Abstract
Aim
The objective of this article is to evaluate the relationship between the changes in prescriptions of antiosteoporotic drugs (mainly the rapid fall in the use of bisphosphonates [BPs]) and standardized hip fracture (HF) rates over the period 2005–2008 in the Australian Capital Territory (ACT).
Methods
Annual sex- and age-specific HF rates (per 100,000 population) were determined and standardized using the Australian 2006 population census. Data on the annual prescriptions of BPs (mainly alendronate and risedronate), strontium ranelate, and hormone replacement therapy were obtained from the Australian Pharmaceutical Benefits Scheme (PBS) and Repatriation Australian Pharmaceutical Benefits Scheme (RPBS) databases.
Results
In the ACT, the peak annual number of prescriptions for BPs was observed in 2006. Following reports linking osteonecrosis of the jaw with BP use, the number of BP prescriptions dropped by 14% in 2007–2008 compared with 2005, when the lowest HF rates were recorded. The reduction in BP prescriptions coincided with increased HF rates in females in 2007 (+22.6%) and in 2008 (+25.2%) compared with 2005; in males, HF incidence declined by 6.6% and 16.7%, respectively. The proportion of filled prescriptions for strontium ranelate, risedronate, and alendronate in 2007–2008 was 1:8.4:15.5, indicating that BPs were the dominant antiosteoporotic drugs. There was an inverse statistically significant relationship between the total annual number of BP prescriptions and standardized HF incidence rates for the 10-year period 1999–2008.
Conclusion
Although currently there is no clear understanding of factors contributing to changing HF epidemiology, the available evidence suggests that much of the decline in HF rates is due to the use of BPs. The fall in the use of BPs is associated with an increase in HF rates in females, indicating that BPs should still be considered the first-line medications for the prevention and treatment of osteoporosis. Our results need to be confirmed in other populations and countries.
Introduction
In the past decade, bisphosphonates (BPs) have become the cornerstone in the treatment of osteoporosis. Their effectiveness in reducing fracture risk, including hip fracture (HF), safety, and good tolerability, has been demonstrated in multiple randomized, placebo-controlled clinical studies.Citation1–Citation4 The use of these drugs has also been shown to be cost-effective for the prevention and treatment of fractures associated with osteoporosis in the older adult population.Citation5–Citation7 However, the effectiveness of BPs in the general population is less certain.Citation8 In a community cohort of postmenopausal women at risk (bone mineral density [BMD] T-score ≤2, or prior fracture), the incidence of fractures in patients who received BPs did not differ from those who did not.Citation9 A recent studyCitation10 on HF prevention in long-term care concluded that there is little evidence to apply existing evidence on osteoporosis treatment to this population, as frail older adults are often neglected in clinical trials.
However, in the province of Ontario, Canada, a decrease in wrist fracture and HF rates from 1997 to 2003 was associated with a significant increase in the number of BMD tests with dual-energy X-ray absorptiometry (DXA) and prescriptions of antiresorptive drugs (mainly etidronate).Citation11 Similarly, an analysis of a large population of BP users in the United States who were followed for 2 years demonstrated that adherence to BP therapy was associated with significantly fewer osteoporotic fractures, including HFs.Citation12 In a previous ecologic study,Citation13 we also found that, coincident with increased prescribing of BPs (in Australia, this treatment became widely available in 2000), HF incidence rates progressively declined (statistically significant in females only), and the lowest rates were recorded in 2005.
When reports linking the use of BPs with osteonecrosis of the jaw (ONJ) were published, subsequent alarmist media coverage had a major effect on patient perceptions about the use of BPs, and widespread fear resulted in discontinuation of BP treatment.
