Abstract
Purpose
To study the efficacy of traditional Thai massage (TTM) versus conventional physical therapy (PT) programs in treating muscle spasticity, functional ability, anxiety, depression, and quality of life (QoL) in Thai stroke patients.
Methods
This randomized controlled trial with a blinded assessor was carried out at the Department of Rehabilitation Medicine, Siriraj Hospital (Bangkok, Thailand). The study included 50 stroke (onset ≥3 months) outpatients experiencing spasticity at the elbow or knee muscles at a grade of ≥1+ on the modified Ashworth Scale who were ≥50 years old and able to communicate. The subjects were randomly allocated to the treatment group receiving TTM (24 subjects) or the control group receiving the PT program (26 subjects). Both groups received treatment (either TTM or PT) twice a week for 6 weeks. Spasticity grade, functional ability, anxiety, depression, and QoL were measured at Week 0 and Week 6.
Results
At Week 6, the percentage of patients whose modified Ashworth Scale score had decreased by at least one grade was not statistically significant between the two groups. Both TTM and PT groups experienced a significant increase in functional ability and QoL, but no difference was found between the groups. Anxiety and depression scores showed a decreasing trend in the TTM group.
Conclusion
This preliminary report showed no evidence that TTM differed from the PT program in decreasing spasticity. However, both interventions may relieve spasticity, increase functional ability, and improve QoL after 6 weeks. Only TTM can decrease anxiety and depression scores. Further studies with adequate sample size are necessary.
Keywords:
Introduction
Worldwide, stroke is one of the common ailments among the elderly. It is the third-ranking cause of death, and therefore affects the health care system in Thailand.Citation1 One of the common consequences of stroke is spasticity. It is defined as a motor disorder that is characterized by a velocity-dependent increase in tonic stretch reflexes (muscle tone) with exaggerated tendon jerks, resulting from hyperexcitability of the stretch reflexes.Citation2 The prevalence of post-stroke spasticity has ranged from 19%Citation3 to 39%Citation4 of stroke patients at 3 months and 12 months after experiencing stroke, respectively. In Thailand, the prevalence of post-stroke spasticity during rehabilitation was 41.6%.Citation5 However, recent studies reported that the increased resistance of muscles with spasticity to passive movement is due not only to hyperexcitability reflexes, but also to altered properties of the muscle tissue.Citation6,Citation7 Spasticity can cause pain, abnormal posture, and joint contracture. It may interfere with functional recovery and the ability to perform daily activities, resulting in decreasing quality of life (QoL) and increasing caregiver burden.
Currently, many methods for decreasing spasticity are available, including pharmacological and nonpharmacological treatments. The pharmacological therapies, such as oral anti-spastic drugs,Citation8,Citation9 botulinum toxin injection,Citation9–Citation11 phenol injections,Citation9,Citation12 alcohol injection,Citation13 and intrathecal baclofen,Citation14,Citation15 usually focus on reducing reflex hyperexcitability. Nonpharmacological treatments, which aim to inhibit neural activity, reduce muscle stiffness, and improve the surrounding connective tissue, include heat modalities, cryotherapy, electrical stimulation, stretching, splinting, acupuncture, and massage.Citation16,Citation17
The mechanisms of massage on spasticity vary depending on technique. Goldberg et al found that petrissage massage above the lumbar area can reduce H-reflex amplitude in the calf muscles of people with traumatic spinal cord injury.Citation18 This result reflects a reduction in motor neuron excitability. Deep massage can stretch the muscle that experiences spasticity and reset sarcomere lengths to a more optimal state. It helps to break down subcutaneous adhesions and prevent fibrosis,Citation19 and may lead to improved sensory feedback from muscle spindle receptors. Moreover, the repetitive cutaneous stimulation provided by massage may reduce pain through the gate control theory.Citation20
There have been a few study reports related to massage and spasticity. Unfortunately, these studies were reported in local languages. Only one randomized control trial was found, which reported the efficacy of rehabilitation exercise therapy in decreasing post-stroke hemiplegia limb muscle spasticity compared with traditional Chinese massage therapy.Citation21 Their curative effects on patients were evaluated 4 weeks after treatment using the modified Ashworth Scale (MAS) and limb motor function integration scale, and by measuring the changes in activities of daily living. The researchers concluded, by examining total effective rates, that rehabilitation exercise therapy could improve muscle spasticity significantly more than traditional Chinese massage therapy. However, this study was published in Chinese. Thus, it cannot clearly be stated how the previous study measured the total effective rate and the details of the massage technique and dosage used.
