Abstract
Purpose
The purpose of this review was to assess the effectiveness of pelvic floor muscle training (PFMT) in the treatment of urinary incontinence (UI) in women, with a particular focus on the impact of this form of therapy on the patients’ quality of life (QoL).
Methods
The following electronic databases were searched: PubMed, Embase, and Cochrane Library (articles only in English, 1990–2017). Search terms were as follows: urinary incontinence, pelvic floor muscle training, pelvic floor exercises, quality of life. Systematic review methods were based on the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement.
Results
The assessment of the impact of PFMT on the QoL of women with UI was conducted among 2,394 women in 24 selected studies. After the end of treatment, the majority of patients in the experimental groups noted a statistically significant improvement in QoL.
Conclusion
The results of this literature review demonstrate that PFMT is an effective treatment for UI in women. PFMT significantly improves the QoL of women with UI, which is an important determinant of their physical, mental, and social functioning.
Introduction
The frequency of urinary incontinence (UI) is difficult to determine, and there is no unequivocal data indicating the percentage of people suffering from this disorder. According to the data adopted during the 6th International Consultation on Incontinence (ICI), the problem of UI in the whole population ranges from 4% to 8%.Citation1 It is worth noting that the number of people affected by this condition in the entire world population has been steadily growing over the last decade. In 2008, 346 million people suffered from UI, while in 2013, 383 million. At the same time, it was estimated that in 2018, the number of people with UI around the world would be ~420 million – 300 million women and 120 million men.Citation2
Based on etiology and pathophysiology, UI is classified into 3 types: Stress UI (SUI), Urge UI (UUI), and Mixed UI (MUI). SUI is defined as the involuntary leakage of urine during exertion, such as coughing, sneezing, or laughing. An increase in abdominal pressure due to physical exertion puts stress on the bladder, causing urine to leak. The basic mechanisms responsible for that reaction are poor urethral support by the pelvic floor muscles and intrinsic sphincter deficiency. Many factors predisposing to SUI are identified in the related literature, and among others, these are as follows, numerous births, previous operations, generalized weakening of connective tissue, hormone deficiency, genital mutilation, or reduction of reproductive organs.Citation1 UUI (commonly referred to as “overactive bladder”) is the involuntary leakage of urine preceded by a strong and sudden urge to urinate. This incontinence is usually caused by involuntary contractions of the detrusor muscles of the bladder wall at inappropriate times. UUI may be triggered by simple everyday occurrences, such as the sound of running water, exposure to cold temperatures, or drinking cold beverages. Idiopathic etiologic factors include myogenic, neurogenic, and urethrogenic symptoms.Citation2 MUI is a mixture of SUI and UUI. Etiologic factors for MUI are also a combination of the factors described earlier.Citation3
In addition to the described somatic symptoms, problems related to urinary iodine excretion have a psychological impact and substantially reduce patients’ quality of life (QoL). They often experience discomfort, low self-esteem, mood deterioration, and the feeling of helplessness. There is a decline in quality of their personal, social, and professional life. Due to the fear of others finding out about their unfortunate condition, patients are forced to change their lifestyle, which, in turn, has a negative impact on socializing, and contributes to alienation, social isolation, changes in sexual activity, and even depression or anxiety disorder.Citation4–Citation8 Therefore, while assessing the effectiveness of various treatments for UI, it is essential to take into consideration the lifestyle factor, which is defined as physical, mental, and social well-being.
