Abstract
Objective
The aim of this study was to investigate the satisfaction of age-related hearing loss (ARHL) or presbycusis patients with individual, accurate, and precise fitting progress, which is a priority for bilateral hearing aids, and to explore the related influencing factors and their role in predicting the efficiency of hearing aids.
Methods
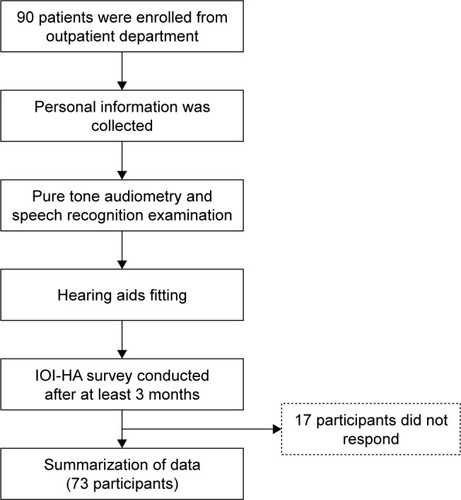
A total of 73 cases of presbycusis patients aged 60–95 years old underwent pure tone audiometry and speech recognition ability examination to obtain the pure tone audiometry of the better ear (BPTA) and maximum speech recognition rate of the better ear (BSRR) in quiet environment before hearing aid fitting. Audiologists evaluated the efficiency and satisfaction of participants according to the International Outcome Inventory for Hearing Aids (IOI-HA) questionnaire scores by face-to-face or telephone investigations after using the hearing aids for at least 3 months. The data were analyzed related to possible influencing factors.
Results
Total satisfaction percentage according to IOI-HA scores was 86.3%. There was no significant correlation between age, first fitting age, unilateral or bilateral hearing aids, BPTA, and IOI-HA total score. BSRR was strongly correlated to total IOI-HA scores (r=0.768). According to the multiple linear regression analysis, BPTA and BSRR both had a statistically significant effect on the total IOI-HA scores after hearing aid intervention.
Conclusion
ARHL patients with accurate hearing aid fitting will have high satisfaction and bilateral hearing aids are better than unilateral ones. Age and first fitting age are not meaningful to satisfaction with hearing aids. A higher maximum speech recognition rate before hearing aids fitting could predict better efficiency and satisfaction with hearing aids. Therefore, completing speech recognition ability examination before fitting would make a great contribution to the efficiency of hearing aids, and help ARHL patients have realistic expectations.
Introduction
Age-related hearing loss (ARHL), or presbycusis, is a general term that refers to hearing loss in the elderly and represents the contributions of a lifetime of insults to the auditory system. Both the peripheral and central auditory pathways are affected in presbycusis, and the clinical findings of the presbycusis often represent a mixture of abnormalities.Citation1 It has a serious impact on the quality of life, and even leads to mental and physical diseases in the elderly.Citation2,Citation3 In addition, ARHL has been reported to be a risk factor and a frailty marker for dementia and Alzheimer disease.Citation4 Many cross-sectional studies found some association between ARHL and cognitive impairment.Citation5–Citation7 One of the potentially modifiable risk factors for cognitive decline is ARHL.Citation1 Therefore, the early intervention for the ARHL is crucial to prevent the disease.
A hearing aid is an effective treatment for ARHL.Citation8 Before fitting hearing aids, pure tone threshold and acoustic immittance are routine examinations. However, we have observed that some patients cannot achieve satisfying effect like other patients though they have similar hearing loss. Current studies have found several influencing factors relate to the efficiency of hearing aids. For example, Meister et al found that cognitive function might be relevant for hearing aid benefit.Citation9 Hickson et al reported that factors that were most strongly associated with positive changes in the International Outcome Inventory for Hearing Aids (IOI-HA) scores were greater satisfaction with the hearing aid attributes of aid fit/comfort, clarity of tone and sound, and comfort with loud sounds, and greater satisfaction in the listening situations of conversation with one person, in small groups, in large groups, and outdoors.Citation10 It is acknowledged that many factors are associated with the efficiency of hearing aids. However, it is unclear as to which is the most significant factor that affects the hearing aid performance of ARHL patients. Here, as we all know, presbycusis involves both the peripheral and central auditory pathways. Speech recognition rate can reflect the ability of hearing center to process sound information. So, we carry out the speech recognition rate examination before fitting hearing aids in order to study its effect on hearing aids satisfaction.