Traditional Thai massage (TTM) is the most popular alternative medicine in Thailand. People have been acquainted with this massage for over a century. Currently, it is well recognized and regulated by the Thai government. Although massage is found worldwide in clinical practice, the scientific evidence that supports the effectiveness of massage in decreasing spasticity is limited. Therefore, a randomized controlled trial with a single-blinded assessor was performed to compare the effects of TTM and conventional physical therapy (PT) on spasticity, functional ability, anxiety, depression, and QoL in stroke patients.
Methods
The current study was a randomized trial. The study protocol was conducted in accordance with the ethical principles stated in the most recent version of the Declaration of Helsinki. After the study protocol was approved by the Institutional Review Board of Siriraj Hospital, stroke patients were recruited from the outpatient unit of the Department of Rehabilitation Medicine, Faculty of Medicine Siriraj Hospital (Bangkok, Thailand) from August 2011 through July 2013. Chronic stroke (onset ≥3 months) patients with moderate-to-severe spasticity of the elbow or knee in at least one limb (grade ≥1+), as evaluated by the MAS, who were aged ≥50 years and able to communicate, were eligible to participate. Subjects who had contraindications for massage, eg, fever 38°C or greater, uncontrolled blood pressure, bleeding tendencies, taking anticoagulant drugs, unhealed fractures, contact dermatitis, skin infections, or severe osteoporosis, were excluded. Additionally, fixed joint contracture, a history of botulinum toxin injection within the last 6 months, a history of nerve block within the past year, severe dementia, or uncontrolled psychological disorders were excluded. The study would be terminated if severe adverse events occurred, including fractures or hematomas in the muscle or soft tissue of the patients.
After providing consent, subjects were randomly assigned to undergo TTM or the conventional PT program. A computer-generated randomization number was used, and the allocation codes were kept in opaque envelopes. An external investigator selected consecutive allocation envelopes for consecutive participants.
Patients who were randomized into the treatment group received court-type TTM, two nonconsecutive days per week for 6 weeks. Five certified personnel who performed massage for the duration of the study were standardized according to a Thai massage organization. Therapists performed the massage with the same procedure over the hemiplegic side for 1 hour per session. The basic massage lines and major signal points were the main massage treatment using only thumb and hand pressing at the point without traction or stretching. The basic massage lines were pressed for 10 seconds and the major signal points were pressed for 30 seconds per point. Massage points included in this study were located in the leg, back, abdomen, arm, shoulder, and neck regions. The details of the massage protocol are presented in .
The PT group received a range of motion exercises for paralyzed limbs, strengthening exercises for the sound limbs, balance exercises for sitting and standing, and ambulation training in those who had potential for walking. The program was administered by a trained physical therapist for 1-hour sessions, two times a week for 6 weeks.