Physiotherapy seems to be an important part of conservative treatment of UI. Pelvic floor muscle training (PFMT) stands out among physiotherapy methods used in the treatment of UI. The scientific basis for pelvic floor muscle rehabilitation was founded by an American gynecologist Arnold Kegel, who, in the 1950s, published results of a 15-year-old study, which covered the use of pelvic floor exercises in patients with UI. Kegel pointed out that systematic muscle activity causes muscles to lose 4 times less of their mass than compared with staying inactive, and hence it is the optimal method for improving the anatomical and functional impairment of muscles. Systematic activity of contractile fragments of impaired muscles improves their coordination. This contributes to a better urethral compression, when the intra-abdominal pressure increases, during exercise. Performing pelvic floor exercises correctly, especially in sensorimotor training sessions, leads to regaining proprioception in the levator ani.Citation9
The purpose of the systematic review
The purpose of this review was to assess the effectiveness of PFMT in the treatment of UI in perimenopausal women, with a particular focus on the impact of this form of therapy on the patients’ QoL. The following databases were searched: PubMed, Embase, and Cochrane Library (articles only in English, 1990–2017). The search terms used were as follows: urinary incontinence “AND” pelvic floor muscle training “OR” pelvic floor exercises “AND”/“OR” quality of life. Systematic review methods were based on the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement.Citation10
Study selections
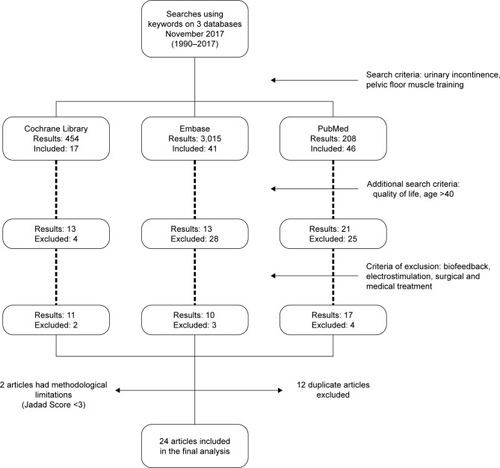
The first and primary criterion of the review was the use of pelvic floor exercises in the treatment of UI. Then, the studies were selected based on the impact of PFMT on the QoL of women with UI. The exclusion of studies with biofeedback, electrostimulation, surgical and medical treatments was the final criterion. Quality of the selected studies was assessed using the Jadad scale. shows a detailed flowchart of search and exclusion strategy.
Data collection
The following data were collected from the selected studies: author name, year of publication, participants (number and age), types of UI, treatment duration, treatment type, objectivization methods of treatment outcomes, main conclusions, and the statistical analysis used. Three authors performed independent data extraction in electronic databases (AS, PubMed; MWR, Embase; and HS, Cochrane Library). One researcher collected data and conducted the data selection process (AS). Moreover, the methodological quality of the selected studies was assessed using the Jadad scale. The Jadad score is often used to assess the methodological quality of controlled trials. Studies are scored according to the presence of 3 key methodological features of clinical trials: randomization, masking, and accountability of all patients, including withdrawals. One point is added for an affirmative answer (“yes”) to each of the first 5 items, while 1 point is subtracted for an affirmative answer (“yes”) from either of the last 2 items, for an overall score from 0 to 5.Citation11 The systematic analysis includes only clinical studies with a score of 3 or higher in the Jadad scale. Two authors (AS and MWR) individually assessed the methodological quality of the collected research using the Jadad scale.
Results and discussion
Study characteristics
Electronic medical databases were searched in November 2017. The search retrieved 3,680 results: a total of 464 in the Cochrane Library, 3,016 in Embase, and 208 in PubMed. The studies were selected using a very detailed flowchart (). Twenty-four articles were included in the final review (). There were between 30 and 446 women (a total of 2,394 patients), aged 40–85 years old in each study group. The Jadad scale showed that 19 research findings were randomized and additionally 5 of them were blinded.
Table 1 Summary of studies’ assessment of pelvic floor muscle training on incontinence-specific quality of life of women with urinary incontinence
Outcome measures
The following diagnostic tests were used in the research studies: the number of UI episodes and the pad test and urinary diary. Pelvic floor muscle strength and function were checked during palpitation, Valsalva maneuver, perinometry, and ultrasound and electromyographic investigation. Rankin Scale, Mini Mental State Examination, Visual Analog Scale, and Time Up and Go test were also used. Patients’ QoL before and after the treatment, assessed during each exam, were the study inclusion criteria. The following questionnaires were used in the QoL assessment: King’s Health Questionnaire (KHQ), Incontinence Impact Questionnaire (IIQ), Urogenital Distress Inventory (UDI), QoL Scale (QoLS), Incontinence QoL (IQoL) questionnaire, Bristol Female Lower Urinary Tract Symptoms (BFLUTS) questionnaire, Health-Related Quality of Life, ICI Modular Questionnaire (ICIQ, ICIQ-UISF; short form; ICIQ-LUTSqol; Lower Urinary Tract Symptoms QoL), Ditrovie Scale, Pelvic Floor Distress Inventory (PFDI), Pelvic Floor Impact Questionnaire (PFIQ), and Symptom Impact Index (SII). Psychometric qualities, accuracy, and credibility of all the questionnaires were confirmed clinically.