Here we adopted the IOI-HA to evaluate the hearing aids effect. The IOI-HA questionnaire was first presented in English version by Cox et alCitation11 and has been translated into up to 20 languages which was presented by Cox in 2002.Citation12 The IOI-HA consists of seven items, including hours of use (item 1), benefit (item 2), residual activity limitations (item 3), satisfaction (item 4), residual participation restriction (item 5), effect on others (item 6), and quality of life (item 7). Each of the items has five options ranging from 1 to 5 which represent the worst to the best outcome. The sum of the seven items forms the global score of IOI-HA. Higher score of the IOI-HA means better outcome of the hearing aids. Liu et al have proved that the implementation of IOI-HA is time-efficient, imposing little burden on the clinician and patient, and could be used as an effective tool to measure the general effectiveness of hearing aids outcomes in China.Citation13 Previous studies have shown that the seven items can be divided into two factors. Cox and Alexander in 2002,Citation12 Brännström and Wennerström in 2010,Citation14 and Jespersen et al in 2014Citation15 all considered that factor 1 including items 1, 2, 4, and 7 mainly concentrates on introspection (me and my hearing aids) and factor 2 including items 3, 5, and 6 mainly concentrates on interaction (me and the rest of the world).
This study intended to conduct an IOI-HA questionnaire survey on ARHL patients with hearing aids and analyzed the correlation among age, gender, first fitting age, unilateral/bilateral hearing aids, pure tone audiometry of the better ear (BPTA), maximum speech recognition rate of the better ear (BSRR), score of factor 1, score of factor 2, and total score of the IOI-HA questionnaire, and to provide reference for clinical hearing aids fitting progress.
Method
At the beginning, a total of 90 patients from the Ninth People’s Hospital affiliated to Shanghai Jiaotong University School of Medicine, Otolaryngology Department, took part in this study and their personal information was collected. All of them were diagnosed with presbycusis excluding other diseases. All the 90 patients can normally communicate in Mandarin in daily life and do not have a medical history of sudden deafness, otitis media, otitis externa, etc. This study was conducted in accordance with the Declaration of Helsinki. All participants gave written informed consent for their participation. The study was approved by Medical Ethics Committee of Shanghai Ninth People’s Hospital, Shanghai JiaoTong University School of Medicine.
Aiming to acquire the mean BPTA (the average hearing threshold of the better ear at 500 Hz, 1 KHz, 2 KHz, and 4 KHz) and BSRR (maximum BSRR), Titan was used to test the tympanogram and Madsen Astera audiometer was used to measure pure tone audiometry and speech recognition rate. The tests were carried out in the standard sound insulation room with noise level lower than 25 dB (A). All the test equipment was calibrated by the Shanghai Institute of Acoustics, Chinese Academy of Sciences. The pure tone hearing threshold test was carried out according to the national standard GB/T 16403–1996. The maximum speech recognition rate was measured by using the single syllable glossary of Mandarin Speech Test Materials, which was compiled by Zhang et al.Citation16
After pure tone audiometry and speech recognition examination, our Hearing and Speech Center gave preference to bilateral, individual, and accurate hearing aids intervention and modulation of ARHL patients. All the participants had never used the hearing aids before and it was the first time for them to use the hearing aid. Sufficient communication and education was arranged for patients before selecting the hearing aid. We informed them of their hearing status, subsequent intervention, and hearing rehabilitation process in order to let them have a correct cognition of their hearing situation in detail. According to personal characteristic and degree of hearing loss, we chose the appropriate hearing aid and debuged it accurately and individually. All the hearing aids used were digital behind-the-ear hearing aids with more than four channels and priced at around ten thousand yuan. Then, the parameters were adjusted based on their own speech quality, bilateral loudness balance, others’ speech quality, and comfortable loudness. After fitting the hearing aids, we provided them with a detailed guidance of hearing aid’s maintenance and hearing rehabilitation orally and literally. At the same time, listing the possible problems and solutions to help patients adapt to the hearing aid, and telling them to come back for follow-up visit and monitoring after 1, 3, and 6 months were both necessary.