Regarding the primary outcome, the percentage of patients who improved after treatment, ie, patients whose MAS decreased by at least one grade after treatment, was measured. The MAS is a common clinical test used to determine spasticity, with ratings from zero (no increase in muscle tone) to four (the affected part is rigid in flexion or extension).Citation22 For secondary outcomes, the Barthel Index (BI) was used to measure functional abilities in self-care and mobility.Citation23 Possible scores range from 0–20, with a higher score meaning better functions. To measure the patients’ psychological status, the Thai version of the Hospital Anxiety and Depression Scale (HADS) was used to screen for anxiety and depression.Citation24 The scores for each subscale (anxiety and depression) range from 0–21 with scores of eleven or greater indicating the presence of a disorder.Citation24–Citation26 Additionally, the Pictorial Thai QoL Test was used to evaluate QoL.Citation27 It is composed of six dimensions: physical, cognitive, affective, social function, economics, and self-esteem. Scores range from 0–72, where a higher score represents a better quality of life. The adverse events that occurred in both groups were also recorded. At the end of the study, the patients were asked about feelings of spasticity and the use of limbs’ functions as subjective outcomes. Satisfaction level was also evaluated among both groups.
Statistical analysis
The sample size of 186 patients (93 in each group) provides a power of 80% to detect differences in the primary outcome (ie, the percentage of patients whose spasticity decreased by at least one grade after treatment) between a PT group of 30% and a TTM group of 50%, at a 5% two-sided significance level.Citation28
Demographic and baseline characteristics are presented as descriptive statistics in . Unpaired t-test was used to compare continuous data including age, BI, HADS, and QoL scores. Chi-square and Fisher’s exact tests were used to compare categorical data. Multiple logistic regression was used to adjust for age and sex for comparing the primary outcome. Mean changes in the scores of the BI, HADS, and Pictorial Thai QoL at baseline, compared with 6-week scores, were analyzed using paired t-tests, and the mean differences in those scores were compared between groups by using unpaired t-tests. The number of adverse events and patients’ assessment of outcomes were compared using the chi-square test and Fisher’s exact test. A P-value of less than 0.05 was considered statistically significant. For the primary outcome, intention-to-treat (ITT) analysis, with the last observation carried forward method, was performed in addition to per protocol (PP) analysis.
Table 1 Demographic and baseline characteristics
Results
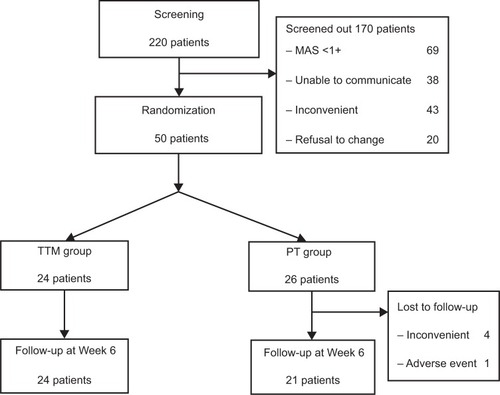
A total of 220 stroke patients were enrolled in the study, but 170 subjects were screened out owing to their spasticity grade (MAS) being <1+ (69 patients), inability to communicate (38 patients), complaints of inconvenience (43 patients), or refusals to change their treatment program (20 patients). Only 50 patients were randomized to receive TTM (24 patients) or the PT program (26 patients) twice weekly for the 6-week duration. At the end of study, five patients in the PT group were lost to follow-up owing to inconvenience (four patients) and having repeat hemorrhagic strokes (one patient), as shown in . The demographic data of the 50 subjects in the TTM and PT groups did not differ except for sex, age, and BI scores (). Patients in the TTM group were predominantly male (92% versus 58%), younger in age (60 years versus 66 years), and had higher BI scores (16.4 versus 10.9) compared with the PT group. A muscle with maximal grading measured by MAS was not different between the groups. Anxiety, depression, and QoL scores did not differ between the groups at baseline.
Figure 1 Flow diagram of the study.
The main outcome was the percentage of subjects whose MAS score decreased by at least one grade after treatment. The TTM group had a higher percentage of subjects whose spasticity improved by at least one grade than the PT group in both types of analysis (70.8% versus 61.9% in PP analysis; 70.8% versus 50.0% in ITT analysis). However, there was no statistically significant difference between the two groups, regardless of whether it was analyzed by PP analysis (P=0.286) or ITT analysis (P=0.058) in muscles with maximal grade ( and , respectively).