The most commonly used questionnaire was the KHQ; it was mentioned in 8 out of 24 studies.Citation12,Citation13,Citation17,Citation18,Citation24,Citation28–Citation31 KHQ is a patient self-administered self-report and has 3 parts consisting of 21 items. Part 1 contains general health perception and incontinence impact (1 item each). Part 2 contains role limitations, physical limitations, social limitations (2 items each), personal relationships, emotions (3 items each) and sleep/energy (2 items), as well as severity measures (4 items). Part 3 is considered as a single item and contains 10 responses in relation to frequency, nocturia, urgency, urge, stress, intercourse incontinence, nocturnal enuresis, infections, pain, and difficulty in voiding.Citation36 KHQ is a tool recommended by the European Clinical Practice Guidelines.Citation37
In 5 out of 24 studies, the QoL was evaluated by the use of IIQ.Citation15,Citation19,Citation20,Citation21,Citation27 This questionnaire was used in 2 versions: the full version – IIQ and the abbreviated one IIQ-7. In 3 out of 24 studies, the full version of the questionnaire was used,Citation15,Citation19,Citation20 while in 2 out of 24 tests, a short form – IIQ-7 was used.Citation21,Citation27 The IIQ was designed by Shumaker et alCitation38 to assess the impact of UI on activities and emotions in women. Thirty self-administered questions cover 4 domains: physical activity, social relationships, traveling, and emotional health.
In 4 out of 24 studies, the ICIQ was applied.Citation22,Citation26,Citation32,Citation34 The ICIQ-SF consists of 3 items (Frequency, Amount, and Impact), and a group of 8 questions related to the type of UI, which are not part of the questionnaire score. The purpose of the 8 questions is to describe a given type of urinary incontinency. The total score is the sum of the first 3 items and it ranges from 0 to 21 points. A score of 21 – the worst possible QoL, and 0 – the best possible QoL.Citation39 ICIQ LUTS QoL is based on KHQ. ICIQ LUTS measures the impact of UI on physical and mental activities, changes in interpersonal relations, and in everyday life. The global score can range between 19 and 79 points – the higher the score, the worse the QoL. The conversion of points of ICIQ LUTS QoL is carried out on the basis of the instructions by Hebbar based on KHQ.Citation36,Citation40
In 2 out of 24 tests, the IQoL questionnaire was implemented.Citation22,Citation26,Citation28 The IQoL questionnaire is composed of 20 questions evaluating limitations on behavior, the psychosocial impact, and the social embarrassment that UI causes.Citation41
The scales, which have only been used in 1 study are as follows, The Norwegian version of the QoL Scale (QoLS-N),Citation14 The BFLUTS questionnaire,Citation14 PFDI,Citation28 PFIQ,Citation28 SII,Citation25 and Ditrovie scale.Citation23 The QoLS-N is adapted and modified for use in the chronic illness population, by Burckhardt et al;Citation42 this scale applies to general health and QoL. The Norwegian version uses a 7-point satisfaction scale.Citation43 The BFLUTS questionnaire was designed to assess a wide range of symptoms, including incontinence, and the impact on sexual function and QoL.Citation44 The PFDI comprises a urinary scale (UDI; score range 0–300), including 3 subscales (Stress, Irritative and Obstructive; score range 0–100), prolapse (POPDI; score range 0–300), and colorectal (CRADI; score range 0–400) scales. Higher PFDI scale and subscale scores reflect increasing symptoms. The PFIQ includes 3 scales, urinary (UIQ), prolapse (POPIQ) and colorectal (CRAIQ) ones, each with score range of 0–300. Higher PFIQ scores – greater daily impact on pelvic symptoms.Citation45 The Ditrovie scale consists of 10 items: activity (4 items), emotional impact (2 items), self-image (2 items), sleep (1 item), and general welfare (1 item). The higher the score, the worse the QoL.Citation46 The SII measures women’s views on stress incontinence severity, as well as the impact or discomfort caused by the symptoms.Citation47
Therapy comparison and treatment duration
The studies compared supervised and unsupervised PFMT, group and individual training, PFMT and bladder training (also with the use of vaginal cones), as well as training groups and a control group (no therapy). Treatment duration was between 6 and 42 weeks; a majority of the therapy sessions were held 1–3 times per week, and lasted 45 minutes each.