Different durations of using hearing aids can affect the total IOI-HA score. Previous research indicated that 3–12 months after fitting hearing aids, score of IOI-HA is expected to be stable. We carried out our survey at least 3 months after fitting the hearing aids. After using the hearing aids for 3 months, trained professionals adopted the IOI-HA questionnaire to investigate the efficiency and satisfaction of hearing aids on ARHL patients through a face-to-face question and answer or telephone interview follow-up. The whole process applied the same unified standard of questioning and recording. The IOI-HA questionnaire included seven core issues that examine hours of use (item 1), benefit (item 2), residual activity limitations (item 3), satisfaction (item 4), residual participation restriction (item 5), impact on others (item 6), and quality of life (item 7). For each item, five responses are possible, ranging from worst (score 1) to best outcome (score 5). The total sum of all item scores forms the global score. Higher scores indicate better hearing aid fitting outcome. Of the 90 participants, 17 did not respond to our survey, so finally there were 73 participants. Of the data sets included, there were 37 male patients and 36 female patients, aged between 60 and 93 years.
The SPSS 24.0 statistical software was used to analyze the data. The difference in the gender and unilateral/bilateral fitting of each IOI-HA questionnaire was compared with the chi-squared test, and variance analysis was used to measure the statistical difference among different levels of IOI-HA score about first fitting age, BPTA, BSRR, and laterality of hearing loss. Pearson’s correlation analysis was used to analyze the correlation among age, first fitting age, PTA of the better ear, BSRR, total score of the IOI-HA questionnaire, score of factor 1 (Q1, 2, 4, 7), and score of the factor 2 (Q3, 5, 6). Multiple linear regression analysis was used to analyze the influence of factors on the total score of IOI-HA questionnaire after hearing aid (see ).
Results
A total of 73 ARHL patients finally participated in this study, including 37 males and 36 females, aged between 60 and 95 years with an average of 77.080±7.933 years old. The first fitting age ranged from 56 to 95 years with an average of 76.080±8.733 years, including 24 with unilateral hearing aids and 49 with bilateral hearing aids. BPTA ranged from 42.5 to 90 dB HL with an average of 63.973±12.616 dB HL; BSRR ranged from 10% to 100% with an average of 78.6%±23.0% HL. All the participants completed the IOI-HA questionnaire (full score 35) at least 3 months after using hearing aid, and the total score ranged from 13 to 35 points, with an average of 24.972±4.252 points. IOI-HA factor 1 score (items 1, 2, 4, 7 focus on the individual’s interaction with the hearing aids) ranged from 10 to 20 points with an average of 14.220±2.529 points. Factor 2 score (items 3, 5, 6 focus on the interaction of the individual with other people) ranged from 3 to 15 points, with an average of 10.700±2.361 points. The numerical and counting variables are shown in and .
