisdom teeth are more complicated and probably more difficult to obtain full anesthesia.
Because dentists are in an ideal position to assess oral bone loss on radiographs, they may be the first to discover early signs of osteoporosis. Identifying individuals with high fracture risk before the first fracture occurs is important in order to avoid suffering and minimize high costs to society. If these patients can be easily identified by a dentist, they can improve their bone quality through training and nutrition, and appropriate medication for older people can be prescribed.
Disclosure
The authors report no conflicts of interest in this work.
References
- Von WowernNBone mass of mandibles. In vitro and in vivo analysesDan Med Bull19863323443948537
- KribbsPJChesnutCHOttSMKilcoyneRFRelationships between mandibular and skeletal bone in an osteoporotic populationJ Prosthet Dent1989627037072585328
- SouthardKASouthardTESchlechteJAMeisPAThe relationship between the density of the alveolar process and that of post-cranial boneJ Dent Res20007996496910831099
- LindhCHornerKJonassonGThe use of visual assessment of dental radiographs for identifying women at risk of having osteoporosis: the OSTEODENT projectOral Surg Oral Med Oral Pathol Oral Radiol Endod200810628529318299223
- BollenAMTaguchiAHujoelPPHollenderLGCase-control study on self-reported osteoporotic fractures and mandibular cortical boneOral Surg Oral Med Oral Pathol Oral Radiol Endod20009051852411027391
- Hassani-NejadAAhlqwistMHakebergMJonassonGMandibular trabecular bone as fracture indicator in 80-year-old men and womenEur J Oral Sci201312152553124102691
- JonassonGBillhultAMandibular bone structure, bone mineral density, and clinical variables as fracture predictors: a 15-year follow-up of female patients in a dental clinicOral Surg Oral Med Oral Pathol Oral Radiol201311636236823953422
- JonassonGSundhVHakebergMHassani-NejadALissnerLAhlqwistMMandibular bone changes in 24 years and skeletal fracture predictionClin Oral Investig201317565572
- JonassonGSundhVAhlqwistMHakebergMBjörkelundCLissnerLA prospective study of mandibular trabecular bone to predict fracture incidence in women: a low-cost screening tool in the dental clinicBone20114987387921777710
- MartinBAging and strength of bone as a structural materialCalcif Tissue Int199353S34S408275378
- LernerUHBone remodeling in post-menopausal osteoporosisJ Dent Res20068558459516798857
- ReddyMSMorganSLDecreased bone mineral density and periodontal managementPeriodontol 200020136119521823240950
- SeemanEDelmasPDBone quality – the material and structural basis of bone strength and fragilityN Engl J Med20063542250226116723616
- KanisJAOsteoporosisOxfordBlackwell Science Ltd1994
- HujaSSFernandezSAHillKJLiYRemodeling dynamics in the alveolar process in skeletally mature dogsAnat Rec Discov Mol Cell Evol Biol200628812431249
- MarxRECillo JrJEUlloaJJOral bisphosphonate-induced osteonecrosis: risk factors, prediction of risk using serum CTX testing, prevention, and treatmentJ Oral Maxillofac Surg2007652397241018022461
- LorentzonMNorjavaaraEKindblomJMPubertal timing predicts leg length and childhood body mass index predicts sitting height in young adult menJ Pediatr201115845245720961561
- SBUOsteoporosis - prevention, diagnosis and treatment. Stockholm: Swedish Council on Health Technology Assessment in Health Care (SBU)SBU report 165/12003
- ItoMYamadaMHayashiKOhkiMUetaniMNakamuraTRelation of early menarche to high bone mineral densityCalcif Tissue Int19955711147671158
- KarlssonMBassSSeemanEThe evidence that exercise during growth or adulthood reduces the risk of fragility fractures is weakBest Pract Res Clin Rheumatol20011542945011485339
- RiggsBLKhoslaSMeltonLJIIISex steroids and the construction and conservation of the adult skeletonEndocrin Rev200223279302
- UlmCWSolarPUlmMRMatejkaMSex-related changes in the bone mineral content of atrophic mandiblesCalcif Tissue Int1994542032078055367
- JonassonGJonassonLKiliaridisSSkeletal bone mineral density in relation to thickness, bone mass, and structure of the mandibular alveolar process in dentate men and womenEur J Oral Sci200711511712317451501