Pelvic floor muscles training and types of UI
The evaluation of the impact of PFMT on the QoL of women with incontinence was carried out in all of the presented studies. In 16 studies, the study population concerned women with SUI. Moreover, in studies, the authors compared the effects of pelvic floor muscle exercises on incontinence depending on the type of urinary incontinence.Citation16,Citation21,Citation27 In addition, each study showed that the statistically highest improvement in QoL occurred in SUI, then a lower result was achieved in UUI, and no significant differences were found in the impact of PFMT on MUI. In the case of 2 studies, the type of UI in the study population was not reported.Citation20,Citation30
Compared treatment methods
A PFM training group and a control group (no training) were compared in 5 out of the 24 studies which qualified for the analysis (223 patients).Citation14,Citation17,Citation26,Citation30,Citation33 In all referenced studies, statistically significant improvement in the QoL in the PFMT group was observed compared with the control group.
In 5 out of the 24 studies (a total of 253 women) qualified for the analysis, a PFM training group was divided into a supervised PFMT group and a control (home-exercise) group. Fan et alCitation21 study results showed a significant improvement of the UDI total result (p<0.01) and the IIQ (p<0.01) in the experimental group compared with the control group after a 6-week training program. Whereas Ferreira et alCitation23 showed that 6 months following the treatment, the QoL improved in both groups. However, the outcome was better in women in the supervised PFMT group than in women who exercised at home (p=0.04). Similar study results were obtained by Sherburn et alCitation34 and Jahromi et al.Citation26 Felicissimo et alCitation22 showed there were no differences between the supervised group and the home-exercise group, with regard to the QoL (p=0.76). The study authors concluded that both supervised PFMT and unsupervised PFMT are effective in UI treatment, if a proper training session is provided.
The effectiveness of group and individual training was compared in 2 out of the 24 selected studies (104 patients).Citation18,Citation19 No significant differences were found between both studies in terms of group and individual training effectiveness.
In 1 out of the 24 selected studies (44 women), PFMT in supine position (KG) was compared with PFMT in supine and standing position (CG). The study results have shown the effectiveness of PFMT, but various training positions had no impact on its effectiveness.Citation15
In 8 out of the 24 selected studies, the effectiveness of PFMT was compared with other methods. In studies conducted by Pereira et al,Citation31 a group of 45 women was divided into 3 distinct groups – a vaginal cone group (VG), a PFMT group, and a control group (no therapy). After 6 weeks of therapy, a significant improvement (p<0.01) in terms of QoL was observed in both the VG group and the PFMT group, compared with the control group. The following 2 studies (186 women) compared abdominal muscle training (TrA) to PFMT monotherapy. Konstantinidou et alCitation29 found that improvement in QoL was observed in both groups, and no significant differences were found between them. Whereas, Ptak et alCitation32 observed better results in the combined therapy group (TrA+PFMT).
In 3 out of the 24 selected studies, bladder training (BT) was compared with PFMT. A total of 238 women participated in the study. Sherburn et alCitation34 showed an improvement in QoL in both groups (p=0.01), without any significant differences between the groups. The next study compared a combined PFMT/BT with a BT monotherapy.Citation27 After treatment, all of the studied women had an improvement in QoL (IIQ-7 p=0.01; UDI-6 p<0.01). The following study (790 patients) compared the effectiveness of combined PFMT/BT (the study group) to no treatment (the control group). After therapy, there was a statistically significant improvement in QoL in the study group, compared with the control group (p=0.05).Citation12
In 2 out of the 24 selected studies (790 women), QoL was evaluated after PFMT, pessary therapy, and combined therapy (PFMT+pessary therapy).Citation16,Citation28 After a 3-month treatment, a statistically significant improvement in QoL (p<0.01) for all women was observed in both studies, and no significant differences were observed between the groups.
In 3 out of the 24 selected studies (505 women), patients received PFMT monotherapy and there was no control group.Citation13,Citation21,Citation24 Each study showed a statistically significant improvement in QoL after PFMT.
Limitations
The limitation of this analysis is primarily the methodical variability in the analyzed studies. The search criteria should be narrowed further, taking into account the methodological homogeneity of the conducted therapy.
Conclusion
The results of this literature review demonstrate that PFMT is an effective treatment for UI in women. PFMT appears to be an effective non-surgical intervention, particularly for women with SUI. It could also be recommended as the first-line conservative treatment for elderly women. PFMT significantly improves the QoL of women with UI, which is an important determinant of their physical, mental, and social functioning. The duration of PFMT should not be shorter than 6 weeks. It is advised to provide supervised PFMT. PFMT can be used either as a monotherapy or as a combined therapy for the treatment of UI in women. The KHQ is useful for following up on the QoL of women with UI in many different clinical settings and in controlled clinical trials.