The incidence of ONJ associated with oral BP treatment for osteoporosis has been estimated to be between <1Citation4,Citation14,Citation15 and 20–28Citation16,Citation17 in 100,000 patient-years of exposure. No cases of ONJ have been reported in clinical trials of alendronate, risedronate, and ibandronate for osteoporosis indications.Citation18 However, in patients with multiple myeloma, advanced cancer, and metastasis to the skeleton for whom BPs are used in high doses intravenously, the incidence of ONJ may be much higher (1 in 1000), specifically after dental procedures (up to 2%–12% at 36 months’ exposure).Citation19–Citation22
Despite the lack of convincing evidence for a direct causative relationship between ONJ and BPs (especially with low doses used in osteoporosis), a very low incidence of ONJ, and its poorly understood and likely multifactorial pathogenesis,Citation4,Citation16,Citation19,Citation23–Citation26 the use of BPs in Australia is decreasing.
The potential impact of this drop in BP use on the incidence of osteoporotic fractures, including HF, is unknown. From the societal perspective, such data are important for a realistic assessment of the real-world effectiveness of current antiosteoporotic and fracture prevention strategies. The aim of this study was to evaluate the relationship between the changes in prescriptions of antiosteoporotic drugs (mainly the rapid fall in the use of BPs) and standardized HF rates over the period 2005–2008.
Materials and methods
The Australian Capital Territory (ACT) region is well suited for an epidemiological study because all HFs occurring in this area are treated at the Canberra Hospital. In 2008, the ACT had a total population of 352,189 people with 15.1% aged 60 years and above.Citation27 The study was approved by the ACT Human Research Ethics Committee. All the data used for the analysis were anonymous and confidential.
Methods of data collection on HF incidence and antiosteoporotic drugs used were presented in detail in our previous study, which covered the years 1994/95 to 2005/06.Citation13 In brief, we utilized the Canberra Hospital electronic administrative database to identify patients discharged with a diagnosis of HF and excluded all readmissions and reoperations, as well as patients with pathological HF (primary or metastatic bone cancer, multiple myeloma, or Paget’s disease). In this study, only cervical and trochanteric fractures of the proximal femur were included, and subtrochanteric and shaft fractures were excluded. Annual sex- and age-specific incidence rates (per 100,000 population) were determined using data from the Australian Bureau of Statistics. Annual HF incidence rates were age- and sex-standardized by the direct method using the Australian 2006 population census as standard. Standardization provides estimates that can be compared directly from one year to another without the confounding effects of the aging of the population and changes in sex distribution.
Data on the annual prescriptions of BPs (mainly alendronate and risedronate), strontium ranelate (approved in Australia in 2006), and hormone replacement therapy (HRT oral or transdermal estrogen only or combined estrogen–progesterone prescriptions) were obtained from the Australian Pharmaceutical Benefits Scheme (PBS) and Repatriation Australian Pharmaceutical Benefits Scheme (RPBS) databases.Citation28 All doses of the aforementioned drugs were considered.
The prescriptions analyzed in this dataset (provided under government subsidy) are restricted to two groups: 1) patients aged 70 years or above with demonstrated low BMD (BMD T-score <−3), and 2) patients with demonstrated fracture due to minimal trauma. Therefore, it can be reasonably postulated that most patients receiving BPs were older adults who are at high risk of fracture. Although private (non-PBS) prescriptions are available, the numbers are low. A marked increase occurred from 2001 when BPs became available as PBS prescriptions. Because vitamin D and calcium supplements are not covered by PBS/RPBS and use of raloxifene and parathyroid hormone (PTH) analogs (teriparatide) was minimal, these preparations were not included in the analysis.
Statistical analysis
Statistical analysis was performed using Stata Version 10 (Stata Corp, College Station, TX, USA). The relationship between HF incidence rate and antiosteoporotic drugs use was examined by calculation of Pearson’s correlation coefficient after logarithmic (log) transformation of variables with skew distribution and by linear regression analysis. All statistical tests were performed at the two-sided P < 0.05 level of significance.
Results
Incidence of HF
Over the 2006–2008 period, the ACT population aged ≥60 years increased by 13.9% in women and 14.9% in men, and the number of subjects ≥85 years, which represented 1.2% of the total ACT population (34.6% male, 65.36% female), increased by 15.4% in women and by 27.3% in men.