- LanyonLEFunctional strain in bone tissue as an objective, and controlling stimulus for adaptive bone remodellingJ Biomech198720108310933323200
- LangTFWhat do we know about fracture risk in long-duration spaceflight?J Musculoskelet Neuronal Interact2006631932117185806
- MosekildeLAge-related changes in bone mass, structure, and strength – effects of loadingZ Rheumatol200059Suppl 11910769428
- RuffCBHayesWCSex differences in age-related remodeling of the femur and tibiaJ Orthop Res198868868963171769
- KarlssonMKHasseriusRObrantKJBone mineral density in athletes during and after career: a comparison between loaded and unloaded skeletal regionsCalcif Tissue Int1996592452488781046
- MagnussonHObrantKJohnellOKarlssonKMBone mass changes in weight- loaded and unloaded skeletal regions following a fracture of the hipOsteoporos Int2001697883
- BresinAJohanssonCBKiliaridisSEffects of occlusal strain on the development of the dentoalveolar process in the growing ratEur J Exp Musculoskel Res19943112122
- KiliaridisSBresinAHolmJStridKGEffects of masticatory muscle function on bone mass in the mandible of the growing ratActa Anat19961552002058870788
- ErhardsonSSheikholeslamAForsbergC-MLockowandtPVertical forces developed by the jaw elevator muscles during unilateral maximal clenching and their distribution on teeth and condylesSwed Dent J19931723348362360
- ElovicRPHippJAHayesWCMaxillary molar extraction causes increased bone loss in the mandible of ovariectomized ratsJ Bone Miner Res199510108710937484284
- Von WowernNHjorting-HansenEStoltzeKChanges in bone mass in rat mandibles after tooth extractionInt J Oral Surg19798229233118129
- CarlssonGEPerssonGMorphologic changes of the mandible after extraction and wearing of dentures; a longitudinal, clinical, and X-ray cephalometric study covering 5 yearsOdontol Revy19671827545227389
- TallgrenAThe continuing reduction of the residual alveolar ridges in complete denture wearers: a mixed-longitudinal study covering 25 yearsJ Prosthet Dent1972271201324500507
- Von WowernNKollerupGSymptomatic osteoporosis: a risk factor for residual ridge reduction of the jawsJ. Prosthet Dent1992676566601527750
- KlemettiEReview of residual ridge resorption and bone densityJ Prosthet Dent1996755125148709016
- KlemettiEKrögerHLassilaVRelationships between body mass index and the remaining alveolar ridgeJ Oral Rehab199724808812
- JonassonGKiliaridisSThe association between the masseter muscle, the mandibular alveolar bone mass and thickness in dentate womenArch Oral Biol2004491001100615485642
- JonassonGBankvallGKiliaridisSEstimation of skeletal bone mineral density by means of the trabecular pattern of the alveolar bone, its interdental thickness, and the bone mass of the mandibleOral Surg Oral Med Oral Pathol Oral Radiol Endod20019234635211552157
- JonassonGJonassonLKiliaridisSChanges in the radiographic characteristics of the mandibular alveolar process in dentate women with varying bone mineral density: a 5-year prospective studyBone20063871472116326156
- JonassonGKiliaridisSGunnarssonRCervical thickness of the mandibular alveolar process and skeletal bone mineral densityActa Odontol Scand19995715516110480282
- JonassonGKiliaridisSChanges in the bucco-lingual thickness of the mandibular alveolar process and skeletal bone mineral density in dentate women: a 5-yr prospective studyEur J Oral Sci2005113211412015819816
- EnlowDHHarrisDBA study of the postnatal growth of the human mandibleAm J Orthodont1964502550
- WHO Scientific GroupPrevention and management of osteoporosisWHO Technical Report Series 921GenevaWHO Press2003
- PascoJASeemanEHenryMJMerrimanENNicholsonGCKotowiczMAThe population burden of fractures originates in women with osteopenia, not osteoporosisOsteoporos Int2006171404140916699736
- KanisJAJohnellOOdenAJohanssonHMcCloskeyEFRAX™ and the assessment of fracture probability in men and women from the UKOsteoporos Int20081938539718292978
- JohanssonCBlackDJohnellOOdénAMellströmDBone mineral density is a predictor of survivalCalcif Tissue Int1998631901969701621