Table 2 Number and percentage of subjects whose spasticity decreased by at least one grade between baseline and after treatment among the two groups, using per protocol analysis
Table 3 Number and percentage of subjects whose spasticity decreased by at least one grade between baseline and after treatment among the two groups, using intention-to-treat analysis with the last observation carried forward method
shows that, for secondary outcomes, BI scores increased significantly at Week 6 compared with baseline in both groups (P=0.008 and P=0.025 in TTM and PT groups, respectively), but no difference was found between the groups (P=0.805). illustrates the psychological aspects; anxiety scores in the TTM group had decreased at Week 6 compared with baseline scores (P=0.083), while the anxiety scores in the PT group had increased at Week 6 (P=0.624). However, there was no difference in the scores when the two groups were compared (P=0.144). shows the depression scores after treatment. The depression scores in the TTM group had decreased at Week 6 compared with baseline scores but were not significantly different (P=0.195), whereas depression scores increased in the PT group (P=0.747). No difference was found between the groups (P=0.313).
Figure 2 Functional ability evaluated using the Barthel Index at Week 0 and Week 6.
Note: *Statistically significant at P<0.05.
Abbreviation: PT, physical therapy.
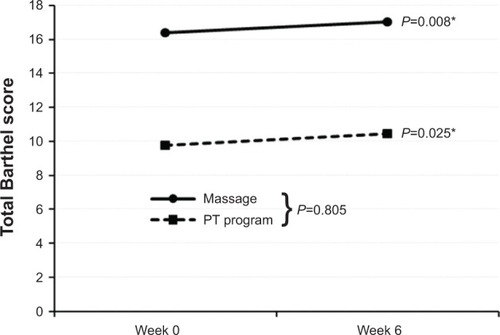
Figure 3 Anxiety scores at Week 0 and Week 6.
Abbreviations: HADS, Hospital Anxiety and Depression Scale; PT, physical therapy.
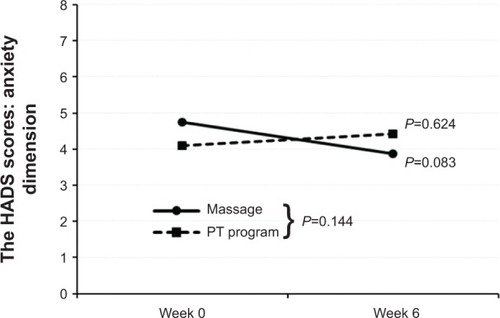
Figure 4 Depression scores at Week 0 and Week 6.
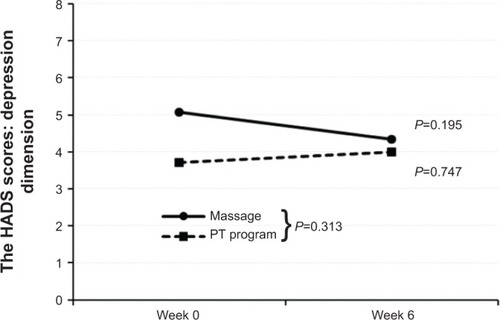
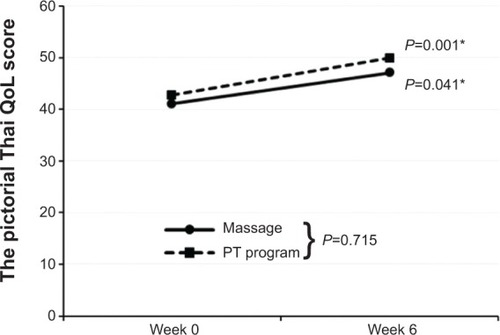
presents the QoL of the TTM and PT groups at Week 0 and Week 6. At the end of study, the total QoL scores of both groups had increased significantly when compared with baseline scores (P=0.041 in TTM; P=0.001 in PT groups). However, there was no significant difference between the groups (P=0.715).