In our region during the last 3 years (2006–2008), there were 494 HFs in older adults (≥60 years), and 72.7% occurred in females. Among females, 53.1% were aged ≥85 years and, among males, 35.6% were aged ≥85 years. In females, the annual numbers of HFs and HF rates during this period progressively increased compared with 2005 (). The crude HF rates among females increased by 11.2% in 2006, 16.2% in 2007, and 22.6% in 2008. The age-specific HF rates in females increased within each group, with the largest absolute increase in those aged ≥85 years (from 2384.3 to 2567.0/100,000 person-years or +182.7 [7.7%]/100,000 person-years from 2007 to 2008) and the largest percentage increase in the age group 70–74 years (from 186.0 to 245.4/100,000 person-years or +31.9% in 2008 compared with 2007). The age-standardized HF rates, which eliminate the effects of the changes in the population structure over time, demonstrate a slightly higher increase: 12.9% in 2006, 22.6% in 2007, and 25.2% in 2008 compared with 2005.
Table 1 Annual absolute number of hip fractures, age- and sex-specific and standardized incidence rates of hip fractures in subjects 60 years of age and older
Among males, the absolute numbers of HFs did not change, but the age-specific rates decreased in 2007 (−8.4%) and 2008 (−17.9%) compared with those in 2005. The age-specific HF rates in 2008 compared with 2007 decreased in those aged 75–79 years (from 348.1 to 170.5 [−177.6]/100,000 person-years, or −51.0%) and in the group 80–84 years of age (from 589.1 to 388.2 [−200.9]/100,000 person-years, or −34.1%), but increased in those aged ≥85 years (from 854.1 to 1276.0 [+421.9]/100,000 person-years, or +49.4%) and 60–74 years of age (from 48.7 to 57.9, or +9.2 [+18.9%]/100,000 person-years). For males, the age-standardized HF rates in 2006 were slightly higher than in 2005 (+7.6%) but lower in 2007 (−6.6%) and 2008 (−16.7%).
Overall in 2008 compared with 2005, age-adjusted HF rates (for females and males) increased by 9.3%, and age-standardized rates increased by 10.5%. The female to male ratio in the standardized HF rates changed from 1.88 in 2005 to 2.82 in 2008, indicating a pronounced increase in HF incidence in women.
Use of BPs and other antiosteoporotic medications and HF incidence
In the ACT, the peak annual number of prescriptions for BPs was observed in 2006. From 2006 to 2008, there has been a steady decline in the number of filled prescriptions for BPs, from 51,271 (2006) to 45,674 (−10.9%) in 2008. In total, the number of prescriptions dispensed in the ACT over 2007–2008 dropped by 6927 or by 14% compared with 2005, when the lowest HF rates were recorded (). Over the same period, the number of HRT prescriptions also continued to decline (−7.6% in 2007 and −12.1% in 2008 compared with 2006). The absolute number of prescriptions for strontium ranelate increased (from 28 in 2006 to 2370 in 2008), but this constitutes only 4.02% of the number of BP prescriptions. The proportion of filled prescriptions for strontium ranelate, risedronate, and alendronate in 2007–2008 was 1:8.4:15.5, indicating that BPs were the dominant antiosteoporotic drugs. In 2007–2008 compared with 2005, among those aged ≥60 years, the absolute number of HFs increased by 75 (all females), and the number of prescriptions for BPs decreased by 6927. This corresponds to a drop of 92.4 prescriptions per one ‘extra’ (unexpected) HF.
Figure 1 Age-adjusted and standardized to 2006 Australian population rates of hip fracture in women and men aged ≥60 years and prescriptions of bisphosphonates, strontium ranelate, and hormone replacement therapy in the Australian Capital Territory from 1999 to 2008.