- GenantHKJiangYAdvanced imaging assessment of bone qualityAnn N Y Acad Sci2006106841042816831940
- LindhCObrantKPeterssonAMaxillary bone mineral density and its relationship to the bone mineral density of the lumbar spine and hipOral Surg Oral Med Oral Pathol Oral Radiol Endod20049810210915243479
- SouthardKASouthardTEDetection of simulated osteoporosis in human anterior maxillary alveolar bone with digital subtractionOral Surg Oral Med Oral Pathol1994786556617838476
- KlemettiEKolmakovSKrögerHPantomography in assessment of the osteoporosis risk groupScand J Dent Res199410268728153584
- TaguchiAAsanoAOhtsukaMObserver performance in diagnosing osteoporosis by dental panoramic radiographs: results from the osteoporosis screening project in dentistry (OSPD)Bone20084320921318482878
- TaguchiATsudaMOhtsukaMUse of dental panoramic radiographs in identifying younger postmenopausal women with osteoporosisOsteoporos Int20061738739416331360
- WhiteSCTaguchiAKaoDClinical and panoramic predictors of femur bone mineral densityOsteoporos Int20051633934615726238
- OkabeSMorimotoYAnsaiTAssessment of the relationship between the mandibular cortex on panoramic radiographs and the risk of bone fracture and vascular disease in 80-year-oldsOral Surg Oral Med Oral Pathol Oral Radiol Endod200810643344218299222
- DevlinHKarayianniKMitseaADiagnosing osteoporosis by using dental panoramic radiographs: the OSTEODENT projectOral Surg Oral Med Oral Pathol Oral Radiol Endod200710482182817428694
- HornerKDevlinHHarveyLDetecting patients with low skeletal bone massJ Dent20023017117512450724
- DevlinHAllenPDGrahamJAutomated osteoporosis risk assessment by dentists: a new pathway to diagnosisBone20074083584217188590
- PhamDKiliaridisSEvaluation of changes in trabecular alveolar bone during growth using conventional panoramic radiographsActa Odontol Scand20127012713221793639
- WhiteSCRudolphDJAlterations of the trabecular pattern of the jaws in patients with osteoporosisOral Surg Oral Med Oral Pathol Oral Radiol Endod19998862863510556761
- WhiteSCAtchisonKAGornbeinJAChange in mandibular trabecular pattern and hip fracture rate in elderly womenDentomaxillofac Radiol20053416817415897288
- VerheijJGGeraetsWGvan der SteltPFPrediction of osteoporosis with dental radiographs and ageDentomaxillofac Radiol20093843143719767512
- ChibaKBurghardtAJOsakiMMajumdarSHeterogeneity of bone microstructure in the femoral head in patients with osteoporosis: an ex vivo HR-pQCT studyBone20135613914623748104
- GeraetsWGVerheijJGvan der SteltPFPrediction of bone mineral density with dental radiographsBone2007401217122117317351
- LindhCPeterssonARohlinMAssessment of the trabecular pattern before endosseous implant treatment: diagnostic outcome of periapical radiography in the mandibleOral Surg Oral Med Oral Pathol Oral Radiol Oral Endod199682335343
- KawalilakCEJohnstonJDOlszynskiWPKontulainenSACharacterizing microarchitectural changes at the distal radius and tibia in postmenopausal women using HR-pQCTOsteoporos Int2014252057206624781379
- PhamDJonassonGKiliaridisSAssessment of trabecular pattern on periapical and panoramic radiographs: a pilot studyActa Odontol Scand201068919720085501
- BartoldPMVan DykeTEPeriodontitis: a host-mediated disruption of microbial homeostasis. Unlearning learned conceptsPeriodontol 200020136220321723574467
- Santos TunesRFoss-FreitasMCNogueira-FilhoGRImpact of periodontitis on the diabetes-related inflammatory statusJ Can Dent Assoc201076a3520831852
- KoromantzosPAMakrilakisKDerekaXKatsilambrosNVrotsosIAMadianosPNA randomized, controlled trial on the effect of nonsurgical periodontal therapy in patients with type 2 diabetesJ Clin Periodontol20113814214721114680
- ChappleILGencoRworking group 2 of the joint EFP/AAP workshopDiabetes and periodontal diseases: consensus report of the Joint EFP/AAP Workshop on Periodontitis and Systemic DiseasesJ Periodontol201384S106S11223631572
- BuhlinKGustafssonAPockleyAGFrostegårdJKlingeBRisk factors for cardiovascular disease in patients with periodontitisEur Heart J2003242099210714643270