Figure 5 Quality of life scores at Week 0 and Week 6.
Abbreviations: PT, physical therapy; QoL, quality of life.
compares patients’ assessments of their outcomes by group. The number of patients in the TTM group who reported that their feelings of spasticity had decreased was greater than those who reported the same in the PT group (79.2% versus 52.4%; P=0.057). However, the functions of their limbs improved only 37%–38% with no difference between the groups (P=0.967). Concerning patient satisfaction, 90.5% of the patients were satisfied with the PT program compared with 75% of the massage patients. Again, there was no significant difference between the two groups (P=0.427). The number of adverse events that occurred during the study did not differ between the groups (P=0.807), as shown in . There were more patients who experienced adverse events of muscle stiffness, muscle pain, and muscle soreness in the TTM group compared with those in the PT group. However, no significant difference between the groups was found.
Table 4 Patients’ assessment of outcomes
Table 5 Number of adverse events that occurred during the study by group
Discussion
TTM is one of the methods of alternative medicine that is easily accessible in Thailand. People choose massage with the aim of relaxing their muscles. It is very popular among Thai people and patients alike. Studies examining whether TTM was effective in decreasing muscle spasticity in stroke patients were scarce. The current study revealed that the percentage of subjects whose MAS scores had decreased by at least one grade after treatment in the TTM group seemed to be greater than that of the PT program group. After using ITT analysis, the results displayed more significant differences than those from the PP analysis; however, no significant difference was found in both analyses. Additionally, the number of patients in the TTM group who reported that their feelings of spasticity decreased was greater than that of the PT group. This subjective outcome was consistent with the number of patients whose MAS (ie, an objective outcome) had decreased by at least one grade. However, these findings were not in line with Chen and Li’s study. They reported that rehabilitation exercise therapy can improve muscle spasticity in post-stroke hemiplegia significantly more than traditional Chinese massage therapy.Citation21 This might be due to the different style, as well as dosage, of massage.
Although both TTM and PT programs increased the BI score by the conclusion of the study, there was no difference in the BI score between the two groups. It was assumed that the decrease in spasticity in both groups may result in subjects using their affected limbs more easily and causing functional improvement after treatment. Additionally, the ability to perform daily activities can improve through spontaneous motor recovery in subacute stroke patients and functional adaptation after PT program.Citation29
A decreasing trend in anxiety and depression scores at Week 6 was only found in the TTM group, whereas those in the PT group seemed to exhibit an increasing trend instead. This means that only the TTM group reported trends of improvement in anxiety and depression post-treatment. The reasons for the differences in psychological outcomes between groups are possible from enhancing the parasympathetic nervous systemCitation30 and relieving muscle tension in the TTM group.Citation31 These results were consistent with a meta-analysis of massage therapy research by Moyer et al who reported that multiple doses of massage therapy can significantly reduce the traits of anxiety and depression.Citation32
Moreover, QoL scores in both the TTM and PT group increased between baseline and Week 6, with no difference between the two groups. This means that both TTM and PT treatments may improve QoL in stroke patients.
Ninety percent of the patients in the PT group were satisfied with the treatment program, compared with only 75% of the TTM group reporting satisfaction. The reason why patients have been less satisfied with TTM may be due to the number of adverse events that occurred in the massage group, especially muscle stiffness, muscle pain, and muscle soreness. This finding was consistent with a qualitative study by van der Riet et al on TTM used in stroke patients.Citation33 They reported that some stroke patients experienced pain after receiving massages, and the younger patients preferred to exercise rather than to receive massages. Though massage seems to be effective in decreasing spasticity in stroke patients, medical personnel should recognize that pressure during massage could adversely affect muscles. Therefore, standardized techniques of massage, in addition to the development of equipment for measuring pressure, are necessary.