Table 1 Demographic data for all included participants
Table 2 Count variable data
In this study, the total score is divided into three levels. The first level (ten patients) called “dissatisfied” (total score <21) consists of seven males (70.0%) and three females (30.0%) including four with unilateral hearing aids (40.0%) and six with bilateral hearing aids (60.0%). Their average first fitting age was 79.3±6.7 years, BPTA was 68.4±13.1 dB HL, and BSRR was 41%±25%. The second level (34 patients) called “general satisfied” (21≤ total score ≤27) consists of 15 males (44.1%) and 19 females (55.9%) including eleven with unilateral hearing aids (32.4%) and 23 with bilateral hearing aids (67.6%). Their average first fitting age was 76.1±8.3 years, BPTA was 59.4±9.4 dB HL, and BSRR was 83%±19%. The third level (29 patients) called “very satisfied” (total score >27) consists of 15 males (51.7%) and 14 females (48.3%), including nine unilateral hearing aids (31.0%) and 20 bilateral hearing aids (69.0%). Their average first fitting age was 74.9±9.8 years, BPTA was 67.8±14.2 dB HL, and BSRR was 86%±13%. Gender and unilateral/bilateral hearing aids of each level were compared with the chi-squared test. The gender difference was not statistically significant (χ2=2.092, P>0.05). There was no statistically significant difference between unilateral group and bilateral group (χ2=0.279, P>0.05). The analysis of variance was used to compare first fitting age, laterality of hearing loss, BPTA, and BSRR among each level. The results showed that there was no statistically significant difference in the first fitting age (χ2=0.979, P>0.05) and laterality of hearing loss (χ2=0.900, P>0.05) among the three levels. BPTA (χ2=4.580, P<0.05) and BSRR (χ2=21.789, P<0.01) were both statistically significant ().
Table 3 Chi-squared test and variance analysis
The Pearson’s correlation analysis was used to analyze the correlation among age, first fitting age, BPTA, BSRR, score of factor 1, score of factor 2, and total score of the IOI-HA questionnaire. According to the Shapiro–Wilk test, all variables conformed to Gaussian distribution (P>0.05) and there was no outlier ().
Table 4 Pearson’s correlation analysis
There was no correlation between age and any other factor except for first fitting time (r=0.965, P<0.01).
First fitting age was not correlated to any other score (P>0.05).
There was no statistically significant correlation between BPTA and IOI-HA score (P>0.05).
BSRR was positively correlated with score of factor 1 (r=0.514, P<0.01), score of factor 2 (Q3, 5, 6, r=0.759, P<0.01), and IOI-HA total score (r=0.810, P<0.01).
A multiple regression analysis was conducted for BPTA and BSRR loading on total score subscales to examine if the demographic variables could predict the outcome measures. The observed values had been verified to be independent of each other (the Durbin–Watson test value was 1.317). It was proved that the data has homoscedasticity by drawing the scatter diagram between the residual error of the students and the unnormalized predicted value (). The regression tolerance was greater than 0.1, and there was no multicollinearity. In the abnormal value test, there was no observed value with the residual error of >3 SDs deleted by students. The data leverage value was less than 0.2, and there was no value with Cook’s distance greater than 1. The QQ graph indicated that the study data fitted the Gaussian distribution hypothesis. The regression model had statistical significance (F[3,71] = 12.748, P<0.001, adjusted R2=0.332). BPTA and BSRR were included in the model, and their influence on the total score of IOI-HA questionnaire total score after fitting hearing aid was statistically significant (P<0.05), which is shown in .
Table 5 Multiple linear regression analysis 1
Figure 2 Scatter diagram of BSRR and BPTA.
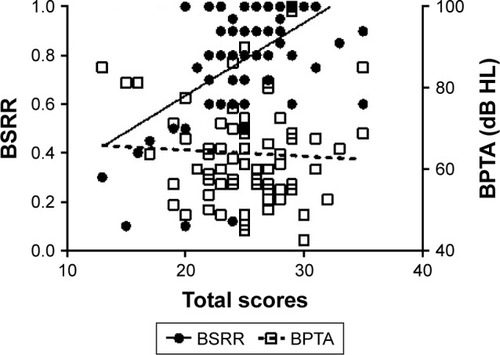
According to the multiple linear regression analysis, prediction equation was obtained: Y=0.109*BPTA + 12.610*BSRR +9.217. That means, when BPTA increases by 10 dB, the total score of IOI-HA is expected to increase by 1.09 points, and 95% of participants are expected to improve by 0.330–1.840 points. When BSRR increases by 10%, the total score of IOI-HA is expected to increase by 1.261, and 95% of the participants are expected to improve by 0.8368–1.6851 points. The effect of first fitting age on the total score of IOI-HA questionnaire after 3 months of hearing aid was not statistically significant ().