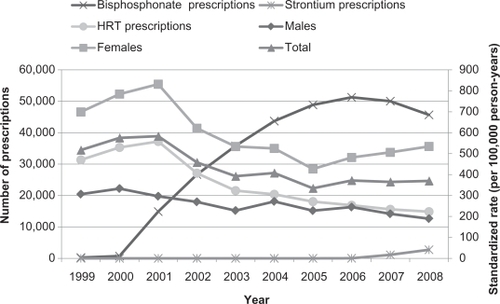
shows that changes in the use of antiosteoporotic drugs, especially BPs, were accompanied by inverse changes in standardized HF rates, particularly in females. After 2001, when BP prescriptions started increasing, the HF rates began to decrease, and this downward trend continued up to 2005, coinciding with a significant increase in BP use. Over the period from 2001 to 2005, the HF incidence declined in total by 42.6% (from 583.0 to 248.6/100,000 person-years), 54.1% in females (from 831.7 to 381.4/100,000 person-years) and 23.2% in males (from 296.5 to 227.6/100,000 person-years). The reduction in BP prescriptions observed in 2007–2008 was associated with increased HF rates in females, whereas male HF rates continued to decline.
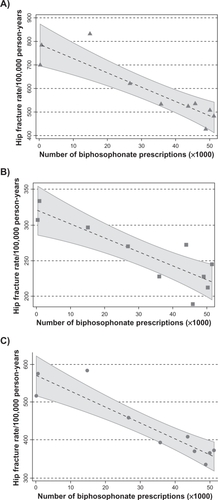
When analyzing the relationship between age-standardized HF rates and BP prescriptions, we calculated Pearson’s correlation coefficient and found a significant inverse relationship between the total annual number of BP prescriptions (log-transformed) and HF rates in the total older adult population (r = −0.735;P = 0.015), in females (r = −0.668;P = 0.027), and in males (r = −0.776;P = 0.008). No significant correlation was found for strontium ranelate. Unfortunately, PBS/RPBS data do not include the gender of the population filling prescriptions for antiosteoporotic medications, so we were unable to analyze the use of BPs separately by females and males.
Linear regression analysis of the relationship between the number of BP prescriptions and standardized HF rates from 1999 to 2008 confirmed the inverse relationship (). As illustrated in , higher BP use was associated with significantly lower HF rates.
Table 2 Linear regression analysis between the number of bisphosphonate prescriptions (×103) and age-standardized hip fracture rates (per 100,000 person-years) in the elderly in 1999–2008 in the Australian Capital Territory
Figure 2 The relationship between the total annual number of prescriptions (×103) for bisphosphonates and age-standardized hip fracture rates (per 100,000 personyears) in A) females, B) males, and C) the total elderly population in the Australian Capital Territory (1999–2008). Regression lines with 95% confidence intervals.
Discussion
The main finding of this ecologic study is an inverse statistically significant relationship between use of osteoporosis treatment, namely the total annual number of BP prescriptions, and standardized HF incidence rates for the 10-year period 1999–2008.
Over the last decade, advances in molecular and cellular biology of bone remodeling have revealed new targets for and novel pharmacological approaches to therapies for osteoporosis. Newer agents include strontium ranelate (capable of both inhibiting bone resorption and increasing bone formation),Citation29,Citation30 new-generation selective estrogen receptor modulators lasofoxifeneCitation31 and bazedoxifene,Citation32 anabolic agents (PTH and its analogs, monoclonal antibody to sclerostin),Citation33–Citation36 and antiresorptive agents such as RANK signaling inhibitors (denosumab), cathepsin K inhibitors (odanacatib, balicatib, and relacatib), and antagonists of α(v)β(3) integrin (L-000845704).Citation34,Citation37–Citation39 Although the newer and emerging therapies as well as combined treatments (eg, with alfacalcidol)Citation2 may be more potent and target-specified,Citation2,Citation33,Citation37,Citation40,Citation41 currently, nitrogen-containing BPs, antiresorptive agents shown to reduce fracture risk by ∼50% at best,Citation42 remain the mainstay for pharmacological treatment of osteoporosis.Citation4,Citation18,Citation43–Citation46 The antiresorptive action of BPs as a class results from both reduced osteoclastic activity (by inhibiting an enzyme farnesyl pyrophosphate synthase) and affinity for bone mineral, but the antiresorptive potency and binding affinity differ among the compounds.
We focused on the BPs because the prevalence of use of other antiosteoporotic drugs over this period was too low to detect an effect on HF incidence. After 2000, when BPs became widely available in Australia, the number of prescriptions steadily increased up to 2006. Between 2001 and 2005, the HF incidence declined in older females (≥60 years) by 54.1%, in males by 23.2%, and in total by 42.6%. These findings are in agreement with those reported from Canada:Citation11 a decline of HF rates with a steady increase in etidronate use between 1996 and 2003.