Study limitations
The main limitation of this study was the small sample size. A large number of patients were excluded for reasons such as communication difficulties, spasticity that was too mild, wishing to avoid inconvenience, and refusal to change their current treatment program. In addition, this study only recruited outpatients. Some patients could not visit the hospital without assistance, so they declined to join the study. Moreover, there were slight differences in the demographic characteristics between the two groups. These differences could influence the results of study. For example, a low BI at baseline has been suggested as one of the predictors for the presence of severe spasticity. Thus, subjects who had a low BI score in the PT group may have a higher chance of developing spasticityCitation34 and less potential for recovery.Citation35 On the other hand, the BI is not sensitive for detecting change in stroke patients with a high BI score at baseline due to its ceiling effect.Citation36 However, these variables were adjusted during analysis of the results. Finally, this study did not evaluate the long-term effect of massage on spasticity. Further studies with adequate sample size and long term follow-up are suggested.
Conclusion
This preliminary study could not demonstrate that TTM differs from conventional PT programs in decreasing spasticity or improving limb functions. Although no statistical significance was found, there were trends in decreasing spasticity, anxiety, and depression scores in the TTM group compared with the PT group. Massage may be an alternative method for stroke patients to decrease spasticity, improve psychological conditions and QoL. Further studies employing an adequate sample size and evaluating the long-term effect of massage are needed.
Acknowledgments
The authors would like to thank Mr Suthiphol Udompunturuk and Ms Julaporn Poolium for statistical analyses, Assistant Professor Somkiat Sangwatanaroj for translating Chinese research into Thai language, and Professor Manee Rattanachaiyanont for reviewing the manuscript.
This study was supported by the National Research Council of Thailand (NRCT). The trial registration number is NCT1448980.
Supplementary material
Table S1 Step, area, and duration of traditional Thai massage protocol
Disclosure
The authors report no conflicts of interest in this work.
Reference
- Bureau of Health Policy and Strategy Ministry of Public HealthPublic Health Statistics 2010BangkokThailand Ministry of Public Health2010 Available from: http://bps.ops.moph.go.th/Healthinformation/statistic53/statistic53.pdfAccessed November 20, 2013 Thai
- LanceJWThe control of muscle tone, reflexes, and movement: Robert Wartenberg LectureNeurology19803012130313137192811
- SommerfeldDKEekEUSvenssonAKHolmqvistLWvon ArbinMHSpasticity after stroke: its occurrence and association with motor impairments and activity limitationsStroke200435113413914684785
- WatkinsCLLeathleyMJGregsonJMMooreAPSmithTLSharmaAKPrevalence of spasticity post strokeClin Rehabil200216551552212194622
- DajprathamPKuptniratsaikulVKovindhaAKuptniratsaikulPDejnuntaratKPrevalence and management of poststroke spasticity in Thai stroke patients: a multicenter studyJ Med Assoc Thai200992101354136019845244
- LieberRLSteinmanSBarashIAChambersHStructural and functional changes in spastic skeletal muscleMuscle Nerve200429561562715116365
- ForanJRSteinmanSBarashIChambersHGLieberRLStructural and mechanical alterations in spastic skeletal muscleDev Med Child Neurol2005471071371716174321
- AbbruzzeseGThe medical management of spasticityEur J Neurol20029Suppl 1S30S34
- GallichioJEPharmacological management of spasticity following strokePhys Ther2004841097398115449979