Another two multiple linear regression models ( and ) were developed to estimate demographic variables (age and gender) and hearing items (first fitting age and laterality of hearing loss). Both of them were not statistically significant as these factors had little effect on the total score of IOI-HA.
Table 6 Multiple linear regression analysis 2
Table 7 Multiple linear regression analysis 3
Discussion
Hearing loss, especially ARHL, is one of the world’s most prevalent sensory deficits. According to the WHO, 32.8% of the world population over 65 years old are diagnosed with hearing loss.Citation2 There is still no other effective treatment for sensorineural deafness like ARHL except using hearing aids or cochlear implant. Therefore, it is important for physicians to evaluate the efficiency of hearing aids and help users predict the outcome at the same time.
With the acceleration of the aging process in China, the number of presbycusis patients is rapidly increasing. According to the second National Disability Sample Survey, the proportion of people with hearing disabilities over 60 years old is up to 11%. Fitting hearing aids is an effective means of hearing aid intervention and rehabilitation for presbycusis patients, and it is also the main way to improve hearing and speech communication ability among them.Citation4 More and more elderly people are beginning to use hearing aids, and as a result, expectations with regard to hearing aids efficiency are also increasing. Therefore, whether the expected efficiency can be achieved after the fitting is not only an urgent concern of the patients, but is also the direction of the audiological work. Our study is the first report to evaluate the efficiency of hearing aids in ARHL patients by IOI-HA questionnaire in China. This research adopts the IOI-HA questionnaire for evaluating the efficiency of hearing aids. According to the results, we may predict the IOI-HA score outcome and propose advice on clinical hearing aids fitting in advance.
The global score of the IOI-HA questionnaire can initially determine the overall satisfaction of the hearing aid users. Some Chinese experts found that when the questionnaire score is greater than 27 points, the user is very satisfied with the efficiency of the hearing aid; when the total score is between 21 and 27 points, the efficiency is general; and when the total score is less than 21 points, the users are not satisfied with the efficiency of hearing aids.Citation17 It has been reported that 4.7%–24% of presbycusis users discard the hearing aids because the hearing aid is ineffective or unacceptable.Citation18 In this study, a total score of ≥21 points on the IOI-HA questionnaire was reported by 86.3% of the participants, indicating that most subjects were satisfied with the efficiency of hearing aids. This result was higher than that reported by previous studies (50%–70%).Citation13,Citation19,Citation20 On one hand, our individual, accurate, and precise fitting process might account for it. A Swedish study proved that different hearing aids from different institutions have different effects on patients.Citation21 On the other hand, higher proportion of bilateral hearing aids (67.1%) than used in other studies might be an influencing factor.Citation12,Citation13 Brännström et al suggested that bilateral or unilateral aids did not significantly affect the subjective outcome.Citation14 While Arlinger et al reported that clients who received bilateral fitting of hearing aids gave significantly higher scores on all seven items compared with clients with unilateral fittings.Citation21 Cox et al reported that patients prefer bilateral hearing aids vs unilateral hearing aids.Citation20 Referring to several previous studies, Schilder’s review concluded that it is difficult to predict if people with hearing loss would prefer one aid or two aids.Citation22 In our study, no differences were seen between unilateral and bilateral hearing aids. However, it has been a common consensus that bilateral hearing aids are more beneficial than unilateral for auditory and equilibratory sensation of presbycusis patients in the hearing community. Therefore, we suggest presbycusis patients to select bilateral hearing aids.
Brännström et al found that no differences were seen between male and female users.Citation14 Arlinger et al reported that the differences between males and females were small except for item 6.Citation21 In our study, it is likely that gender difference had no statistical effect on the IOI-HA score.