The new and intriguing observation of this study is that the substantial fall in BP use (following reports on ONJ associated with BPs) since 2006 coincides with increased standardized HF rates in females in 2007 (+22.6%) and in 2008 (+25.2%) compared with 2005, whereas, in males, HF incidence declined in the same period. Older females are known to comprise the majority of BP users, whereas male osteoporosis is much less frequently recognized and treated.Citation47,Citation48 Our observations are in line with data showing an inverse relation between adherence to BP and fracture rate. High adherence to BP therapy was associated with a 23% reduction in HF rates,Citation49 and poor compliance resulted in a 28% increased HF risk.Citation50 A recently published Australian study concluded that, in 2008, a 13.2% estimated reduction in the number of BP prescriptions may have resulted in 70 (+16.9%) HFs and 14 deaths.Citation51 Importantly, BPs not only effectively prevent fragility fractures but also improve quality of lifeCitation52 and reduce the risk of breast cancer in postmenopausal women,Citation53,Citation54 as well as reduce all-cause mortality.Citation55–Citation57
The fact that reduction in BP prescriptions was followed by an increase in HF rates in females, along with the previously observed decline in HF rates when BP use rapidly increased, does not necessarily establish a causal connection between the two. Other factors may also have contributed to the short-term changes in HF incidence rates. Indeed, trends toward decreasing HF rates were observed in some countries (United States, Canada, and Sweden) before widespread availability of current antiosteoporotic medications.Citation8,Citation58–Citation60 No consistent changes or even increasing HF trends were recently reported in other developed countries (Germany, Austria, Finland, Switzerland, and Japan),Citation61–Citation65 and some found declining HF incidence only in the new millennium,Citation11,Citation61,Citation66,Citation67 although none of these studies, except one,Citation11 provided information on BP use.
The continuing fall in the use of HRT since 2001 is unlikely to account for the increase in HF incidence in females in 2007–2008, as in the previous period (2001–2005), despite HRT prescriptions having decreased by half and HF rates having declined by 54.1%.
Different patterns in HF rates seen in males and females may argue against the role of BPs. In contrast to some recent studiesCitation61 reporting no downward trend in the HF rates in males, but in accordance with others,Citation59 we found a reduction in HF incidence in males in 2007–2008 despite the drop in BP prescriptions. This is difficult to interpret. As men are rarely treated for osteoporosis, the reduction in use of BPs may be too small to lead to a detectable decrease in HF rates. Other factors possibly associated with a decrease in HF rates in males may include overweight and obesity, declining smoking rates,Citation68 and a birth cohort effect.Citation69 These explanations are still hypothetical. The complex relationship between HF and gender requires further investigations.
This study has certain limitations in addition to its ecologic design. No information was available on individual demographic and clinical characteristics of BP users. Similarly, the proportion of patients receiving adequate antiosteoporotic therapy (including calcium and vitamin D supplementation) is unknown. There is also a possibility that the medication was prescribed but not taken. On the other hand, because of the remaining effect of BP on fracture risk after cessation of treatment,Citation70,Citation71 it is likely that a short-term study, like ours, underestimates the impact of the current fall in BP use on HF rates. Despite these limitations, our ecological analysis provides strong support for the antifracture effectiveness of BPs in real-world practice.
In conclusion, although currently there is no clear understanding of factors contributing to changing HF epidemiology, the available evidence suggests that much of the decline in HF rates is due to the use of BPs. A fall in the use of BPs is associated with increased HF rates in females, indicating that BPs should still be considered the first-line medications for the prevention and treatment of osteoporosis. Our results need to be confirmed in other populations and countries.
Acknowledgements
The authors gratefully acknowledge Novartis Pharmaceuticals for supporting the publishing of this manuscript after its acceptance by the journal. The sponsor did not influence this manuscript in any way and played no role in the design of the study; the collection, analysis, or interpretation of data; or the preparation of the manuscript.