- BelstrømDDamgaardCNielsenCHHolmstrupPDoes a causal relation between cardiovascular disease and periodontitis exist?Microbes Infect20121441141822200601
- TonettiMSVan DykeTEPeriodontitis and atherosclerotic cardiovascular disease: consensus report of the joint EFP/AAP workshop on periodontitis and systemic diseasesJ Periodontol201384242922420871
- KaurSWhiteSBartoldPMPeriodontal disease and rheumatoid arthritis: a systematic reviewJ Dent Res20139239940823525531
- SanzMKornmanKWorking group 3 of the joint EFP/AAP workshop. periodontitis and adverse pregnancy outcomes: consensus report of the joint EFP/AAP workshop on periodontitis and systemic diseasesJ Periodontol201384S164S16923631576
- LernerUHInflammation-induced bone remodeling in periodontal disease and the influence of post-menopausal osteoporosisJ Dent Res20068559660716798858
- ChesnutCH3rdThe relationship between skeletal and oral bone mineral density: an overviewAnn Periodontol2001619319611887464
- JeffcoatMThe Association between osteoporosis and oral bone lossJ Periodontol2005762125213216277585
- Otomo-CorgelJOsteoporosis and osteopenia: implications for periodontal and implant therapyPeriodontol. 200020125911113922507063
- HildeboltCFPilgramTKYokoyama-CrothersNAlveolar bone height and postcranial bone mineral density: negative effects of cigarette smoking and parityJ Periodontol20007168368910872947
- PayneJBReinhardtRANummikoskiPVPatilKDLongitudinal alveolar bone loss in postmenopausal osteoporotic⁄osteopenic womenOsteoporos Int199910344010501777
- TezalMWactawski-WendeJGrossiSGHoAWDunfordRGencoRJThe relationship between bone mineral density and periodontitis in postmenopausal womenJ Periodontol2000711492149811022780
- YoshiharaASeidaYHanadaNMiyazakiHA longitudinal study of the relationship between periodontal disease and bone mineral density in community-dwelling older adultsJ Clin Periodontol20043168068415257747
- Wactawski-WendeJHausmannEHoveyKTrevisanMGrossiSGencoRJThe association between osteoporosis and alveolar crestal height in postmenopausal womenJ Periodontol2005772116212416277584
- EldersPJHabetsLLNetelenbosJCvan der LindenLWvan der SteltPFThe relation between periodontitis and systemic bone mass in women between 46 and 55 years of ageJ Clin Periodontol1992194924961430285
- KinaneDFMarshallGJPeriodontal manifestations of systemic diseaseAust Dent J20014621211355236
- CivitelliR1PilgramTKDotsonMAlveolar and postcranial bone density in postmenopausal women receiving hormone/estrogen replacement therapy: a randomized, double-blind, placebo-controlled trialArch Intern Med2002241621409141512076241
- KlemettiECollinHLForssHMarkkanenHLassilaVMineral status of skeleton and advanced periodontal diseaseJ Clin Periodontol1994211841888157771
- JonassonGFive-year alveolar bone level changes in women of varying skeletal bone mineral density and bone trabeculationOral Surg Oral Med Oral Pathol Oral Radiol2015120869326093684
- RizzoliRBonjourJ-PHormones and bonesLancet1997349120123
- RiggsBLKhoslaSAtkinsonEJDunstanCRMeltonLJIIIEvidence that type I osteoporosis results from enhanced responsiveness of bone to estrogen deficiencyOsteoporos Int20031472873312879223
- JacobsRGhyselenJKoninckxPvan SteenbergheDLong-term bone mass evaluation of mandible and lumbar spine in a group of women receiving hormone replacement therapyEur J Oral Sci199610410168653490
- Thumbigere-MathVMichalowiczBSHodgesJSPeriodontal disease as a risk factor for bisphosphonate-related osteonecrosis of the jawJ Periodontol20148522623323786404
- FribergBJemtTLekholmUEarly failures in 4,641 consecutively placed Brånemark dental implants: a study from stage 1 surgery to the connection of completed prosthesesInt J Oral Maxillofac Implants199161421461809668
- FribergBEkestubbeAMellstromDSennerbyLBranemark implants and osteoporosis: a clinical exploratory studyClin Implant Dent Relat Re200135056
- BridgesTKingGMohammadAThe effect of age on tooth movement and mineral density in the alveolar tissue of the ratAm J Orthod Dentofacial Orthop1988932452503422781
- GoldieRSKingGJRoot resorption and tooth movement in orthodontically treated, calcium-deficient, and lactating ratsAm J Orthod1984854244306586081