There is still no firm conclusion about whether age or first fitting age may affect the satisfaction of hearing aids. de Wolf et al proved that hearing aid users in younger group experienced more benefit than those in older group.Citation23 Cook et al reported that none of the seven items were significantly related to age.Citation24 We found that age and first fitting age have no influence on IOI-HA outcome. This indicated that ARHL patients should receive hearing aid intervention regardless of age in order to improve their living quality and cognitive ability. In addition, some studies found that hearing aids may increase their communication skills.Citation25 Therefore, it is necessary to fit hearing aids as early as possible.
This study also showed that BPTA and BSRR were associated with satisfaction of hearing aids. Brännström et al found that PTA was not associated with any of the IOI-HA items expect item 1.Citation14 Alinger et al reported that there was no significant correlation between degree of hearing loss and IOI-HA score.Citation21 Jespersen et al found a weak but statistically positive correlation between PTA and items 1 and 4, and a weak but statistically negative correlation between PTA and item 5.Citation15 In our study, according to the multiple linear regression, BSRR and BPTA were statistically related to total score of IOI-HA questionnaire. However, Pearson’s correlation analysis showed that BPTA and total score of IOI-HA did not correlate with each other. That means the degree of hearing loss was partly dependent on the total score, but it was not the main influencing factor. Chang et al considered word recognition score as the most significant associated factor for the outcome of hearing aid use in their research.Citation26 Similarly, we found that main influential factor was BSRR which was positively associated with score of IOI-HA questionnaire. The speech recognition ability is involved in the pathogenesis of the presbycusis. Generally speaking, its pathogenesis refers to degeneration of auditory center more than aging or disease of auditory organ. As is well known, speech recognition ability represents the ability of auditory center and it explains the phenomenon that some patients cannot well digest others after fitting hearing aids so as to affect their satisfaction of hearing aids without serious loss of hearing. It reminds us of defects in our former hearing aids fitting work only according to the pure tone auditory threshold.
Conclusion
The results of this study show that the BSRR is the main positive influencing factor of the IOI-HA questionnaire score. That is to say, the higher the BSRR, the better the efficiency of the hearing aid in presbycusis patients. The speech recognition ability plays a major role in the efficiency of the hearing aid when the patients use the hearing aids. Hearing threshold is partly associated with the efficiency. Those who hear well possibly benefit more from the hearing aids. But it is not an important factor, as the efficiency mainly relies on the cognitive function. Therefore, before fitting the hearing aids, individual, accurate, and precise fitting process, which is a priority for bilateral hearing aids, will achieve high degree of satisfaction. The speech recognition rate can be used to make a relatively accurate prediction of the effect on the patient, not only to guide the patient to establish a reasonable expectation value, but also to promote the trusted relationship between the audiologists and the patient.
There are still some shortcomings in this study. For example, it was difficult to assess the patients’ well-being or quality of life. We hope to expand the sample size of the research in the future work, obtain more possible effective factors, and try to establish an effective prediction equation for the efficiency of hearing aids in ARHL patients.
Acknowledgments
Xu Wu and Yan Ren are co-first authors. Zhiwu Huang and Xueling Wang are co-first corresponding authors. This study was supported by grants from National Natural Science Foundation of China (No 81700899), the National Science Foundation for Young Scientists of China (No 81700903), The State Key Program of National Natural Science Foundation of China (No 81330023), and Shanghai Key Laboratory of Translational Medicine on Ear and Nose Diseases (14DZ2260300). Additional support was received from the Shanghai Key Laboratory of Translational Medicine on Ear and Nose Diseases.
Disclosure
The authors report no conflicts of interest in this work.