Disclosure
Dr M Davis has received honoraria from Sanofi Aventis, Servier, and Merck Sharp & Dohme for presentations at scientific educational sessions. The three other authors have no conflicts of interest to declare.
References
- HarrisSTReginsterJYHarleyCRisk of fracture in women treated with monthly oral ibandronate or weekly bisphosphonates: the eValuation of IBandronate Efficacy (VIBE) database fracture studyBone200944575876519168160
- RingeJDDohertyJGAbsolute risk reduction in osteoporosis: assessing treatment efficacy by number needed to treatRheumatol Int201030786386920035331
- StevensonMJonesMLde NigrisEBrewerNDavisSOakleyJA systematic review and economic evaluation of alendronate, etidronate, risedronate, raloxifene and teriparatide for the prevention and treatment of postmenopausal osteoporosisHealth Technol Assess2005922116015929857
- WattsNBDiabDLLong-term use of bisphosphonates in osteoporosisJ Clin Endocrinol Metab20109541555156520173017
- BorgstromFStromOCoelhoJThe cost-effectiveness of risedronate in the UK for the management of osteoporosis using the FRAXOsteoporos Int201021349550519565175
- KanisJAAdamsJBorgstromFThe cost-effectiveness of alendronate in the management of osteoporosisBone200842141518156107
- TostesonANMeltonLJ3rdDawson-HughesBCost-effective osteoporosis treatment thresholds: the United States perspectiveOsteoporos Int200819443744718292976
- MeltonLJ3rdKanisJAJohnellOPotential impact of osteoporosis treatment on hip fracture trendsJ Bone Miner Res200520689589715883627
- FeldsteinACWeyckerDNicholsGAEffectiveness of bisphosphonate therapy in a community settingBone200944115315918926939
- CrillyRGHillierLMMasonMGutmanisICoxLPrevention of hip fractures in long-term care: relevance of community-derived dataJ Am Geriatr Soc201058473874520345863
- JaglalSBWellerIMamdaniMPopulation trends in BMD testing, treatment, and hip and wrist fracture rates: are the hip fracture projections wrong?J Bone Miner Res200520689890515883628
- SirisESHarrisSTRosenCJAdherence to bisphosphonate therapy and fracture rates in osteoporotic women: relationship to vertebral and nonvertebral fractures from 2 US claims databasesMayo Clin Proc20068181013102216901023
- FisherAAO’BrienEDDavisMWTrends in hip fracture epidemiology in Australia: possible impact of bisphosphonates and hormone replacement therapyBone200945224625319409518
- KhoslaSBurrDCauleyJBisphosphonate-associated osteonecrosis of the jaw: report of a task force of the American Society for Bone and Mineral ResearchJ Bone Miner Res200722101479149117663640
- PazianasMMillerPBlumentalsWABernalMKothawalaPA review of the literature on osteonecrosis of the jaw in patients with osteoporosis treated with oral bisphosphonates: prevalence, risk factors, and clinical characteristicsClin Ther20072981548155817919538
- AbrahamsenBBisphosphonate adverse effects, lessons from large databasesCurr Opin Rheumatol201022440440920473174
- LoJCO’RyanFSGordonNPPrevalence of osteonecrosis of the jaw in patients with oral bisphosphonate exposureJ Oral Maxillofac Surg201068224325319772941
- PazianasMCooperCEbetinoFHRussellRGLong-term treatment with bisphosphonates and their safety in postmenopausal osteoporosisTher Clin Risk Manag2010632534320668715
- KhanAASandorGKDoreEBisphosphonate associated osteonecrosis of the jawJ Rheumatol200936347849019286860
- MavrokokkiTChengASteinBGossANature and frequency of bisphosphonate-associated osteonecrosis of the jaws in AustraliaJ Oral Maxillofac Surg200765341542317307586
- WalterCAl-NawasBFrickhofenNPrevalence of bisphosphonate associated osteonecrosis of the jaws in multiple myeloma patientsHead Face Med201061120615236
- WooSBHellsteinJWKalmarJRNarrative [corrected] review: bisphosphonates and osteonecrosis of the jawsAnn Intern Med20061441075376116702591
- KhanAASandorGKDoreECanadian consensus practice guidelines for bisphosphonate associated osteonecrosis of the jawJ Rheumatol20083571391139718528958
- RizzoliRBurletNCahallDOsteonecrosis of the jaw and bisphosphonate treatment for osteoporosisBone200842584184718314405
- SambrookPNEbelingPOsteonecrosis of the jawCurr Rheumatol Rep20081029710118460263
- SilvermanSLLandesbergROsteonecrosis of the jaw and the role of bisphosphonates: a critical reviewAm J Med2009122Suppl 2S33S4519187811
- Australian Bureau of StatisticsAustralian Demographic Statistics: Population Projections Catalogue No 3101.0Canberra (ACT)Australian Bureau of Statistics2009
- Medicare AustraliaPBS Statistics2010 Available from: http://www.medicareaustralia.gov.au/provider/pbs/stats.jsp. Accessed 2010 Oct 29.