Author contributions
All authors contributed toward data analysis, drafting and critically revising the paper, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- The Global Forum on IncontinenceAbout incontinence Available from: http://www.gfiforum.com/incontinenceAccessed January 15, 2018
- AbramsPCardozoLWaggAWeinAIncontinence6th edition20176th International Consultation on IncontinenceTokyo9s. 228788
- EdwallLCarlstromKJonassonAFDifferent estrogen sensitivity of urogenital tissue from women with and without stress urinary incontinenceNeurourol Urodyn20092851652019260092
- MelvilleJLFanMYRauHNygaardIEKatonWJMajor depression and urinary incontinence in women: temporal associations in an epidemiologic sampleAm J Obstet Gynecol2009201549049719716547
- van der VaartCHRooversJPde LeeuwJRHeintzAPAssociation between urogenital symptoms and depression in community-dwelling women aged 20 to 70 yearsUrology200769469169617445653
- FeldeGBjellandIHunskaarSAnxiety and depression associated with incontinence in middle-aged women: a large Norwegian crosssectional studyInt Urogynecol J201223329930622068320
- TettamantiGAltmanDIliadouANBelloccoRPedersenNLDepression, neuroticism, and urinary incontinence in premenopausal women: a nationwide twin studyTwin Res Hum Genet201316597798423985362
- FarageMAMillerKWBerardescaEMaibachHIPsychosocial and societal burden of incontinence in the aged population: a reviewArch Gynecol Obstet2008277428529018026973
- KegelAPowellTThe physiologic treatment of urinary stress incontinenceJ Urol19506380881415422687
- LiberatiAAltmanDGTetzlaffJThe PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaborationBMJ2009339b270019622552
- JadadARMooreRADawnCAssessing the quality of reports of randomized clinical trials: is blinding necessary?Control Clin Trials1996171128721797
- AslanEKomurcuNBejiNKYalcinOBladder training and Kegel exercises for women with urinary complaints living in a rest homeGerontology200854422423118483451
- BalmforthJRMantleJBidmeadJCardozoLA prospective observational trial of pelvic floor muscle training for female stress urinary incontinenceBJU Int200698481181716978276
- BøKTalsethTVinsnesARandomized controlled trial on the effect of pelvic floor muscle training on quality of life and sexual problems in genuine stress incontinent womenActa Obstet Gynecol Scand200079759860310929962
- Borello-FranceDFZyczynskiHMDowneyPARauseCRWisterJAEffect of pelvic-floor muscle exercise position on continence and quality-of-life outcomes in women with stress urinary incontinencePhys Ther200686797498616813477
- BradleyCSRahnDDNygaardIEThe questionnaire for urinary incontinence diagnosis (QUID): validity and responsiveness to change in women undergoing non-surgical therapies for treatment of stress predominant urinary incontinenceNeurourol Urodyn201029572773419787711
- CarneiroEFAraujo NdosSBeuttenmüllLThe anatomical-functional characteristics of the pelvic floor and quality of life of women with stress urinary incontinence subjected to perineal exercisesActas Urol Esp201034978879320843456
- de Oliveira CamargoFRodriguesAMPelvic floor muscle training in female stress urinary incontinence: comparison between group training and individual treatment using PERFECT assessment schemeInt Urogynecol J Pelvic Floor Dysfunct200920121455146219690792
- DemainSSmithJDHillerLDziedzicKComparison of group and individual physiotherapy for female urinary incontinence in primary care: pilot studyPhysiotherapy2001875235242
- DuganSALavenderMDHebert-BeirneJBrubakerLA pelvic floor fitness program for older women with urinary symptoms: a feasibility studyPMR201358672676
- FanHLChanSSLawTSCheungRYChungTKPelvic floor muscle training improves quality of life of women with urinary incontinence: a prospective studyAust N Z J Obstet Gynaecol201353329830423551071
- FelicíssimoMFCarneiroMMSalemeCSPintoRZda FonsecaAMda Silva-FilhoALIntensive supervised versus unsupervised pelvic floor muscle training for the treatment of stress urinary incontinence: a randomized comparative trialInt Urogynecol J201021783584020179901
- FerreiraMSantosPCImpact of exercise programs in woman’s quality of life with stress urinary incontinenceRev Port Saude Publica201231310
- FitzFFCostaTFYamamotoDMImpact of pelvic floor muscle training on the quality of life in women with urinary incontinenceRev Assoc Med Bras (1992)2012582155159 Portuguese22569609