- TurkelCCBowenBLiuJBrinMFPooled analysis of the safety of botulinum toxin type A in the treatment of poststroke spasticityArch Phys Med Rehabil200687678679216731213
- OzcakirSSivriogluKBotulinum toxin in poststroke spasticityClin Med Res20075213213817607049
- McCreaPHEngJJWillmsRPhenol reduces hypertonia and enhances strength: a longitudinal case studyNeurorehabil Neural Repair200418211211615228807
- JangSHAhnSHParkSMKimSHLeeKHLeeZIAlcohol neurolysis of tibial nerve motor branches to the gastrocnemius muscle to treat ankle spasticity in patients with hemiplegic strokeArch Phys Med Rehabil200485350650815031842
- MeythalerJMGuin-RenfroeSBrunnerRCHadleyMNIntrathecal baclofen for spastic hypertonia from strokeStroke20013292099210911546903
- FranciscoGEBoakeCImprovement in walking speed in poststroke spastic hemiplegia after intrathecal baclofen therapy: a preliminary studyArch Phys Med Rehabil20038481194119912917859
- NancePWMeythalerJMSpasticity managementBraddomRLPhysical Medicine and Rehabilitation3rd edPhiladelphiaSaunders2007661
- WatanabeTThe role of therapy in spasticity managementAm J Phys Med Rehabil20048310 SupplS45S4915448577
- GoldbergJSeaborneDESullivanSJLeducBEThe effect of therapeutic massage on H-reflex amplitude in persons with a spinal cord injuryPhys Ther19947487287378047561
- DonnellyCJWiltonJThe effect of massage to scars on active range of motion and skin mobilityHand Ther200271511
- GraciesJMPhysical modalities other than stretch in spastic hypertoniaPhys Med Rehabil Clin N Am200112476979211723865
- ChenQLiLObservation on curative effect of rehabilitation exercise therapy to treat patients with post-stroke hemiplegia and muscles spasmChinese Nursing Research20102411416
- BohannonRWSmithMBInterrater reliability of a modified Ashworth scale of muscle spasticityPhys Ther19876722062073809245
- MahoneyFIBarthelDWFunctional evaluation: the Barthel IndexMd State Med J196514616514258950
- NilchaikovitTLortrakulMPhisansuthidethUDevelopment of Thai version of Hospital Anxiety and Depression Scale in cancer patientsJ Psychiatr Assoc Thai19964111830
- ZigmondASSnaithRPThe Hospital Anxiety and Depression ScaleActa Psychiatr Scand19836763613706880820
- BjellandIDahlAAHaugTTNeckelmannDThe validity of the Hospital Anxiety and Depression Scale: an updated literature reviewJ Psychosom Res2002522697711832252
- PhattharayuttawatSNgamthipwatthanaTPitiyawaranunBThe development of the Pictorial Thai Quality of LifeJ Med Assoc Thai200588111605161816471109
- Barros GalvaoSCBorba Costa dos SantosRBorba dos SantosPCabralMEMonte-SilvaKEfficacy of coupling repetitive transcranial magnetic stimulation and physical therapy to reduce upper-limb spasticity in patients with stroke: a randomized controlled trialArch Phys Med Rehabil201495222222924239881
- KotilaMWaltimoONiemiMLLaaksonenRLempinenMThe profile of recovery from stroke and factors influencing outcomeStroke1984156103910446506115
- DiegoMAFieldTModerate pressure massage elicits a parasympathetic nervous system responseInt J Neurosci2009119563063819283590
- JormAFChristensenHGriffithsKMParslowRARodgersBBlewittKAEffectiveness of complementary and self-help treatments for anxiety disordersMed J Aust20041817 SupplS29S4615462640
- MoyerCARoundsJHannumJWA Meta-analysis of massage therapy researchPsychol Bull2004130131814717648
- van der RietPDedkhardSSrithongKComplementary therapies in rehabilitation: stroke patients’ narratives. Part 2J Clin Nurs2012215–666867622098401
- WisselJScheloskyLDScottJChristeWFaissJHMuellerJEarly development of spasticity following stroke: a prospective, observational trialJ Neurol201025771067107220140444
- CouparFPollockARowePWeirCLanghornePPredictors of upper limb recovery after stroke: a systematic review and meta-analysisClin Rehabil201226429131322023891
- DuncanPWSamsaGPWeinbergerMHealth status of individuals with mild strokeStroke19972847407459099189