- DeeksEDDhillonSSpotlight on strontium ranelate: in postmenopausal osteoporosisDrugs Aging201027977177320809666
- MariePJFelsenbergDBrandiMLHow strontium ranelate, via opposite effects on bone resorption and formation, prevents osteoporosisOsteoporos Int201092 [Epub ahead of print]
- GennariLMerlottiDNutiRSelective estrogen receptor modulator (SERM) for the treatment of osteoporosis in postmenopausal women: focus on lasofoxifeneClin Interv Aging20105192920169039
- KungAWChuEYXuLBazedoxifene: a new selective estrogen receptor modulator for the treatment of postmenopausal osteoporosisExpert Opin Pharmacother20091081377138519445558
- CanalisEUpdate in new anabolic therapies for osteoporosisJ Clin Endocrinol Metab20109541496150420375217
- DealCFuture therapeutic targets in osteoporosisCurr Opin Rheumatol200921438038519461517
- FabbricianiGPirroMManfredelliMRTransient osteoporosis of the hip: successful treatment with teriparatideRheumatol Int2010318 [Epub ahead of print]
- LiXWarmingtonKSNiuQTInhibition of sclerostin by monoclonal antibody increases bone formation, bone mass and bone strength in aged male ratsJ Bone Miner Res2010716 [Epub ahead of print]
- JulesJAshleyJWFengXSelective targeting of RANK signaling pathways as new therapeutic strategies for osteoporosisExpert Opin Ther Targets201014992393420678025
- PalaniswamyCSelvarajDRRaoVPatelUNewer therapies for osteoporosisAm J Ther201017219720020305400
- RouxSNew treatment targets in osteoporosisJoint Bone Spine201077322222820381400
- InderjeethCAFooACLaiMMGlendenningPEfficacy and safety of pharmacological agents in managing osteoporosis in the old old: review of the evidenceBone200944574475119130909
- Salari SharifPAbdollahiMLarijaniBCurrent, new and future treatments of osteoporosisRheumatol Int2010730 [Epub ahead of print]
- LibermanUAHochbergMCGeusensPHip and non-spine fracture risk reductions differ among antiresorptive agents: evidence from randomised controlled trialsInt J Clin Pract200660111394140017026515
- AbelsonARingeJDGoldDTLangeJLThomasTLongitudinal change in clinical fracture incidence after initiation of bisphosphonatesOsteoporos Int20102161021102919722103
- Le GoffBGuillotPGlemarecJBerthelotJMMaugarsYA comparison between bisphosphonates and other treatments for osteoporosisCurr Pharm Des201016273037304420722614
- MacLeanCNewberrySMaglioneMSystematic review: comparative effectiveness of treatments to prevent fractures in men and women with low bone density or osteoporosisAnn Intern Med2008148319721318087050
- MasudTMcClungMGeusensPReducing hip fracture risk with risedronate in elderly women with established osteoporosisClin Interv Aging2009444544919966913
- FeldsteinACNicholsGOrwollEThe near absence of osteoporosis treatment in older men with fracturesOsteoporos Int200516895396215928798
- PapaioannouAKennedyCCIoannidisGThe osteoporosis care gap in men with fragility fractures: the Canadian Multicentre Osteoporosis studyOsteoporos Int200819458158717924051
- PatrickARBrookhartMALosinaEThe complex relation between bisphosphonate adherence and fracture reductionJ Clin Endocrinol Metab20109573251325920444916