References
- GatesGAMillsJHPresbycusisMJHPresbycusisLancet200536694911111112016182900
- BlusteinJWeinsteinBEChodoshJTackling hearing loss to improve the care of older adultsBMJ2018360k2129348197
- HuangQTangJAge-related hearing loss or PresbycusisEur Arch Otorhinolaryngol201026781179119120464410
- PanzaFSolfrizziVLogroscinoGAge-related hearing impairment-a risk factor and frailty marker for dementia and ADNat Rev Neurol201511316617525686757
- HodkinsonHMMental impairment in the elderlyJ R Coll Physicians Lond1973743053174717170
- ThomasPDHuntWCGarryPJHoodRBGoodwinJMGoodwinJSHearing acuity in a healthy elderly population: effects on emotional, cognitive, and social statusJ Gerontol19833833213256841927
- UhlmannRFLarsonEBReesTSKoepsellTDDuckertLGRelationship of hearing impairment to dementia and cognitive dysfunction in older adultsJAMA198926113191619192926927
- ChisolmTHJohnsonCEDanhauerJLA systematic review of health-related quality of life and hearing aids: final report of the American Academy of audiology Task Force on the health-related quality of life benefits of amplification in adultsJ Am Acad Audiol200718215118317402301
- MeisterHRählmannSWalgerMMargolf-HacklSKießlingJHearing aid fitting in older persons with hearing impairment: the influence of cognitive function, age, and hearing loss on hearing aid benefitClin Interv Aging20151043525709417
- HicksonLClutterbuckSKhanAFactors associated with hearing aid fitting outcomes on the IOI-HAInt J Audiol201049858659520515423
- CoxRHydeMGatehouseSOptimal outcome measures, research priorities, and international cooperationEar Hear2000214 Suppl106S115S10981601
- CoxRMAlexanderGCThe international outcome inventory for hearing aids (IOI-HA): psychometric properties of the English versionInt J Audiol2002411303512467367
- LiuHZhangHLiuSChenXHanDZhangLInternational outcome inventory for hearing aids (IOI-HA): results from the Chinese versionInt J Audiol2011501067367821916818
- BrännströmKJWennerströmIHearing aid fitting outcome: clinical application and psychometric properties of a Swedish translation of the international outcome inventory for hearing aids (IOI-HA)J Am Acad Audiol201021851252121034698
- Thunberg JespersenCBilleMLegarthJVPsychometric properties of a revised Danish translation of the international outcome inventory for hearing aids (IOI-HA)Int J Audiol201453530230824475867
- ZhangHWangSWangLDevelopment and equivalence evaluation of spondee lists of mandarin speech test materialsZhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi2006416425429 Chinese16927797
- KongYZhangHChenXWuYLiuHThe application of the international outcome inventory for hearing aids on the hearing aid outcome measurementJournal of Audiology and Speech Pathology (in Chinese)2010186591594
- MccormackAFortnumHHjijoaFWhy do people fitted with hearing aids not wear them?Int J Audiol201352536036823473329
- WuYHHoHCHsiaoSHBrummetRBChiparaOPredicting three-month and 12-month post-fitting real-world hearing-aid outcome using pre-fitting acceptable noise level (ANL)Int J Audiol201655528529426878163
- CoxRMSchwartzKSNoeCMAlexanderGCPreference for one or two hearing aids among adult patientsEar Hear201132218119720890203
- ArlingerSNordqvistPÖbergMInternational outcome inventory for hearing aids: data from a large Swedish quality register databaseAm J Audiol2017263S44345029049627
- SchilderAGChongLYFtouhSBurtonMJBilateral versus unilateral hearing aids for bilateral hearing impairment in adultsCochrane Database Syst Rev201712CD01266529256573
- de WolfMJFLeijendeckersJMMylanusEAMAge-related use and benefit of the bone-anchored hearing aid compactOtology & Neurotology200930678779219638942
- CookJAHawkinsDBOutcome measurement for patients receiving hearing aid servicesLaryngoscope2007117461061317415130
- KayabaşoğluGKaymazRErkorkmazÜGüvenMStudy of hearing aid effectiveness and patient satisfactionKulak Burun Bogaz Ihtis Derg201525315816226050856
- ChangYSChoiJMoonIJHongSHChungWHChoYSFactors associated with self-reported outcome in adaptation of hearing aidActa Otolaryngol2016136990591127110845