- HungHCHsiaoSMChihSYLinHHTsauoJYAn alternative intervention for urinary incontinence: retraining diaphragmatic, deep abdominal and pelvic floor muscle coordinated functionMan Ther201015327327920185357
- JahromiMKTalebizadehMMirzaeiMThe effect of pelvic muscle exercises on urinary incontinency and self-esteem of elderly females with stress urinary incontinencyGlob J Health Sci2015277179
- KayaSAkbayrakTGursenCShort-term effect of adding pelvic floor muscle training to bladder training for female urinary incontinence: a randomized controlled trialInt Urogynecol J201526228529325266357
- KentonKBarberMWangLPelvic floor symptoms improve similarly after pessary and behavioral treatment for stress incontinenceFemale Pelvic Med Reconstr Surg201218211812122453323
- KonstantinidouEKalaitziMMytilekasKVIoannidesEIHatzichristouDApostolidisADoes the type of physiotherapy affect the quality of life and clinical outcomes in female urinary incontinence? A comparative study of two physiotherapy schemesEur Urol Suppl2013121e733
- Nascimento-CorreiaGSantos-PereiraVTaharaNDriussoPEffects of pelvic floor muscle training on quality of life of a group of women with urinary incontinence: randomized controlled trialActas Urológicas Españolas (English Edition)2012364216221 Spanish
- PereiraVSde MeloMVCorreiaGNDriussoPVaginal cone for postmenopausal women with stress urinary incontinence: randomized, controlled trialClimacteric2012151455122066898
- PtakMBrodowskaACiećwieżSRotterIQuality of life in women with stage 1 stress urinary incontinence after application of conservative treatment-A randomized trialInt J Environ Res Public Health2017146577
- SarDKhorshidLThe effects of pelvic floor muscle training on stress and mixed urinary incontinence and quality of lifeJ Wound Ostomy Continence Nurs200936442943519609165
- SherburnMBirdMCareyMBøKGaleaMPIncontinence improves in older women after intensive pelvic floor muscle training: an assessor-blinded randomized controlled trialNeurourol Urodyn201130331732421284022
- ZanettiMRCastro RdeARottaALSantosPDSartoriMGirãoMJImpact of supervised physiotherapeutic pelvic floor exercises for treating female stress urinary incontinenceSao Paulo Med J2007125526526918094892
- HebbarSPandeyHChawlaAUnderstanding Kings Health Questionnaire (KHQ) in assessment of female urinary incontinenceInt J Res Med Sci20153531538
- ViktrupLSummersKHDennettSLClinical practice guidelines for the initial management of urinary incontinence in women: a European-focused reviewBJU Int20049411422
- ShumakerSAWymanJFUebersaxJSMcClishDFantlJAfor the Continence Program in Women (CPW) Research GroupHealth-related quality of life measures for women with urinary incontinence: the incontinence impact questionnaire and the urogenital distress inventoryQual Life Res199432913067841963
- TamaniniJTDambrosMD’AnconaCAPalmaPCRodrigues-NettoNJrResponsiveness to the Portuguese version of the International Consultation on Incontinence Questionnaire–Short Form (ICIQ-SF) after urinary stress incontinence surgeryInt Braz J Urol20053148248916255798
- KelleherCJCardozoLDKhullarVSalvatoreSA new questionnaire to assess the quality of life of urinary incontinent womenBr J Obstet Gyneacol199714013741379
- PatrickDLMartinMLBushnellDMYalcinIWagnerTHBueschingDPQuality of life of women with urinary incontinence: further development of the incontinence quality of life instrument (I-QOL)Urology199953171769886591
- BurckhardtCWoodsSSchultzAZiebarthDQuality of life in adults with chronic illness: a psychometric studyRes Nurs Health1989123473542602575
- WahlABurckhardtCWiklundIHanestadVThe Norwegian version of the quality of life scale (QoLS-N)Scand J Caring Sci19981221522210067647
- JacksonSDonovanJBrookesSEckfordSSwithinbankLAbramsPThe Bristol female lower urinary tract symptoms questionnaire: development and psychometric testingBr J Urol1996778058128705212
- BarberMDSpinoCJanzNKThe minimum important differences for the urinary scales of the Pelvic Floor Distress Inventory and Pelvic Floor Impact QuestionnaireAm J Obstet Gynecol200920058019375574
- AmarencoGMarquisPLericheBRichardFZerbibMJacquetinBA specific scale for assessing the disruption of quality of life during voiding disorders: scale DitrovieAnn Réadapt Méd Phys1997402126
- BlackNGriffithsJPopeCDevelopment of a symptom severity index and a symptom impact index for stress incontinence in womenNeurourol Urodyn19961566306408916115