- ImazIZegarraPGonzalez-EnriquezJRubioBAlcazarRAmateJMPoor bisphosphonate adherence for treatment of osteoporosis increases fracture risk: systematic review and meta-analysisOsteoporos Int201021111943195119967338
- SambrookPNChenJSSimpsonJMMarchLMImpact of adverse news media on prescriptions for osteoporosis: effect on fractures and mortalityMed J Aust2010193315415620678043
- KawateHOhnakaKAdachiMAlendronate improves QOL of postmenopausal women with osteoporosisClin Interv Aging2010512313120458350
- ChlebowskiRTChenZCauleyJAOral bisphosphonate use and breast cancer incidence in postmenopausal womenJ Clin Oncol201028223582359020567009
- RennertGPinchevMRennertHSUse of bisphosphonates and risk of postmenopausal breast cancerJ Clin Oncol201028223577358120567021
- BollandMJGreyABGambleGDReidIREffect of osteoporosis treatment on mortality: a meta-analysisJ Clin Endocrinol Metab20109531174118120080842
- CreeMWJubyAGCarriereKCMortality and morbidity associated with osteoporosis drug treatment following hip fractureOsteoporos Int200314972272712904833
- LylesKWColon-EmericCSMagazinerJSZoledronic acid in reducing clinical fracture and mortality after hip fractureN Engl J Med2007357 nihpa40967.
- GehlbachSHAvruninJSPuleoETrends in hospital care for hip fracturesOsteoporos Int200718558559117146592
- LeslieWDO’DonnellSJeanSTrends in hip fracture rates in CanadaJAMA2009302888388919706862
- LofmanOBerglundKLarssonLTossGChanges in hip fracture epidemiology: redistribution between ages, genders and fracture typesOsteoporos Int2002131182511878451
- ChevalleyTGuilleyEHerrmannFRHoffmeyerPRapinCHRizzoliRIncidence of hip fracture over a 10-year period 1991–2000 reversal of a secular trendBone20074051284128917292683
- HaginoHKatagiriHOkanoTYamamotoKTeshimaRIncreasing incidence of hip fracture in Tottori Prefecture, Japan: trend from 1986 to 2001Osteoporos Int200516121963196816133645
- IcksAHaastertBWildnerMBeckerCMeyerGTrend of hip fracture incidence in Germany 1995–2004 a population-based studyOsteoporos Int20081981139114518087659
- LonnroosEKautiainenHKarppiPIncreased incidence of hip fractures. A population based-study in FinlandBone200639362362716603427
- MannEIcksAHaastertBMeyerGHip fracture incidence in the elderly in Austria: an epidemiological study covering the years 1994 to 2006BMC Geriatr200883519105814
- DimaiHPSvedbomAFahrleitner-PammerAEpidemiology of hip fractures in Austria: evidence for a change in the secular trendOsteoporos Int2010511 [Epub ahead of print]
- HernandezJLOlmosJMAlonsoMATrend in hip fracture epidemiology over a 14-year period in a Spanish populationOsteoporos Int200617346447016283063
- KanisJAJohnellOOdenASmoking and fracture risk: a meta-analysisOsteoporos Int200516215516215175845
- KannusPNiemiSParkkariJPalvanenMVuoriIJärvinenMNationwide decline in incidence of hip fractureJ Bone Miner Res200621121836183817002578
- EnsrudKEBarrett-ConnorELSchwartzARandomized trial of effect of alendronate continuation versus discontinuation in women with low BMD: results from the Fracture Intervention Trial long-term extensionJ Bone Miner Res20041981259126915231012
- BlackDMSchwartzAVEnsrudKEEffects of continuing or stopping alendronate after 5 years of treatment: the Fracture Intervention Trial Long-term Extension (FLEX): a randomized trialJAMA2006296242927293817190893
